Cutaneous Manifestations in Confirmed COVID-19 Patients: A Systematic Review
Abstract
Simple Summary
Abstract
1. Introduction
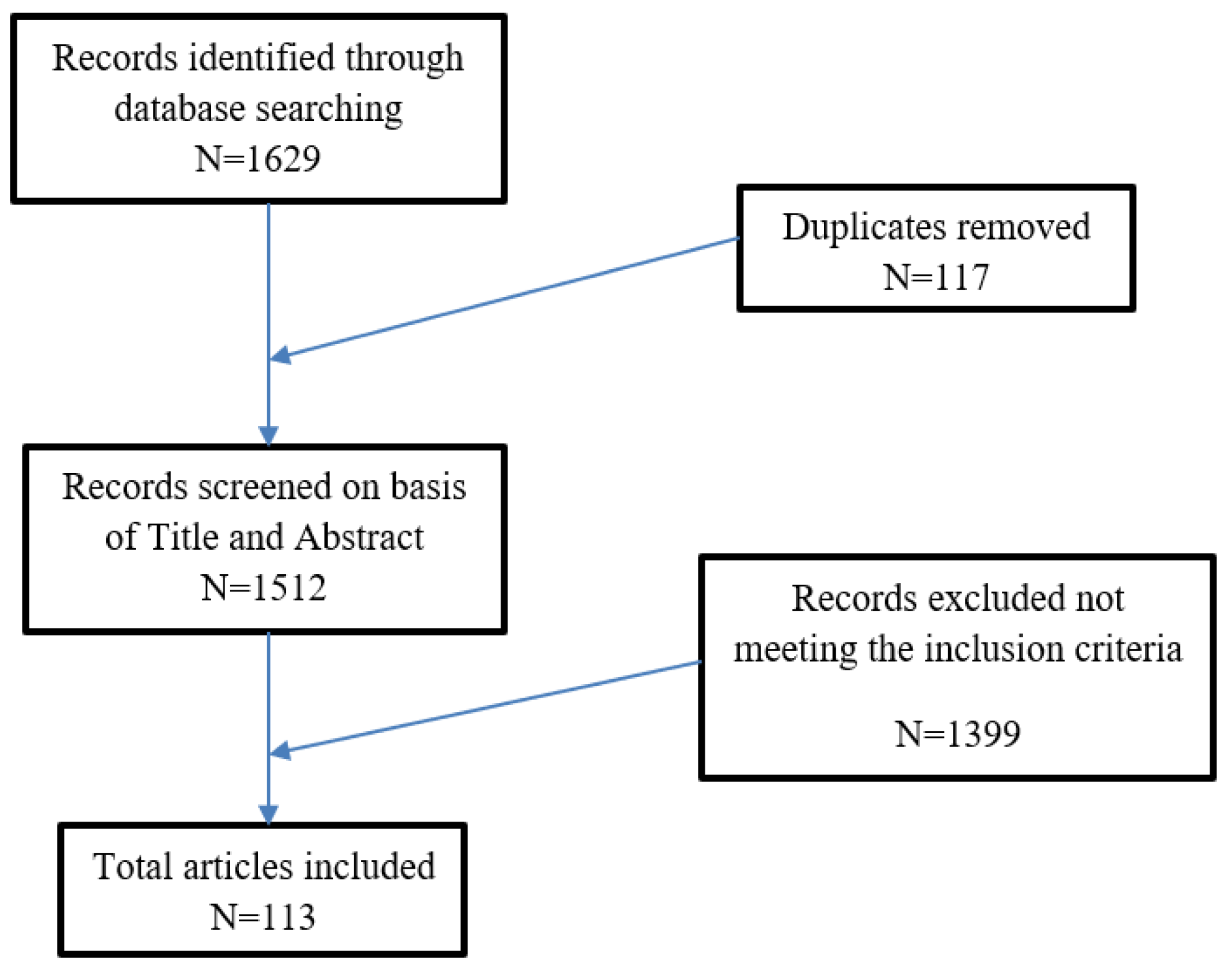
2. Materials and Methods
3. Results
3.1. Erythematous Maculopapular
3.2. Vascular Lesions
3.3. Vesicular Rash
3.4. Urticarial Rash
3.5. Erythema Multiforme/Generalized Pustular Figurate Erythema/Stevens-Johnson Syndrome
3.6. Ocular/Periocular Involvement
3.7. Atypical Cutaneous Manifestations
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus Update (Live): 41,298,621 Cases and 1,132,895 Deaths from COVID-19 Virus Pandemic—Worldometer. Available online: https://www.worldometers.info/coronavirus/#countries.%20Last%20accessed:%2019%20september%202020 (accessed on 19 September 2020).
- Yang, P.; Wang, X. COVID-19: A new challenge for human beings. Cell Mol. Immunol. 2020, 17, 555–557. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Estébanez, A.; Pérez-Santiago, L.; Silva, E.; Guillen-Climent, S.; García-Vázquez, A.; Ramón, M.D. Cutaneous manifestations in COVID-19: A new contribution. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e250–e251. [Google Scholar] [CrossRef] [PubMed]
- Daneshgaran, G.; Dubin, D.P.; Gould, D.J. Cutaneous Manifestations of COVID-19: An Evidence-Based Review. Am. J. Clin. Dermatol. 2020, 21, 627–639. [Google Scholar] [CrossRef]
- Oxford Centre for Evidence-Based Medicine 2011 Levels of Evidence. Available online: http://www.cebm.net/wp-content/uploads/2014/06/CEBM-Levels-of-Evidence-2.1.pdf (accessed on 19 September 2020).
- Rosell-Díaz, A.; Mateos-Mayo, A.; Nieto-Benito, L.; Balaguer-Franch, I.; De La Torre-Ruiz, E.H.; Lainez-Nuez, A.; Suárez-Fernández, R.; Bergón-Sendín, M. Exanthema and eosinophilia in COVID-19 patients: Has viral infection a role in drug induced exanthemas? J. Eur. Acad. Dermatol. Venereol. 2020, 34, 561. [Google Scholar] [CrossRef]
- Sachdeva, M.; Gianotti, R.; Shah, M.; Bradanini, L.; Tosi, D.; Veraldi, S.; Ziv, M.; Leshem, E.; Dodiuk-Gad, R.P. Cutaneous manifestations of COVID-19: Report of three cases and a review of literature. J. Dermatol. Sci. 2020, 98, 75–81. [Google Scholar] [CrossRef]
- Tamai, M.; Maekawa, A.; Goto, N.; Ge, L.; Nishida, T.; Iwahashi, H.; Yokomi, A. Three cases of COVID-19 patients presenting with erythema. J. Dermatol. 2020, 47, 1175–1178. [Google Scholar] [CrossRef]
- Mahé, A.; Birckel, E.; Krieger, S.; Merklen, C.; Bottlaender, L. A distinctive skin rash associated with coronavirus disease 2019? J. Eur. Acad. Dermatol. Venereol. 2020, 34, e246–e247. [Google Scholar] [CrossRef]
- Sanchez, A.; Sohier, P.; Benghanem, S.; L’Honneur, A.-S.; Rozenberg, F.; Dupin, N.; Garel, B. Digitate Papulosquamous Eruption Associated With Severe Acute Respiratory Syndrome Coronavirus 2 Infection. JAMA Dermatol. 2020, 156, 819. [Google Scholar] [CrossRef]
- Recalcati, S. Cutaneous manifestations in COVID-19: A first perspective. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e212–e213. [Google Scholar] [CrossRef] [PubMed]
- Bouaziz, J.; Duong, T.; Jachiet, M.; Velter, C.; Lestang, P.; Cassius, C.; Arsouze, A.; Trong, E.D.T.; Bagot, M.; Begon, E.; et al. Vascular skin symptoms in COVID-19: A French observational study. J. Eur. Acad. Dermatol. Venereol. 2020, 34. [Google Scholar] [CrossRef] [PubMed]
- Casas, C.G.; Català, A.; Hernández, G.C.; Rodríguez-Jiménez, P.; Fernandez-Nieto, D.; Lario, A.R.; Fernández, I.N.; Ruiz-Villaverde, R.; Falkenhain-López, D.; Llamas-Velasco, M.; et al. Classification of the cutaneous manifestations of COVID-19: A rapid prospective nationwide consensus study in Spain with 375 cases. Br. J. Dermatol. 2020, 183, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Hedou, M.; Carsuzaa, F.; Chary, E.; Hainaut, E.; Cazenave-Roblot, F.; Regnault, M.M. Comment on ‘Cutaneous manifestations in COVID-19: A first perspective’ by Recalcati S. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 299. [Google Scholar] [CrossRef] [PubMed]
- Rivera-Oyola, R.; Koschitzky, M.; Printy, R.; Liu, S.; Stanger, R.; Golant, A.K.; Lebwohl, M. Dermatologic findings in 2 patients with COVID-19. JAAD Case Rep. 2020, 6, 537–539. [Google Scholar] [CrossRef] [PubMed]
- Morey-Olivé, M.; Espiau, M.; Mercadal-Hally, M.; Lera-Carballo, E.; García-Patos, V. Cutaneous manifestations in the current pandemic of coronavirus infection disease (COVID 2019). An Pediatría 2020, 92, 374–375. [Google Scholar] [CrossRef]
- Annunziata, M.C.; Patrì, A.; Ruggiero, A.; Di Guida, A.; Menicanti, C.; Greco, V.; Fabbrocini, G. Cutaneous involvement during COVID-19 pandemic: An emerging sign of infection. J. Eur. Acad. Dermatol. Venereol. 2020. [Google Scholar] [CrossRef]
- Chaabane, I.; Loukil, M.; Amri, R.; Badri, I.; Baha, H.; Lajmi, M.; Bouzaidi, K.; Ghrairi, H. Cutaneous manifestations of COVID-19: Report of three cases. Arch. Dermatol. Res. 2020, 7, 1–4. [Google Scholar] [CrossRef]
- Dalal, A.; Jakhar, D.; Agarwal, V.; Beniwal, R. Dermatological findings in SARS-CoV -2 positive patients: An observational study from North India. Dermatol. Ther. 2020, 16, 13849. [Google Scholar] [CrossRef]
- Freeman, E.E.; McMahon, D.E.; Lipoff, J.B.; Rosenbach, M.; Kovarik, C.; Desai, S.R.; Harp, J.; Takeshita, J.; French, L.E.; Lim, H.W.; et al. The spectrum of COVID-19–associated dermatologic manifestations: An international registry of 716 patients from 31 countries. J. Am. Acad. Dermatol. 2020, 83, 1118–1129. [Google Scholar] [CrossRef]
- Gianotti, R.; Recalcati, S.; Fantini, F.; Riva, C.; Milani, M.; Dainese, E.; Boggio, F. Histopathological Study of a Broad Spectrum of Skin Dermatoses in Patients Affected or Highly Suspected of Infection by COVID-19 in the Northern Part of Italy: Analysis of the Many Faces of the Viral-Induced Skin Diseases in Previous and New Reported Cases. Am. J. Dermatopathol. 2020, 42, 564–570. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Muniz, C.; Puerta-Peña, M.; Falkenhain-López, D.; Arroyo-Andrés, J.; Agud-Dios, M.; Rodriguez-Peralto, J.; Ortiz-Romero, P.; Rivera-Díaz, R. The broad spectrum of dermatological manifestations in COVID-19: Clinical and histopathological features learned from a series of 34 cases. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 574. [Google Scholar] [CrossRef] [PubMed]
- Gianotti, R.; Veraldi, S.; Recalcati, S.; Cusini, M.; Ghislanzoni, M.; Boggio, F.; Fox, L. Cutaneous Clinico-Pathological Findings in three COVID-19-Positive Patients Observed in the Metropolitan Area of Milan, Italy. Acta Derm. Venereol. 2020, 100, adv00124–2. [Google Scholar] [CrossRef] [PubMed]
- Zengarini, C.; Orioni, G.; Cascavilla, A.; Solera, C.H.; Fulgaro, C.; Misciali, C.; Patrizi, A.; Gaspari, V. Histological pattern in COVID-19-induced viral rash. J. Eur. Acad. Dermatol. Venereol. 2020, 2. [Google Scholar] [CrossRef]
- Rossi, E.; Lasagni, C.; Trakatelli, M.; Rowan, S.W.; Magnoni, C. Acute maculopapular eruption in Covid-19 patient: A case report. Dermatol. Ther. 2020. [Google Scholar] [CrossRef]
