Abstract
In recent years, several studies have examined the potential associations between mitochondrial dysfunction and neurodegenerative diseases such as multiple sclerosis (MS), Parkinson’s disease and Alzheimer’s disease. In MS, neurological disability results from inflammation, demyelination, and ultimately, axonal damage within the central nervous system. The sustained inflammatory phase of the disease leads to ion channel changes and chronic oxidative stress. Several independent investigations have demonstrated mitochondrial respiratory chain deficiency in MS, as well as abnormalities in mitochondrial transport. These processes create an energy imbalance and contribute to a parallel process of progressive neurodegeneration and irreversible disability. The potential roles of mitochondria in neurodegeneration are reviewed. An overview of mitochondrial diseases that may overlap with MS are also discussed, as well as possible therapeutic targets for the treatment of MS and other neurodegenerative conditions.
1. Introduction
Neurodegenerative diseases are characterized by neurologic dysfunction with a progressive course and consequent neuronal death [1]. Although these diseases, including multiple sclerosis, Alzheimer’s disease, and Parkinson’s disease, have different physiopathologies in their onset, they have a similar eventual course of gradual neurological decline and neuronal loss [2].
Multiple sclerosis (MS) is a leading cause of neurologic disability in young adults. MS is characterized by focal areas of demyelination in the white matter of the central nervous system (CNS) with secondary neuroaxonal degeneration [3,4]. The mean age of onset in females is approximately 30, compared to 33 years in males [5]. The sex ratio is 3:1, female to male, though men often progress more quickly and experience more rapid disability accumulation [3].
Among all patients with MS, about 85% present with a relapsing remitting form, which has alternate periods of acute demyelination (relapses) and periods of neurological recovery and stability (RRMS). For most patients, after 15–20 years the disease passes into a secondary progressive course (SPMS) which is characterized by an insidious progression of worsened neurological function with few or no acute relapses [3,4]. The remaining 10–15% of patients progress continuously from the first clinical manifestation of symptoms [4]; this is called the primary progressive form of multiple sclerosis (PPMS) and presents later in life, with a mean age of 45 years. The incidence of this form of the disease is approximately equivalent for men and women [6].
At the pathophysiological level, MS is characterized by two phases: At the initiation of a new lesion, there is a predominance of acute inflammation; subsequently, a state of chronic inflammation ensues with neurodegeneration. During the former, there is penetration of the blood brain barrier by activated immune cells against the myelin sheath. Inflammation in MS is due in part to components of both the innate and adaptive immune systems [7,8]. In brief, there is proliferation and dysregulation of pro-inflammatory T lymphocytes (Th1 and Th 17), as well as activation of B cells and secretion of inflammatory cytokines [9].
Pathognomonic inflammatory events in MS also activate neurodegenerative processes that lead to the destruction of oligodendrocytes, axons, and ultimately, neurons [7,8]. Brain, spinal cord and retinal atrophy are the result of the presence of neurodegeneration even at early stages of MS, meaning that both processes of acute inflammation and neurodegeneration co-exist since the first symptoms of the disease in the gray and white matter [3]. RRMS has a more prominent neuro-inflammatory phenotype, while the SPMS and PPMS forms are largely characterized by neurodegeneration [3].
The current available treatments for MS are directed against the acute episodes of neuroinflammation; this works well to prevent relapse events but is an approach with limited efficacy for protection against neurodegeneration, particularly in progressive forms of the disease [4]. The recent advancements in the understanding of mitochondrial dysfunction in neurodegenerative diseases, and in particular MS, bring new perspectives for future prevention of neuronal loss. We herein review the multifaceted role of mitochondria in MS pathology and the unique genetic factors that may contribute to the disease.
2. Mitochondria and Their Role in Neurodegeneration in Multiple Sclerosis
2.1. Mitochondria
Mitochondria uniquely have dual genomic expression of proteins that originate from both nuclear and mitochondrial DNA (mtDNA) [10]. The multi-copy nature of mitochondria gives rise to the concept of heteroplasmy (when both mutated and wild-type mtDNA molecules coexist in the same cell) and homoplasmy (when only mutant mtDNA molecules are present in the mitochondria of the cell). For a disease to manifest symptoms, the mutated mtDNA molecules in a tissue must increase to a pivotal threshold beyond which oxidative phosphorylation (OXPHOS) is impaired, thereby demonstrating a critical ratio of mutant to wild-type mtDNA [11,12,13]. The mitochondrial genome (5-μm circles, or 16.569 kilobases) is smaller than the nuclear genome, is highly compacted, and has only one DNA polymerase (polymerase γ) without any introns [13,14]. The lack of protective histones facilitates the accumulation of mtDNA mutations in an environment with a high concentration of reactive oxygen species (ROS) [15].
Mitochondria are organelles which are responsible for cellular bioenergetics via the Krebs cycle (with the production of NADH and FADH) and oxidative phosphorylation (OXPHOS), for cellular bioenergetics with secondary ATP production [16,17]. The mitochondria’s main functions in bioenergetics include acting upon the electron transport chain (ETC) on the inner mitochondrial membrane, which is composed by four complexes (complex I, II, III and IV). They are also involved in the sequential reaction of reduction, OXPHOS, and electron flow (derived from NADH and FADH). This causes energy release which is used to transport protons from the matrix to the intermembrane space, creating an electrochemical gradient. ATP synthase (considered the complex V) uses this gradient to phosphorylate ADP to ATP [4].
Mitochondria participate in other crucial cells functions including calcium (Ca2+) storage, cell signaling (proliferation, adaptation to different environments and stress response) and apoptosis [18,19]. Ca2+ storage in mitochondria is involved in the regulation of ion homeostasis, cell signaling, and apoptosis (when prolonged high levels of Ca2+ in plasma concentrations) [20].
Also, important to understanding the potential role of mitochondria in neuronal death is the regulation of mitochondrial outer membrane permeabilization (MOMP). This is well controlled by different mechanisms, and when significant permeation does occur there is an activation of caspases and a release of pro-apoptotic factors into the cytosol, initiating the apoptosis-cascade [21,22,23,24,25,26].
2.2. Inflammation and Glia in Multiple Sclerosis
During acute events of inflammation, immune cells (mainly CD4+ T helper lymphocytes and also CD8+ T cells) cross the blood–brain barrier (BBB) and B cells and monocytes are activated. The primary target in MS is the myelin sheath of CNS white matter, though in recent years there has been growing evidence of direct attack against cortical and deep gray matter [27]. The release of pro-inflammatory cytokines (e.g., IL-17, IL-4, IL-10, TNF-α), activation of microglia and macrophages with the release of toxic substances such as reactive oxygen species (ROS), tumor necrosis factor, reactive nitrogen species (RNS), and glutamate [28] further damage the myelin. Enzymes involved in this neuroinflammation include myeloperoxidase, xanthine, NADPH oxidases (responsible for neuronal injury) [29,30], excitotoxins, cytotoxic cytokines, proteases and, lipases [31].
The damaged BBB subsequently becomes increasingly permeable, allowing further migration of immune cells leading to the formation of plaques of focal demyelination [32,33]. Focal plaques may converge, forming confluent demyelinated areas in both the white and grey matter [34]. The lymphocytic neuroinflammation process that characterizes the acute phase of the disease leads not only to the damage of myelin fibers synthesized by oligodendrocytes, but also to the death of the oligodendrocytes. The combination of demyelination and loss of trophic stimuli of oligodendrocytes then progresses to axonal degeneration, axon and neuron death with permanent neurologic disability [35]. Remyelination, if it occurs, is often only partial and astrocytes form sclerotic glial scars in the damaged white matter [36]. Chronic inflammation is also responsible for cumulative oxidation of phospholipids and DNA strand breaks [37].
In multiple sclerosis, there is also production of intrathecal, oligoclonal IgG and IgM. Although investigated extensively, no clear antigenic pattern identifying a specific potential trigger for MS has been found in studying these CSF antibodies. In SPMS there are also “meningeal lymphoid-like structures” that correlate with the pathology of the gray matter [38].
