Engineered Exosomes Complexed with Botulinum Toxin Type A for Enhanced Anti-Aging Effects on Skin
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Cell Culture
2.2. Plasmid Construction
2.3. Lentiviral Packaging and Transduction
2.4. Quantitative PCR (qPCR)
2.5. Exosome Isolation and Characterization
2.6. Cell Senescence Model Induction
2.7. Cell Viability Assay
2.8. Scratch Wound Healing Assay
2.9. Mouse Skin Aging Model
2.10. Determination of Mouse Lethal Dose
2.11. Malondialdehyde Assay
2.12. Histological Evaluation
2.13. Western Blot Analysis
2.14. Immunofluorescence Staining and SA-β-Galactosidase Assay
2.15. Statistical Analysis
3. Results
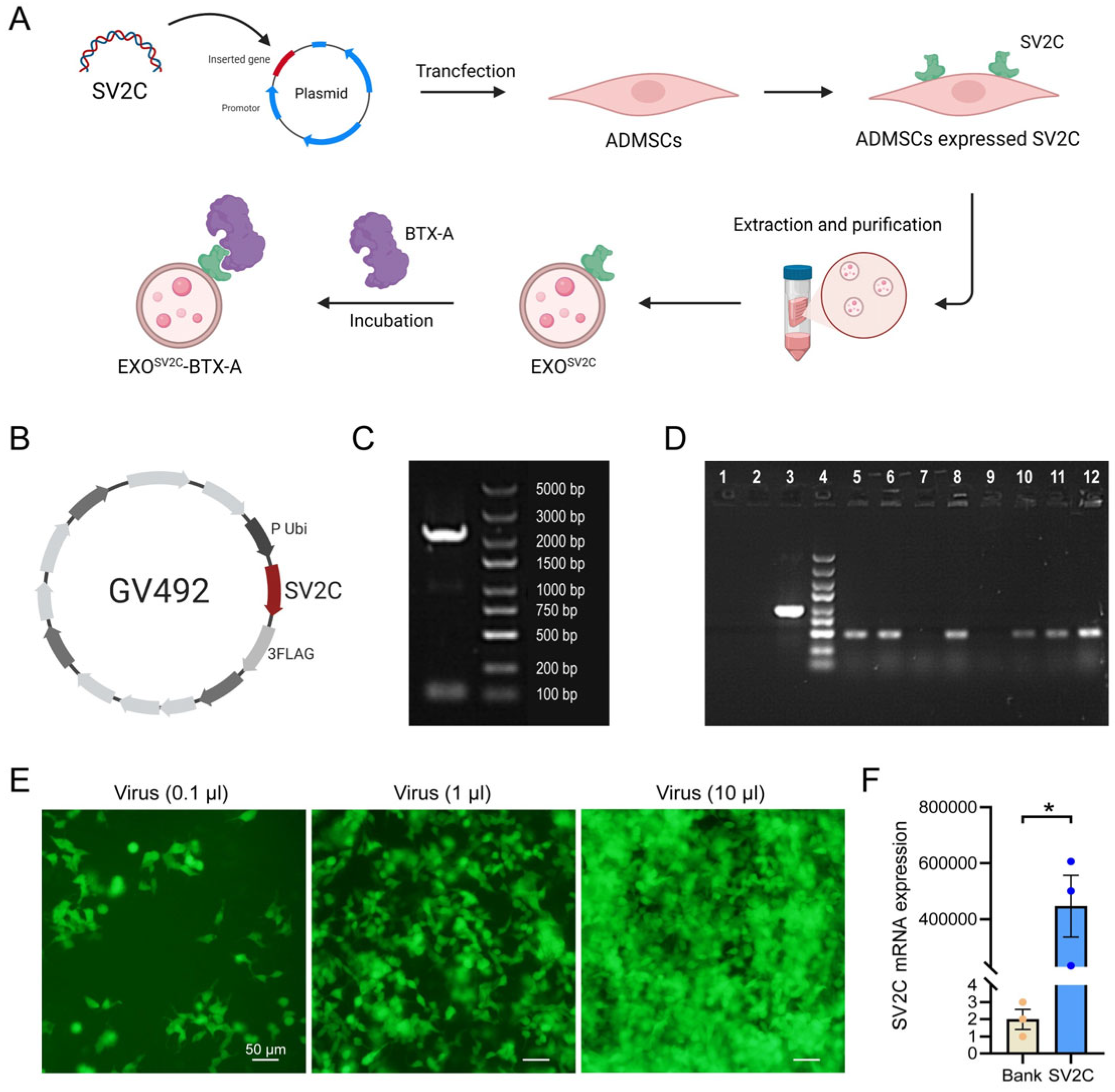
3.1. Construction of SV2C-Overexpressing Lentiviral Vector
3.2. Generation of SV2C-Overexpressing ADMSCs
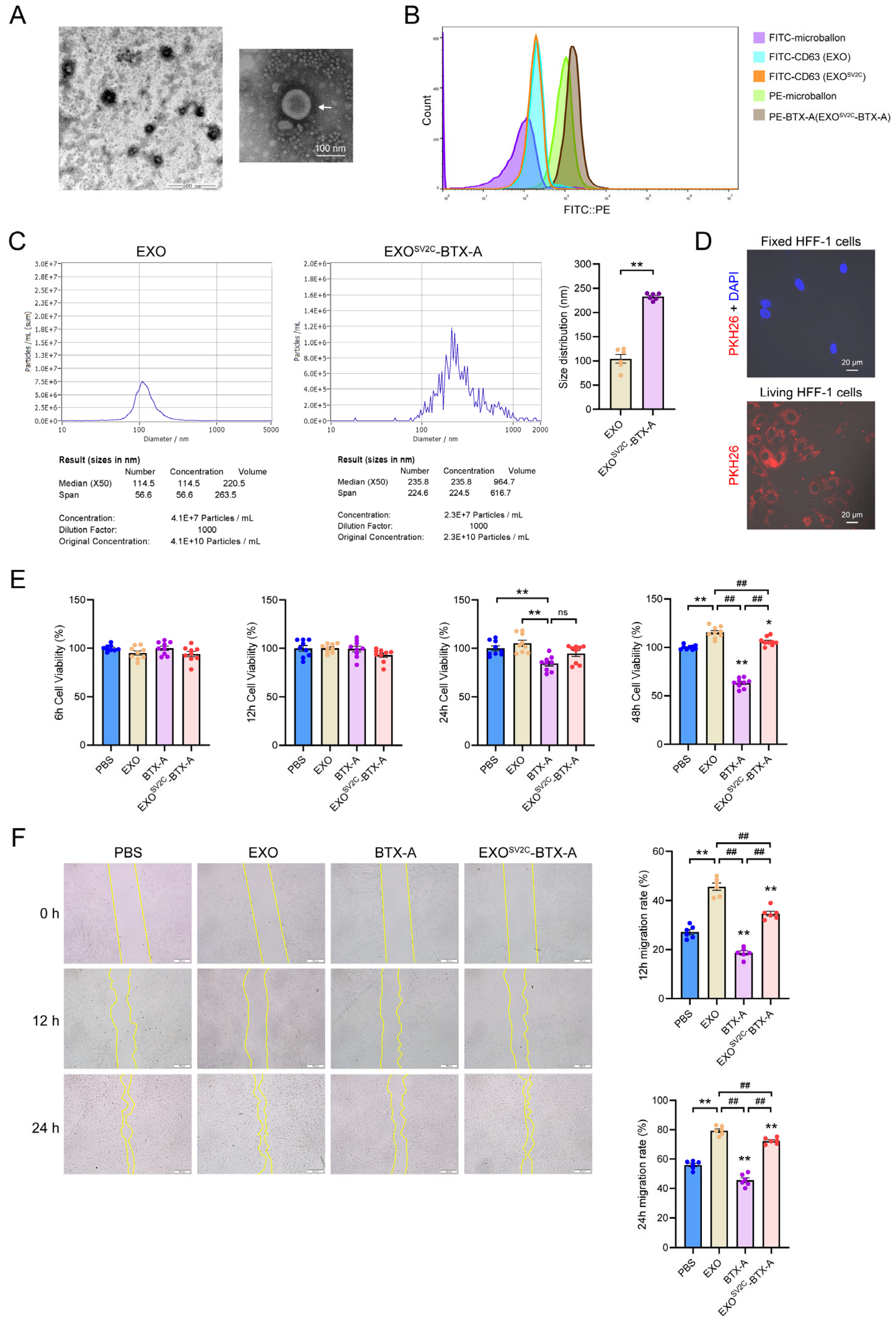
3.3. SV2C-Exosomes Bind BTX-A and Reduce Cytotoxicity
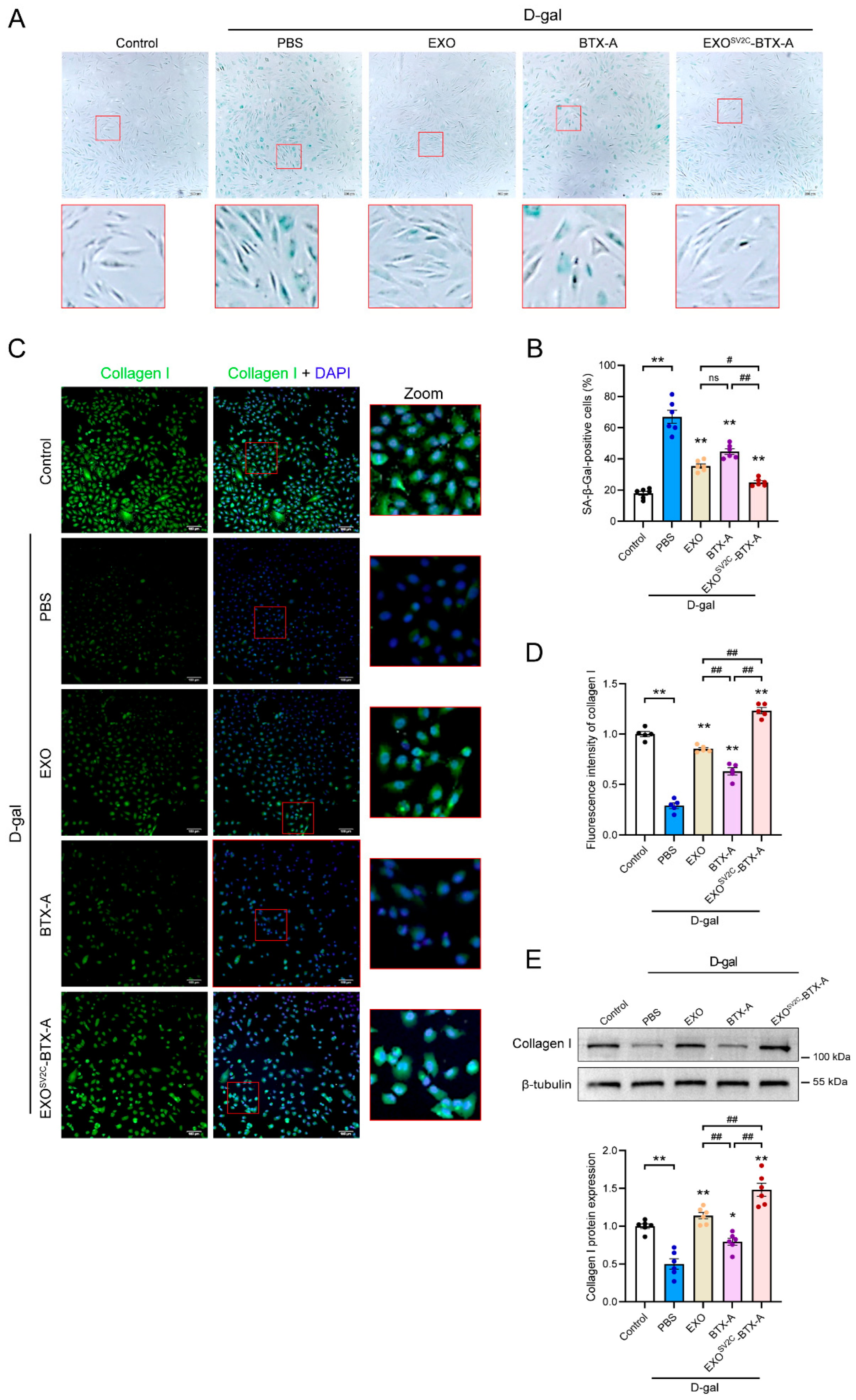
3.4. EXOSV2C-BTX-A Inhibits D-Galactose-Induced Collagen Loss and Cellular Senescence
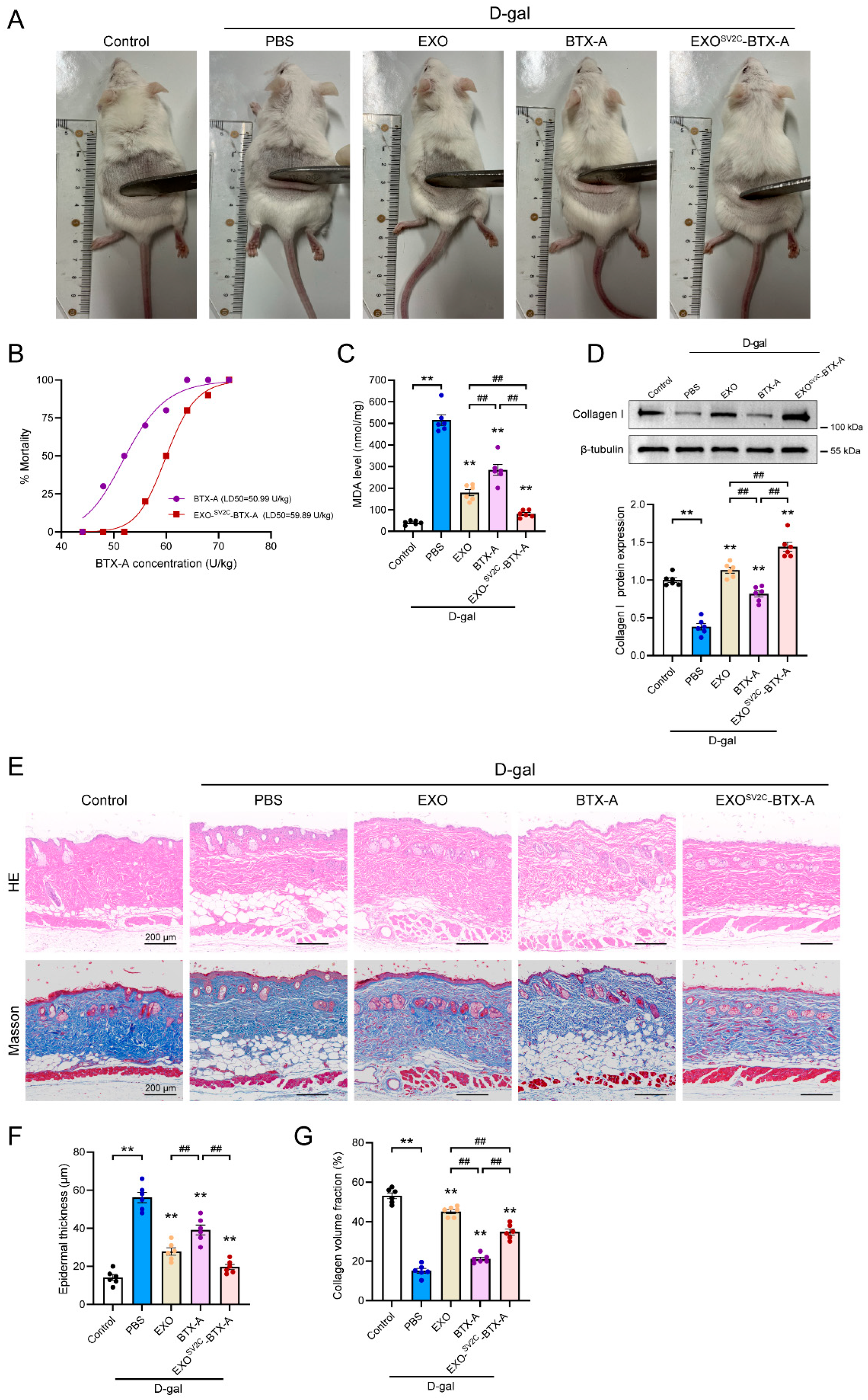
3.5. EXOSV2C-BTX-A Attenuates D-Galactose-Induced Skin Aging in Mice
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BTX-A | Botulinum toxin type A |
| SV2C | synaptic vesicle glycoprotein 2C |
| EXOSV2C | SV2C-overexpressing exosomes |
| MSCs | Mesenchymal stem cells |
| MDA | Malondialdehyde |
References
- Wang, N.; Dong, Y.; Xu, X.; Shen, Y.; Huang, Z.; Yu, Y.; Liu, Z.; Gong, W.; Zhang, S.; Zheng, Y.; et al. Fibroblast growth factor 10 protects against UVB-induced skin injury by activating the ERK/YAP signalling pathway. Cell Prolif. 2022, 55, e13315. [Google Scholar] [CrossRef]