- Gonçalves, C.S.; Carreira, N.R.; Passos, D.; Barbosa, A.L.; Baltazar, A.M.; Wahnon, A.; Abrantes, A.M.; Garrido, P.M.; Ferreira, T.; Silva, M.T.; et al. Erythematous Papular Rash: A Dermatological Feature of COVID-19. Eur J. Case Rep. Intern. Med. 2020, 7, 001768. [Google Scholar]
- Moreno, R.A.; Villa, L.E.; Villa, C.E.; Aparicio, M.M.; Fontanella, J.A. Cutaneous manifestation of COVID-19 in images: A case report. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 307. [Google Scholar] [CrossRef]
- Hunt, M.; Koziatek, C. A Case of COVID-19 Pneumonia in a Young Male with Full Body Rash as a Presenting Symptom. Clin. Pract. Cases Emerg. Med. 2020, 4, 219–221. [Google Scholar] [CrossRef][Green Version]
- Najarian, D.J. Morbilliform exanthem associated with COVID-19. JAAD Case Rep. 2020, 6, 493–494. [Google Scholar] [CrossRef]
- Rebollar, J.C.O. Cutaneous manifestations of COVID infection 19. About a case. Med. Clínica 2020, 155, 50. [Google Scholar] [CrossRef]
- Iancu, G.M.; Solomon, A.; Birlutiu, V. Viral exanthema as manifestation of SARS-CoV-2 infection. Medicine 2020, 99, e21810. [Google Scholar] [CrossRef] [PubMed]
- Macedo-Pérez, M.; Barragán-Estudillo, Z.F.; Castillo-Montufar, E.; Choi, S.J.; Fernández-Rueda, P.; Donis-Hernández, J.; Virgen-Cuevas, M.M.; López-Enriquez, C.C.; Martínez-Hernández, L.; Carballo-Zarate, A.A.; et al. Dermatological findings in COVID-19 patients: Mexican experience. Int. J. Dermatol. 2020, 59, 872–873. [Google Scholar] [CrossRef] [PubMed]
- Mizutani, Y.; Nagai, M.; Tsuzuku, A. Late-onset cutaneous manifestations in a patient with severe COVID-19 infection. J. Dermatol. 2020, 47, e347–e348. [Google Scholar] [CrossRef] [PubMed]
- Freeman, E.E.; McMahon, D.E.; Lipoff, J.B.; Rosenbach, M.; Kovarik, C.; Takeshita, J.; French, L.E.; Thiers, B.H.; Hruza, G.J.; Fox, L.P. Pernio-like skin lesions associated with COVID-19: A case series of 318 patients from 8 countries. J. Am. Acad. Dermatol. 2020, 83, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Abadías-Granado, I.; Palma-Ruiz, A.; Cerro, P.; Morales-Callaghan, A.; Gómez-Mateo, M.; Gilaberte, Y.; Schwartz, R.A. Generalized Pustular Figurate Erythema. First Report in Two COVID-19 Patients on Hydroxychloroquine. J. Eur. Acad. Dermatol. Venereol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Aghazadeh, N.; Homayouni, M.; Sartori-Valinotti, J.C. Oral vesicles and acral erythema: Report of a cutaneous manifestation of COVID-19. Int. J. Dermatol. 2020, 59, 1153–1154. [Google Scholar] [CrossRef]
- Ahouach, B.; Harent, S.; Ullmer, A.; Martres, P.; Bégon, E.; Blum, L.; Tess, O.; Bachmeyer, C. Cutaneous lesions in a patient with COVID-19: Are they related? Br. J. Dermatol. 2020, 183, 31. [Google Scholar] [CrossRef]
- Alramthan, A.; Aldaraji, W. Two cases of COVID-19 presenting with a clinical picture resembling chilblains: First report from the Middle East. Clin. Exp. Dermatol. 2020, 45, 746–748. [Google Scholar] [CrossRef]
- Amatore, F.; Macagno, N.; Mailhe, M.; Demarez, B.; Gaudy-Marqueste, C.; Grob, J.; Raoult, D.; Brouqui, P.; Richard, M. SARS-CoV-2 infection presenting as a febrile rash. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e304–e306. [Google Scholar] [CrossRef]
- Andina, D.; Noguera-Morel, L.; Bascuas-Arribas, M.; Gaitero-Tristán, J.; Alonso-Cadenas, J.A.; Escalada-Pellitero, S.; Hernández-Martín, Á.; De La Torre-Espi, M.; Colmenero, I.; Torrelo, A. Chilblains in children in the setting of COVID-19 pandemic. Pediatr. Dermatol. 2020, 37, 406–411. [Google Scholar] [CrossRef]
- Balestri, R.; Termine, S.; Rech, G.; Girardelli, C. Late onset of acral necrosis after SARS-CoV-2 infection resolution. J. Eur. Acad. Dermatol. Venereol. 2020, 26. [Google Scholar] [CrossRef]
- Bosch-Amate, X.; Giavedoni, P.; Podlipnik, S.; Andreu-Febrer, C.; Sanz-Beltran, J.; Herrera-García, A.; Alós, L.; Mascaró, J.M. Retiform purpura as a dermatological sign of coronavirus disease 2019 (COVID-19) coagulopathy. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e548–e549. [Google Scholar] [CrossRef] [PubMed]
- Conforti, C.; Zalaudek, I.; Giuffrida, R.; Zorat, F.; Grillo, A.; Colapietro, N.; Francica, M.; Di Meo, N. “ COVID-Mask”: An atypical livedoid manifestation of COVID -19 observed in a Northern Italy hospital. Dermatol. Ther. 2020, 33, e13701. [Google Scholar] [CrossRef] [PubMed]
- Davoodi, L.; Jafarpour, H.; Kazeminejad, A.; Soleymani, E.; Akbari, Z.; Razavi, A. Hydroxychloroquine-induced Stevens–Johnson syndrome in COVID-19: A rare case report. Oxf. Med. Case Rep. 2020, 2020. [Google Scholar] [CrossRef] [PubMed]
- De Masson, A.; Bouaziz, J.-D.; Sulimovic, L.; Bagot, M.; Duong, T.-A. Chilblains is a common cutaneous finding during the COVID-19 pandemic: A retrospective nationwide study from France. J. Am. Acad Dermatol. 2020, 83, 667–670. [Google Scholar] [CrossRef] [PubMed]
- De Medeiros, V.L.S.; Silva, L.F.T. Follow-up of skin lesions during the evolution of COVID-19: A case report. Arch. Dermatol. Res. 2020, 14, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Guimaraens, B.; Dominguez-Santas, M.; Suarez-Valle, A.; Pindado-Ortega, C.; Selda-Enriquez, G.; Bea-Ardebol, S.; Fernandez-Nieto, D. Petechial Skin Rash Associated With Severe Acute Respiratory Syndrome Coronavirus 2 Infection. JAMA Dermatol. 2020, 156, 820. [Google Scholar] [CrossRef]
- Dominguez-Santás, M.; Diaz-Guimaraens, B.; Abellas, P.G.; Del Real, C.M.; Burgos-Blasco, P.; Suárez-Valle, A. Cutaneous small-vessel vasculitis associated with novel 2019 coronavirus SARS-CoV-2 infection (COVID-19). J. Eur. Acad. Dermatol. Venereol. 2020, 34, e536–e537. [Google Scholar] [CrossRef]
- Droesch, C.; Do, M.H.; DeSancho, M.; Lee, E.-J.; Magro, C.; Harp, J. Livedoid and Purpuric Skin Eruptions Associated with Coagulopathy in Severe COVID-19. JAMA Dermatol. 2020, 156, 1022. [Google Scholar] [CrossRef]
- Elsaie, M.L.; Nada, H.A. Herpes zoster (shingles) complicating the course of COVID19 infection. J. Dermatol. Treat. 2020, 12, 1–3. [Google Scholar] [CrossRef]
- Elsaie, M.L.; Youssef, E.A.; Nada, H.A. Herpes zoster might be an indicator for latent COVID 19 infection. Dermatol. Ther. 2020, 33, e13666. [Google Scholar] [CrossRef] [PubMed]
- Falkenhain-López, D.; Sánchez-Velázquez, A.; López-Valle, A.; De Frutos, J.O. SARS-Coronavirus-2 and acute urticaria. Int. J. Dermatol. 2020, 59, 867–868. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Nieto, D.; Ortega-Quijano, D.; Jimenez-Cauhe, J.; Burgos-Blasco, P.; De Perosanz-Lobo, D.; Suarez-Valle, A.; Cortes-Cuevas, J.L.; Carretero, I.; Del Real, C.G.; Fernandez-Guarino, M. Clinical and histological characterization of vesicular COVID-19 rashes: A prospective study in a tertiary care hospital. Clin. Exp. Dermatol. 2020, 8. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Nieto, D.; Ortega-Quijano, D.; Segurado-Miravalles, G.; Pindado-Ortega, C.; Prieto-Barrios, M.; Jimenez-Cauhe, J. Comment on: Cutaneous manifestations in COVID-19: A first perspective. Safety concerns of clinical images and skin biopsies. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e252–e254. [Google Scholar] [CrossRef] [PubMed]