2.3. Neurodegeneration in Multiple Sclerosis and Evidence for Mitochondrial Involvement
Historically, the neurodegeneration of MS was understood as a sequential process following chronic neuroinflammation, but some evidence suggests that the neurodegenerative component is already present during the initial clinical manifestations of the disease [3]. The number of relapses in RRMS does not correlate with the probability or latency of progression of SPMS [39]. Tissue atrophy is considered an imaging marker of neurodegeneration in MS, and cerebral, spinal, and retinal atrophy have been reported to be present at the first clinical manifestations of RRMS, affecting both white and gray matter [40,41,42]. The accepted explanation for this observation is that neuroinflammation is followed by a failure in the process of remyelination, axonal damage and Wallerian degeneration [42]. Normal appearing white matter (NAWM), with normal macroscopic appearance and microscopically normal myelination, has a decreased density of axons; this is, in part justified by Wallerian degeneration, but also indicates more widespread early damage than captured by routine MRI [43,44,45,46,47,48]. Neuropathological findings from brain tissue blocks of MS patients show evidence of gray matter lesions (axonal and dendritic transection, apoptotic neurons and demyelinated cortical plaques) [49] present from the time of initial disease onset; this is, particularly prominent in SPMS and PPMS.
The chronic neuro-inflammatory stimuli of MS disrupt neuro-axonal hemostasis, leading to a simultaneous increase in oxidative stress, marked by a rise in ROS, and secondary damage to mitochondria and macromolecules (mtDNA, proteins from ETC, lipids). Excitotoxicity and an imbalance of neurotrophic substances for neurons and oligodendrocytes occurs [3,50,51]. This damage impairs mitochondrial function (below described), which further increases ROS production in a vicious cycle [4]. The result is a reduction in the efficiency of energy production, creating an imbalance between energy generation and consumption. The final result is an environment with a failure to provide required levels of energy within the demyelinated axons, and after reduced ATP production reaches a critical point there is an imbalance in ionic homeostasis leading to activation of apoptosis mechanisms [52,53].
Of relevance to understanding the pathology of MS, the central nervous system (CNS) has increased susceptibility to oxidative damage because of the high metabolic rate (consumption of oxygen) of neurons and the rich composition of polyunsaturated fatty acids in CNS cells [54]. Furthermore, mitochondria influence the differentiation of oligodendroglial cells through overexpression of mitochondrial transcripts and mtDNA [55]. An environment of oxidative stress reduces the expression of these transcripts involved with oligodendrocyte differentiation [56]. Double strand breaks in mtDNA have been shown to cause an oligodendropathy and exaggerated injury responses in an animal model of MS [57]. Additional observations have demonstrated a potential direct link between mitochondrial dysfunction and oligodendrocyte myelination. N-acetyl aspartate (NAA), is a mitochondrial metabolite and also an indirect oligodendrocyte substrate for the production of myelin (after breakdown into acetate and aspartate). A lack in the availability of NAA, from damaged mitochondria, was associated with lower levels of acetate in the cortex (parietal and motor) in postmortem tissue from patients with MS [58].
Though they are often overridden and unable to counter the stress burden, there are compensatory mechanisms to counter these mitochondria-related degenerative processes. The body has intrinsic mechanisms of self-protection against ROS, including nuclear factor erythroid 2related factor 2 (NRF2) and antioxidant enzymes such as heme oxygenase 1 (HMOX1) which are activated during periods of hypoxic stress [59]. But after a critical point in the reduction in ATP production, an imbalance in ionic homeostasis occurs, leading to the activation of apoptosis mechanisms mediated by ions (Ca2+ dependent proteases) in those axons with chronic inflammation and demyelination [60].
2.3.1. Human Studies of Mitochondria Function in Multiple Sclerosis
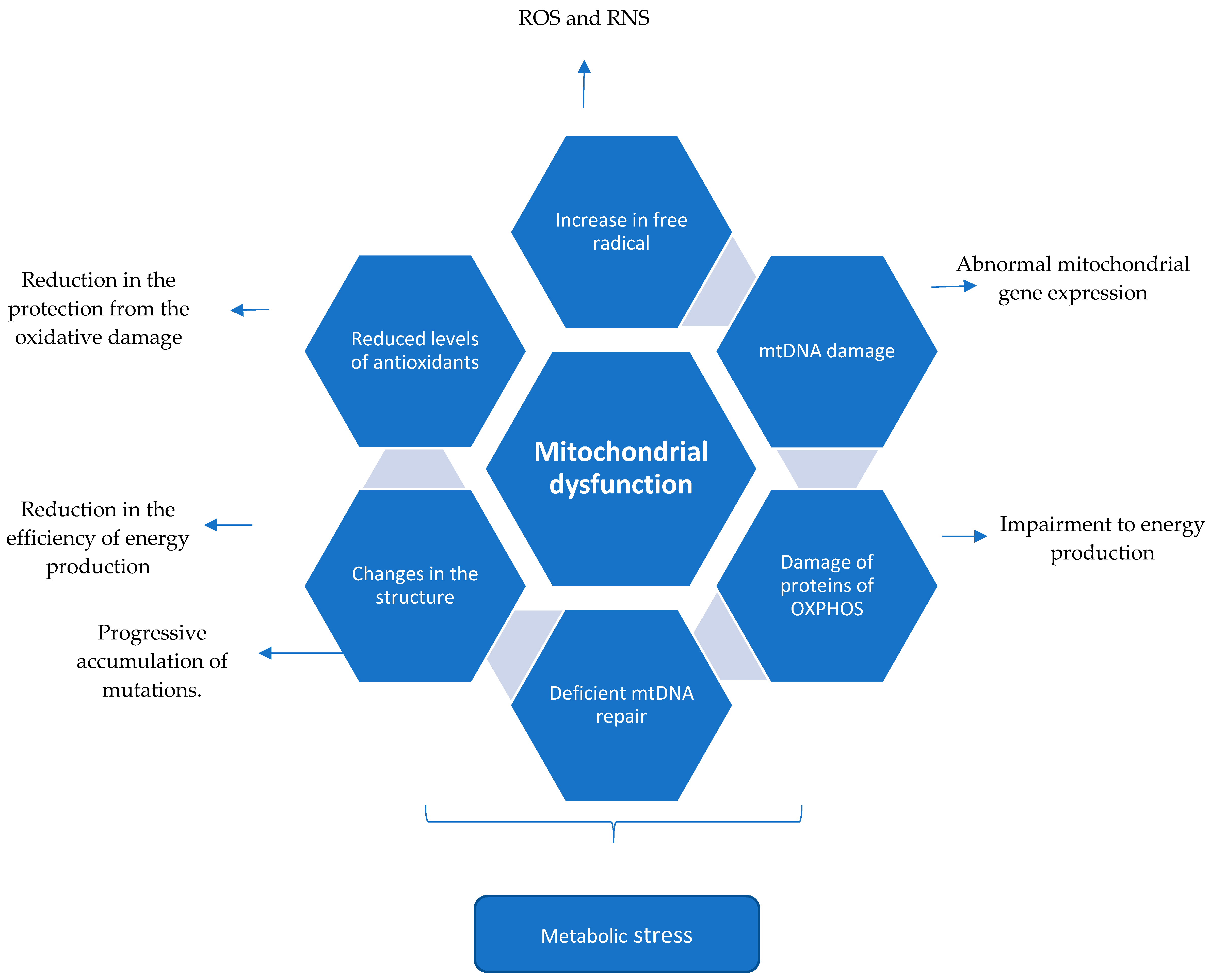
Multiple human studies have demonstrated evidence of mitochondrial dysfunction in MS patients (Figure 1, Table 1). One publication compared 10 post mortem brains of patients with MS (n = 9 SPMS and n = 1 PPMS) to healthy controls paired for age and sex. The MS cortex exhibited distinctive levels of both mtDNA transcripts (488 decreased and 67 increased compared to controls), and nuclear mitochondrial DNA transcripts (26 decreased transcripts). In a study of function in the same samples there was a decrease in complex I and III activity from the neurons of motor cortex in MS patients, and a decrease in GABAergic synaptic components [52]. Another study of thirteen patients with MS (SPMS) identified large mtDNA deletions in neurons, with some showing specific deletions in the subunits of complex IV [59].
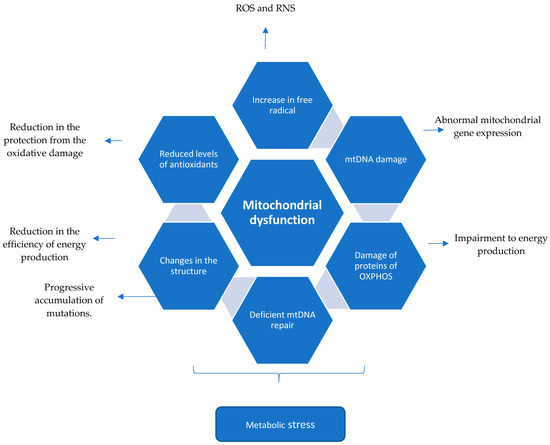
Figure 1.