- De Cauwer, A.; Loustau, T.; Erne, W.; Pichot, A.; Molitor, A.; Stemmelen, T.; Carapito, R.; Orend, G.; Bahram, S.; Georgel, P. Dicer1 deficient mice exhibit premature aging and metabolic perturbations in adipocytes. Iscience 2022, 25, 105149. [Google Scholar] [CrossRef] [PubMed]
- Rorteau, J.; Chevalier, F.P.; Bonnet, S.; Barthelemy, T.; Lopez-Gaydon, A.; Martin, L.S.; Bechetoille, N.; Lamartine, J. Maintenance of Chronological Aging Features in Culture of Normal Human Dermal Fibroblasts from Old Donors. Cells 2022, 11, 858. [Google Scholar] [CrossRef] [PubMed]
- Sethi, N.; Singh, S.; DeBoulle, K.; Rahman, E. A Review of Complications Due to the Use of Botulinum Toxin A for Cosmetic Indications. Aesthetic Plast. Surg. 2021, 45, 1210–1220. [Google Scholar] [CrossRef] [PubMed]
- Hanna, E.; Xing, L.; Taylor, J.H.; Bertucci, V. Role of botulinum toxin A in improving facial erythema and skin quality. Arch. Dermatol. Res. 2022, 314, 729–738. [Google Scholar] [CrossRef]
- Lee, K.W.A.; Chan, L.K.W.; Lee, A.W.K.; Lee, C.H.; Wan, J.; Yi, K.H. Immunogenicity of Botulinum Toxin Type A in Different Clinical and Cosmetic Treatment, a Literature Review. Life 2024, 14, 1217. [Google Scholar] [CrossRef]
- Li, X.; Sui, C.; Xia, X.; Chen, X. Efficacy and Safety of Botulinum Toxin Type A for Treatment of Glabellar Lines: A Network Meta-Analysis of Randomized Controlled Trials. Aesthetic Plast. Surg. 2023, 47, 365–377. [Google Scholar] [CrossRef]