- Martínez, M.G.; Martínez-Doménech, Á.; Magdaleno-Tapial, J.; Valenzuela-Oñate, C.; Partarrieu-Mejías, F.; Lorca-Spröhnle, J.; Casanova-Esquembre, A.; Pérez-Ferriols, A.; Miquel, V.A. Acute acral cutaneous manifestations during the COVID-19 pandemic: A single-centre experience. J. Eur. Acad. Dermatol. Venereol. 2020, 26. [Google Scholar] [CrossRef]
- Genovese, G.; Colonna, C.; Marzano, A.V. Varicella-like exanthem associated with COVID-19 in an 8-year-old girl: A diagnostic clue? Pediatr. Dermatol. 2020, 37, 435–436. [Google Scholar] [CrossRef]
- Gunawan, C.; Angela, A.; Widysanto, A. Urticarial eruption in coronavirus disease 2019 infection: A case report in Tangerang, Indonesia. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e372–e373. [Google Scholar] [CrossRef]
- Hassan, K. Urticaria and angioedema as a prodromal cutaneous manifestation of SARS-CoV-2 (COVID-19) infection. BMJ Case Rep. 2020, 13. [Google Scholar] [CrossRef]
- Henry, D.; Ackerman, M.; Sancelme, E.; Finon, A.; Esteve, E. Urticarial eruption in COVID-19 infection. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e244–e245. [Google Scholar] [CrossRef]
- Jmenez-Cauhe, J.; Ortega-Quijano, D.; Prieto-Barrios, M.; Moreno-Arrones, O.M.; Fernandez-Nieto, D. Reply to “COVID-19 can present with a rash and be mistaken for dengue”: Petechial rash in a patient with COVID-19 infection. J. Am. Acad. Dermatol. 2020, 83, e141–e142. [Google Scholar] [CrossRef]
- Jimenez-Cauhe, J.; Ortega-Quijano, D.; Carretero-Barrio, I.; Suarez-Valle, A.; Saceda-Corralo, D.; Del Real, C.M.; Fernandez-Nieto, D. Erythema multiforme-like eruption in patients with COVID-19 infection: Clinical and histological findings. Clin. Exp. Dermatol. 2020, 45, 892–895. [Google Scholar] [CrossRef] [PubMed]
- Jones, V.G.; Mills, M.; Suarez, D.; Hogan, C.A.; Yeh, D.; Segal, J.B.; Nguyen, E.L.; Barsh, G.R.; Maskatia, S.; Mathew, R. COVID-19 and Kawasaki Disease: Novel Virus and Novel Case. Hosp. Pediatr. 2020, 10, 537–540. [Google Scholar] [CrossRef] [PubMed]
- Joob, B.; Wiwanitkit, V. COVID-19 can present with a rash and be mistaken for dengue. J. Am. Acad. Dermatol. 2020, 82, e177. [Google Scholar] [CrossRef] [PubMed]
- Kalner, S.; Vergilis, I.J. Periorbital erythema as a presenting sign of COVID-19. JAAD Case Rep. 2020, 6, 996–998. [Google Scholar] [CrossRef] [PubMed]
- Klimach, A.; Evans, J.; Stevens, J.; Creasey, N. Rash as a presenting complaint in a child with COVID-19. Pediatr. Dermatol. 2020, 37, 966–967. [Google Scholar] [CrossRef] [PubMed]
- Kolivras, A.; Dehavay, F.; Delplace, D.; Feoli, F.; Meiers, I.; Milone, L.; Olemans, C.; Sass, U.; Theunis, A.; Thompson, C.T.; et al. Coronavirus (COVID-19) infection–induced chilblains: A case report with histopathologic findings. JAAD Case Rep. 2020, 6, 489–492. [Google Scholar] [CrossRef]
- Landa, N.; Mendieta-Eckert, M.; Fonda-Pascual, P.; Aguirre, T. Chilblain-like lesions on feet and hands during the COVID-19 Pandemic. Int. J. Dermatol. 2020, 59, 739–743. [Google Scholar] [CrossRef]
- Llamas-Velasco, M.; Rodríguez-Jiménez, P.; Chicharro, P.; De Argila, D.; Muñoz-Hernández, P.; Daudén, E. Reply to “Varicella-like exanthem as a specific COVID-19-associated skin manifestation: Multicenter case series of 22 patients”: To consider varicella-like exanthem associated with COVID-19, virus varicella zoster and virus herpes simplex must be ruled out. J. Am. Acad. Dermatol. 2020, 83, e253–e254. [Google Scholar] [CrossRef]
- Locatelli, A.; Test, E.R.; Vezzoli, P.; Carugno, A.; Moggio, E.; Consonni, L.; Gianatti, A.; Sena, P. Histologic features of long-lasting chilblain-like lesions in a paediatric COVID-19 patient. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 365. [Google Scholar] [CrossRef]
- Magro, C.; Mulvey, J.J.; Berlin, D.; Nuovo, G.; Salvatore, S.; Harp, J.; Baxter-Stoltzfus, A.; Laurence, J.C. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl. Res. 2020, 220, 1–13. [Google Scholar] [CrossRef]
- Manalo, I.F.; Smith, M.K.; Cheeley, J.; Jacobs, R. A dermatologic manifestation of COVID-19: Transient livedo reticularis. J. Am. Acad. Dermatol. 2020, 83, 700. [Google Scholar] [CrossRef] [PubMed]
- Marzano, A.V.; Genovese, G.; Fabbrocini, G.; Pigatto, P.; Monfrecola, G.; Piraccini, B.M.; Veraldi, S.; Rubegni, P.; Cusini, M.; Caputo, V.; et al. Varicella-like exanthem as a specific COVID-19–associated skin manifestation: Multicenter case series of 22 patients. J. Am. Acad. Dermatol. 2020, 83, 280–285. [Google Scholar] [CrossRef]
- Navaeifar, M.R.; Ghazaghi, M.P.; Shahbaznejad, L.; Rouhanizadeh, H.; Abutalebi, M.; Varandi, M.R.; Rezai, M.S. Fever with Rash is One of the First Presentations of COVID-19 in Children: A Case Report. Int. Med. Case Rep. J. 2020, 13, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Olisova, O.Y.; Anpilogova, E.M.; Shnakhova, L.M. Cutaneous manifestations in COVID-19: A skin rash in a child. Dermatol. Ther. 2020. [Google Scholar] [CrossRef] [PubMed]
- Ordieres-Ortega, L.; Toledo-Samaniego, N.; Parra-Virto, A.; Fernández-Carracedo, E.; Lavilla-Olleros, C.; Demelo-Rodríguez, P. Atypical erythema nodosum in a patient with COVID-19 pneumonia. Dermatol. Ther. 2020, 33, e13658. [Google Scholar] [CrossRef]
- Patel, N.; Kho, J.; Smith, K.E.; Ahmed, A.; Abbeele, K.V.D.; Mandal, A.K.; Missouris, C.G. Polymorphic cutaneous manifestations of COVID-19 infection in a single viral host. Int. J. Dermatol. 2020, 59, 1149–1150. [Google Scholar] [CrossRef]
- Piccolo, V.; Neri, I.; Filippeschi, C.; Oranges, T.; Argenziano, G.; Battarra, V.C.; Berti, S.; Manunza, F.; Fortina, A.B.; Di Lernia, V.; et al. Chilblain-like lesions during COVID-19 epidemic: A preliminary study on 63 patients. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e291–e293. [Google Scholar] [CrossRef]
- Wu, P.; Duan, F.; Luo, C.; Liu, Q.; Qu, X.; Liang, L.; Wu, K. Characteristics of Ocular Findings of Patients With Coronavirus Disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020, 138, 575–578. [Google Scholar] [CrossRef]
- Wu, P.; Liang, L.; Chen, C.; Nie, S. A child confirmed COVID-19 with only symptoms of conjunctivitis and eyelid dermatitis. Graefe Arch. Clin. Exp. Ophthalmol. 2020, 258, 1565–1566. [Google Scholar] [CrossRef]
- Quintana-Castanedo, L.; Feito-Rodríguez, M.; Valero-López, I.; Chiloeches-Fernández, C.; Sendagorta-Cudós, E.; Herranz-Pinto, P. Urticarial exanthem as early diagnostic clue for COVID-19 infection. JAAD Case Rep. 2020, 6, 498–499. [Google Scholar] [CrossRef]
- Riphagen, S.; Gomez, X.; Gonzalez-Martinez, C.; Wilkinson, N.; Theocharis, P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 2020, 395, 1607–1608. [Google Scholar] [CrossRef]
