The Biological Impacts of Sitagliptin on the Pancreas of a Rat Model of Type 2 Diabetes Mellitus: Drug Interactions with Metformin
Abstract
1. Introduction
2. Materials and Methods
2.1. Drugs, Chemicals, and Supplements
- Streptozotocin (STZ), a chemical powder supplied as 1 g vial, was obtained from Sigma-Aldrich Company (St. Louis, Mo, USA).
- Sitagliptin, in the form of JANUVIA® 100 tablet was obtained from Merck Sharp and Dohme Ltd. (Pavia, Italy). Each JANUVIA® 100 tablet was ground and dissolved in 10 mL solution of 0.5% carboxymethyl cellulose (CMC), and afterward shaken to obtain a suspension form (10 mg/mL).
- Metformin, in the form of GLUCOPHAGE® 500 mg tab, was purchased from Minapharm (Cairo, Egypt) under license of Merck Santé France. Each Metformin 500 mg tablet was ground and dissolved in 10 mL solution of 0.5% CMC, and afterward shaken to obtain a suspension form (50 mg/mL).
- Citric acid, sodium citrate, and sodium carboxymethyl cellulose (Na-CMC) were obtained from ADWIC CO. (Cairo, Egypt). Citric acid and sodium citrate were used for the preparation of the citrate buffer.
- The diet ingredients such as lard and soybean oil were purchased from commercial sources.
2.2. Animals
2.3. Induction of Type 2 Diabetes Mellitus
2.4. Experimental Design
- Group 1: Normal control rats were fed a basal diet, received an equivalent volume of citrate buffer solution (parallel to STZ), through the same route of administration.
- Group 2: untreated diabetic rats. The animals of this group were subdivided into 2 subgroups, 5 rats received no treatment (subgroup 2a), and the remaining 5 rats received CMC, orally for 4 weeks (subgroup 2b), parallel to sitagliptin and metformin.
- Group 3: sitagliptin-treated diabetic rats were treated with sitagliptin (10 mg/kg/day) via oral gavage for 4 weeks.
- Group 4: metformin-treated diabetic rats were treated with metformin (200 mg/kg/day) via oral gavage for 4 weeks.
- Group 5: both combined-treated diabetic rats received both sitagliptin (10 mg/kg/day) and metformin (200 mg/kg/day) via oral gavage for 4 weeks.