Mitochondrial dysfunction described in the literature associated with Multiple Sclerosis. Chronic neuroinflammation leading to mitochondrial dysfunction.

Table 1.
Evidence of mitochondrial involvement in Progressive Forms of Multiple Sclerosis compared to Controls or RRMS.
Additionally, reports of a decrease in PGC-1α levels (a transcriptional co-activator and regulator of mitochondrial function) in pyramidal neurons of MS patients (7 SPMS, 7 PPMS and 1 subtype not determined) was associated with reduced expression of mitochondrial machinery components (OXPHOS subunits, antioxidants and uncoupling proteins 4 and 5). This finding was confirmed in a functional model (with neuronal cells) showing association of these changes with more ROS production [60]. Another publication reported that increases in ROS affect the ability of NRF-2 (a transcription factor for ETC proteins) to bind promotors, even in apparently normal areas of gray matter cortex of SPMS patients [61]. Higher ROS production in the CNS of progressive MS patients (14 SPMS, 5 PPMS and 7 subtypes not determined) has also been associated with a rise in the number of mitochondria in axon and astrotcytes. Increased ROS is also associated with the translation of mitochondrial proteins in active and chronic inactive MS lesions, including elevated expression of proteins from the mitochondrial ETC complex IV and higher levels of a heat shock protein (mtHSP70) compared to the brain of controls. The mtHSP70 protein is a marker of mitochondrial stress [62]. A recent publication found in fronto-parietal areas decreased levels of the potent antioxidant, glutathione (GSH), in PPMS and SPMS compared with RRMS and controls, suggesting that oxidative stress affects the neurodegeneration phase more than the neuroinflammatory phase [63]. Another study compared the mitochondrial proteome from the brains of MS (eight SPMS) patients and controls. The findings showed different patterns by mass spectrometry in levels of human cytochrome c oxidase subunit 5b (COX5b), the brain-specific creatine kinase isoform, and the β-chain of hemoglobin between groups [64].
2.3.2. Neurodegeneration in Multiple Sclerosis Animal Models
There have been many attempts to reproduce the spectrum of inflammation (acute and chronic), demyelination/remyelination, and neurodegeneration that characterize the different clinical syndromes (PP, SP, RR) of the disease. There is no single experimental model that fully covers the spectrum of pathology in human MS. Each model available has strengths for certain questions, but without completely recapitulating all of the mitochondrial deficiencies in MS [67]. In trial design it is important to focus on the mechanism of the potential drug and choose the animal model in which it is possible to induce the disease process of interest [67,68].
In one of the most commonly used models for MS, experimental autoimmune encephalomyelitis (EAE), there are morphology changes in the mitochondria (swelling) [69], early mitochondrial dysfunction even in normal appearing white matter [70], and impairment of mitochondrial and axonal depolarization [71]. Some of the mitochondrial damage can be rescued with specific interventions such as gene therapy for expressing complex I ETC proteins [72,73] and antioxidant cocktails [74,75]. In a myelin basic protein (MBP) knockout, considered a model for the chronic demyelination of MS, there were increased numbers of mitochondria observed by electron microscopy. Additionally, there was a two-fold increase in the cytochrome c staining in the white matter, showing mitochondrial changes associated with cases of reduction in myelin [76]. A summary of previous animal models’ findings regarding the association of mitochondrial involvement in multiple sclerosis is presented in Table 2.

Table 2.
Mouse models to study multiple sclerosis [77].
2.4. Summary (Mechanism of Mitochondrial Dysfunction Perpetuating the CNS Injury in Multiple Sclerosis)
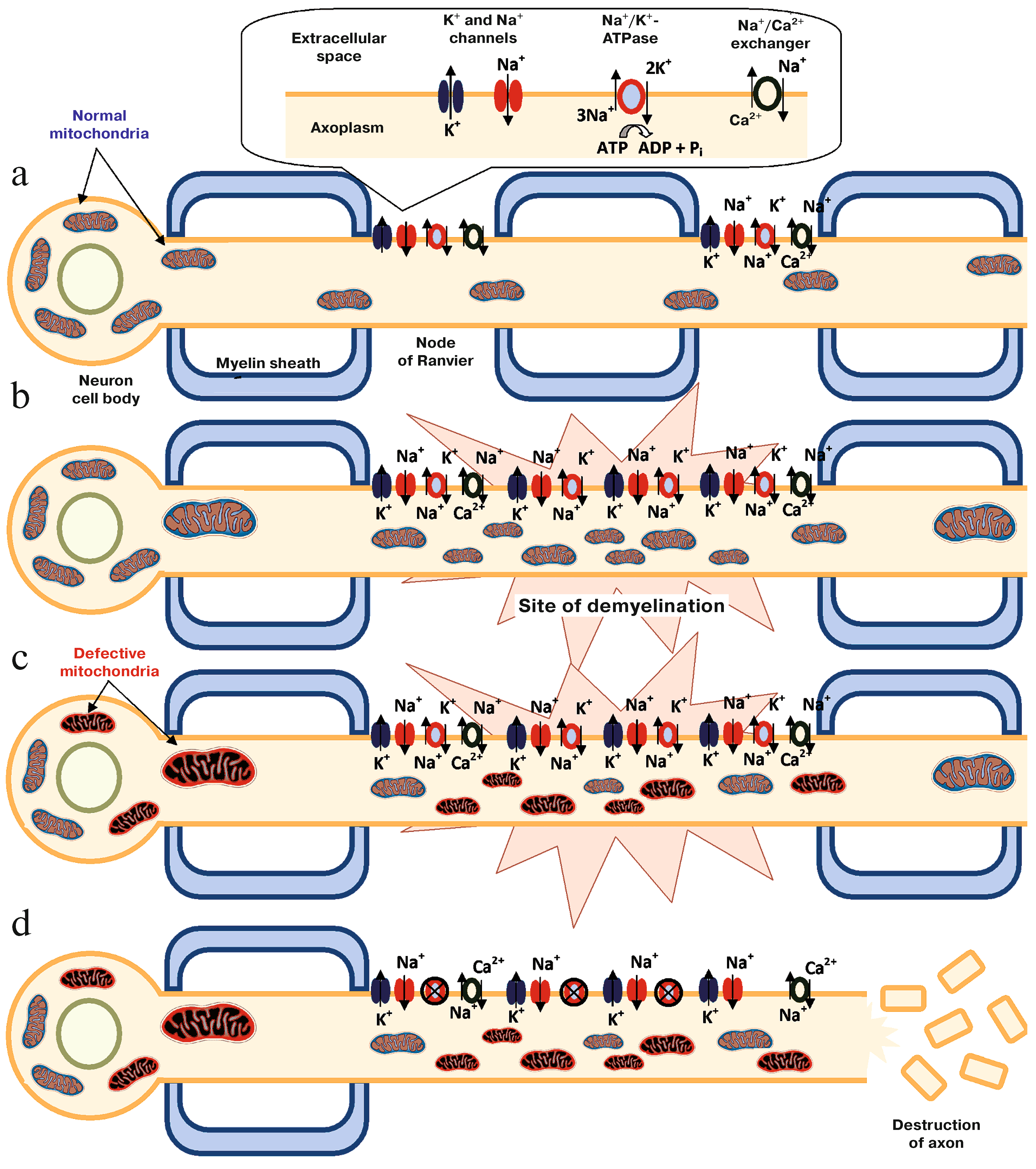
The brain has a high metabolic rate and consumes 20% of the total energy produced in the human body, which is mainly utilized in neurotransmission (more than half of that consumed to maintain the ionic equilibrium and the membrane potential) and the axoplasmic flow (to conduct nerve impulses); these functions depend substantially on mitochondria machinery [4,85]. The neurologic signal transmission is due to propagation of the membrane depolarization through the neuron, and the electrochemical gradient is created by the Na+/K+-ATPase, allocated in the nodes of Ranvier. Oligodendrocytes are not only responsible for the myelin sheath but also release lactate for the neuron as energy supply. With the chronic inflammation and myelin destruction, there is redistribution of the ion channels. Consequently, there is more ATP consumption by the increased number of Na+/K+-ATPase. With the purpose of balancing the ratio and demand for energy, mitochondria begin compensatory modifications (increasing in number and size, changing the localization in the neuron and its morphology). In parallel, the chronic inflammation creates an environment of oxidative stress secondary to ROS release by macrophages and the microglia and increases in glutamate released in response to neuronal damage. TNF-α damages the OXPHOS process through Ca++ regulated mechanisms [86]. With mitochondrial progressive accumulative damage (mtDNA alteration and increased heteroplasmy, OXPHOSP subunits dysfunction, alteration in proteins that regulates the migration of the organelle from neuron body to the axon) significant impairment in energy production develops. [51]. If ATP production is compromised, the Na+/K+-ATPase is not able to keep the gradient after an action potential, which leads to Na+ accumulation in the neuron cytoplasm. This forces the Na+/Ca2+ channel to transfer Ca2+ inside the cell, activating the Ca2+ apoptosis-depend-cascade, which results in neuron death, Wallerian degeneration and irreversible neurologic dysfunction [34,53,65,66,86,87,88,89]. This process is represented in Figure 2. The progressive degenerative process initiated in the axon can continue to the neuron body and dendrites, also reaching presynaptic and postsynaptic neurons [34], chronic failure to provide energy to the tissue increases the oxidative stress in a vicious cycle that increases mitochondrial damage [51].