- Test, E.R.; Vezzoli, P.; Carugno, A.; Raponi, F.; Gianatti, A.; Rongioletti, F.; Sena, P. Acute generalized exanthematous pustulosis with erythema multiforme-like lesions induced by Hydroxychloroquine in a woman with coronavirus disease 2019 (COVID-19). J. Eur. Acad. Dermatol. Venereol. 2020, 34. [Google Scholar] [CrossRef]
- Rotman, J.A.; Dean, K.E.; Magro, C.M.; Nuovo, G.; Bartolotta, R.J. Concomitant calciphylaxis and COVID-19 associated thrombotic retiform purpura. Skelet. Radiol. 2020, 49, 1879–1884. [Google Scholar] [CrossRef] [PubMed]
- Sakaida, T.; Tanimoto, I.; Matsubara, A.; Nakamura, M.; Morita, A. Unique skin manifestations of COVID-19: Is drug eruption specific to COVID-19? J. Dermatol. Sci. 2020, 99, 62–64. [Google Scholar] [CrossRef]
- Shors, A.R. Herpes zoster and severe acute herpetic neuralgia as a complication of COVID-19 infection. JAAD Case Rep. 2020, 6, 656–657. [Google Scholar] [CrossRef]
- Do, N.S.; Bridwell, R.E.; Do, J.R. Erythema nodosum-like rash in a COVID-19 patient: A case report. Am. J. Emerg. Med. 2020. [Google Scholar] [CrossRef]
- Skroza, N.; Bernardini, N.; Balduzzi, V.; Mambrin, A.; Marchesiello, A.; Michelini, S.; Tolino, E.; Proietti, I.; Di Cristofano, C.; Petrozza, V.; et al. A late-onset widespread skin rash in a previous COVID-19-infected patient: Viral or multidrug effect? J. Eur. Acad. Dermatol. Venereol. 2020, 34. [Google Scholar] [CrossRef]
- Spencer, R.; Closson, R.C.; Gorelik, M.; Boneparth, A.D.; Hough, R.F.; Acker, K.P.; Krishnan, U. COVID-19 Inflammatory Syndrome with Clinical Features Resembling Kawasaki Disease. Pediatrics 2020, 146, e20201845. [Google Scholar] [CrossRef]
- Suarez-Valle, A.; Fernandez-Nieto, D.; Diaz-Guimaraens, B.; Dominguez-Santas, M.; Carretero, I.; Garcia, B.P. Acro-ischaemia in hospitalized COVID-19 patients. J. Eur. Acad. Dermatol. Venereol. 2020, 34. [Google Scholar] [CrossRef]
- Suter, P.; Mooser, B.; Thien, H.P.P.H. Erythema nodosum as a cutaneous manifestation of COVID-19 infection. BMJ Case Rep. 2020, 13, e236613. [Google Scholar] [CrossRef]
- Tahir, A.; Sohail, Z.; Nasim, B.; Parmar, N. Widespread cutaneous small vessel vasculitis secondary to COVID-19 infection. Int. J. Dermatol. 2020, 59, 1278–1279. [Google Scholar] [CrossRef] [PubMed]
- Tammaro, A.; Adebanjo, G.A.R.; Parisella, F.; Pezzuto, A.; Rello, J. Cutaneous manifestations in COVID-19: The experiences of Barcelona and Rome. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e306–e307. [Google Scholar] [CrossRef]
- Taşkın, B.; Vural, S.; Altuğ, E.; Demirkesen, C.; Kocatürk, E.; Çelebi, I.; Ferhanoğlu, B.; Alper, S. Coronavirus 19 presenting with atypical Sweet’s syndrome. J. Eur. Acad. Dermatol. Venereol. 2020, 26. [Google Scholar] [CrossRef] [PubMed]
- Van Damme, C.; Berlingin, E.; Saussez, S.; Accaputo, O. Acute urticaria with pyrexia as the first manifestations of a COVID-19 infection. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e300–e301. [Google Scholar] [CrossRef] [PubMed]
- Verheyden, M.; Grosber, M.; Gutermuth, J.; Velkeniers, B. Relapsing symmetric livedo reticularis in a patient with COVID-19 infection. J. Eur. Acad. Dermatol. Venereol. 2020, 25. [Google Scholar] [CrossRef]
- Wolfe, D.M.; Nassar, G.N.; Divya, K.; Krilov, L.R.; Noor, A. Young Children Presenting with Fever and Rash in the Midst of SARS-CoV-2 Outbreak in New York. Clin. Pediatr. 2020, 59, 1112–1118. [Google Scholar] [CrossRef] [PubMed]
- Young, S.; Fernandez, A.P. Skin manifestations of COVID-19. Clevel. Clin. J. Med. 2020, 14. [Google Scholar] [CrossRef]
- Zhang, Y.; Cao, W.; Xiao, M.; Li, Y.J.; Yang, Y.; Zhao, J.; Zhou, X.; Jiang, W.; Zhao, Y.Q.; Zhang, S.Y.; et al. Clinical and coagulation characteristics of 7 patients with critical COVID-2019 pneumonia and acro-ischemia. Zhonghua Xue Ye Xue Za Zhi 2020, 41, E006. [Google Scholar] [CrossRef] [PubMed]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Panigada, M.; Bottino, N.; Tagliabue, P.; Grasselli, G.; Novembrino, C.; Chantarangkul, V.; Pesenti, A.; Peyvandi, F.; Tripodi, A. Hypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis. J. Thromb. Haemost. 2020, 18, 1738–1742. [Google Scholar] [CrossRef]
- Tang, N.; Bai, H.; Chen, X.; Gong, J.; Li, D.; Sun, Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J. Thromb. Haemost. 2020, 18, 1094–1099. [Google Scholar] [CrossRef]
- Zhai, Z.; Li, C.; Chen, Y.; Gerotziafas, G.; Zhang, Z.; Wan, J.; Liu, P.; Elalamy, I.; Wang, C. Prevention and Treatment of Venous Thromboembolism Associated with Coronavirus Disease 2019 Infection: A Consensus Statement before Guidelines. Thromb. Haemost. 2020, 120, 937–948. [Google Scholar] [CrossRef]
- Molina-Ruiz, A.M.; Santonja, C.; Rütten, A.; Cerroni, L.; Kutzner, H.; Requena, L. Immunohistochemistry in the Diagnosis of Cutaneous Viral Infections—Part I. Cutaneous Viral Infections by Herpesviruses and Papillomaviruses. Am. J. Dermatopathol. 2015, 37, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Muehlenbachs, A.; Bhatnagar, J.; Zaki, S.R. Tissue tropism, pathology and pathogenesis of enterovirus infection. J. Pathol. 2014, 235, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Szatkowski, J.; Schwartz, R.A. Acute generalized exanthematous pustulosis (AGEP): A review and update. J. Am. Acad. Dermatol. 2015, 73, 843–848. [Google Scholar] [CrossRef]
- Schwartz, R.A.; Janniger, C.K. Generalized pustular figurate erythema: A newly delineated severe cutaneous drug reaction linked with hydroxychloroquine. Dermatol. Ther. 2020, 33, e13380. [Google Scholar] [CrossRef]
- Lin, J.-H.; Sheu, H.-M.; Lee, J.Y.-Y. Acute generalized exanthematous pustulosis with erythema multiforme-like lesions. Eur. J. Dermatol. 2002, 12, 475–478. [Google Scholar]
- Kostopoulos, T.; Krishna, S.; Brinster, N.; Ortega-Loayza, A. Acute generalized exanthematous pustulosis: Atypical presentations and outcomes. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 209–214. [Google Scholar] [CrossRef]
- Sidoroff, A.; Dunant, A.; Viboud, C.; Halevy, S.; Bavinck, J.B.; Naldi, L.; Mockenhaupt, M.; Fagot, J.-P.; Roujeau, J.-C. Risk factors for acute generalized exanthematous pustulosis (AGEP)—Results of a multinational case–control study (EuroSCAR). Br. J. Dermatol. 2007, 157, 989–996. [Google Scholar] [CrossRef]
- Sharma, A.N.; Mesinkovska, N.A.; Paravar, T. Characterizing the adverse dermatologic effects of hydroxychloroquine: A systematic review. J. Am. Acad. Dermatol. 2020, 83, 563–578. [Google Scholar] [CrossRef]
- Clinical Protocols for the Diagnosis and Treatment of COVID-19. Available online: https://www.chinadaily.com.cn/pdf/2020/1.Clinical.Protocols.for.the.Diagnosis.and.Treatment.of.COVID-19.V7.pdf (accessed on 19 September 2020).
- Krajewski, P.K.; Szepietowski, J.C.; Maj, J. Cutaneous hyperesthesia: A novel manifestation of COVID-19. Brain Behav. Immun. 2020, 87, 188. [Google Scholar] [CrossRef] [PubMed]
- Marasca, C.; Ruggiero, A.; Fontanella, G.; Ferrillo, M.; Fabbrocini, G.; Villani, A. Telemedicine and support groups could be used to improve adherence to treatment and health-related quality of life in patients affected by inflammatory skin conditions during the COVID-19 pandemic. Clin. Exp. Dermatol. 2020, 45, 749. [Google Scholar] [CrossRef] [PubMed]