2.5. Blood Glucose Tolerance Test (OGTT)
2.6. Biochemical Profile Assays
2.7. Histological Procedures
- Hematoxylin and eosin (H&E) according to previously stated protocols [22].
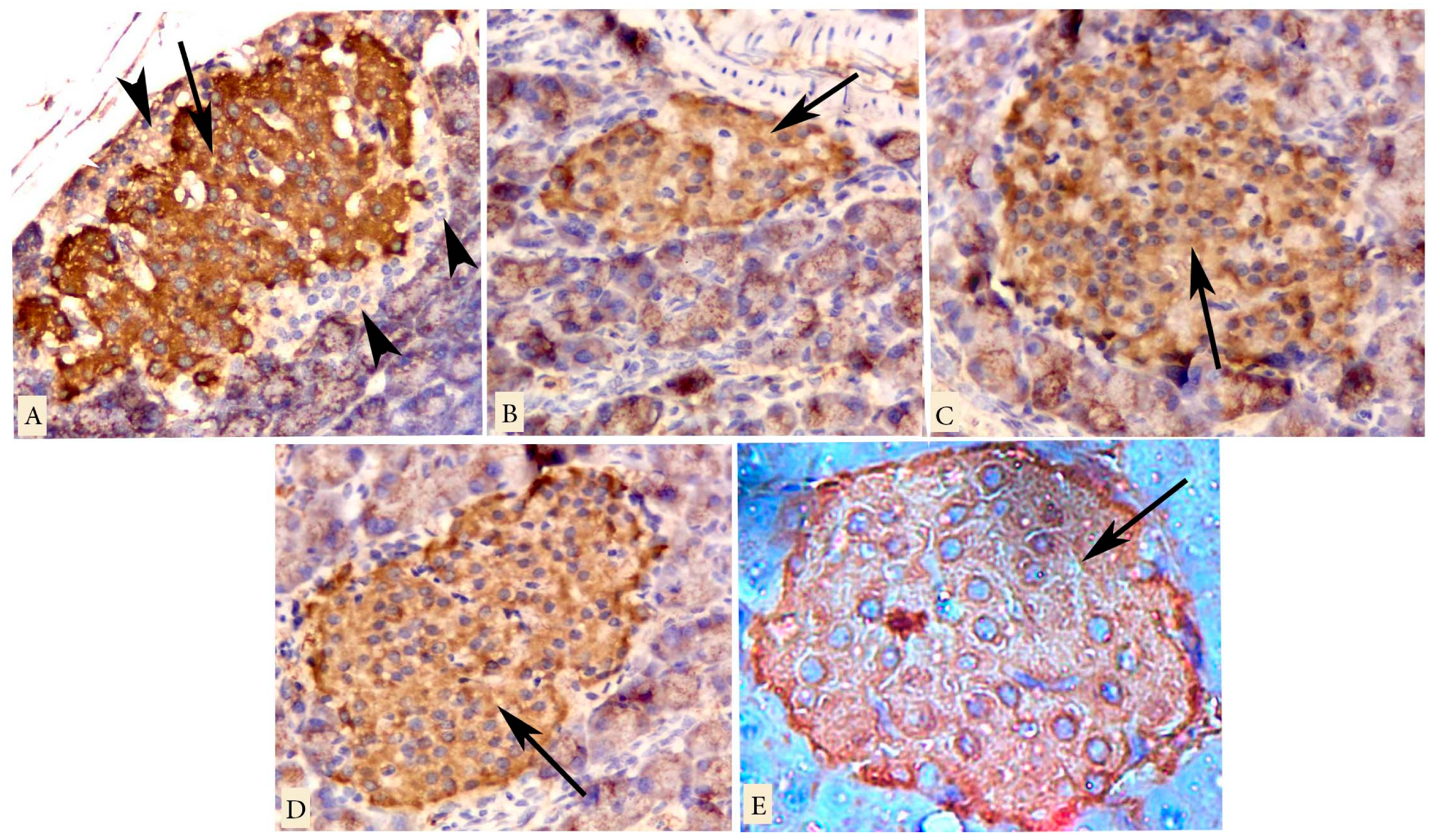
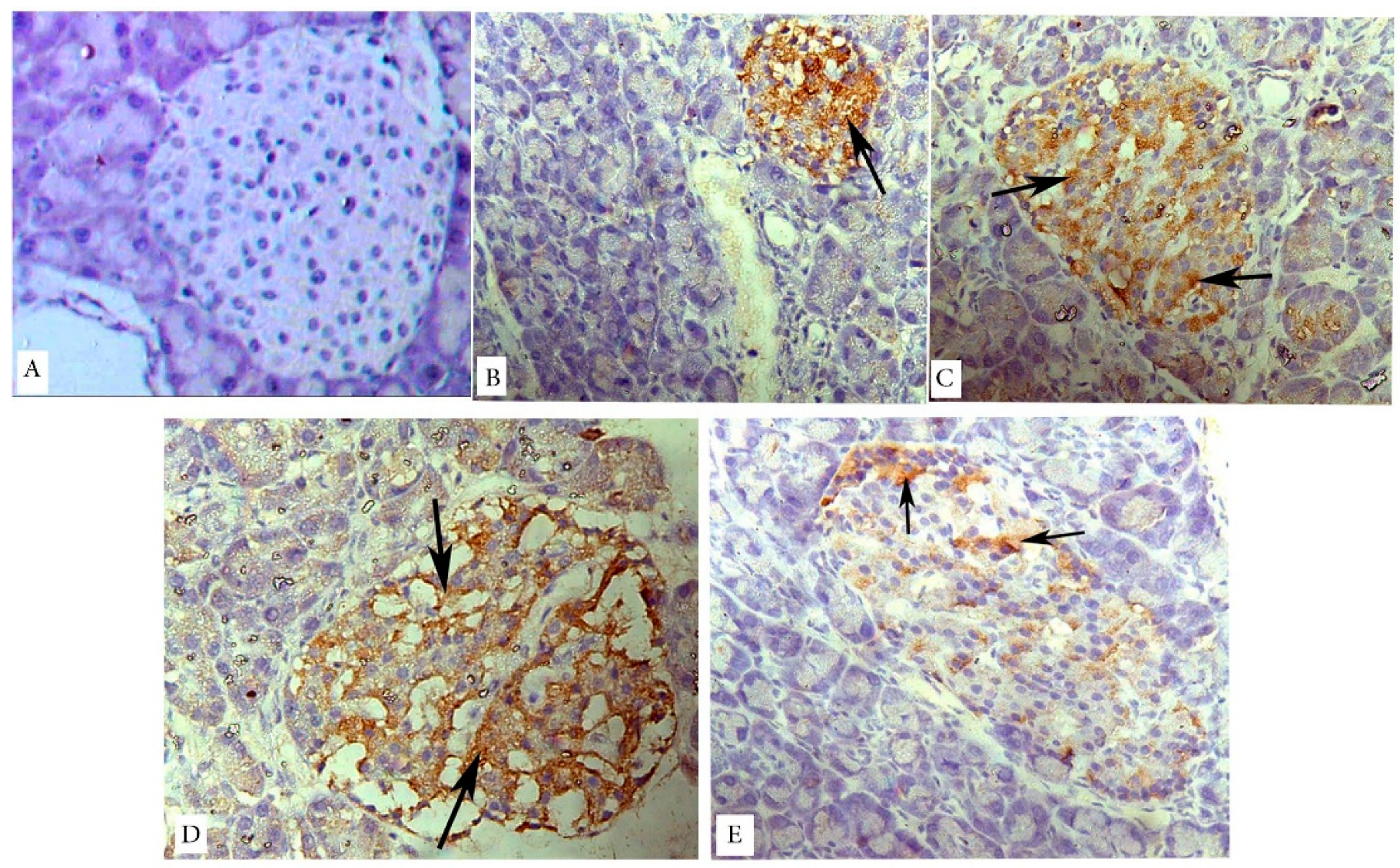
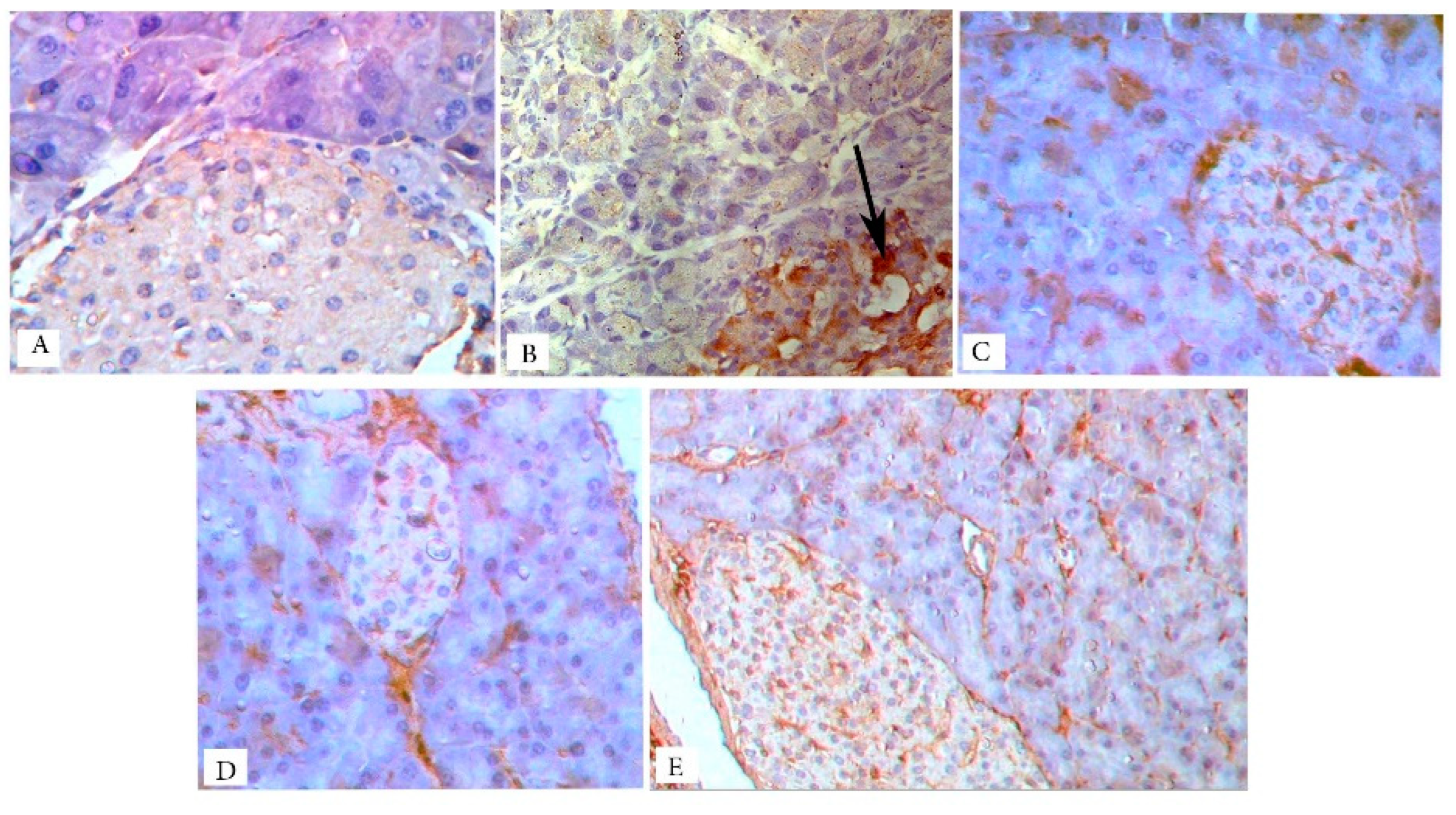
- Immunohistochemical techniques, using the peroxidase-labeled streptavidin-biotin method, according to previously demonstrated protocols [23].Immunohistochemical staining was applied for the detection of insulin antibody (INS05 (2D11-H5)). The primary antibody used was mouse monoclonal insulin antibody (Labvision Corporation, Fremont, CA, USA). It was supplied at a dilution of 0.5–1.0 µg/mL and incubated with the slides for one hour at room temperature.Immunohistochemical staining for the detection of the caspase-3 antibody as a marker of apoptosis. The primary antibody used was rabbit polyclonal caspase-3 antibody (Labvision Corporation, Fremont, CA, USA). It was supplied at a dilution of 1:100 and incubated with the slides for one hour at room temperature.Immunohistochemical staining for the detection of inducible nitric oxide synthase (iNOS) antibody as a marker of inflammation. The primary antibody used was rabbit polyclonal iNOS antibody (Labvision Corporation, Fremont, CA, USA). It was supplied at a dilution of 1 µg/mL and incubated with the slides for one hour at room temperature.
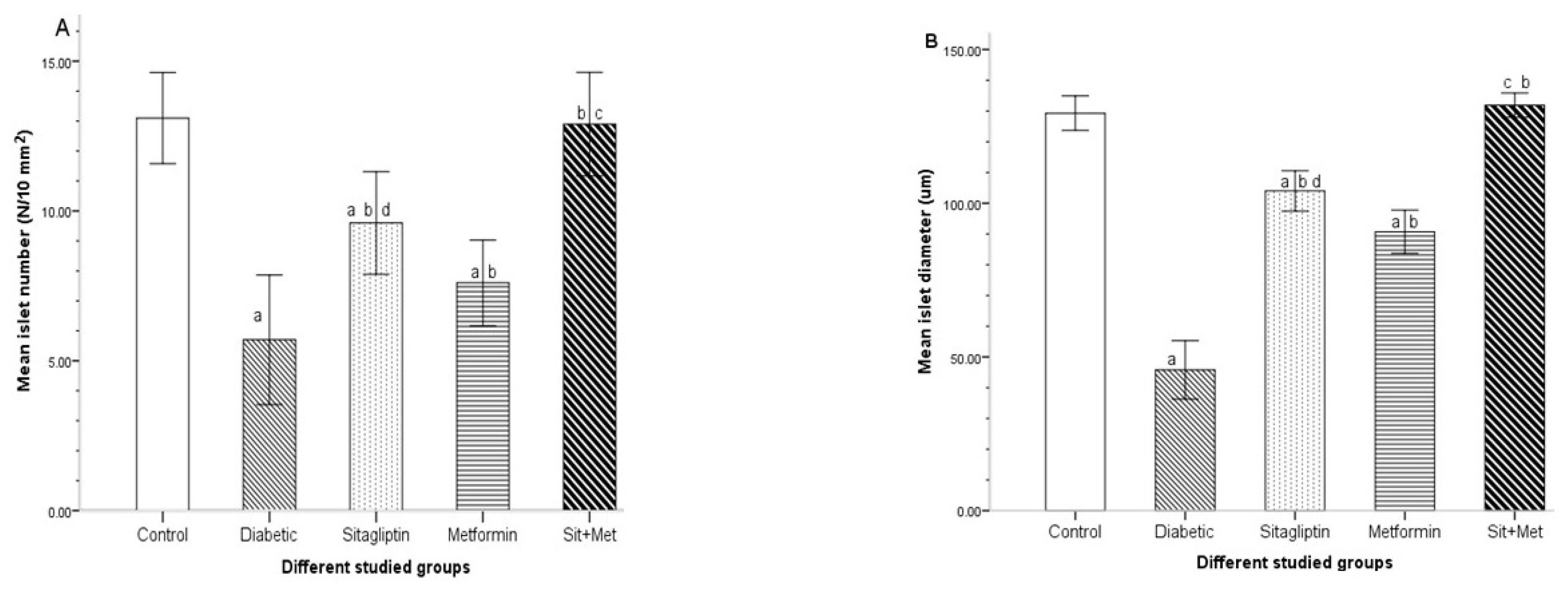
2.8. Histomorphometric Analysis
- Assessment of the islet number and islet size: For each study group, the islets were counted, and islet size was evaluated in 10 different, randomly selected microscopic fields, using lower magnification. Then, the mean islet number per field and mean islet size were calculated for each group of animals. The number of islets was expressed as N/10 mm2 of the pancreatic parenchyma, according to Noor et al. [24]. For the islet size, the maximum diameter of the islet was selected by comparing all possible radii diameters per islet and choosing the greatest according to previous work [4].