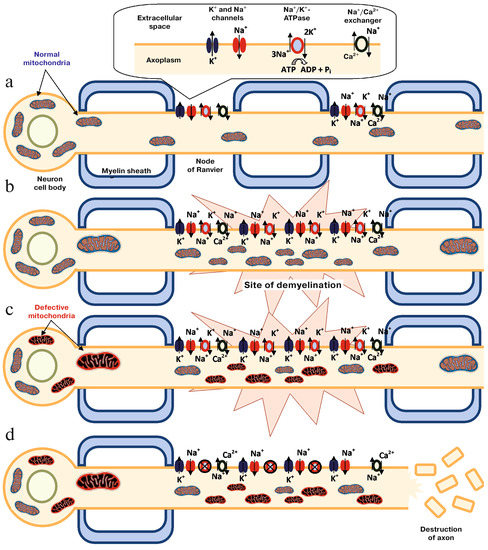
Figure 2.
The role of mitochondria in the process of neurodegeneration. a. Normal nerve. b. Site of demyelination with secondary modification of the distribution of ion channels in the nerve. c. Structural and functional modification in mitochondria caused by oxidative stress. d. Cascade of apoptosis activated by Ca2+. Figure reprinted with permission from the article “Involvement of Mitochondria in Neurodegeneration in Multiple Sclerosis”, Kozin et al., Biochemistry (Moscow), 2018, Vol. 83, No. 7, pp. 813–830 [4].
Important to mention is that mitochondrial DNA damage is amplified during the process of expansion of the clones (with deletions or mutations), changing the levels of heteroplasmy of the tissue [51,59]. This process increases the failure to provide appropriate energy supply for the tissue, contributing to the death of the cells [90].
3. Mitochondrial Mutations in Multiple Sclerosis and Overlapping Diseases
3.1. Mitochondrial Mutations and Multiple Sclerosis Risk
The current consensus is that MS is a multifactorial disease, with 25% of the risk related to heritable factors [91]. The important role of the class II region of the human leukocyte antigen (HLA) gene cluster has been well recognized for several decades. There are now over 100 loci identified in the HLA region found to be associated with susceptibility and over 200 in non-HLA loci [92]. Several single site mutations in mtDNA have been reported to increase the risk of MS, including the mtDNA nt13708A [93] and mtDNA T4216C [94] variants. A large consortium study by Tranah et al. examined mitochondrial DNA sequence variation and MS risk. In the discovery dataset they compared over 7000 MS cases and over 14,000 controls from seven countries. Haplotype group and more than 100 common mtDNA mutations were evaluated. While they reported an elevated risk of MS (OR 1.15, p = 0002) among haplotype JT carriers, they found no associations between common mtDNA mutations and MS risk [95].
3.2. Leber’s Hereditary Optic Neuropathy
Leber’s hereditary optic neuropathy (LHON) is a mitochondrial disease resulting in severe bilateral optic neuropathy, characterized by central vision loss and dyschromatopsia. There is degeneration of the retinal ganglion cells (RGC) and axonal tracts of the optic nerve. There are numerous mitochondrial mutations associated with LHON, but the vast majority of patients have one of three different mitochondrial mutations at nucleotides 3460, 11778 and 14484. The mutations are single amino acid substitutions in one of the mitochondrially encoded subunits of NADH: ubiquinone oxidoreductase, complex I of the electron transport chain (ETC). There is some evidence suggesting that the exposure to high nitric oxide concentrations could impair in vivo the ability to cope with the oxidative stress caused by the genetic defect, thereby driving the pathology in LHON. This was described by Flabella et al. in one patient carrying the 11788/ND4 mutation [96]. This same increase in ROS was described in MS as previously discussed [3,50,51].
Males are more frequently affected, and there is incomplete penetrance seen in LHON families [97]. There is a modest epidemiological overlap between MS and LHON, with a subset of patients developing both diseases (Table 3). Harding first described this association in 1992 in case studies of eight women with matrilineal relatives with LHON who presented with optic neuritis; six of the eight progressed to clinical MS with neurologic symptoms. Seven of the eight also had characteristic white matter lesions on MRI [98]. Since Harding’s first report of the association of LHON and MS this relationship has continued to be observed with females being predominantly affected at a ratio of more than two to one [99]. In one review the incidence of demyelination among LHON affected persons was up to five percent, which is fifty times greater than the prevalence of MS in the general population [100]. RGC thinning is also noted in MS. While the exact pathophysiology may be different in LHON and MS, the mitochondrial dysfunction in LHON may be instructive to the understanding of mitochondria’s role in MS.

Table 3.
Associations between MS and mitochondrial diseases.
3.3. Dominant Optic Atrophy and OPA1 Mutations
An additional example of potential overlap between mitochondrial genetic optic atrophy and MS has been described by Yu-Wai-Man et al. in a paper detailing three cases of MS-like disease associated with OPA1 mutations (Table 3). OPA1 mutations have previously been discussed in the literature in association with autosomal dominant optic atrophy (DOA), the most common inherited form of optic nerve visual loss. OPA1 has multiple roles in mitochondrial function as it encodes for an inner mitochondrial membrane protein, and is involved in respiratory chain complexes, cytochrome c molecules, and fusion/fission balance. There are over 90 known gene mutations (substitutions, deletions and insertions) associated with OPA1 mutations and thought to be due to a truncated protein [101]. Like LHON, DOA is a mitochondrial determined optic neuropathy preferentially affecting the ganglion cells within the inner retina. The exact relationship between OPA1 proteins and MS has yet to be clearly elucidated, with only the above few cases being reported.
3.4. POLG1 Mutations
The mitochondrial gene POLG1 is the larger catalytic subunit of polymerase gamma which is the only known DNA polymerase active in human mitochondria. POLG1 mutations have been implicated in a number of mitochondrial disorders and more recently have also been identified in several cases of demyelination. Two cases of non-related individuals with novel POLG1 mutations who had optic neuritis and white matter lesions consistent with clinical MS were reported in the literature. Of note both of these patients progressed into a more classic POLG1 phenotype with bilateral ophthalmoplegia, ptosis, myopathy, cardiomyopathy, ataxia, dysphagia, and hearing and cognitive impairment. These patients also had muscle biopsies showing red ragged fibers [99,102]. Therefore, their progression calls into question whether or not they truly had MS or if their initial presentations were instead MS mimics. Clearly more research is needed. Yet it is important to consider these cases as they may offer further evidence of the role of the mitochondria within MS and MS-like disease processes. Further research may lead to the discovery of more MS patients with mitochondrial mutations.
4. Potential Therapies and Targets
The treatment of most mitochondrial diseases is still largely supportive at this time, although some therapies have been tried such as vitamins, co-enzymes, creatine, free radical scavengers and hyperbaric oxygen treatments. Despite the widespread use of a multitude of co-enzymes and vitamin supplements there is currently limited evidence that these are effective in the treatment of primary mitochondrial disorders. For targeted treatment of MS the use of alpha lipoic acid and co-enzyme Q10 are being investigated. A randomized controlled phase 2 trial of alpha lipoic acid (ALA) versus placebo was studied in SPMS and found to slow whole brain atrophy [103]; further studies are ongoing. Other studies are examining a synthetic analogue of co-enzyme Q10, idebenone, which is being targeted for treatment of neurodegenerative disorders such as LHON [99]. Phase I/II trials of idebonone in PPMS demonstrated safety but initial data showed no change in progression of the disease (http://www.santhera.com/assets/files/press-releases/2018-03-05_PR_PPMS_e_final.pdf). An expansion study is ongoing with completion planned for later this year (https://www.clinicaltrials.gov/ct2/show/NCT01854359). In addition to these targets there are several other potential approaches for mitochondrial based therapy and limiting neurodegeneration in MS.