- Gregory, K.S.; Mahadeva, T.B.; Liu, S.M.; Acharya, K.R. Structural Features of Clostridium botulinum Neurotoxin Subtype A2 Cell Binding Domain. Toxins 2022, 14, 356. [Google Scholar] [CrossRef]
- Polo, M. Botulinum Toxin and Smile Design. Dent. Clin. N. Am. 2022, 66, 419–429. [Google Scholar] [CrossRef]
- Agarwal, U.; Hamilton, K.; Ali, A.; Mathew, P.G. The use of onabotulinum toxin type A and other neurotoxins for the treatment of chronic migraine: An American Headache Society survey study. Clin. Neurol. Neurosurg. 2025, 254, 108960. [Google Scholar] [CrossRef]
- Alhejaili, A.L.; Alkayyal, A.A.; Alawaz, R.A.; Alshareef, E.K.; Al-Habboubi, H. Dose-Effect Relationship of Botulinum Toxin Type A in the Management of Strabismus: A Review. Cureus 2024, 16, e71271. [Google Scholar] [CrossRef]
- Farham, F.; Onan, D.; Martelletti, P. Non-Migraine Head Pain and Botulinum Toxin. Toxins 2024, 16, 431. [Google Scholar] [CrossRef]
- Maytharakcheep, S.; Bhidayasiri, R. Botulinum toxin treatment for hemifacial spasm: Harmonising neurological and aesthetic outcomes. J. Neural Transm. 2025, 132, 23–38. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Lv, Q.; Zheng, Y.; Gao, S.; Huang, W.; Liu, P.; Kong, D.; Wang, Y.; Yu, Y.; Jiang, Y.; et al. Rapid and sensitive detection of botulinum toxin type A in complex sample matrices by AlphaLISA. Front. Public Health 2022, 10, 987517. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Lan, D.; Ning, S.; Jia, H.; Yu, S. Botulinum toxin type A prevents the phenotypic transformation of fibroblasts induced by TGF-beta1 via the PTEN/PI3K/Akt signaling pathway. Int. J. Mol. Med. 2019, 44, 661–671. [Google Scholar] [CrossRef] [PubMed]
