The Impact of Insurance and Marital Status on Survival in Patients with Nasopharyngeal Carcinoma
Abstract
1. Introduction
2. Materials and Methods
2.1. Data and Patient Selection
2.2. Study Variables
2.3. Statistical Analysis
3. Results
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Syse, A.; Lyngstad, T.H. In sickness and in health: The role of marital partners in cancer survival. SSM-Popul. Health 2017, 3, 99–110. [Google Scholar] [CrossRef] [PubMed]
- Shi, R.-l.; Qu, N.; Lu, Z.-w.; Liao, T.; Gao, Y.; Ji, Q.-h. The impact of marital status at diagnosis on cancer survival in patients with differentiated thyroid cancer. Cancer Med. 2016, 5, 2145–2154. [Google Scholar] [CrossRef]
- Wang, L.; Wilson, S.E.; Stewart, D.B.; Hollenbeak, C.S. Marital status and colon cancer outcomes in US Surveillance, Epidemiology and End Results registries: Does marriage affect cancer survival by gender and stage? Cancer Epidemiol. 2011, 35, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.D.; Wang, X.; Habif, D.V., Jr.; Ma, C.X.; Johnson, K.J. Breast cancer stage variation and survival in association with insurance status and sociodemographic factors in US women 18 to 64 years old. Cancer 2017, 123, 3125–3131. [Google Scholar] [CrossRef]
- Zhang, Y.; Franzini, L.; Chan, W.; Xu, H.; Du, X.L. Effects of Health Insurance on Tumor Stage, Treatment, and Survival in Large Cohorts of Patients with Breast and Colorectal Cancer. J. Health Care Poor Underserved 2015, 26, 1336–1358. [Google Scholar] [CrossRef]
- Churilla, T.; Egleston, B.; Dong, Y.; Shaikh, T.; Murphy, C.; Mantia-Smaldone, G.; Chu, C.; Rubin, S.; Anderson, P. Disparities in the management and outcome of cervical cancer in the United States according to health insurance status. Gynecol. Oncol. 2016, 141, 516–523. [Google Scholar] [CrossRef]
- Niu, X.; Roche, L.M.; Pawlish, K.S.; Henry, K.A. Cancer survival disparities by health insurance status. Cancer Med. 2013, 2, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Qiu, M.; Yang, D.; Xu, R. Impact of marital status on survival of gastric adenocarcinoma patients: Results from the Surveillance Epidemiology and End Results (SEER) Database. Sci. Rep. 2016, 6, 21098. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics, 2017. CA Cancer J. Clin. 2017, 67, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Ou, S.H.; Zell, J.; Ziogas, A.; Anton-Culver, H. Epidemiology of nasopharyngeal carcinoma in the United States: Improved survival of Chinese patients within the keratinizing squamous cell carcinoma histology. Ann. Oncol. 