4.1. Mitochondrial Metabolism and Chronic Neuroinflammation
Neurodegeneration is in part driven by the activation of mononuclear phagocytes. When mononuclear phagocytes are persistently activated it can lead to a state of chronic neuroinflammation. Mitochondrial metabolism has a role in the inflammation cascade and targeting the metabolism of innate immune cells may be of benefit. Future studies may address this relationship to aid in the development of novel molecular and cellular therapies that could disrupt the state of chronic neuroinflammation as a way of preventing secondary neurologic damage [104]. Therapies that support cellular metabolism such as high dose biotin, iron and vitamin D have been proposed as possible treatment therapies in progressive MS, and studies looking at each of these treatments are ongoing (https://clinicaltrials.gov). The pilot studies of high dose biotin are encouraging and results suggest both a reduction in disease progression as well as decreased disability in PPMS [105]. Furthermore, these therapies may also have a role in preventing progression of RRMS to SPMS [50].
4.2. Gene Therapy
Gene therapies are being developed in mitochondrial disorders, though most are still in early phases of development. In vivo studies in mice using several vectors have been promising in some disease models such as LHON [106]. Gene Therapy GS010 was shown to be safe in LHON patients carrying the G11778A mutation in a phase 1/2 clinical trial (https://clinicaltrials.gov/ct2/show/NCT02064569). Although the results did not have sufficient power to definitively demonstrate efficacy, 6/14 patients who received GS010 had visual acuity improvements [107]. While these early results in LHON do not immediately translate to MS care, the suggestion of treatment effect is promising for the future of gene therapy in this field of mitochondrial dysfunction.
5. Conclusions
There is compelling data to suggest an important role for mitochondria in the pathophysiology of MS. Further work is needed to move from studies of association to understanding causal relationships between failure of mitochondrial function and MS phenotype. Targeting energy failure and mitochondrial dysfunction is a novel potential therapeutic approach for the challenging progressive phase of MS. Trials are already underway to begin exploring these pathways as treatment targets, including studies of biotin and alpha lipoic acid in progressive MS.
Funding
I.P.d.B. is recipient of a postdoctoral fellowship from the North American Mitochondrial Disease Consortium (NAMDC) supported by National Institute of Health (NIH) U54 grant NS078059.
Conflicts of Interest
The authors declare no conflict of interest related to the content of this manuscript.
References
- Rafael, H. Omental transplantation for neurodegenerative diseases. Am. J. Neurodegener. Dis. 2014, 3, 50–63. [Google Scholar] [PubMed]
- Burnside, S.W.; Hardingham, G.E. Transcriptional regulators of redox balance and other homeostatic processes with the potential to alter neurodegenerative disease trajectory. Biochem. Soc. Trans. 2017, 45, 1295–1303. [Google Scholar] [CrossRef]
- Friese, M.A.; Schattling, B.; Fugger, L. Mechanisms of neurodegeneration and axonal dysfunction in multiple sclerosis. Nat. Rev. Neurol. 2014, 10, 225–238. [Google Scholar] [CrossRef] [PubMed]
- Kozin, M.S.; Kulakova, O.G.; Favorova, O.O. Involvement of Mitochondria in Neurodegeneration in Multiple Sclerosis. Biochemistry (Mosc) 2018, 83, 813–830. [Google Scholar] [CrossRef]
- Ahlgren, C.; Oden, A.; Lycke, J. High nationwide incidence of multiple sclerosis in Sweden. PLoS ONE 2014, 9, e108599. [Google Scholar] [CrossRef]
- Koch, M.; Kingwell, E.; Rieckmann, P.; Tremlett, H. The natural history of primary progressive multiple sclerosis. Neurology 2009, 73, 1996–2002. [Google Scholar] [CrossRef] [PubMed]
- Steinman, L. Multiple sclerosis: A two-stage disease. Nat. Immunol. 2001, 2, 762–764. [Google Scholar] [CrossRef]
- Ellwardt, E.; Zipp, F. Molecular mechanisms linking neuroinflammation and neurodegeneration in MS. Exp. Neurol. 2014, 262 Pt A, 8–17. [Google Scholar] [CrossRef]
- Sospedra, M.; Martin, R. Immunology of multiple sclerosis. Annu. Rev. Immunol. 2005, 23, 683–747. [Google Scholar] [CrossRef]
- Haas, R.H.; Zolkipli, Z. Mitochondrial disorders affecting the nervous system. Semin. Neurol. 2014, 34, 321–340. [Google Scholar] [PubMed]
- Pitceathly, R.D.; McFarland, R. Mitochondrial myopathies in adults and children: Management and therapy development. Curr. Opin. Neurol. 2014, 27, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, A.M.; Taylor, R.W.; Turnbull, D.M.; Chinnery, P.F. The epidemiology of mitochondrial disorders--past, present and future. Biochim. Biophys. Acta 2004, 1659, 115–120. [Google Scholar] [CrossRef]
- Mazunin, I.O.; Volod’ko, N.V.; Starikovskaia, E.B.; Sukernik, R.I. Mitochondrial genome and human mitochondrial diseases. Mol. Biol. (Mosk) 2010, 44, 755–772. [Google Scholar] [CrossRef]
- Holt, I.J.; Reyes, A. Human mitochondrial DNA replication. Cold Spring Harb. Perspect. Biol. 2012, 4, 12. [Google Scholar] [CrossRef]
- Wallace, D.C.; Fan, W.; Procaccio, V. Mitochondrial energetics and therapeutics. Annu. Rev. Pathol. 2010, 5, 297–348. [Google Scholar] [CrossRef]
- Dyall, S.D.; Brown, M.T.; Johnson, P.J. Ancient invasions: From endosymbionts to organelles. Science 2004, 304, 253–257. [Google Scholar] [CrossRef]
- Emes, R.D. The Logic of Evolution: Review of the Logic of Chance by Eugene V. Koonin. Front. Genet. 2012, 3, 135. [Google Scholar] [CrossRef][Green Version]
- Hunt, R.J.; Bateman, J.M. Mitochondrial retrograde signaling in the nervous system. FEBS Lett. 2017, 592, 663–678. [Google Scholar] [CrossRef]
- Mitra, K. Mitochondrial fission-fusion as an emerging key regulator of cell proliferation and differentiation. Bioessays 2013, 35, 955–964. [Google Scholar] [CrossRef]
- Glancy, B.; Balaban, R.S. Role of mitochondrial Ca2+ in the regulation of cellular energetics. Biochemistry 2012, 51, 2959–2973. [Google Scholar] [CrossRef]
- Suhaili, S.H.; Karimian, H.; Stellato, M.; Lee, T.H.; Aguilar, M.I. Mitochondrial outer membrane permeabilization: A focus on the role of mitochondrial membrane structural organization. Biophys. Rev. 2017, 9, 443–457. [Google Scholar] [CrossRef] [PubMed]
- Zamzami, N.; Kroemer, G. The mitochondrion in apoptosis: How Pandora’s box opens. Nat. Rev. Mol. Cell Biol. 2001, 2, 67–71. [Google Scholar] [CrossRef]
- Tait, S.W.; Green, D.R. Mitochondria and cell death: Outer membrane permeabilization and beyond. Nat. Rev. Mol. Cell Biol. 2010, 11, 621–632. [Google Scholar] [CrossRef]