- Aseervatham, J. Dynamic Role of Exosome microRNAs in Cancer Cell Signaling and Their Emerging Role as Noninvasive Biomarkers. Biology 2023, 12, 710. [Google Scholar] [CrossRef]
- Ha, D.H.; Kim, H.K.; Lee, J.; Kwon, H.H.; Park, G.H.; Yang, S.H.; Jung, J.Y.; Choi, H.; Lee, J.H.; Sung, S.; et al. Mesenchymal Stem/Stromal Cell-Derived Exosomes for Immunomodulatory Therapeutics and Skin Regeneration. Cells 2020, 9, 1157. [Google Scholar] [CrossRef]
- Jadamba, B.; Jin, Y.; Lee, H. Harmonising cellular conversations: Decoding the vital roles of extracellular vesicles in respiratory system intercellular communications. Eur. Respir. Rev. 2024, 33, 230272. [Google Scholar] [CrossRef]
- Ngo, J.M.; Williams, J.K.; Zhang, C.; Saleh, A.H.; Liu, X.M.; Ma, L.; Schekman, R. Extracellular Vesicles and Cellular Homeostasis. Annu. Rev. Biochem. 2025, 94, 587–609. [Google Scholar] [CrossRef]
- Ben, X.Y.; Wang, Y.R.; Zheng, H.H.; Li, D.X.; Ren, R.; Ni, P.L.; Zhang, H.Y.; Feng, R.J.; Li, Y.Q.; Li, Q.F.; et al. Construction of Exosomes that Overexpress CD47 and Evaluation of Their Immune Escape. Front. Bioeng. Biotechnol. 2022, 10, 936951. [Google Scholar] [CrossRef]
- Yan, C.; Chen, J.; Wang, C.; Yuan, M.; Kang, Y.; Wu, Z.; Li, W.; Zhang, G.; Machens, H.G.; Rinkevich, Y.; et al. Milk exosomes-mediated miR-31-5p delivery accelerates diabetic wound healing through promoting angiogenesis. Drug Deliv. 2022, 29, 214–228. [Google Scholar] [CrossRef]