2006, 18, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.G.; Zhang, Q.H.; Zhang, W.W.; Sun, J.Y.; Lin, Q.; He, Z.Y. The Effect of Marital Status on Nasopharyngeal Carcinoma Survival: A Surveillance, Epidemiology and End Results Study. J. Cancer 2018, 9, 1870–1876. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Liu, X.; Chen, Y.P.; Mao, Y.P.; Guo, R.; Zhou, G.Q.; Tang, L.L.; Lin, A.H.; Sun, Y.; Ma, J. Impact of marital status at diagnosis on survival and its change over time between 1973 and 2012 in patients with nasopharyngeal carcinoma: A propensity score-matched analysis. Cancer Med. 2017, 6, 3040–3051. [Google Scholar] [CrossRef] [PubMed]
- Osborne, C.; Ostir, G.V.; Du, X.; Peek, M.K.; Goodwin, J.S. The Influence of Marital Status on the Stage at Diagnosis, Treatment, and Survival of Older Women with Breast Cancer. Breast Cancer Res. Treat. 2005, 93, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Aizer, A.A.; Chen, M.H.; McCarthy, E.P.; Mendu, M.L.; Koo, S.; Wilhite, T.J.; Graham, P.L.; Choueiri, T.K.; Hoffman, K.E.; Martin, N.E.; et al. Marital status and survival in patients with cancer. J. Clin. Oncol. 2013, 31, 3869–3876. [Google Scholar] [CrossRef] [PubMed]
- Liao, P.-H.; Lee, C.-C. The influence of marital status on survival for patients aged 65 years and younger with oral cavity cancer. Auris Nasus Larynx 2018, 45, 1227–1232. [Google Scholar] [CrossRef] [PubMed]
- Gomez, S.L.; Hurley, S.; Canchola, A.J.; Keegan, T.H.; Cheng, I.; Murphy, J.D.; Clarke, C.A.; Glaser, S.L.; Martinez, M.E. Effects of marital status and economic resources on survival after cancer: A population-based study. Cancer 2016, 122, 1618–1625. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Fan, J. The effect of a complex healing treatment on 2-year survival rate of patients with malignant tumors. Integr. Cancer Ther. 2008, 7, 18–23. [Google Scholar]
- Tam Ashing, K.; Padilla, G.; Tejero, J.; Kagawa-Singer, M. Understanding the breast cancer experience of Asian American women. Psycho-Oncol. 2003, 12, 38–58. [Google Scholar]
- Ozkan, S.; Ogce, F. Importance of social support for functional status in breast cancer patients. Asian Pac. J. Cancer Prev. APJCP 2008, 9, 601–604. [Google Scholar] [PubMed]
- Walker, G.V.; Grant, S.R.; Guadagnolo, B.A.; Hoffman, K.E.; Smith, B.D.; Koshy, M.; Allen, P.K.; Mahmood, U. Disparities in stage at diagnosis, treatment, and survival in nonelderly adult patients with cancer according to insurance status. J. Clin. Oncol. 2014, 32, 3118–3125. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Insured | Any Medicaid | Uninsured | |