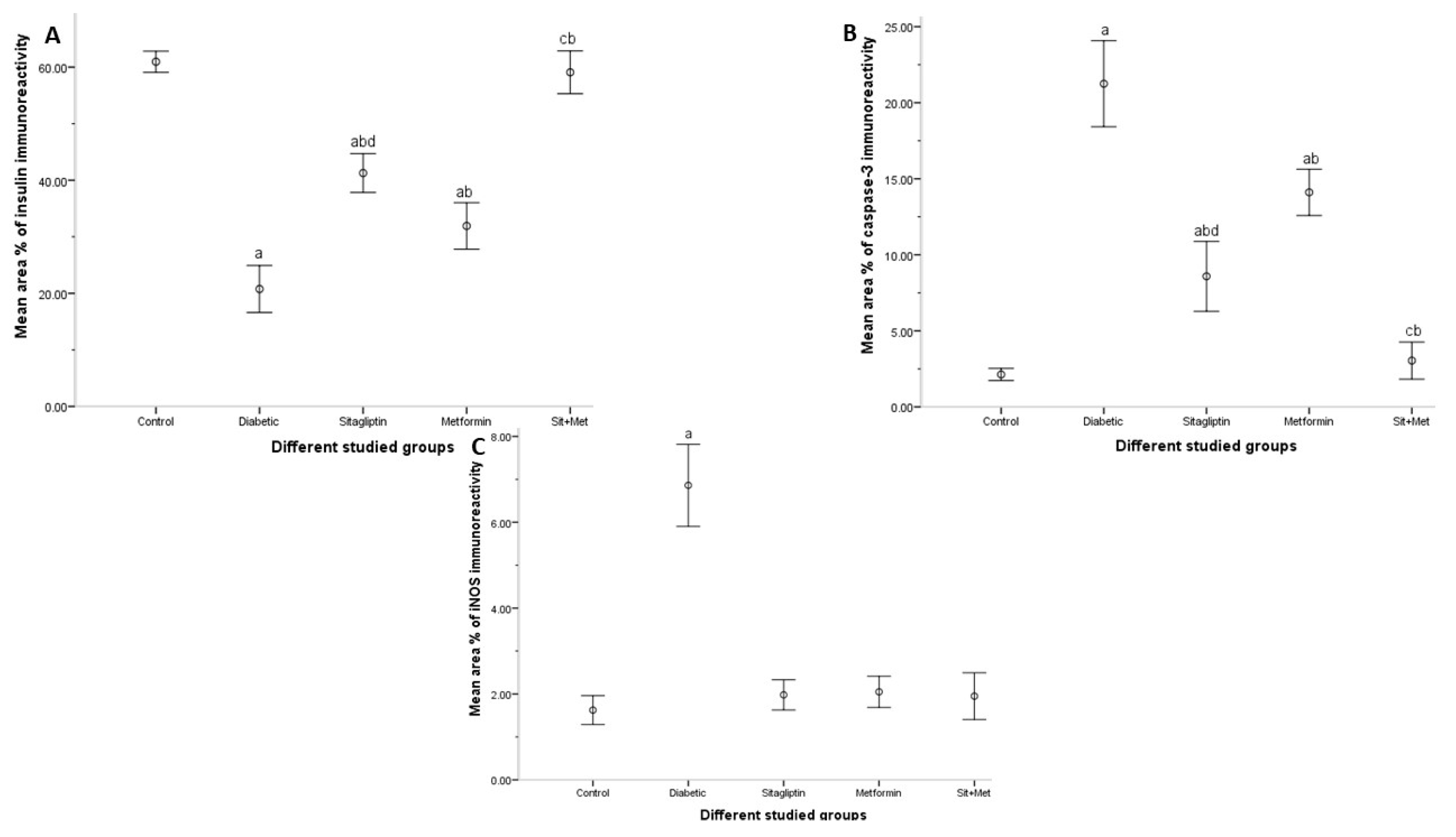
- Evaluation of the area % of insulin, caspase-3, and iNOS immunostaining: They were measured in 10 non-overlapping high power fields, using the interactive measurements menu. The brown coloration of the immunoreaction was covered automatically by a blue mask (binary image). The area of this binary image was then calculated, which reflected the positively stained cells for insulin, caspase-3, and iNOS.
2.9. Statistical Analyses
3. Results
3.1. Mortality, Food Intake, Water Intake, and Changes in Body Weight, Pancreas Weight, and Pancreas Weight to Body Weight Ratio
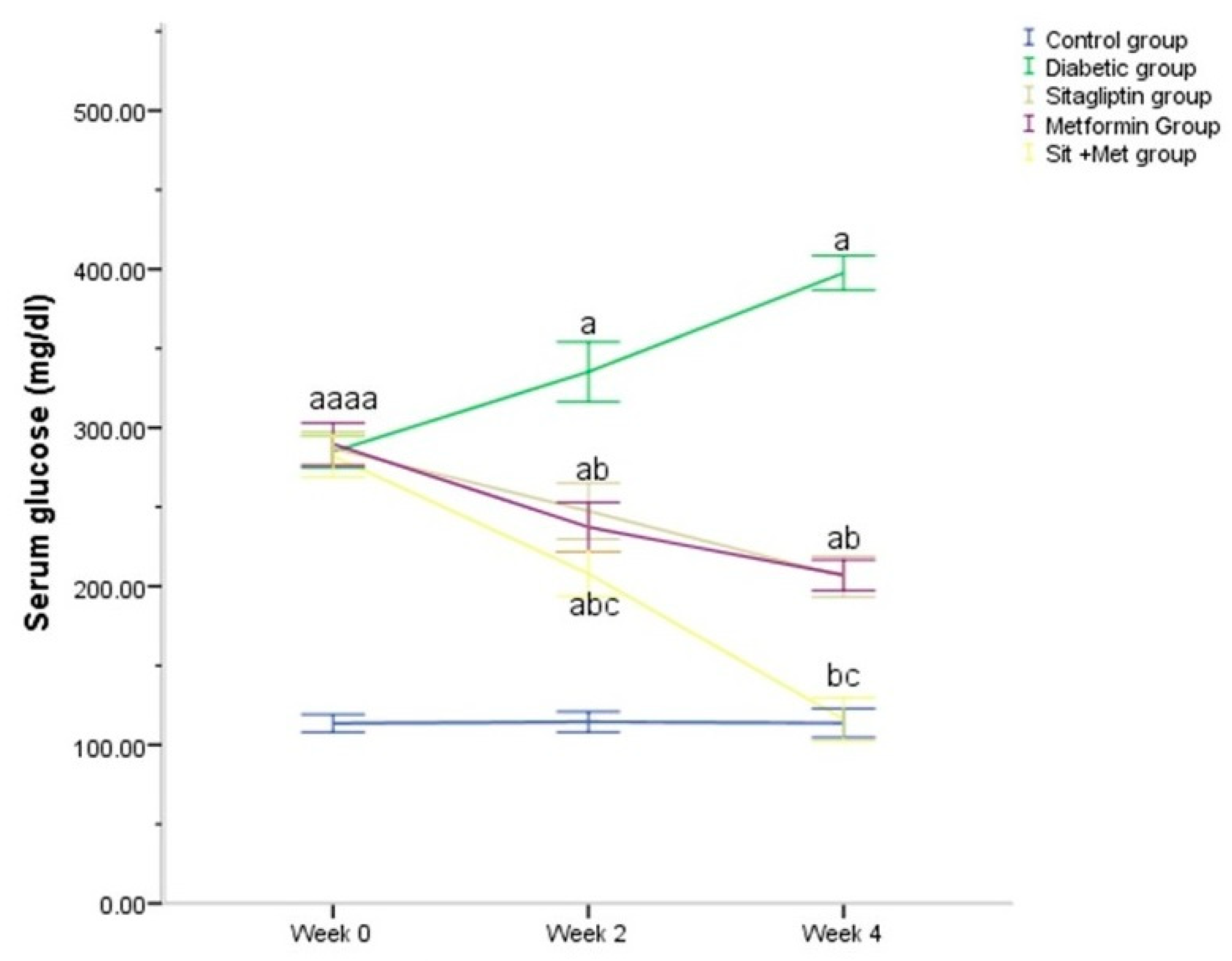
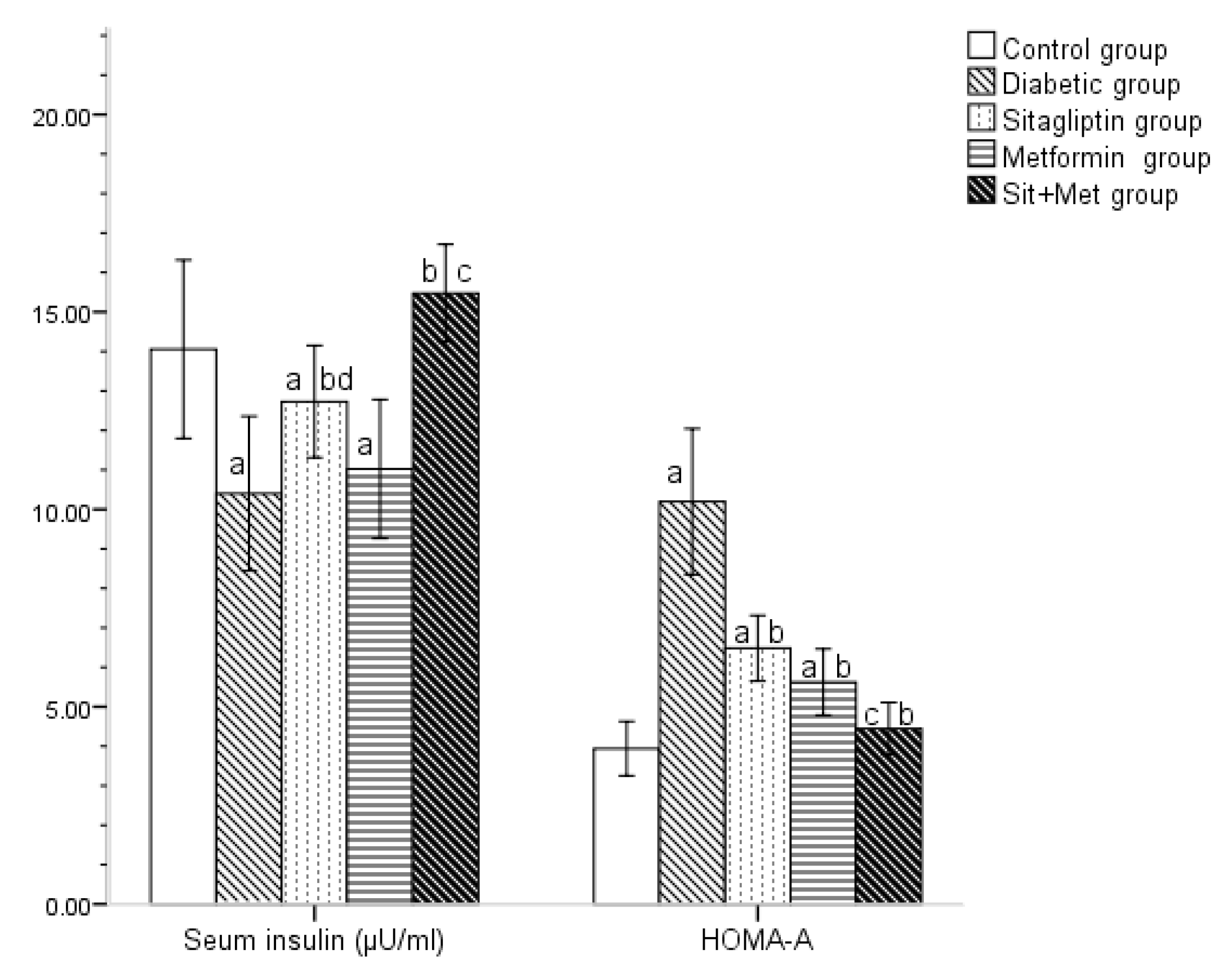
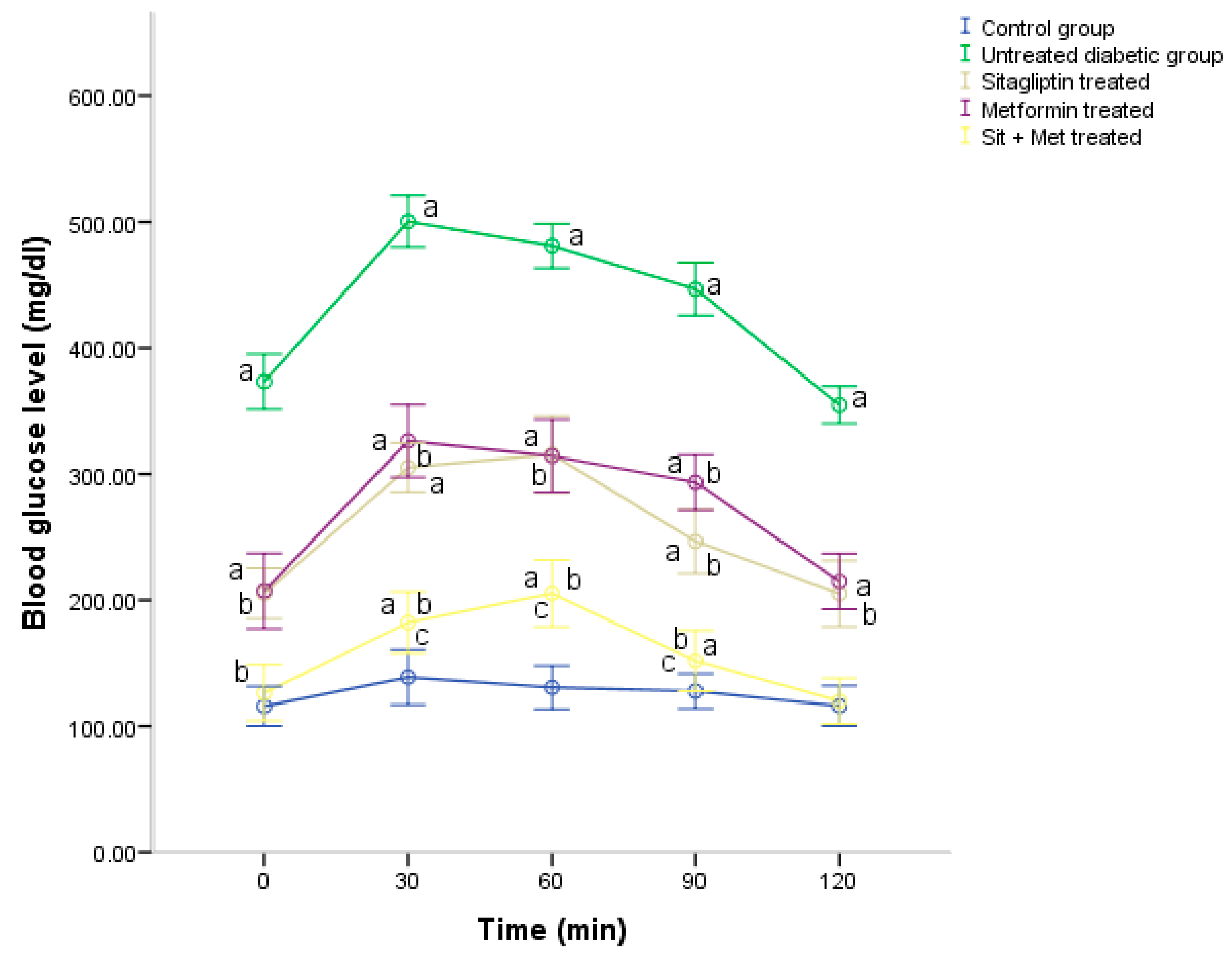
3.2. Glucose Homeostasis Parameters
3.3. Lipid Profile
3.4. Serum Lipase
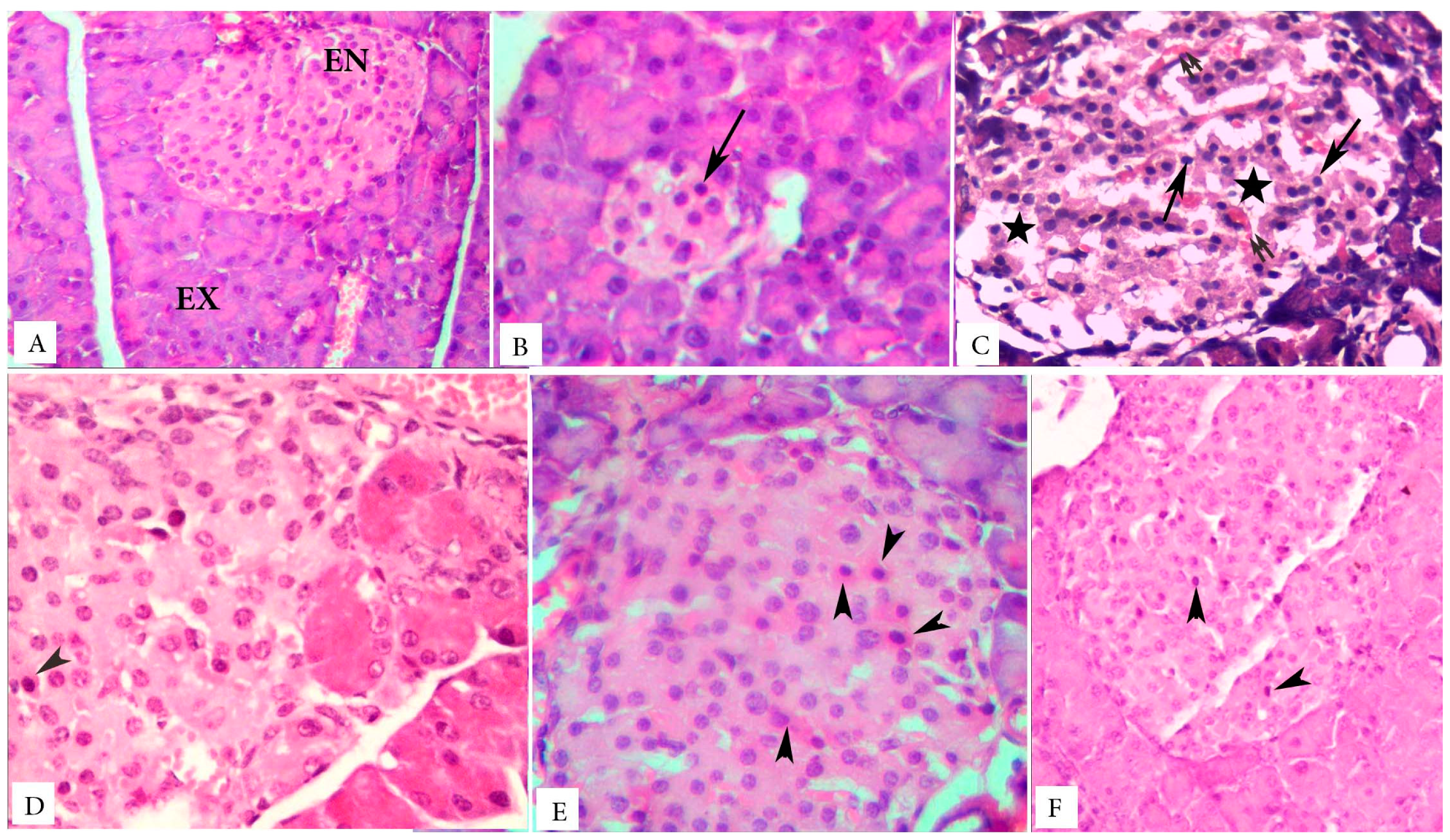
3.5. Islet Cells Morphology and Pancreatic Acini
3.6. Immunohistochemical Observations
3.7. Histomorphometric Results
3.7.1. The Mean Islet Number and Islet Size
3.7.2. Area Percent of Insulin Immunoreactivity
3.7.3. Area Percent of Caspase-3 Immunoreactivity
3.7.4. Area Percent of iNOS Immunoreactivity
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Tao, Z.; Shi, A.; Zhao, J. Epidemiological Perspectives of Diabetes. Cell Biochem. Biophys. 2015, 73, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Magalhaes, D.A.; Kume, W.T.; Correia, F.S.; Queiroz, T.S.; Allebrandt Neto, E.W.; Santos, M.P.; Kawashita, N.H.; França, S.A. High-fat diet and streptozotocin in the induction of type 2 diabetes mellitus: A new proposal. An. Acad. Bras. Cienc. 2019, 91. [Google Scholar] [CrossRef] [PubMed]
- Hostalek, U.; Gwilt, M.; Hildemann, S. Therapeutic use of metformin in prediabetes and diabetes prevention. Drugs 2015, 75, 1071–1094. [Google Scholar] [CrossRef] [PubMed]
- Mega, C.; Vala, H.; Rodrigues-Santos, P.; Oliveira, J.; Teixeira, F.; Fernandes, R.; Reis, F.; de Lemos, E.T. Sitagliptin prevents aggravation of endocrine and exocrine pancreatic damage in the Zucker Diabetic Fatty rat—Focus on amelioration of metabolic profile and tissue cytoprotective properties. Diabetol. Metab. Syndr. 2014, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- Nauck, M. Incretin therapies: Highlighting common features and differences in the modes of action of glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors. Diabetes Obes. Metab. 2016, 18, 203–216. [Google Scholar] [CrossRef]
- Mega, C.; Teixeira-de-Lemos, E.; Fernandes, R.; Reis, F. Renoprotective Effects of the Dipeptidyl Peptidase-4 Inhibitor Sitagliptin: A Review in Type 2 Diabetes. J. Diabetes Res. 2017, 2017, 5164292. [Google Scholar] [CrossRef]
- Teodoro, J.S.; Nunes, S.; Rolo, A.P.; Reis, F.; Palmeira, C.M. Therapeutic options targeting oxidative stress, mitochondrial dysfunction and inflammation to hinder the progression of vascular complications of diabetes. Front. Physiol. 2018, 9, 1857. [Google Scholar] [CrossRef]
- Sakura, H.; Hashimoto, N.; Sasamoto, K.; Ohashi, H.; Hasumi, S.; Ujihara, N.; Kasahara, T.; Tomonaga, O.; Nunome, H.; Honda, M.; et al. Effect of sitagliptin on blood glucose control in patients with type 2 diabetes mellitus who are treatment naive or poorly responsive to existing antidiabetic drugs: The JAMP study. BMC Endocr. Disord. 2016, 16, 70. [Google Scholar] [CrossRef]
- Nachnani, J.S.; Bulchandani, D.G.; Nookala, A.; Herndon, B.; Molteni, A.; Pandya, P.; Taylor, R.; Quinn, T.; Weide, L.; Alba, L.M. Biochemical and histological effects of exendin-4 (exenatide) on the rat pancreas. Diabetologia 2010, 53, 153–159. [Google Scholar] [CrossRef]
- Nelson, M.; Bhandari, N.; Wener, J. Sitagliptin-induced pancreatitis—A longer road than expected. Clin. Case Rep. 2014, 2, 149–152. [Google Scholar] [CrossRef]
- Buse, J.B.; Bethel, M.A.; Green, J.B.; Stevens, S.R.; Lokhnygina, Y.; Aschner, P.; Grado, C.R.; Tankova, T.; Wainstein, J.; Josse, R.; et al. Pancreatic safety of sitagliptin in the TECOS study. Diabetes Care 2017, 40, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Vrang, N.; Jelsing, J.; Simonsen, L.; Jensen, A.E.; Thorup, I.; Soeborg, H.; Knudsen, L.B. The effects of 13 wk of liraglutide treatment on endocrine and exocrine pancreas in male and female ZDF rats: A quantitative and qualitative analysis revealing no evidence of drug-induced pancreatitis. AJP Endocrinol. Metab. 2012, 303, E253–E264. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-G.; Kim, S.; Han, S.J.; Kim, D.J.; Lee, K.-W.; Kim, H.J. Dipeptidyl Peptidase-4 Inhibitors and the Risk of Pancreatitis in Patients with Type 2 Diabetes Mellitus: A Population-Based Cohort Study. J. Diabetes Res. 2018, 2018. [Google Scholar] [CrossRef] [PubMed]