| References | Level of Evidence | Country | Total Number of RT-PCR Confirmed Cases | RT-PCR Confirmed Cases with Cutaneous Involvement | Age (Years) And Sex (M/F) | Rash Type | Rash Location | Fever | Relation to Onset of COVID Symptoms | Relation to Medication |
|---|---|---|---|---|---|---|---|---|---|---|
| Abadias et al. [37] | 4 | Spain | 2 | 2 | M 64 F 60 | GPFE | trunk, limbs, scalp, axillae | - | - | 2 and 3 weeks after hydroxychloroquine, lopinavir/ritonavir; teicoplanin, azithromycin |
| Aghazadeh et al. [38] | 5 | Iran | 1 | 1 | F 9 | polymorphic pattern: Vesicular oral eruption, and acral erythematous papules and plaques | oral; acral | yes | - | acetaminophen |
| Ahouach et al. [39] | 5 | France | 1 | 1 | F 57 | urticaria | trunk, limbs | yes | 2 days after | acetaminophen |
| Alramthan et al. [40] | 4 | Qattar | 2 | 2 | F 27, 35 | chilblain-like | hands | - | - | - |
| Amatore et al. [41] | 5 | France | 1 | 1 | M 39 | urticaria (annular) | upper limbs, chest, neck, abdomen | yes | concomitant | - |
| Andina et al. [42] | 5 | Spain | 1 | 1 | - | chilblain-like | acral | - | - | - |
| Annunziata et al. [19] | 4 | Italy | 4 | 4 | F 66 F 60 M 30 M 30 | - macular - vesicular - vesicular - urticarial | - trunk - abdomen - trunk - legs | yes yes yes yes | 2–10 days after | - |
| Avellana et al. [29] | 5 | Spain | 1 | 1 | F 32 | maculopapular | generalized | yes | 6 days after | after acetaminophen |
| Balestri et al. [43] | 5 | Italy | 1 | 1 | F 74 | chilblain-like with digital infarcts and ischemic necrosis of the left third fingertip | acral | - | - | - |
| Bosch-Amate et al. [44] | 5 | Spain | 1 | 1 | F 79 | retiform purpura | knee area | yes | - | - |
| Bouaziz et al. [14] | 4 | France | 14 | 14 | - | four macular erythema, two vesicular, one cold urticaria, seven vascular | - | - | a few days after | - |
| Chaabane et al. [20] | 4 | Tunisia | 3 | 3 | F 20 F 35 F 36 | - erythema multiforme pattern - polymorphic pattern: Rash on upper chest and livedo reticularis on arm - maculopapular | - trunk, upper limbs, thighs -upper chest and arm - sub-mammary fold and trunk | yes no yes | 3–4 days after | - |
| Conforti et al. [45] | 5 | Italy | 1 | 1 | F 62 | transient livedo reticularis of the back, abdomen, and face; periorbital livedoid maculae | back, abdomen, and face | yes | 14 days after | - |
| Dalal et al. [21] | 4 | India | 102 | 13 | Mean 39 | three maculopapular, two urticaria, eight generalized pruritus | trunk and extremities | yes | 2–3 days after | - |
| Davoodi et al. [46] | 5 | Iran | 1 | 1 | F 42 | Stevens-Johnson syndrome with positive Nikolsky sign | generalized, orolabial and genital | yes | - | 2 days after hydroxychloroquine, acetaminophen; then it was changed to lopinavir/ritonavir |
| de Masson et al. [47] | 4 | France | 25 | 7 | - | chilblain-like | acral | - | - | - |
| de Medeiros et al. [48] | 5 | Brazil | 1 | 1 | F 55 | urticaria with palmar erythema | shoulders, inguinal region, palms | yes | concomitant | - |
| Diaz-Guimaraens et al. [49] | 5 | Spain | 1 | 1 | M 48 | petechial | buttocks, popliteal fossae, proximal anterior thighs, and lower abdomen | yes | few days after | no |
| Dominguez-Santas et al. [50] | 5 | Spain | 1 | 1 | F 71 | petechial | both legs, extending from the ankle and up to the thigh | yes | 7 days after | no |
| Droesch et al. [51] | 4 | USA | 4 | 4 | - | three livedo racemosa one retiform purpura | hands and forearms | - | 19–23 days after | - |
| Elsaie et al. [52] | 5 | Egypt | 1 | 1 | M 44 | herpes zoster | upper chest and back | - | 7 days after | - |
| Elsaie et al. [53] | 5 | Egypt | 2 | 2 | M 68 F 60 | herpes zoster | - right thigh - chest and neck | yes no | - 2 days before - concomitant | - |
| Estebanez et al. [5] | 5 | Spain | 1 | 1 | F 28 | maculopapular | heels | - | - | 10 days after acetaminophen |
| Falkenhain-López et al. [54] | 5 | Spain | 1 | 1 | F 51 | urticaria | trunk, thighs, upper limbs, face, dorsal aspects of hands | - | concomitant | no medication |
| Fernandez-Nieto et al. [55] | 4 | Spain | 24 | 24 | Median 45 | vesicular | trunk, limbs, head, palms, soles | - | 2 before, 3 concomitant, 19 after | In seven patients after hydroxychloroquine, lopinavir/ritonavir; azithromycin |
| Fernandez-Nieto et al. [56] | 5 | Italy | 1 | 1 | F 32 | urticaria | lower trunk, thighs | - | 6 days after | 4 days after hydroxychloroquine and azithromycin |
| Freeman et al. [22] | 4 | 31 countries | 135 | 135 | Median 45 | 32 morbiliform, 19 macular erythema, 14 papulo-squamous, 16 vesicular, 23 urticarial, 16 pernio, 10 retiform purpura, 5 polymorphic | - | - | - | - |
| Freeman et al. [36] | 4 | 8 countries | 14 | 14 | Median 25 | chilblain-like | acral | - | - | - |
| Galvan et al. [15] | 4 | Spain | 375 | 234 | - | 29 chilblain-like, 17 vesicular, 49 urticarial, 122 maculopapular, 17 livedo/necrosis | - | - | 22 before; 212 at the same time; 139 after | - |
| García-Legaz et al. [57] | 4 | Spain | 2 | 2 | - | chilblain-like papulosquamous | - | - | after | - |
| Genovese et al. [58] | 5 | Italy | 1 | 1 | F 8 | vesicular | trunk | no | 6 days after | - |
| Gianotti et al. [25] | 4 | Italy | 3 | 3 | F 59 F 89 M 57 | maculopapular | - arms, trunk, and lower limbs - trunk and arms - generalized | yes yes yes | 7 days after 2 days before | 3 days after lopinavir-ritonavir, heparin and levofloxacin |
| Gianotti et al. [23] | 4 | Italy | 8 | 8 | - | four maculopapular, two vesicular, one of which presented with Grover disease-like pattern, two livedoid | - | - | - | - |
| Goncalves et al. [28] | 5 | Portugal | 1 | 1 | M 57 | maculopapular | elbows and abdomen | yes | 2 days after | - |
| Gunawan et al. [59] | 5 | Indonesia | 1 | 1 | M 51 | urticaria | face | yes | 5 days after | 3 days after azithromycin, hydroxychloroquine, cefoperazone-sulbactam, omeprazole |
| Hassan et al. [60] | 5 | Scothland | 1 | 1 | F 46 | urticaria with angioedema of the lips and hands | generalized; lips and face | no | 2 days before | - |
| Hedou et al. [16] | 4 | France | 103 | 5 | Mean 47 | 2 macular erythema, 2 urticaria, 1 vesicular (HSV-1) | - | - | 4 concomitant 1 (urticaria) before | - |
| Henry et al. [61] | 5 | France | 1 | 1 | F 27 | urticaria | generalized | no | a few days before | - |
| Hunt et al. [30] | 5 | USA | 1 | 1 | M 20 | maculopapular | generalized | yes | concomitant | - |
| Iancu et al. [33] | 5 | Romania | 1 | 1 | F 41 | maculopapular | generalized | yes | 17 days after | 15 days after hydroxychloroquine, azithromycin, lopinavir/ritonavir |
| Jimenez-Cauhe et al. [62] | 5 | Spain | 1 | 1 | elderly M | purpuric | axilary | - | - | hydroxychloroquine, lopinavir/ritonavir |
| Jimenez-Cauhe et al. [63] | 4 | Spain | 4 | 4 | Mean 66 | erythema multiforme pattern; enanthema | trunk, face, limbs; oral mucosa | - | 16–24 days after | 10-16 days after hydroxychloroquine; lopinavir/ ritonavir; azithromycin; |