- Wu, J.Y.; Wu, S.N.; Zhang, L.P.; Zhao, X.S.; Li, Y.; Yang, Q.Y.; Yuan, R.Y.; Liu, J.L.; Mao, H.J.; Zhu, N.W. Stem Cell-Derived Exosomes: A New Method for Reversing Skin Aging. Tissue Eng. Regen. Med. 2022, 19, 961–968. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.C.; Zheng, C.X.; Sui, B.D.; Liu, W.J.; Jin, Y. Mesenchymal stem cell-derived exosomes: A novel and potential remedy for cutaneous wound healing and regeneration. World J. Stem Cells 2022, 14, 318–329. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Yu, Z.; Li, Y.; Wang, Y.; Li, Q.; Han, D. GelMA combined with sustained release of HUVECs derived exosomes for promoting cutaneous wound healing and facilitating skin regeneration. J. Mol. Histol. 2020, 51, 251–263. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.H.; Ben, X.Y.; Wang, Y.R.; Tian, M.S.; Meng, Q.W.; Li, D.X.; Wen, S.L.; Ni, P.L.; Hao, J.W.; Zhang, Q.P.; et al. Experimental study on the effect and mechanism of adipose stem cell-derived exosomes combined with botulinum toxin A on skin trauma in rats. J. Cosmet. Dermatol. 2024, 23, 271–283. [Google Scholar] [CrossRef]
- He, X.; Wan, F.; Su, W.; Xie, W. Research Progress on Skin Aging and Active Ingredients. Molecules 2023, 28, 5556. [Google Scholar] [CrossRef]
- Umbayev, B.; Askarova, S.; Almabayeva, A.; Saliev, T.; Masoud, A.R.; Bulanin, D. Galactose-Induced Skin Aging: The Role of Oxidative Stress. Oxidative Med. Cell. Longev. 2020, 2020, 7145656. [Google Scholar] [CrossRef]