|---|---|---|---|---|
| Variables | n (%) | n (%) | n (%) | p Value |
| Age, years (Mean ± SD) | 54 ± 13 | 49 ± 16 | 48 ± 10 | <0.001 |
| Gender | 0.115 | |||
| Male | 649 (69.6%) | 200 (70.2%) | 66 (80.5%) | |
| Female | 284 (30.4%) | 85 (29.8%) | 16 (19.5%) | |
| AJCC cT | <0.001 | |||
| T1 | 358 (38.4%) | 98 (34.4%) | 22 (26.8%) | |
| T2 | 302 (32.4%) | 67 (23.5%) | 25 (30.5%) | |
| T3 | 223 (23.9%) | 90 (31.6%) | 21 (25.6%) | |
| T4 | 50 (5.4%) | 30 (10.5%) | 14 (17.1%) | |
| AJCC cN | <0.001 | |||
| N0 | 248 (26.6%) | 51 (17.9%) | 17 (20.7%) | |
| N1 | 337 (36.1%) | 99 (34.7%) | 23 (28.0%) | |
| N2 | 251 (26.9%) | 73 (25.6%) | 22 (26.8%) | |
| N3 | 97 (10.4%) | 62 (21.8%) | 20 (24.4%) | |
| AJCC cM | <0.001 | |||
| M0 | 841 (90.1%) | 239 (83.9%) | 59 (72.0%) | |
| M1 | 92 (9.9%) | 46 (16.1%) | 23 (28.0%) | |
| Radiotherapy | <0.001 | |||
| Yes | 841 (90.1%) | 244 (85.6%) | 62 (75.6%) | |
| No | 92 (9.9%) | 41 (14.4%) | 20 (24.4%) | |
| WHO category | 0.070 | |||
| WHO I-II | 541 (58.0%) | 148 (51.9%) | 53 (64.6%) | |
| WHO III | 392 (42.0%) | 137 (48.1%) | 29 (35.4%) | |
| Race | <0.001 | |||
| Non black | 865 (92.7%) | 240 (84.2%) | 62 (75.6%) | |
| Black | 68 (7.3%) | 45 (15.8%) | 20 (24.4%) | |
| Marital status | <0.001 | |||
| Married | 670 (71.8%) | 121 (42.5%) | 34 (41.5%) | |
| Others | 263 (28.2%) | 164 (57.5%) | 48 (58.5%) |
| Variables | Total | Event (%) | HR (95%CI) | p Value |
|---|---|---|---|---|
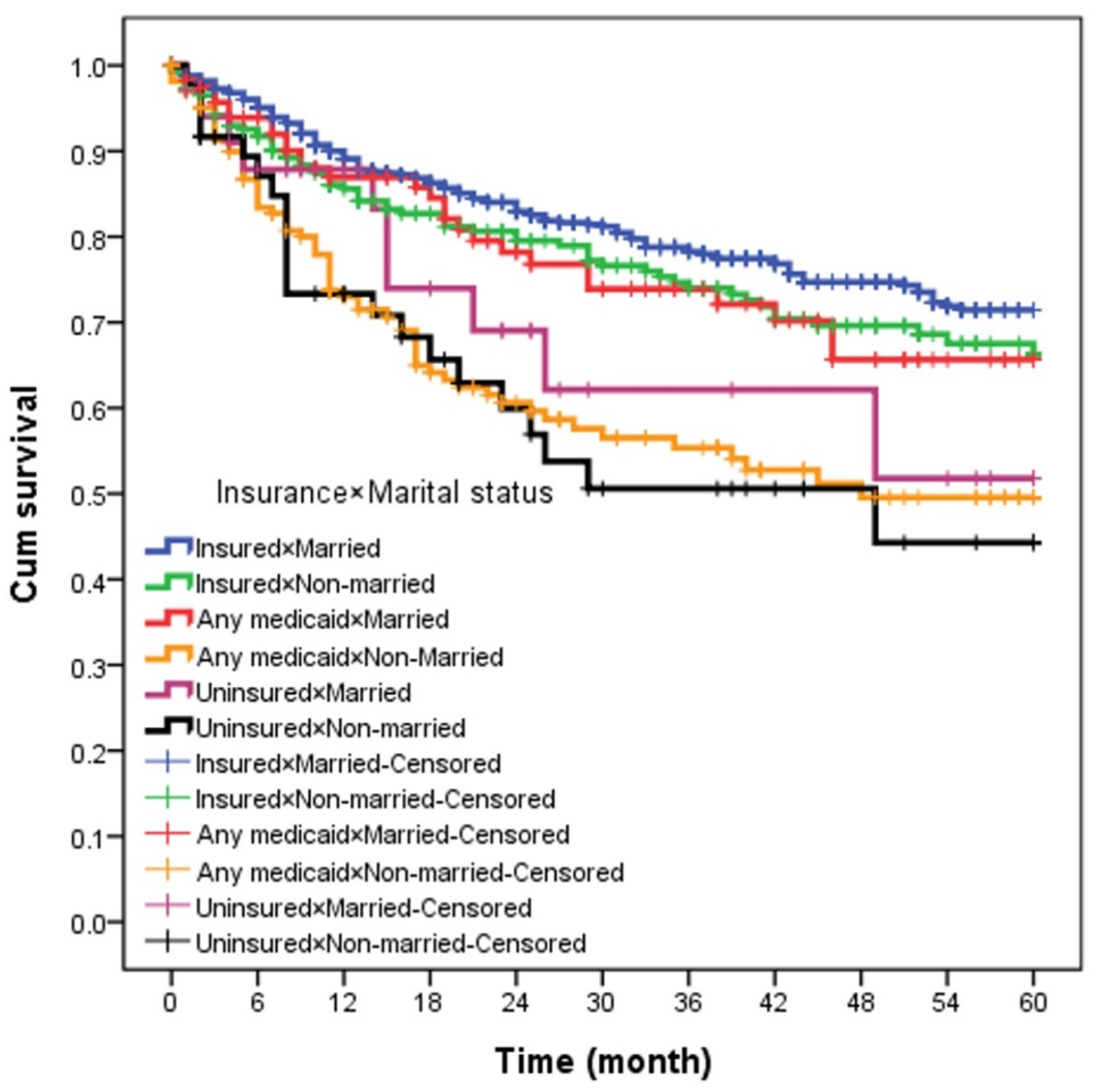
| Insurance × marital status | ||||
| Insured × married | 670 | 138 (20.6%) | 1 | |
| Insured × non-married | 263 | 65 (24.7%) | 1.26 (0.94–1.69) | 0.125 |
| Any Medicaid × married | 121 | 28 (23.1%) | 1.28 (0.86–1.93) | 0.228 |
| Any Medicaid × non-married | 164 | 65 (39.6%) | 2.42 (1.80–3.25) | <0.0001 |
| Uninsured × married | 34 | 10 (29.4%) | 1.88 (0.99–3.57) | 0.054 |
| Uninsured × non-married | 48 | 21 (43.8%) | 2.66 (1.68–4.21) | <0.0001 |
| Variables | OR (95%CI) | p Value |
|---|---|---|
| Insurance × marital status | ||
| Insured × married | 1 | |
| Insured × non-married | 0.77 (0.47–1.26) | 0.304 |
| Any Medicaid × married | 1.02 (0.50–2.08) | 0.937 |
| Any Medicaid × non-married | 0.40 (0.24–0.69) | 0.001 |
| Uninsured × married | 0.62 (0.24–1.60) | 0.325 |
| Uninsured × non-married | 0.24 (0.11–0.53) | <0.001 |
| Age | 0.98 (0.96–0.99) | 0.005 |
| Gender | ||
| Male | 1 | |
| Female | 0.86 (0.57–1.30) | 0.491 |
| AJCC cT | ||
| T1 | 1 | |
| T2 | 1.19 (0.75–1.88) | 0.444 |