- Committee NRC. Guide for the Care and Use of Laboratory Animals: NIH Publications No. 8023, 8th ed.; National Academies Press: Cambridge, MA, USA, 2010; 220p. [Google Scholar]
- Furman, B.L. Streptozotocin-induced diabetic models in mice and rats. Curr. Protoc. Pharmacol. 2015, 70, 5–47. [Google Scholar] [CrossRef] [PubMed]
- Mega, C.; Vala, H.; Teixeira de Lemos, E.; Fernandes, R.; Oliveira, J.; Ferreira, L.; Teixeira, F.; Reis, F. Biochemical and histological effects of sitagliptin on Zucker Diabetic Fatty rat pancreas. Virchows Arch. 2010, 457, 91–281. [Google Scholar]
- Saad, M.I.; Kamel, M.A.; Hanafi, M.Y. Modulation of adipocytokines production and serum NEFA level by metformin, glimepiride, and sitagliptin in HFD/STZ diabetic rats. Biochem. Res. Int. 2015, 2015, 138134. [Google Scholar] [CrossRef]
- Mohamed, N.A.; Zaitone, S.A.; Moustafa, Y.M. Effect of Sitagliptin in Combination with Glimepiride on Glycemic Control and Islet Cell Diameter / Proliferation in A Model of Type 2 Diabetic Rats. IOSR J. Pharm. 2013, 3, 72–80. [Google Scholar] [CrossRef]
- Jin, J.; Lim, S.W.; Jin, L.; Yu, J.H.; Kim, H.S.; Chung, B.H. Effects of metformin on hyperglycemia in an experimental model of tacrolimus- and sirolimus-induced diabetic rats. Korean J. Intern Med. 2017, 32, 314–322. [Google Scholar] [CrossRef]
- Tsukamoto, A.; Niino, N.; Sakamoto, M.; Ohtani, R.; Inomata, T. The validity of anesthetic protocols for the surgical procedure of castration in rats. Exp. Anim. 2018, 67, 329–336. [Google Scholar] [CrossRef]
- Guo, X.; Wang, Y.; Wang, K.; Ji, B.; Zhou, F. Stability of a type 2 diabetes rat model induced by high-fat diet feeding with low-dose streptozotocin injection. J. Zhejiang Univ. B 2018, 19, 559–569. [Google Scholar] [CrossRef]
- Bancroft, J.D.; Lyton, C. The Hematoxylins and Eosin. In Theory and Practice of Histological Techniques, 8th ed.; Suvarna, S.K., Bancroft, J.D., Lyton, C., Eds.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2018; pp. 126–138. [Google Scholar]
- Kiernan, J.A. Immunohistochemistry. In Histological and Histochemical Methods Theory and Practice, 4th ed.; Kiernan, J., Ed.; Scion Publishing Ltd.: Banbury, UK, 2015; pp. 454–490. [Google Scholar]
- Noor, A.; Gunasekaran, S.; Vijayalakshmi, M.A. Improvement of Insulin Secretion and Pancreatic β-cell Function in Streptozotocin-induced Diabetic Rats Treated with Aloe vera Extract. Pharmacogn. Res. 2017, 9, S99–S104. [Google Scholar] [CrossRef] [PubMed]
- Andersen, E.S.; Deacon, C.F.; Holst, J.J. Do we know the true mechanism of action of the DPP-4 inhibitors? Diabetes Obes. Metab. 2018, 20, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Matveyenko, A.V.; Dry, S.; Cox, H.I.; Moshtaghian, A.; Gurlo, T.; Galasso, R.; Butler, A.E.; Butler, P.C. Beneficial endocrine but adverse exocrine effects of sitagliptin in the human islet amyloid polypeptide transgenic rat model of type 2 diabetes: Interactions with metformin. Diabetes 2009, 58, 1604–1615. [Google Scholar] [CrossRef] [PubMed]
- Rouse, R.; Xu, L.; Stewart, S.; Zhang, J. High fat diet and GLP-1 drugs induce pancreatic injury in mice. Toxicol. Appl. Pharmacol. 2014, 276, 104–114. [Google Scholar] [CrossRef] [PubMed]
- Czech, M.P. Insulin action and resistance in obesity and type 2 diabetes. Nat. Med. 2017, 23, 804–814. [Google Scholar] [CrossRef] [PubMed]
- Wortham, M.; Sander, M. Mechanisms of β-cell functional adaptation to changes in workload. Diabetes Obes. Metab. 2016, 18, 78–86. [Google Scholar] [CrossRef]
- DeFronzo, R.A. Pathogenesis of type 2 diabetes mellitus. In Diabetes Epidemiology, Genetics, Pathogenesis, Diagnosis, Prevention, and Treatment; Bonora, E., DeFronzo, R.A., Eds.; Springer: Cham, Switzerland, 2018; pp. 181–253. [Google Scholar]