- Guo, Q.; Kawahata, I.; Degawa, T.; Ikeda-Matsuo, Y.; Sun, M.; Han, F.; Fukunaga, K. Fatty Acid-Binding Proteins Aggravate Cerebral Ischemia-Reperfusion Injury in Mice. Biomedicines 2021, 9, 529. [Google Scholar] [CrossRef]
- Guo, Q.; Kawahata, I.; Cheng, A.; Wang, H.; Jia, W.; Yoshino, H.; Fukunaga, K. Fatty acid-binding proteins 3 and 5 are involved in the initiation of mitochondrial damage in ischemic neurons. Redox Biol. 2023, 59, 102547. [Google Scholar] [CrossRef]
- Bauwens, E.; Paree, T.; Meurant, S.; Bouriez, I.; Hannart, C.; Wera, A.C.; Khelfi, A.; Fattaccioli, A.; Burteau, S.; Demazy, C.; et al. Senescence Induced by UVB in Keratinocytes Impairs Amino Acids Balance. J. Investig. Dermatol. 2023, 143, 554–565.e9. [Google Scholar] [CrossRef]
- Jiang, H.; Zhou, X.; Chen, L. Asiaticoside delays senescence and attenuate generation of ROS in UV-exposure cells through regulates TGF-beta1/Smad pathway. Exp. Ther. Med. 2022, 24, 667. [Google Scholar] [CrossRef]
- Desplantes, R.; Leveque, C.; Muller, B.; Lotierzo, M.; Ferracci, G.; Popoff, M.; Seagar, M.; Mamoun, R.; El Far, O. Affinity biosensors using recombinant native membrane proteins displayed on exosomes: Application to botulinum neurotoxin B receptor. Sci. Rep. 2017, 7, 1032. [Google Scholar] [CrossRef] [PubMed]
- Flores, A.; Ramirez-Franco, J.; Desplantes, R.; Debreux, K.; Ferracci, G.; Wernert, F.; Blanchard, M.P.; Maulet, Y.; Youssouf, F.; Sangiardi, M.; et al. Gangliosides interact with synaptotagmin to form the high-affinity receptor complex for botulinum neurotoxin B. Proc. Natl. Acad. Sci. USA 2019, 116, 18098–18108. [Google Scholar] [CrossRef] [PubMed]