| T3 | 1.00 (0.64–1.57) | 0.979 |
| T4 | 2.81 (1.30–6.07) | 0.009 |
| AJCC cN | ||
| N0 | 1 | |
| N1 | 1.77 (1.13–2.79) | 0.012 |
| N2 | 2.58 (1.51–4.39) | <0.001 |
| N3 | 1.60 (0.88–2.89) | 0.120 |
| AJCC cM | ||
| M0 | 1 | |
| M1 | 0.17 (0.10–0.27) | <0.001 |
| WHO category | ||
| WHO I–II | 1 | |
| WHO III | 1.72 (1.15–2.56) | 0.007 |
| Race | ||
| Non black | 1 | |
| Black | 0.59 (0.35–0.99) | 0.046 |
| Variables | HR (95% CI) | p Value |
|---|---|---|
| Insurance × marital status | ||
| Insured × married | 1 | |
| Insured × non-married | 1.52 (1.12–2.06) | 0.007 |
| Any Medicaid × married | 1.41 (0.93–2.13) | 0.105 |
| Any Medicaid × non-married | 2.76 (2.03–3.76) | <0.001 |
| Uninsured × married | 1.27 (0.65–2.46) | 0.477 |
| Uninsured × non-married | 2.82 (1.74–4.58) | <0.001 |
| Age | 1.05 (1.04–1.06) | <0.001 |
| Gender | ||
| Male | 1 | |
| Female | 0.69 (0.52–0.90) | 0.007 |
| AJCC cT | ||
| T1 | 1 | |
| T2 | 1.10 (0.82–1.48) | 0.509 |
| T3 | 1.61 (1.21–2.14) | 0.001 |
| T4 | 1.88 (1.27–2.78) | 0.001 |
| AJCC cN | ||
| N0 | 1 | |
| N1 | 1.30 (0.96–1.77) | 0.090 |
| N2 | 1.61 (1.16–2.25) | 0.004 |
| N3 | 2.01 (1.39–2.89) | <0.001 |
| AJCC cM | ||
| M0 | 1 | |
| M1 | 2.98 (2.25–3.93) | <0.001 |
| Radiotherapy | ||
| Yes | 1 | |
| No | 2.31 (1.76–3.04) | <0.001 |
| WHO category | ||
| WHO I–II | 1 | |
| WHO III | 0.75 (0.59–0.96) | 0.023 |
| Race | ||
| Non black | 1 | |
| Black | 1.45 (1.05–2.00) | 0.022 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, C.-C.; Yang, C.-C.; Yeh, S.-A.; Huang, C.-I.; Hwang, T.-Z.; Yang, C.-C.; Su, Y.-C. The Impact of Insurance and Marital Status on Survival in Patients with Nasopharyngeal Carcinoma. Biology 2020, 9, 84. https://doi.org/10.3390/biology9040084
Wang C-C, Yang C-C, Yeh S-A, Huang C-I, Hwang T-Z, Yang C-C, Su Y-C. The Impact of Insurance and Marital Status on Survival in Patients with Nasopharyngeal Carcinoma. Biology. 2020; 9(4):84. https://doi.org/10.3390/biology9040084
Chicago/Turabian StyleWang, Chih-Chun, Ching-Chieh Yang, Shyh-An Yeh, Chung-I Huang, Tzer-Zen Hwang, Chuan-Chien Yang, and Yu-Chieh Su. 2020. "The Impact of Insurance and Marital Status on Survival in Patients with Nasopharyngeal Carcinoma" Biology 9, no. 4: 84. https://doi.org/10.3390/biology9040084
APA StyleWang, C.-C., Yang, C.-C., Yeh, S.-A., Huang, C.-I., Hwang, T.-Z., Yang, C.-C., & Su, Y.-C. (2020). The Impact of Insurance and Marital Status on Survival in Patients with Nasopharyngeal Carcinoma. Biology, 9(4), 84. https://doi.org/10.3390/biology9040084