- Skovsø, S. Modeling type 2 diabetes in rats using high fat diet and streptozotocin. J. Diabetes Investig. 2014, 5, 349–358. [Google Scholar] [CrossRef]
- Reimer, R.A.; Grover, G.J.; Koetzner, L.; Gahler, R.J.; Lyon, M.R.; Wood, S. Combining sitagliptin/metformin with a functional fiber delays diabetes progression in Zucker rats. J. Endocrinol. 2014, 220, 361–373. [Google Scholar] [CrossRef]
- Zhou, J.; Zhou, S.; Zeng, S. Experimental diabetes treated with trigonelline: Effect on β cell and pancreatic oxidative parameters. Fundam. Clin. Pharmacol. 2013, 27, 279–287. [Google Scholar] [CrossRef]
- Zhuo, J.; Zeng, Q.; Cai, D.; Zeng, X.; Chen, Y.; Gan, H.; Huang, X.; Yao, N.; Huang, D.; Zhang, C. Evaluation of type 2 diabetic mellitus animal models via interactions between insulin and mitogen-activated protein kinase signaling pathways induced by a high fat and sugar diet and streptozotocin. Mol. Med. Rep. 2018, 17, 5132–5142. [Google Scholar] [CrossRef]
- Kahn, S.E.; Cooper, M.E.; Del Prato, S. Pathophysiology and treatment of type 2 diabetes: Perspectives on the past, present, and future. Lancet 2014, 383, 1068–1083. [Google Scholar] [CrossRef]
- Lindsay, J.R.; Duffy, N.A.; McKillop, A.M.; Ardill, J.; O’Harte, F.P.M.; Flatt, P.R.; Bell, P.M. Inhibition of dipeptidyl peptidase IV activity by oral metformin in Type 2 diabetes. Diabet Med. 2005, 22, 654–657. [Google Scholar] [CrossRef] [PubMed]
- Naidu, P.B.; Ponmurugan, P.; Begum, M.S.; Mohan, K.; Meriga, B.; RavindarNaik, R.; Saravanan, G. Diosgenin reorganises hyperglycaemia and distorted tissue lipid profile in high-fat diet–streptozotocin-induced diabetic rats. J. Sci. Food Agric. 2015, 95, 3177–3182. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.A.; Sarkerm, M.M.R.; Gousuddin, M. Antidiabetic potential of Brassica Oleracea Var. Italica in type 2 diabetic sprague dawley (sd) rats. Int. J. Pharmacogn. Phytochem. Res. 2016, 8, 462–469. [Google Scholar]
- Hussien, N.I.; Ebrahim, N.; Mohammed, O.M.; Sabry, D. Combination of obestatin and bone marrow mesenchymal stem cells prevents aggravation of endocrine pancreatic damage in type II diabetic rats. Int. J. Stem. Cells 2017, 10, 129–143. [Google Scholar] [CrossRef]
- Saad, M.I.; Kamel, M.A.; Hanafi, M.Y.; Helmy, M.H.; Shehata, R.R. Effect of sitagliptin and glimepiride on glucose homeostasis and cAMP levels in peripheral tissues of HFD/STZ diabetic rats. Am. J. Biomed. Res. 2014, 2, 52–60. [Google Scholar] [CrossRef]
- Eitah, H.E.; Maklad, Y.A.; Abdelkader, N.F.; el Din, A.A.G.; Badawi, M.A.; Kenawy, S.A. Modulating impacts of quercetin/sitagliptin combination on streptozotocin-induced diabetes mellitus in rats. Toxicol. Appl. Pharmacol. 2019, 365, 30–40. [Google Scholar] [CrossRef]
- Antony, P.J.; Gandhi, G.R.; Stalin, A.; Balakrishna, K.; Toppo, E.; Sivasankaran, K.; Ignacimuthu, S.; Al-Dhabi, N.A. Myoinositol ameliorates high-fat diet and streptozotocin-induced diabetes in rats through promoting insulin receptor signaling. Biomed. Pharmacother. 2017, 88, 1098–1113. [Google Scholar] [CrossRef]
- Zheng, W.; Zhou, J.; Song, S.; Kong, W.; Xia, W.; Chen, L.; Zeng, T. Dipeptidyl-peptidase 4 inhibitor sitagliptin ameliorates hepatic insulin resistance by modulating inflammation and autophagy in ob/ob mice. Int. J. Endocrinol. 2018, 2018, 8309723. [Google Scholar] [CrossRef]
- Hu, H.; Xu, M.; Qi, R.; Wang, Y.; Wang, C.; Liu, J.; Luo, L.; Xia, L.; Fang, Z. Sitagliptin downregulates retinol-binding protein 4 and upregulates glucose transporter type 4 expression in a type 2 diabetes mellitus rat model. Int. J. Clin. Exp. Med. 2015, 8, 17902. [Google Scholar]
- Shao, Y.; Yu, Y.; Li, C.; Yu, J.; Zong, R.; Pei, C. Synergistic effect of quercetin and 6-gingerol treatment in streptozotocin induced type 2 diabetic rats and poloxamer P-407 induced hyperlipidemia. RSC Adv. 2016, 6, 12235–12242. [Google Scholar] [CrossRef]
- Abbas, N.A.T.; El Salem, A. Metformin, sitagliptin, and liraglutide modulate serum retinol-binding protein-4 level and adipocytokine production in type 2 diabetes mellitus rat model. Can. J. Physiol. Pharmacol. 2018, 96, 1226–1231. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhang, S.-T.; Yin, Y.-C.; Xing, S.; Li, W.-N.; Fu, X.-Q. Hypoglycemic effect and mechanism of isoquercitrin as an inhibitor of dipeptidyl peptidase-4 in type 2 diabetic mice. RSC Adv. 2018, 8, 14967–14974. [Google Scholar] [CrossRef]