- Park, G.S.; An, M.K.; Yoon, J.H.; Park, S.S.; Koh, S.H.; Mauro, T.M.; Cho, E.B.; Park, E.J.; Kim, K.H.; Kim, K.J. Botulinum toxin type A suppresses pro-fibrotic effects via the JNK signaling pathway in hypertrophic scar fibroblasts. Arch. Dermatol. Res. 2019, 311, 807–814. [Google Scholar] [CrossRef] [PubMed]
- Jhawar, N.; Wang, J.V.; Saedi, N. Oral collagen supplementation for skin aging: A fad or the future? J. Cosmet. Dermatol. 2020, 19, 910–912. [Google Scholar] [CrossRef]
- Wasityastuti, W.; Habib, N.A.; Sari, D.C.R.; Arfian, N. Effects of low and moderate treadmill exercise on liver of d-galactose-exposed aging rat model. Physiol. Rep. 2019, 7, e14279. [Google Scholar] [CrossRef]
- Widgerow, A.D.; Napekoski, K. New approaches to skin photodamage histology-Differentiating ‘good’ versus ‘bad’ Elastin. J. Cosmet. Dermatol. 2021, 20, 526–531. [Google Scholar] [CrossRef]
- Ellistasari, E.Y.; Kariosentono, H.; Purwanto, B.; Wasita, B.; Riswiyant, R.C.A.; Pamungkasari, E.P.; Soetrisno, S. Exosomes Derived from Secretome Human Umbilical Vein Endothelial Cells (Exo-HUVEC) Ameliorate the Photo-Aging of Skin Fibroblast. Clin. Cosmet. Investig. Dermatol. 2022, 15, 1583–1591. [Google Scholar] [CrossRef]
- Oh, M.; Lee, J.; Kim, Y.J.; Rhee, W.J.; Park, J.H. Exosomes Derived from Human Induced Pluripotent Stem Cells Ameliorate the Aging of Skin Fibroblasts. Int. J. Mol. Sci. 2018, 19, 1715. [Google Scholar] [CrossRef]
- Zhang, K.; Yu, L.; Li, F.R.; Li, X.; Wang, Z.; Zou, X.; Zhang, C.; Lv, K.; Zhou, B.; Mitragotri, S.; et al. Topical Application of Exosomes Derived from Human Umbilical Cord Mesenchymal Stem Cells in Combination with Sponge Spicules for Treatment of Photoaging. Int. J. Nanomed. 2020, 15, 2859–2872. [Google Scholar] [CrossRef]