| Jones et al. [64] | 5 | USA | 1 | 1 | F 6 months | Kawasaki disease | - | yes | 1 day after | - |
| Joob et al. [65] | 5 | Thailand | 1 | 1 | - | petechial | - | yes | few days before | no |
| Kalner et al. [66] | 4 | USA | 2 | 2 | F 43 M 50 | eyelid dermatitis | ocular | yes | 2 days before | - |
| Klimach et al. [67] | 5 | UK | 1 | 1 | M 13 | polymorphic pattern: Maculopapular, chilblain-like | axillary, plantar aspects of his feet | yes | - | after acetaminophen |
| Kolivras et al. [68] | 5 | Belgium | 1 | 1 | M 23 | chilblain-like | acral | yes | 3 days after | - |
| Landa et al. [69] | 4 | Spain | 2 | 2 | M 91 F 24 | chilblain-like | acral | - | - | - |
| Llamas-Velasco et al. [70] | 4 | Spain | 3 | 3 | F 59 M 69 M 79 | vesicular | trunk, perioral | yes | 21–43 days after | - |
| Locatelli et al. [71] | 5 | Italy | 1 | 1 | M 16 | chilblain-like | acral | - | 3 days after | - |
| Macedo-Pérez et al. [34] | 4 | Mexico | 1 | 1 | M 33 M 36 | macular erythema | trunk and limbs | yes yes | 7 days after 3 days after | - - |
| Magro et al. [72] | 4 | USA | 3 | 3 | M 32 F 66 F 40 | - retiform purpura - dusky purpuric patches - livedo racemosa | - buttocks - palms and soles - chest, legs and arms | yes yes yes | after | - hydroxychloroquine, azithromycin and remdesivir - hydroxychloroquine, enoxaparin - |
| Mahe et al. [11] | 5 | Italy | 1 | 1 | F 64 | macular erythema | antecubital fossae, extended to the trunk and axillary folds | yes | 4 days after | 4 days after acetaminophen |
| Manalo et al. [73] | 4 | USA | - | 2 | M 67 F 47 | unilateral livedo reticularis | - | - | after | - |
| Marzano et al. [74] | 4 | Italy | 22 | 22 | Mean 60 | vesicular | trunk, limbs | yes | 0–12 days after | - |
| Mizutani et al. [35] | 5 | Japan | 1 | 1 | M 69 | macular erythema | abdomen and upper thighs | - | - | after 38 days of favipiravir, ampicillin, sulbactam, and ceftriaxone |
| Morey-Olivé et al. [18] | 4 | Spain | 2 | 2 | M 6 y F 2 months | - maculopapular - urticaria | - generalized, including palms - generalized, with sparing of palms and soles | yes yes | - 2 days after - 4 days before | - |
| Najarian et al. [31] | 5 | USA | 1 | 1 | M 58 | maculopapular | generalized | yes | 1 day after | - |
| Navaeifar et al. [75] | 5 | Iran | 1 | 1 | M 1 | erythema multiforme pattern | generalized | yes | 1 day after | - |
| Olisova et al. [76] | 5 | Russia | 1 | 1 | F 12 | polymorphic pattern: Macular erythema with purpuric areas; strawberry tongue | upper eyelids, above the eyebrows, and in temporal region; tongue | yes | 3 days after | after paracetamol |
| Ordieres-Ortega et al. [77] | 5 | Spain | 1 | 1 | F 57 | atypical erythema nodosum | right leg | yes | - | 8 days after hydroxychloroquine, lopinavir/ritonavir |
| Patel et al. [78] | 5 | UK | 1 | 1 | F 78 | purpuric | back | yes | 7 days before | - |
| Piccolo et al. [79] | 4 | Italy | 2 | 2 | 12–16 | chilblain-like | acral | - | - | - |
| Ping et al. [80] | 4 | China | 28 | 11 | - | conjunctivitis | ocular | - | - | - |
| Ping et al. [81] | 5 | China | 1 | 1 | 2 y and 10 m | eyelid dermatitis and conjunctivitis | ocular | - | after | - |
| Quintana-Castanedo et al. [82] | 5 | Spain | 1 | 1 | M 61 | urticaria | thighs, arms, forearms | yes | before | - |
| Recalati S et al. [13] | 4 | Italy | 88 | 18 | - | 14 macular erythema; three urticarial; one vesicular | - | 8 concomitant; 10 after | - | |
| Riphagen et al. [83] | 4 | UK | 2 | 2 | M 14 M 6 | Kawasaki Disease | - | yes yes | - | - |
| Rivera-Oyola et al. [17] | 4 | USA | 2 | 2 | M 60 F 60 | - maculopapular - urticaria | generalized | yes yes | 3 to 9 days after | - |
| Robustelli et al. [84] | 5 | Italy | 1 | 1 | F 70 | atypical AGEP/ GPFE | generalized | - | - | 3 days after treatment withdrawal; 13 days after treatment inception hydroxychloroquine, lopinavir/ritonavir |
| Rosell-Díaz et al. [8] | 4 | Spain | 12 | 12 | Mean 66 | five maculopapular; seven erythema multiforme pattern | generalized | 3/12 | - | 10-28 days after hydroxychloroquine, lopinavir/ritonavir |
| Rossi et al. [27] | 5 | Italy | 1 | 1 | M 34 | maculopapular | generalized with sparing of palms and soles | yes | 5 days after | a few days after acetaminophen |
| Rotman et al. [85] | 5 | USA | 1 | 1 | F 62 | retiform purpura and calciphylaxis | bilateral lower extremities | - | 21 days after | - |
| Rubio-Muniz et al. [24] | 4 | Spain | 17 | 16 | - | six maculopapular, two chilblain, four erythema multiforme pattern, two palpable purpura, two urticaria | - | - | - | - |
| Sachdeva et al. [9] | 4 | Italy | 3 | 3 | F 71 F 77 F 72 | - maculopapular (Grover disease- like) - maculopapular with purpuric areas - vesicular | sub-mammary folds, trunk and hips | yes yes yes | - 4 days after | - a few days after - 1 day after lopinavir/ritonavir, hydroxychloroquine, ceftriaxone |
| Sakaida et al. [86] | 5 | Japan | 1 | 1 | F 52 | erythema multiforme pattern; | trunk and limbs | yes | 7 days before | 3 days after cefcapene and loxoprofen |
| Sanchez et al. [12] | 5 | France | 1 | 1 | elderly M | pityriasis rosea-like | abdomen, trunk, thighs | yes | 8 days after | after cefpodoxime |
| Shors et al. [87] | 5 | USA | 1 | 1 | F 49 | herpes zoster | face | yes | 7 days after | - |
| Sipfle et al. [88] | 5 | USA | 1 | 1 | F 54 | atypical erythema nodosum | lower back, upper extremities, and face | - | - | - |
| Skorza et al. [89] | 5 | Italy | 1 | 1 | 47 | urticaria vasculitis | trunk | - | - | a few days after ceftriaxon, lopinavir/ ritonavir, hidroxicloroquine, enoxaparin |
| Spencer et al. [90] | 4 | USA | 2 | 2 | M 11 F 7 | Kawasaki Disease | - | yes yes | 5–7 days after | - |
| Suarez-Valle et al. [91] | 4 | Spain | 3 | 3 | - | Chilblain-like | acral | - | 17 to 28 days after | - |
| Suter et al. [92] | 5 | Switzerland | 1 | 1 | M 42 | atypical erythema nodosum | shins | yes | 12 days after | - |
| Tahir et al. [93] | 5 | Dubai | 1 | 1 | M 47 | targetoid rash with central necrosis; palpable purpura and areas of vesiculation; 1 cm tender ulcer of on the undersurface of the tongue, gingival and lingual purpura | extremities, buttocks, and lower trunk; oral mucosa | yes | concomitant | - |
| Tamai et al. [10] | 4 | Japan | 3 | 3 | M 54 M 24 F 81 | maculopapular | - | yes yes yes | - 11 days after - 10 days after - 22 days after | - 6 days after hydroxychloroquine and favipiravir - - |
| Tammaro et al. [94] | 4 | Italy, Spain | - | 3 | - | vesicular | trunk | - | - | - |
| Taşkın et al. [95] | 5 | Turkey | 1 | 1 | F 61 | atypical Sweet syndrome; aphthous ulcers | cheek, scalp, extremities, trunk; hard palate and oral mucosa | yes | - | - |
| Van Damme et al. [96] | 5 | Belgium | 2 | 2 | M 71 F 39 | urticaria | generalized | yes | 1–2 days before | - |
| Verheyden et al. [97] | 5 | Belgium | 2 | 1 | M 57 | symmetric livedo reticularis | trunk, abdomen, and thighs | yes | after | - |