- Mu, J.; Woods, J.; Zhou, Y.P.; Roy, R.S.; Li, Z.; Zycband, E.; Feng, Y.; Zhu, L.; Li, C.; Howard, A.D.; et al. Chronic inhibition of dipeptidyl peptidase-4 with a sitagliptin analog preserves pancreatic β-cell mass and function in a rodent model of type 2 diabetes. Diabetes 2006, 55, 1695–1704. [Google Scholar] [CrossRef] [PubMed]
- Shigematsu, E.; Yamakawa, T.; Kadonosono, K.; Terauchi, Y. Effect of sitagliptin on lipid profile in patients with type 2 diabetes mellitus. J. Clin. Med. Res. 2014, 6, 327–335. [Google Scholar] [CrossRef]
- Bolevich, S.; Draginic, N.; Andjic, M.; Jeremic, N.; Bolevich, S.; Litvitskiy, P.F.; Jakovljevic, V. The Effects of DPP4 Inhibitors on Lipid Status and Blood Pressure in Rats with Diabetes Mellitus Type 2. Serb. J. Exp. Clin. Res. 2019, 1. [Google Scholar] [CrossRef]
- Kamble, H.V.; Bodhankar, S.L. Cardioprotective effect of concomitant administration of trigonelline and sitagliptin on cardiac biomarkers, lipid levels, electrocardiographic and heamodynamic modulation on cardiomyopathy in diabetic Wistar rats. Biomed. Aging Pathol. 2014, 4, 335–342. [Google Scholar] [CrossRef]
- Hayes, J.; Anderson, R.; Stephens, J.W. Sitagliptin/metformin fixed-dose combination in type 2 diabetes mellitus: An evidence-based review of its place in therapy. Drug Des. Devel. Ther. 2016, 10, 2263. [Google Scholar]
- Ismail, O.Z.; Bhayana, V. Lipase or amylase for the diagnosis of acute pancreatitis? Clin. Biochem. 2017, 50, 1275–1280. [Google Scholar] [CrossRef]
- Tatarkiewicz, K.; Smith, P.A.; Sablan, E.J.; Polizzi, C.J.; Aumann, D.E.; Villescaz, C.; Hargrove, D.M.; Gedulin, B.R.; Lu, M.G.; Adams, L.; et al. Exenatide does not evoke pancreatitis and attenuates chemically induced pancreatitis in normal and diabetic rodents. Am. J. Physiol. Metab. 2010, 299, E1076–E1086. Available online: http://www.physiology.org/doi/10.1152/ajpendo.00479.2010 (accessed on 1 July 2019). [CrossRef]
- Usborne, A.; Byrd, R.A.; Meehan, J.; Blackbourne, J.L.; Sullivan, J.; Poitout-Belissent, F.; Prefontaine, A.; Martin, J.A.; Vahle, J.L. An investigative study of pancreatic exocrine biomarkers, histology, and histomorphometry in male Zucker diabetic fatty (ZDF) rats given dulaglutide by subcutaneous injection twice weekly for 13 weeks. Toxicol Pathol. 2015, 43, 1093–1102. [Google Scholar] [CrossRef] [PubMed]
- Halban, P.A.; Polonsky, K.S.; Bowden, D.W.; Hawkins, M.A.; Ling, C.; Mather, K.J.; Powers, A.C.; Rhodes, C.J.; Sussel, L.; Weir, G.C. β-cell failure in type 2 diabetes: Postulated mechanisms and prospects for prevention and treatment. J. Clin. Endocrinol. Metab. 2014, 99, 1983–1992. [Google Scholar] [CrossRef] [PubMed]
- Tangvarasittichai, S. Oxidative stress, insulin resistance, dyslipidemia and type 2 diabetes mellitus. World J. Diabetes 2015, 6, 456. [Google Scholar] [CrossRef] [PubMed]
- Kou, K.; Saisho, Y.; Sato, S.; Yamada, T.; Itoh, H. Islet number rather than islet size is a major determinant of β-and α-cell mass in humans. J. Clin. Endocrinol. Metab. 2014, 99, 1733–1740. [Google Scholar] [CrossRef] [PubMed]
- Smits, M.M.; Tonneijck, L.; Muskiet, M.H.A.; Kramer, M.H.H.; Pieters-van den Bos, I.C.; Vendrik, K.E.W.; Hoekstra, T.; Bruno, M.J.; Diamant, M.; van Raalte, D.H.; et al. Pancreatic effects of liraglutide or sitagliptin in overweight patients with type 2 diabetes: A 12-week randomized, placebo-controlled trial. Diabetes Care 2017, 40, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Kirk, R.K.; Pyke, C.; von Herrath, M.G.; Hasselby, J.P.; Pedersen, L.; Mortensen, P.G.; Knudsen, L.B.; Coppieters, K. Immunohistochemical assessment of glucagon-like peptide 1 receptor (GLP-1R) expression in the pancreas of patients with type 2 diabetes. Diabetes Obes. Metab. 2017, 19, 705–712. [Google Scholar] [CrossRef]
- Gier, B.; Matveyenko, A.V.; Kirakossian, D.; Dawson, D.; Dry, S.M.; Butler, P.C. Chronic GLP-1 receptor activation by exendin-4 induces expansion of pancreatic duct glands in rats and accelerates formation of dysplastic lesions and chronic pancreatitis in the KrasG12D mouse model. Diabetes 2012, 61, 1250–1262. [Google Scholar] [CrossRef]