- Walle, L.V.; Lamkanfi, M.; Vandenabeele, P. The mitochondrial serine protease HtrA2/Omi: An overview. Cell Death Differ. 2008, 15, 453–460. [Google Scholar] [CrossRef]
- Ding, Z.J.; Chen, X.; Tang, X.X.; Wang, X.; Song, Y.L.; Chen, X.D.; Wang, J.; Wang, R.F.; Mi, W.J.; Chen, F.Q.; et al. Apoptosis-inducing factor and calpain upregulation in glutamate-induced injury of rat spiral ganglion neurons. Mol. Med. Rep. 2015, 12, 1685–1692. [Google Scholar] [CrossRef][Green Version]
- Jang, D.S.; Penthala, N.R.; Apostolov, E.O.; Wang, X.; Crooks, P.A.; Basnakian, A.G. Novel cytoprotective inhibitors for apoptotic endonuclease G. DNA Cell Biol. 2015, 34, 92–100. [Google Scholar] [CrossRef]
- Von Budingen, H.C.; Bar-Or, A.; Zamvil, S.S. B cells in multiple sclerosis: Connecting the dots. Curr. Opin. Immunol. 2011, 23, 713–720. [Google Scholar] [CrossRef]
- Cunningham, C. Microglia and neurodegeneration: The role of systemic inflammation. Glia 2013, 61, 71–90. [Google Scholar] [CrossRef] [PubMed]
- Gray, E.; Thomas, T.L.; Betmouni, S.; Scolding, N.; Love, S. Elevated activity and microglial expression of myeloperoxidase in demyelinated cerebral cortex in multiple sclerosis. Brain Pathol. 2008, 18, 86–95. [Google Scholar] [CrossRef]
- Fischer, M.T.; Sharma, R.; Lim, J.L.; Haider, L.; Frischer, J.M.; Drexhage, J.; Mahad, D.; Bradl, M.; van Horssen, J.; Lassmann, H. NADPH oxidase expression in active multiple sclerosis lesions in relation to oxidative tissue damage and mitochondrial injury. Brain 2012, 135, 886–899. [Google Scholar] [CrossRef]
- Lassmann, H. Models of multiple sclerosis: New insights into pathophysiology and repair. Curr. Opin. Neurol. 2008, 21, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Bjartmar, C.; Wujek, J.R.; Trapp, B.D. Axonal loss in the pathology of MS: Consequences for understanding the progressive phase of the disease. J. Neurol. Sci. 2003, 206, 165–171. [Google Scholar] [CrossRef]
- Bruck, W. The pathology of multiple sclerosis is the result of focal inflammatory demyelination with axonal damage. J. Neurol. 2005, 252 (Suppl. 5), v3–v9. [Google Scholar] [CrossRef] [PubMed]
- Dendrou, C.A.; Fugger, L.; Friese, M.A. Immunopathology of multiple sclerosis. Nat. Rev. Immunol. 2015, 15, 545–558. [Google Scholar] [CrossRef] [PubMed]
- Fünfschilling, U.; Supplie, L.M.; Mahad, D.; Boretius, S.; Saab, A.S.; Edgar, J.; Brinkmann, B.G.; Kassmann, C.M.; Tzvetanova, I.D.; Möbius, W.; et al. Glycolytic oligodendrocytes maintain myelin and long-term axonal integrity. Nature 2012, 485, 517–521. [Google Scholar] [CrossRef] [PubMed]
- Popescu, B.F.; Lucchinetti, C.F. Pathology of demyelinating diseases. Annu. Rev. Pathol. 2012, 7, 185–217. [Google Scholar] [CrossRef] [PubMed]
- Fischer, M.T.; Wimmer, I.; Höftberger, R.; Gerlach, S.; Haider, L.; Zrzavy, T.; Hametner, S.; Mahad, D.; Binder, C.J.; Krumbholz, M.; et al. Disease-specific molecular events in cortical multiple sclerosis lesions. Brain 2013, 136, 1799–1815. [Google Scholar] [CrossRef]
- Howell, O.W.; Reeves, C.A.; Nicholas, R.; Carassiti, D.; Radotra, B.; Gentleman, S.M.; Serafini, B.; Aloisi, F.; Roncaroli, F.; Magliozzi, R.; et al. Meningeal inflammation is widespread and linked to cortical pathology in multiple sclerosis. Brain 2011, 134, 2755–2771. [Google Scholar] [CrossRef]
- Scalfari, A.; Neuhaus, A.; Daumer, M.; Deluca, G.C.; Muraro, P.A.; Ebers, G.C. Early relapses, onset of progression, and late outcome in multiple sclerosis. JAMA Neurol. 2013, 70, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Barkhof, F.; Calabresi, P.A.; Miller, D.H.; Reingold, S.C. Imaging outcomes for neuroprotection and repair in multiple sclerosis trials. Nat. Rev. Neurol. 2009, 5, 256–266. [Google Scholar] [CrossRef]
- Chard, D.T.; Griffin, C.M.; Parker, G.J.; Kapoor, R.; Thompson, A.J.; Miller, D.H. Brain atrophy in clinically early relapsing-remitting multiple sclerosis. Brain 2002, 125, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.H.; Barkhof, F.; Frank, J.A.; Parker, G.J.; Thompson, A.J. Measurement of atrophy in multiple sclerosis: Pathological basis, methodological aspects and clinical relevance. Brain 2002, 125, 1676–1695. [Google Scholar] [CrossRef] [PubMed]
- Frischer, J.M.; Bramow, S.; Dal-Bianco, A.; Lucchinetti, C.F.; Rauschka, H.; Schmidbauer, M.; Laursen, H.; Sorensen, P.S.; Lassmann, H. The relation between inflammation and neurodegeneration in multiple sclerosis brains. Brain 2009, 132, 1175–1189. [Google Scholar] [CrossRef] [PubMed]
- Kornek, B.; Storch, M.K.; Weissert, R.; Wallstroem, E.; Stefferl, A.; Olsson, T.; Linington, C.; Schmidbauer, M.; Lassmann, H. Multiple sclerosis and chronic autoimmune encephalomyelitis: A comparative quantitative study of axonal injury in active, inactive, and remyelinated lesions. Am. J. Pathol. 2000, 157, 267–276. [Google Scholar] [CrossRef]
- Kutzelnigg, A.; Lucchinetti, C.F.; Stadelmann, C.; Brück, W.; Rauschka, H.; Bergmann, M.; Schmidbauer, M.; Parisi, J.E.; Lassmann, H. Cortical demyelination and diffuse white matter injury in multiple sclerosis. Brain 2005, 128, 2705–2712. [Google Scholar] [CrossRef] [PubMed]
- DeLuca, G.C.; Ebers, G.C.; Esiri, M.M. Axonal loss in multiple sclerosis: A pathological survey of the corticospinal and sensory tracts. Brain 2004, 127, 1009–1018. [Google Scholar] [CrossRef]
- Bitsch, A.; Schuchardt, J.; Bunkowski, S.; Kuhlmann, T.; Bruck, W. Acute axonal injury in multiple sclerosis. Correlation with demyelination and inflammation. Brain 2000, 123 Pt 6, 1174–1183. [Google Scholar] [CrossRef]
- DeLuca, G.C.; Williams, K.; Evangelou, N.; Ebers, G.C.; Esiri, M.M. The contribution of demyelination to axonal loss in multiple sclerosis. Brain 2006, 129 Pt 6, 1507–1516. [Google Scholar] [CrossRef]
- Peterson, J.W.; Bo, L.; Mork, S.; Chang, A.; Trapp, B.D. Transected neurites, apoptotic neurons, and reduced inflammation in cortical multiple sclerosis lesions. Ann. Neurol. 2001, 50, 389–400. [Google Scholar] [CrossRef]
- Heidker, R.M.; Emerson, M.R.; LeVine, S.M. Metabolic pathways as possible therapeutic targets for progressive multiple sclerosis. Neural Regen. Res. 2017, 12, 1262–1267. [Google Scholar]
- Mahad, D.H.; Trapp, B.D.; Lassmann, H. Pathological mechanisms in progressive multiple sclerosis. Lancet Neurol. 2015, 14, 183–193. [Google Scholar] [CrossRef]
- Dutta, R.; McDonough, J.; Yin, X.; Peterson, J.; Chang, A.; Torres, T.; Gudz, T.; Macklin, W.B.; Lewis, D.A.; Fox, R.J.; et al. Mitochondrial dysfunction as a cause of axonal degeneration in multiple sclerosis patients. Ann. Neurol. 2006, 59, 478–489. [Google Scholar] [CrossRef]
- Trapp, B.D.; Stys, P.K. Virtual hypoxia and chronic necrosis of demyelinated axons in multiple sclerosis. Lancet Neurol. 2009, 8, 280–291. [Google Scholar] [CrossRef]