| Wolfe et al. [98] | 5 | USA | 1 | 1 | M 4 | polymorphic pattern: Bilateral nonpurulent conjunctivitis, strawberry tongue, erythematous lacy rash on the palms | ocular, oral, palmar | yes | - | - |
| Young et al. [99] | 5 | USA | 2 | 2 | M 68 F 39 | - polymorphic pattern: Morbilliform rash on his trunk, acral purpura and an ulcerated, purpuric plaque with livedoid borders on his buttocks - urticaria | - trunk, buttocks, acral - generalized | - yes | - - before | - - |
| Zengarini et al. [26] | 5 | Italy | 1 | 1 | F 67 | macular erythema | neck, trunk, back, and proximal portions of upper and lower limbs | yes | concomitant with fever recurrence | after 1 month of hydroxychloroquine, omeprazole, piperacillin/ tazobactam, remdesivir |
| Zhang Y et al. [100] | 4 | China | 7 | 7 | median 59 | vascular: Acro-ischemia with finger/toe cyanosis, skin bullae, and dry gangrene | acral | yes | - | 2 and 3 weeks after |
| References | Age Sex | Rash Type | Histopathology |
|---|---|---|---|
| Abadias et al. [37] | M 64 F 60 | generalized pustular figurate erythema; drug eruption | Acanthotic epidermis with parakeratosis and numerous intracorneal, subcorneal, and intraepidermal pustules. Exocytosis of neutrophils and mild spongiosis were present at the periphery of the intraepidermal pustules. |
| Ahouach et al. [39] | F 57 | diffuse fixed erythematous blanching maculopapular lesions | Slight spongiosis, basal cell vacuolation, and mild perivascular lymphocytic infiltrate. |
| Amatore et al. [41] | M 39 | annular urticaria | Superficial perivascular infiltrate of lymphocytes without eosinophils, papillary dermal oedema, subtle epidermal spongiosis, mild lymphocyte exocytosis, lichenoid and vacuolar interface dermatitis with occasional dyskeratotic keratinocytes in the basal layer. |
| Bosch-Amate et al. [44] | F 79 | painful retiform purpuric-violaceous rash | Multiple thrombi occluding most small sized vessels of the superficial and mid-dermis. Direct immunofluorescence showed the deposition of IgM, C3, and fibrinogen within superficial-to-deep dermal blood vessel walls. |
| de Masson et al. [47] | chilblain-like | Lichenoid dermatitis with a perivascular and eccrine mononuclear infiltrate and vascular microthrombi in two cases. | |
| Diaz-Guimaraens et al. [49] | M 48 | confluent erythematous macules and papules | Superficial perivascular lymphocytic infiltrate with abundant red cell extravasation and focal papillary oedema, along with focal parakeratosis and isolated dyskeratotic cells. No features of thrombotic vasculopathy were present. |
| Dominguez-Santas et al. [50] | F 71 | purpuric macules and papules | Vessel damage with fibrinoid necrosis of vessel walls, transmural infiltration by neutrophils with karyorrhexis, leukocytoclasia, and extravasated erythrocyte, with granular deposition of C3 within vessel walls. |
| Droesch et al. [51] | livedo racemosa and retiform purpura | Pauci-inflammatory thrombogenic vasculopathy involving capillaries, venules, and/or arterioles or small arteries. In three of dermal arterial thrombosis was noted, reminiscent of antiphospholipid syndrome, without any diagnostic confirmation of these antibodies. | |
| Fernandez-Nieto et al. [55] | varicella-like exanthem | Intraepidermal vesicles with mild acantholysis and ballooned keratinocytes. | |
| Fernandez-Nieto et al. [56] | F 32 | urticaria | Perivascular infiltrate of lymphocytes, some eosinophils, and upper dermal oedema. |
| Freeman et al. [36] | chilblain-like | Mild vacuolar interface dermatitis with dense superficial and deep lymphocytic inflammation, consistent with pernio versus connective tissue disease. No thrombi were noted. | |
| Gianotti et al. [25] | F 59 F 89 M 57 | erythematous macules and papules | Superficial perivascular dermatitis |
| Gianotti et al. [23] | four maculopapular rash, two chickenpox like, one of which presented with Grover disease-like pattern, two livedoid exanthemas | Papular phase: Exocytosis with minimal vacuolar changes near the dermal–epidermal junction. In one of these patients, there were nests of intraepidermal Langerhans cells associated with signs of vasculitis and extravasation of red blood cells. Chickenpox eruption: Characteristic clefts in the lower epidermis, as well as dyskeratotic keratinocytes in the granular layer and also near the basement membrane. Livedoid exanthematous eruption: Nest of Langerhans cells in the epidermis. In the deep dermis and occasionally in the superficial dermis, there were microthrombi admixed with nuclear and eosinophilic debris. | |
| Jimenez-Cauhe et al. [63] | F 58-77 | erythema multiforme-like eruption | Normal basket-weave stratum corneum, and mild to moderate spongiosis in epidermis. The dermis showed dilated vessels filled with neutrophils, extravasation of red blood cells, and lymphocytic perivascular and interstitial infiltrate. Basal vacuolar changes with interface dermatitis were observed in one patient, and lymphocytic exocytosis in another. |
| Kolivras et al. [68] | M 23 | chilblain-like | Superficial and deep lichenoid, perivascular, and perieccrine infiltrate of lymphocytes, with occasional plasma cells; necrotic (apoptotic) keratinocytes. |
| Locatelli et al. [71] | M 16 | chilblain-like | Oedema of the papillary dermis, superficial and deep lymphocytic infiltrate in a perivascular and strong perieccrine pattern; there were no signs of endothelial damage. |
| Macedo-Pérez et al. [34] | M 33 M 36 | maculopapular rash | Nonspecific mild to moderate dermatitis with isolated areas with interphase dermatitis and isolated apoptotic bodies. |
| Magro et al. [72] | M 32 F 66 F 40 | - retiform purpura - dusky purpuric patches - livedo racemosa | Striking thrombogenic vasculopathy accompanied by extensive necrosis of the epidermis and adnexal structures, including the eccrine coil. There was a significant degree of interstitial and perivascular neutrophilia with prominent leukocytoclasia. IHC showed striking and extensive deposition of C5b-9 within the microvasculature. Superficial vascular ectasia and an occlusive arterial thrombus within the deeper reticular dermis in the absence of inflammation. Extensive vascular deposits of C5b-9, C3d, and C4d were observed throughout the dermis, with marked deposition in an occluded artery. A biopsy of normal-appearing deltoid skin also showed conspicuous microvascular deposits of C5b-9. Modest perivascular lymphocytic infiltrate in the superficial dermis along with deeper seated small thrombi within rare venules of the deep dermis, in the absence of a clear vasculitis. Significant vascular deposits of C5b-9 and C4d. |
| Rivera-Oyola et al. [17] | M 60 F 60 | maculopapular rash urticaria | Mild perivascular infiltrate of predominantly mononuclear cells surrounding the superficial blood vessels and epidermis showed scattered foci of hydropic changes along with minimal acanthosis, slight spongiosis, and foci of parakeratosis. |