- Suman, R.K.; Ray Mohanty, I.; Borde, M.K.; Maheshwari, U.; Deshmukh, Y.A. Development of an experimental model of diabetes co-existing with metabolic syndrome in rats. Adv. Pharmacol. Sci. 2016, 2016, 9463476. [Google Scholar] [CrossRef]
- Remedi, M.S.; Emfinger, C. Pancreatic β-cell identity in diabetes. Diabetes Obes. Metab. 2016, 18, 110–116. [Google Scholar] [CrossRef]
- Solano-Gálvez, S.G.; Abadi-Chiriti, J.; Gutiérrez-Velez, L.; Rodríguez-Puente, E.; Konstat-Korzenny, E.; Álvarez-Hernández, D.-A.; Hernández, D.A.; Franyuti-Kelly, G.; Gutiérrez-Kobeh, L.; Vázquez-López, R. Apoptosis: Activation and inhibition in health and disease. Med. Sci. 2018, 6, 54. [Google Scholar] [CrossRef]
- Liu, L.; Du, X.; Zhang, Z.; Zhou, J. Trigonelline inhibits caspase 3 to protect β cells apoptosis in streptozotocin-induced type 1 diabetic mice. Eur. J. Pharmacol. 2018, 836, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Tomita, T. Apoptosis in pancreatic β-islet cells in Type 2 diabetes. Bosn. J. Basic Med. Sci. 2016, 16, 162–179. Available online: https://www.ncbi.nlm.nih.gov/pubmed/27209071 (accessed on 15 July 2019). [CrossRef] [PubMed]
- Samaha, M.M.; Said, E.; Salem, H.A. A comparative study of the role of crocin and sitagliptin in attenuation of STZ-induced diabetes mellitus and the associated inflammatory and apoptotic changes in pancreatic β-islets. Environ. Toxicol. Pharmacol. 2019, 72, 103238. [Google Scholar] [CrossRef] [PubMed]
- Cinelli, M.A.; Do, H.T.; Miley, G.P.; Silverman, R.B. Inducible nitric oxide synthase: Regulation, structure, and inhibition. Med. Res. Rev. 2019, 1–32. [Google Scholar] [CrossRef]
- Sai Varsha, M.K.N.; Thiagarajan, R.; Manikandan, R.; Dhanasekaran, G. Vitamin K1 alleviates streptozotocin-induced type 1 diabetes by mitigating free radical stress, as well as inhibiting NF-kB activation and iNOS expression in rat pancreas. Nutrition 2015, 31, 214–222. [Google Scholar] [CrossRef]
- Garcia, F.A.O.; Pinto, S.F.; Cavalcante, A.F.; Lucetti, L.T.; Menezes, S.M.S.; Felipe, C.F.B.; Alves, A.P.N.; Brito, G.A.C.; Cerqueira, G.S.; Viana, G.S. Pentoxifylline decreases glycemia levels and TNF-alpha, iNOS and COX-2 expressions in diabetic rat pancreas. Springerplus 2014, 3, 283. [Google Scholar] [CrossRef]
- Salehi, A.; Abaraviciene, S.M.; Jimenez-Feltstrom, J.; Östenson, C.-G.; Efendic, S.; Lundquist, I. Excessive islet NO generation in type 2 diabetic GK rats coincides with abnormal hormone secretion and is counteracted by GLP-1. PLoS ONE 2008, 3, e2165. [Google Scholar]
- Ferreira, L.; Teixeira-de-Lemos, E.; Pinto, F.; Parada, B.; Mega, C.; Vala, H.; Pinto, R.; Garrido, P.; Sereno, J.; Fernandes, R.; et al. Effects of sitagliptin treatment on dysmetabolism, inflammation, and oxidative stress in an animal model of type 2 diabetes (ZDF rat). Mediators Inflamm. 2010, 2010, 592760. [Google Scholar] [CrossRef]
- Bae, E.J. DPP-4 inhibitors in diabetic complications: Role of DPP-4 beyond glucose control. Arch. Pharm. Res. 2016, 39, 1114–1128. [Google Scholar] [CrossRef]
- Lee, Y.-S.; Jun, H.-S. Anti-inflammatory effects of GLP-1-based therapies beyond glucose control. Mediators Inflamm. 2016, 2016, 3094642. [Google Scholar] [CrossRef]
- Govindaraj, J.; Pillai, S.S. Rosmarinic acid modulates the antioxidant status and protects pancreatic tissues from glucolipotoxicity mediated oxidative stress in high-fat diet: Streptozotocin-induced diabetic rats. Mol. Cell. Biochem. 2015, 404, 143–159. [Google Scholar] [CrossRef] [PubMed]
- Pernicova, I.; Korbonits, M. Metformin—Mode of action and clinical implications for diabetes and cancer. Nat. Rev. Endocrinol. 2014, 10, 143. [Google Scholar] [CrossRef] [PubMed]
- Migoya, E.M.; Bergeron, R.; Miller, J.L.; Snyder, R.N.K.; Tanen, M.; Hilliard, D.; Weiss, B.; Larson, P.; Gutierrez, M.; Jiang, G.; et al. Dipeptidyl peptidase-4 inhibitors administered in combination with metformin result in an additive increase in the plasma concentration of active GLP-1. Clin. Pharmacol. Ther. 2010, 88, 801–808. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Hong, T. Combination therapy of dipeptidyl peptidase-4 inhibitors and metformin in type 2 diabetes: Rationale and evidence. Diabetes Obes. Metab. 2014, 16, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Saisho, Y. Metformin and inflammation: Its potential beyond glucose-lowering effect. Endocr. Metab. Immune Disord-Drug Targets 2015, 15, 196–205. [Google Scholar] [CrossRef]