- Wang, Y.; Shen, X.; Song, S.; Chen, N.; Wang, Y.; Liao, W.; Jia, C.; Zeng, L. Evaluation of the Effect of Exosomes From Adipose Derived Stem Cells on Changes in GSH/ROS Levels During Skin Photoaging. Photodermatol. Photoimmunol. Photomed. 2025, 41, e70009. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Wang, K.; Ben, X.; Tian, M.; Liu, X.; Li, Z.; Ni, P.; Liu, Q.; Ma, Z.; Yi, X.; et al. Engineered Exosomes Complexed with Botulinum Toxin Type A for Enhanced Anti-Aging Effects on Skin. Biology 2025, 14, 1040. https://doi.org/10.3390/biology14081040
Wang Y, Wang K, Ben X, Tian M, Liu X, Li Z, Ni P, Liu Q, Ma Z, Yi X, et al. Engineered Exosomes Complexed with Botulinum Toxin Type A for Enhanced Anti-Aging Effects on Skin. Biology. 2025; 14(8):1040. https://doi.org/10.3390/biology14081040
Chicago/Turabian StyleWang, Yaru, Kunju Wang, Xinyu Ben, Mengsi Tian, Xinyu Liu, Zaihong Li, Panli Ni, Qibing Liu, Zhijian Ma, Xinan Yi, and et al. 2025. "Engineered Exosomes Complexed with Botulinum Toxin Type A for Enhanced Anti-Aging Effects on Skin" Biology 14, no. 8: 1040. https://doi.org/10.3390/biology14081040
APA StyleWang, Y., Wang, K., Ben, X., Tian, M., Liu, X., Li, Z., Ni, P., Liu, Q., Ma, Z., Yi, X., & Guo, Q. (2025). Engineered Exosomes Complexed with Botulinum Toxin Type A for Enhanced Anti-Aging Effects on Skin. Biology, 14(8), 1040. https://doi.org/10.3390/biology14081040