- Patergnani, S.; Fossati, V.; Bonora, M.; Giorgi, C.; Marchi, S.; Missiroli, S.; Rusielewicz, T.; Wieckowski, M.R.; Pinton, P. Mitochondria in Multiple Sclerosis: Molecular Mechanisms of Pathogenesis. Int. Rev. Cell Mol. Biol. 2017, 328, 49–103. [Google Scholar] [PubMed]
- Schoenfeld, R.; Wong, A.; Silva, J.; Li, M.; Itoh, A.; Horiuchi, M.; Itoh, T.; Pleasure, D.; Cortopassi, G. Oligodendroglial differentiation induces mitochondrial genes and inhibition of mitochondrial function represses oligodendroglial differentiation. Mitochondrion 2010, 10, 143–150. [Google Scholar] [CrossRef]
- French, H.M.; Reid, M.; Mamontov, P.; Simmons, R.A.; Grinspan, J.B. Oxidative stress disrupts oligodendrocyte maturation. J. Neurosci. Res. 2009, 87, 3076–3087. [Google Scholar] [CrossRef]
- Madsen, P.M.; Pinto, M.; Patel, S.; McCarthy, S.; Gao, H.; Taherian, M.; Karmally, S.; Pereira, C.V.; Dvoriantchikova, G.; Ivanov, D.; et al. Mitochondrial DNA Double-Strand Breaks in Oligodendrocytes Cause Demyelination, Axonal Injury, and CNS Inflammatio. J. Neurosci., vol. 2017, 37, 10185–10199. [Google Scholar] [CrossRef]
- Li, S.; Clements, R.; Sulak, M.; Gregory, R.; Freeman, E.; McDonough, J. Decreased NAA in gray matter is correlated with decreased availability of acetate in white matter in postmortem multiple sclerosis cortex. Neurochem. Res. 2013, 38, 2385–2396. [Google Scholar] [CrossRef]
- Campbell, G.R.; Ziabreva, I.; Reeve, A.K.; Krishnan, K.J.; Reynolds, R.; Howell, O.; Lassmann, H.; Turnbull, D.M.; Mahad, D.J. Mitochondrial DNA deletions and neurodegeneration in multiple sclerosis. Ann. Neurol. 2011, 69, 481–492. [Google Scholar] [CrossRef] [PubMed]
- Witte, M.E.; Nijland, P.G.; Drexhage, J.A.; Gerritsen, W.; Geerts, D.; van Het Hof, B.; Reijerkerk, A.; de Vries, H.E.; van der Valk, P.; van Horssen, J. Reduced expression of PGC-1alpha partly underlies mitochondrial changes and correlates with neuronal loss in multiple sclerosis cortex. Acta Neuropathol. 2013, 125, 231–243. [Google Scholar] [CrossRef]
- Pandit, A.; Vadnal, J.; Houston, S.; Freeman, E.; McDonough, J. Impaired regulation of electron transport chain subunit genes by nuclear respiratory factor 2 in multiple sclerosis. J. Neurol. Sci. 2009, 279, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Witte, M.E.; Bø, L.; Rodenburg, R.J.; Belien, J.A.; Musters, R.; Hazes, T.; Wintjes, L.T.; Smeitink, J.A.; Geurts, J.J.; De Vries, H.E.; et al. Enhanced number and activity of mitochondria in multiple sclerosis lesions. J. Pathol. 2009, 219, 193–204. [Google Scholar] [CrossRef]
- Choi, I.Y.; Lee, P.; Adany, P.; Hughes, A.J.; Belliston, S.; Denney, D.R.; Lynch, S.G. In vivo evidence of oxidative stress in brains of patients with progressive multiple sclerosis. Mult. Scler. 2018, 24, 1029–1038. [Google Scholar] [CrossRef]
- Broadwater, L.; Pandit, A.; Clements, R.; Azzam, S.; Vadnal, J.; Sulak, M.; Yong, V.W.; Freeman, E.J.; Gregory, R.B.; McDonough, J. Analysis of the mitochondrial proteome in multiple sclerosis cortex. Biochim. Biophys. Acta 2011, 1812, 630–641. [Google Scholar] [CrossRef]
- Mahad, D.J.; Ziabreva, I.; Campbell, G.; Lax, N.; White, K.; Hanson, P.S.; Lassmann, H.; Turnbull, D.M. Mitochondrial changes within axons in multiple sclerosis. Brain 2009, 132, 1161–1174. [Google Scholar] [CrossRef] [PubMed]
- Zambonin, J.L.; Zhao, C.; Ohno, N.; Campbell, G.R.; Engeham, S.; Ziabreva, I.; Schwarz, N.; Lee, S.E.; Frischer, J.M.; Turnbull, D.M.; et al. Increased mitochondrial content in remyelinated axons: Implications for multiple sclerosis. Brain 2011, 134, 1901–1913. [Google Scholar] [CrossRef] [PubMed]
- Lassmann, H.; Bradl, M. Multiple sclerosis: Experimental models and reality. Acta Neuropathol. 2017, 133, 223–244. [Google Scholar] [CrossRef]
- Hampton, D.W.; Serio, A.; Pryce, G.; Al-Izki, S.; Franklin, R.J.; Giovannoni, G.; Baker, D.; Chandran, S. Neurodegeneration progresses despite complete elimination of clinical relapses in a mouse model of multiple sclerosis. Acta Neuropathol. Commun. 2013, 1, 84. [Google Scholar] [CrossRef] [PubMed]
- Recks, M.S.; Stormanns, E.R.; Bader, J.; Arnhold, S.; Addicks, K.; Kuerten, S. Early axonal damage and progressive myelin pathology define the kinetics of CNS histopathology in a mouse model of multiple sclerosis. Clin. Immunol. 2013, 149, 32–45. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Tao, T.; Yan, W.; Chen, C.S.; Qin, X. Curcumin inhibits mitochondrial injury and apoptosis from the early stage in EAE mice. Oxid. Med. Cell. Longev. 2014, 2014, 728751. [Google Scholar] [CrossRef]
- Sadeghian, M.; Mastrolia, V.; Rezaei Haddad, A.; Mosley, A.; Mullali, G.; Schiza, D.; Sajic, M.; Hargreaves, I.; Heales, S.; Duchen, M.R.; et al. Mitochondrial dysfunction is an important cause of neurological deficits in an inflammatory model of multiple sclerosis. Sci. Rep. 2016, 6, 33249. [Google Scholar] [CrossRef]
- Talla, V.; Yu, H.; Chou, T.H.; Porciatti, V.; Chiodo, V.; Boye, S.L.; Hauswirth, W.W.; Lewin, A.S.; Guy, J. NADH-dehydrogenase type-2 suppresses irreversible visual loss and neurodegeneration in the EAE animal model of MS. Mol. Ther. 2013, 21, 1876–1888. [Google Scholar] [CrossRef]
- Talla, V.; Koilkonda, R.; Porciatti, V.; Chiodo, V.; Boye, S.L.; Hauswirth, W.W.; Guy, J. Complex I subunit gene therapy with NDUFA6 ameliorates neurodegeneration in EAE. Investig. Ophthalmol. Vis. Sci. 2015, 56, 1129–1140. [Google Scholar] [CrossRef]
- Fetisova, E.; Chernyak, B.; Korshunova, G.; Muntyan, M.; Skulachev, V. Mitochondria-targeted Antioxidants as a Prospective Therapeutic Strategy for Multiple Sclerosis. Curr. Med. Chem. 2017, 24, 2086–2114. [Google Scholar] [CrossRef] [PubMed]
- Mao, P.; Manczak, M.; Shirendeb, U.P.; Reddy, P.H. MitoQ, a mitochondria-targeted antioxidant, delays disease progression and alleviates pathogenesis in an experimental autoimmune encephalomyelitis mouse model of multiple sclerosis. Biochim. Biophys. Acta. 2013, 1832, 2322–2331. [Google Scholar] [CrossRef]
- Andrews, H.; White, K.; Thomson, C.; Edgar, J.; Bates, D.; Griffiths, I.; Turnbull, D.; Nichols, P. Increased axonal mitochondrial activity as an adaptation to myelin deficiency in the Shiverer mouse. J. Neurosci. Res. 2006, 83, 1533–1539. [Google Scholar] [CrossRef]
- Procaccini, C.; de Rosa, V.; Pucino, V.; Formisano, L.; Matarese, G. Animal models of Multiple Sclerosis. Eur. J. Pharmacol. 2015, 759, 182–191. [Google Scholar] [CrossRef]
- Warford, J.; Robertson, G.S. New methods for multiple sclerosis drug discovery. Expert Opin. Drug Discov. 2011, 6, 689–699. [Google Scholar] [CrossRef]