- Shen, T.; Xu, B.; Lei, T.; Chen, L.; Zhang, C.; Ni, Z. Sitagliptin reduces insulin resistance and improves rat liver steatosis via the SIRT1/AMPKα pathway. Exp. Ther. Med. 2018, 16, 3121–3128. [Google Scholar] [CrossRef]
- Rosenstock, J.; Allison, D.; Birkenfeld, A.L.; Blicher, T.M.; Deenadayalan, S.; Jacobsen, J.B.; Davies, M. Effect of additional oral semaglutide vs sitagliptin on glycated hemoglobin in adults with type 2 diabetes uncontrolled with metformin alone or with sulfonylurea: The PIONEER 3 randomized clinical trial. JAMA 2019, 321, 1466–1480. [Google Scholar] [CrossRef]
| Stages | Days | Events | |
|---|---|---|---|
| HFD feeding |  | D0-D21 |
|
| STZ injection | D22 | After overnight fasting of the animals, STZ was injected once intraperitoneally at a dose of 40 mg/kg. | |
| Diabetes mellitus | D32 |
| |
| Initiation of treatment | D32 | All treatment started on the 10th day after STZ injection and continued for 4 consecutive weeks:
| |
| OGTT | D60 | At the end of the treatment period (4 weeks), an oral glucose tolerance test (OGTT) was done. | |
| End of experiment | D60 | At the end of the treatment period (4 weeks) and 8 h after performing the OGTT:
| |
| Groups | Body Weight (g) | Pancreas Weight (g) | Pancreas to Body Weight Ratio (%) | ||
|---|---|---|---|---|---|
| Time (weeks) | Time (weeks) | Time (weeks) | |||
| 0 | 2 | 4 | 4 | 4 | |
| Normal control | 245.15 ± 9.79 | 261.88 ± 9.62 | 296.75 ± 9.08 | 0.800 ± 0.049 | 0.27 ± 0.014 |
| Diabetic | 261.56 ± 8.77 a | 305.52 ± 11.33 a | 341.80 ± 11.27 a | 0.462 ± 0.026 a | 0.14 ± 0.008 a |
| Sitagliptin | 262.22 ± 13.68 a | 282.25 ± 10.58 ab | 318.66 ± 8.97 ab | 0.713 ± 0.411 abd | 0.22 ± 0.017 abd |
| Metformin | 261.91± 11.08 a | 290.51 ± 12.51 ab | 318.40 ± 8.65 ab | 0.497 ± 0.013 ab | 0.16 ± 0.006 ab |
| Combined | 262.74 ± 11.68 a | 279.30 ± 16 ab | 309.20 ± 9.19 abc | 0.802 ± 0.023 bc | 0.26 ± 0.009 bc |
| Groups | Serum Insulin (μU/mL) | HOMA-IR |
|---|---|---|
| Normal control | 13.91 ± 2.33 | 3.90 ± 0.71 |
| Diabetic | 10.44 ± 2.04 a | 7.35 ± 1.49 a |
| Sitagliptin | 10.93 ± 1.86 a | 7.73 ± 1.23 a |
| Metformin | 11.07 ± 1.99 a | 7.42 ± 1.37 a |
| Combined | 10.28 ± 2.01 a | 7.70 ± 1.37 a |
| Groups | Cholesterol (mg/dL) | Triglycerides (mg/dL) | Lipase (U/L) |
|---|---|---|---|
| Normal control | 111.92 ± 5.07 | 64.25 ± 3.40 | 514.50 ± 19.80 |
| Diabetic | 161.80 ± 8.35 a | 138.30 ± 8.63 a | 517.55 ± 19.82 |
| Sitagliptin | 160.70 ± 6.55 a | 137.90 ± 7.48 a | 516.70 ± 16.89 |
| Metformin | 160.43 ± 7.54 a | 137.85 ± 8.33 a | 518 ± 19.64 |
| Combined | 159.96 ± 8.19 a | 137.20 ± 8.35 a | 517.30 ± 14.47 |
| Groups | Cholesterol (mg/dL) | Triglycerides (mg/dL) | Lipase (U/L) |
|---|---|---|---|
| Normal control | 111.31 ± 5.14 | 64.10 ± 3.41 | 515.35 ± 19.90 |
| Diabetic | 161.35 ± 6.68 a | 137.70 ± 8.29 a | 518.05 ± 19.54 |
| Sitagliptin | 119.10 ± 9.68 abc | 71.70 ± 6.44 ab | 516.90 ± 16.96 |
| Metformin | 128.95 ± 10.12 ab | 70.36 ± 5.04 ab | 517.95 ± 18.64 |
| Combined | 113 ± 7.16 bc | 63.67 ± 7.32 bd | 517.23 ± 17.36 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shawky, L.M.; Morsi, A.A.; El Bana, E.; Hanafy, S.M. The Biological Impacts of Sitagliptin on the Pancreas of a Rat Model of Type 2 Diabetes Mellitus: Drug Interactions with Metformin. Biology 2020, 9, 6. https://doi.org/10.3390/biology9010006
Shawky LM, Morsi AA, El Bana E, Hanafy SM. The Biological Impacts of Sitagliptin on the Pancreas of a Rat Model of Type 2 Diabetes Mellitus: Drug Interactions with Metformin. Biology. 2020; 9(1):6. https://doi.org/10.3390/biology9010006
Chicago/Turabian StyleShawky, Lamiaa M., Ahmed A. Morsi, Eman El Bana, and Safaa Masoud Hanafy. 2020. "The Biological Impacts of Sitagliptin on the Pancreas of a Rat Model of Type 2 Diabetes Mellitus: Drug Interactions with Metformin" Biology 9, no. 1: 6. https://doi.org/10.3390/biology9010006
APA StyleShawky, L. M., Morsi, A. A., El Bana, E., & Hanafy, S. M. (2020). The Biological Impacts of Sitagliptin on the Pancreas of a Rat Model of Type 2 Diabetes Mellitus: Drug Interactions with Metformin. Biology, 9(1), 6. https://doi.org/10.3390/biology9010006