| Robustelli et al. [84] | F 70 | AGEP; drug eruption | Subcorneal pustule with mild focal acanthosis and spongiosis, neutrophilic exocytosis, sparse keratinocyte necrosis, and a perivascular lymphocytic infiltrate with rare neutrophils and eosinophils, consistent with AGEP. |
| Rosell-Díaz et al. [8] | papular exanthema; seven patients developed target-like areas; three developed fever and facial edema; | One of them showed a superficial perivascular inflammation with eosinophils and the other showed a lichenoid pattern with eosinophils. | |
| Rotman et al. [85] | F 62 | retiform purpura plaques with concomitant calciphylaxis | Occlusive luminal thrombi and focal mural fibrin deposition. |
| Rubio-Muniz et al. [24] | six maculopapular rash, two chilblain, four targetoid lesions, two palpable purpura, two urticaria | Maculopapular: In early-onset cases, histopathology showed moderate epidermal spongiosis and perivascular lymphocytic infiltrate with eosinophils in the dermis, whereas the analysis of the delayed lesions showed perivascular lymphocytic infiltrate and histiocytes among collagen fibers without mucin deposits. | |
| Sakaida et al. [86] | F 52 | erythema multiforme-like; drug eruption | Interface changes with liquefaction and perivascular mixed cell infiltrations in the papillary dermis are observed. There are histiocytic infiltrations around the capillary vessels and neutrophils are scattered in the upper dermis. |
| Sanchez et al. [12] | elderly M | digitate papulosquamous eruption | Foci of spongiosis with focal parakeratosis in the epidermis and a few rounded spongiotic vesicles containing aggregates of lymphocytes and Langerhans cells. A moderate lymphohistiocytic infiltrate was present in the superficial dermis and was associated with papillary dermal oedema. |
| Skorza et al. [89] | 47 | urticarial vasculitis; drug eruption on EHP | Orthokeratotic hyperkeratosis, spongiosis, focal vacuolar degeneration of basal keratinocytes, and focal lymphocytic exocytosis. Slight inflammatory lymphomorphonuclear infiltrate of superficial dermis with minimal perivascular neutrophilic component was observed, with occasional aspects of vessel wall damage. |
| Suarez-Valle et al. [91] | Chilblain-like | Ischemic necrosis affecting the epidermis and dermis with signs of re-epithelialization. Vasculitis or microthrombi were not found after reviewing extensive deep sections. | |
| Tahir et al. [93] | M 47 | targetoid rash with central necrosis; palpable purpura and areas of vesiculation; 1 cm tender ulcer of on the undersurface of the tongue, gingival, and lingual purpura | Endothelial swelling, neutrophilic vessel wall infiltration, karyorrhectic debris, and fibrin deposition in small and medium-sized dermal vessels with extravasated erythrocytes. There were microthrombi occluding lumina of smaller dermal capillaries. |
| Taşkın et al. [95] | F 61 | atypical Sweet syndrome with aphthous ulcers | Diffuse neutrophilic infiltration in the upper dermis and vascular proliferation with swollen endothelial cells and extravasated erythrocytes. |
| Young et al. [99] | M 68 F 39 | - polymorphic pattern: Morbilliform rash on his trunk, acral purpura reminiscent of perniosis, and an ulcerated, purpuric plaque with livedoid borders on his buttocks - urticaria | Groups of apoptotic keratinocytes in the epidermis, suggestive of a viral exanthema. A biopsy from the buttocks showed features consistent with thrombotic vasculopathy. |
| Zengarini et al. [26] | F 67 | erythematous confluent rash | Haematoxylin–eosin-stained tissue specimens showed slight superficial perivascular lymphocytic infiltrate, extremely dilated vessel in the papillary and mid dermis. |
| References | Cutaneous Manifestation | PCR Skin Lesions |
|---|---|---|
| Ahouach et al. [39] | maculopapular rash | negative |
| Dominguez-Santas et al. [50] | maculopapular rash | negative |
| Fernandez-Nieto et al. [55] | vesicular rash | negative four tested |
| Llamas-Velasco et al. [70] | vesicular rash | PCR in the vesicle fluid: A combination of Herpes Simplex-1 virus, Herpes Simplex-6 virus, and Epstein Barr virus in case #1, Herpes Simplex-1 virus and Herpes Simplex-7 in case #2, and Varicella Zoster virus in case #3. |
| Ping et al. [80] | conjunctivitis | two positive from conjunctival swabs |
| Sanchez et al. [12] | digitate papulosquamous eruption | negative |
| References | Cutaneous Manifestation | Coagulation Markers |
|---|---|---|
| Bosch-Amate et al. [44] | painful retiform purpuric-violaceous patches of 15 cm with some hemorrhagic blisters and crusts on both legs | D-Dimer of >10,000 ng/mL (reference value, <500). |
| Droesch et al. [51] | livedo racemosa on hands and forearms in three patients and retiform purpura on hands and forearms | All four patients had D-dimer levels of more than 3 μg/mL (normal range, 0-0.229 μg/mL) |
| Magro et al. [72] | retiform purpura, buttocks | elevated D-dimer of 1024 ng/mL (normal range 0–229) on presentation, which peaked at 2090 ng/mL on hospital day 19, and a persistently elevated INR of 1.6–1.9, but a normal PTT and platelet count. |
| dusky purpuric patches, palms, and soles | markedly elevated D-dimer of 7030 ng/mL, but normal INR and PTT | |
| reticulated eruptions, consistent with livedo racemosa, chest, legs, and arms | D-dimer was elevated at 1187 ng/mL, with a normal platelet count and PTT, but an elevated INR of 1.4. | |
| Suarez-Valle et al. [91] | chilblain-like eruption | D-dimer was elevated in the three of them and fibrinogen in two, but no other coagulation abnormalities were detected |
| Verheyden et al. [97] | symmetric livedo reticularis | elevated D-dimers |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Conforti, C.; Dianzani, C.; Agozzino, M.; Giuffrida, R.; Marangi, G.F.; di Meo, N.; Morariu, S.-H.; Persichetti, P.; Segreto, F.; Zalaudek, I.; et al. Cutaneous Manifestations in Confirmed COVID-19 Patients: A Systematic Review. Biology 2020, 9, 449. https://doi.org/10.3390/biology9120449
Conforti C, Dianzani C, Agozzino M, Giuffrida R, Marangi GF, di Meo N, Morariu S-H, Persichetti P, Segreto F, Zalaudek I, et al. Cutaneous Manifestations in Confirmed COVID-19 Patients: A Systematic Review. Biology. 2020; 9(12):449. https://doi.org/10.3390/biology9120449
Chicago/Turabian StyleConforti, Claudio, Caterina Dianzani, Marina Agozzino, Roberta Giuffrida, Giovanni Francesco Marangi, Nicola di Meo, Silviu-Horia Morariu, Paolo Persichetti, Francesco Segreto, Iris Zalaudek, and et al. 2020. "Cutaneous Manifestations in Confirmed COVID-19 Patients: A Systematic Review" Biology 9, no. 12: 449. https://doi.org/10.3390/biology9120449
APA StyleConforti, C., Dianzani, C., Agozzino, M., Giuffrida, R., Marangi, G. F., di Meo, N., Morariu, S.-H., Persichetti, P., Segreto, F., Zalaudek, I., & Neagu, N. (2020). Cutaneous Manifestations in Confirmed COVID-19 Patients: A Systematic Review. Biology, 9(12), 449. https://doi.org/10.3390/biology9120449