- Furlan, R.; Poliani, P.L.; Marconi, P.C.; Bergami, A.; Ruffini, F.; Adorini, L.; Glorioso, J.C.; Comi, G.; Martino, G. Central nervous system gene therapy with interleukin-4 inhibits progression of ongoing relapsing-remitting autoimmune encephalomyelitis in Biozzi AB/H mice. Gene Ther. 2001, 8, 13–19. [Google Scholar] [CrossRef][Green Version]
- Al-Izki, S.; Pryce, G.; O’Neill, J.K.; Butter, C.; Giovannoni, G.; Amor, S.; Baker, D. Practical guide to the induction of relapsing progressive experimental autoimmune encephalomyelitis in the Biozzi ABH mouse. Mult. Scler. Relat. Disord. 2012, 1, 29–38. [Google Scholar] [CrossRef]
- Praet, J.; Guglielmetti, C.; Berneman, Z.; van der Linden, A.; Ponsaerts, P. Cellular and molecular neuropathology of the cuprizone mouse model: Clinical relevance for multiple sclerosis. Neurosci. Biobehav. Rev. 2014, 47, 485–505. [Google Scholar] [CrossRef] [PubMed]
- Schreiner, B.; Heppner, F.L.; Becher, B. Modeling multiple sclerosis in laboratory animals. Semin. Immunopathol. 2009, 31, 479–495. [Google Scholar] [CrossRef] [PubMed]
- Hemm, R.D.; Carlton, W.W.; Welser, J.R. Ultrastructural changes of cuprizone encephalopathy in mice. Toxicol. Appl. Pharmacol. 1971, 18, 869–882. [Google Scholar] [CrossRef]
- Bénardais, K.; Kotsiari, A.; Skuljec, J.; Koutsoudaki, P.N.; Gudi, V.; Singh, V.; Vulinović, F.; Skripuletz, T.; Stangel, M. Cuprizone [bis(cyclohexylidenehydrazide)] is selectively toxic for mature oligodendrocytes. Neurotox. Res. 2013, 24, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Howarth, C.; Gleeson, P.; Attwell, D. Updated energy budgets for neural computation in the neocortex and cerebellum. J. Cereb. Blood Flow Metab. 2012, 32, 1222–1232. [Google Scholar] [CrossRef] [PubMed]
- Dziedzic, T.; Metz, I.; Dallenga, T.; König, F.B.; Müller, S.; Stadelmann, C.; Brück, W. Wallerian degeneration: A major component of early axonal pathology in multiple sclerosis. Brain Pathol. 2010, 20, 976–985. [Google Scholar] [CrossRef]
- Campbell, G.; Mahad, D.J. Mitochondrial dysfunction and axon degeneration in progressive multiple sclerosis. FEBS Lett. 2018, 592, 1113–1121. [Google Scholar] [CrossRef] [PubMed]
- Kiryu-Seo, S.; Ohno, N.; Kidd, G.J.; Komuro, H.; Trapp, B.D. Demyelination increases axonal stationary mitochondrial size and the speed of axonal mitochondrial transport. J. Neurosci. 2010, 30, 6658–6666. [Google Scholar] [CrossRef] [PubMed]
- Tsutsui, S.; Stys, P.K. Metabolic injury to axons and myelin. Exp. Neurol. 2013, 246, 26–34. [Google Scholar] [CrossRef]
- Witte, M.E.; Mahad, D.J.; Lassmann, H.; van Horssen, J. Mitochondrial dysfunction contributes to neurodegeneration in multiple sclerosis. Trends Mol. Med. 2014, 20, 179–187. [Google Scholar] [CrossRef]
- Willer, C.J.; Dyment, D.A.; Risch, N.J.; Sadovnick, A.D.; Ebers, G.C. Twin concordance and sibling recurrence rates in multiple sclerosis. Proc. Natl. Acad. Sci. USA 2003, 100, 12877–12882. [Google Scholar] [CrossRef] [PubMed]
- Hollenbach, J.A.; Oksenberg, J.R. The immunogenetics of multiple sclerosis: A comprehensive review. J. Autoimmun. 2015, 64, 13–25. [Google Scholar] [CrossRef]
- Yu, X.; Koczan, D.; Sulonen, A.M.; Akkad, D.A.; Kroner, A.; Comabella, M.; Costa, G.; Corongiu, D.; Goertsches, R.; Camina-Tato, M.; et al. mtDNA nt13708A variant increases the risk of multiple sclerosis. PLoS ONE 2008, 3, e1530. [Google Scholar] [CrossRef]
- Andalib, S.; Emamhadi, M.; Yousefzadeh-Chabok, S.; Salari, A.; Sigaroudi, A.E.; Vafaee, M.S. MtDNA T4216C variation in multiple sclerosis: A systematic review and meta-analysis. Acta Neurol. Belg. 2016, 116, 439–443. [Google Scholar] [CrossRef]
- Tranah, G.J.; Santaniello, A.; Caillier, S.J.; D’Alfonso, S.; Martinelli Boneschi, F.; Hauser, S.L.; Oksenberg, J.R. Mitochondrial DNA sequence variation in multiple sclerosis. Neurology 2015, 85, 325–330. [Google Scholar] [CrossRef]
- Falabella, M.; Forte, E.; Magnifico, M.C.; Santini, P.; Arese, M.; Giuffrè, A.; Radić, K.; Chessa, L.; Coarelli, G.; Buscarinu, M.C.; et al. Evidence for Detrimental Cross Interactions between Reactive Oxygen and Nitrogen Species in Leber’s Hereditary Optic Neuropathy Cells. Oxid. Med. Cell. Longev. 2016, 2016, 3187560. [Google Scholar] [CrossRef]
- Howell, N. Leber hereditary optic neuropathy: Mitochondrial mutations and degeneration of the optic nerve. Vision Res. 1997, 37, 3495–3507. [Google Scholar] [CrossRef]
- Harding, A.E.; Sweeney, M.G.; Miller, D.H.; Mumford, C.J.; Kellar-Wood, H.; Menard, D.; McDonald, W.I.; Compston, D.A. Occurrence of a multiple sclerosis-like illness in women who have a Leber’s hereditary optic neuropathy mitochondrial DNA mutation. Brain 1992, 115 Pt 4, 979–989. [Google Scholar] [CrossRef]
- Yu-Wai-Man, P.; Griffiths, P.G.; Chinnery, P.F. Mitochondrial optic neuropathies - disease mechanisms and therapeutic strategies. Prog. Retin. Eye Res. 2011, 30, 81–114. [Google Scholar] [CrossRef]
- Palace, J. Multiple sclerosis associated with Leber’s Hereditary Optic Neuropathy. J. Neurol. Sci. 2009, 286, 24–27. [Google Scholar] [CrossRef]
- Zanna, C.; Ghelli, A.; Porcelli, A.M.; Karbowski, M.; Youle, R.J.; Schimpf, S.; Wissinger, B.; Pinti, M.; Cossarizza, A.; Vidoni, S.; et al. OPA1 mutations associated with dominant optic atrophy impair oxidative phosphorylation and mitochondrial fusion. Brain 2008, 131, 352–367. [Google Scholar] [CrossRef]
- Echaniz-Laguna, A.; Chassagne, M.; de Sèze, J.; Mohr, M.; Clerc-Renaud, P.; Tranchant, C.; Mousson de Camaret, B. POLG1 variations presenting as multiple sclerosis. Arch. Neurol. 2010, 67, 1140–1143. [Google Scholar] [CrossRef]
- Spain, R.; Powers, K.; Murchison, C.; Heriza, E.; Winges, K.; Yadav, V.; Cameron, M.; Kim, E.; Horak, F.; Simon, J.; et al. Lipoic acid in secondary progressive MS: A randomized controlled pilot trial. Neurol. Neuroimmunol. Neuroinflamm. 2017, 4, e374. [Google Scholar] [CrossRef]
- Peruzzotti-Jametti, L.; Pluchino, S. Targeting Mitochondrial Metabolism in Neuroinflammation: Towards a Therapy for Progressive Multiple Sclerosis. Trends Mol. Med. 2018, 24, 838–855. [Google Scholar] [CrossRef] [PubMed]
- Tourbah, A.; Lebrun-Frenay, C.; Edan, G.; Clanet, M.; Papeix, C.; Vukusic, S.; De Sèze, J.; Debouverie, M.; Gout, O.; Clavelou, P.; et al. MD1003 (high-dose biotin) for the treatment of progressive multiple sclerosis: A randomised, double-blind, placebo-controlled study. Mult. Scler. 2016, 22, 1719–1731. [Google Scholar] [CrossRef]
- Jang, Y.-H.; Lim, K.-I. Recent Advances in Mitochondria-Targeted Gene Delivery. Molecules 2018, 23, 2316. [Google Scholar] [CrossRef] [PubMed]
- Finsterer, J.; Zarrouk-Mahjoub, S. Re: Guy et al.: Gene therapy for Leber hereditary optic neuropathy: Low-and medium-dose visual results (Ophthalmology. 2017; 124:1621–1634). Ophthalmology 2018, 125, e14–e15. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).