Curcumin-Rich Diet Mitigates Non-Alcoholic Fatty Liver Disease (NAFLD) by Attenuating Fat Accumulation and Improving Insulin Sensitivity in Aged Female Mice under Nutritional Stress
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals and Treatment
2.2. MRI Imaging
2.3. Body Composition Analysis Using PIXIMUS
2.4. Glucose and Insulin Tolerance Test
2.5. Immunoblotting Analysis
2.6. Hepatic Triglyceride and Cholesterol Measurements
2.7. Histological Analysis
2.8. Real-Time Quantitative Polymerase Chain Reaction (qPCR)
2.9. Statistical Analysis
3. Results
3.1. Curcumin Reduced Body Fat Mass in HFHSD-Fed Aged Female Mice
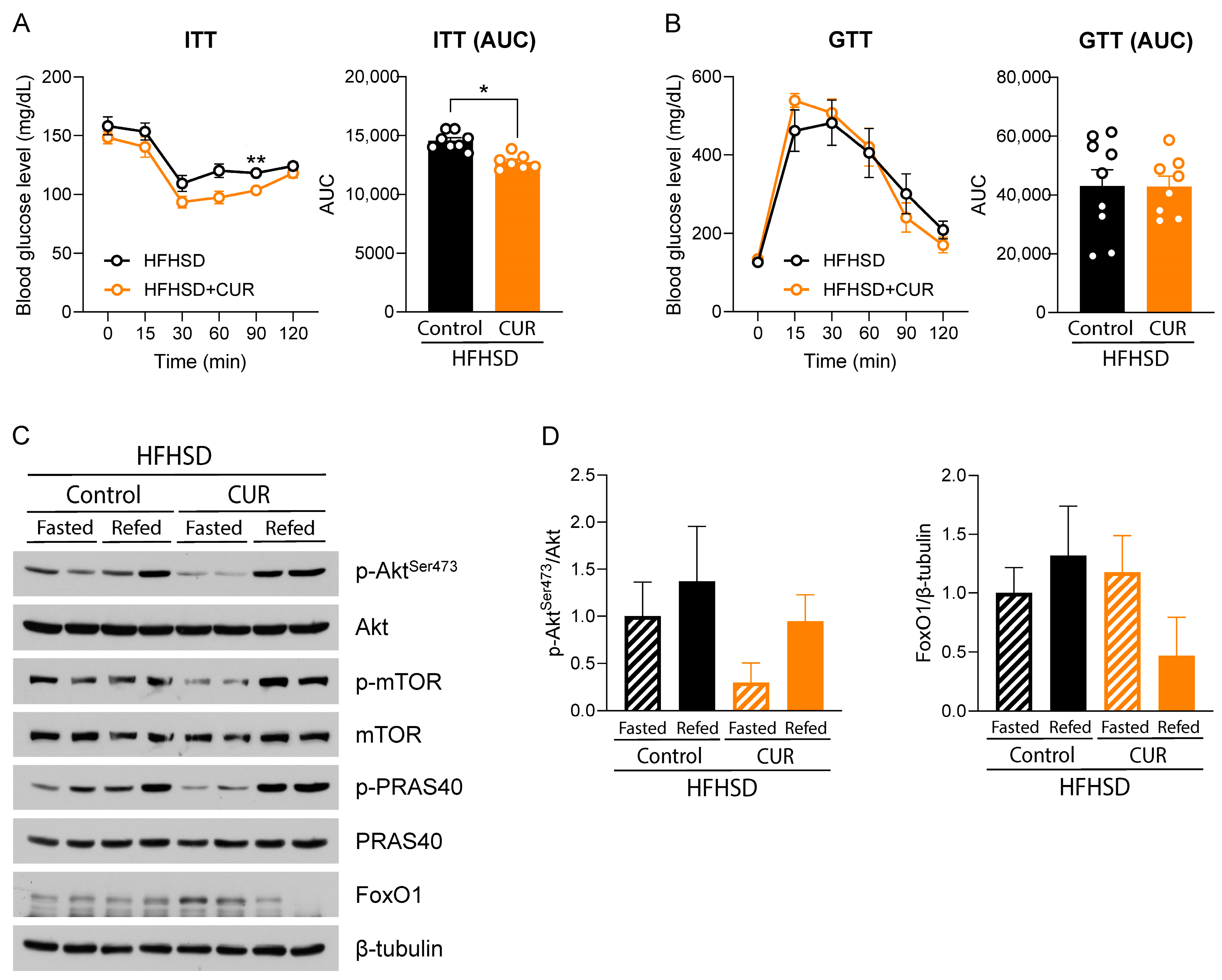
3.2. Curcumin Modulated Hepatic Insulin Signaling in HFHSD-Fed Female Mice
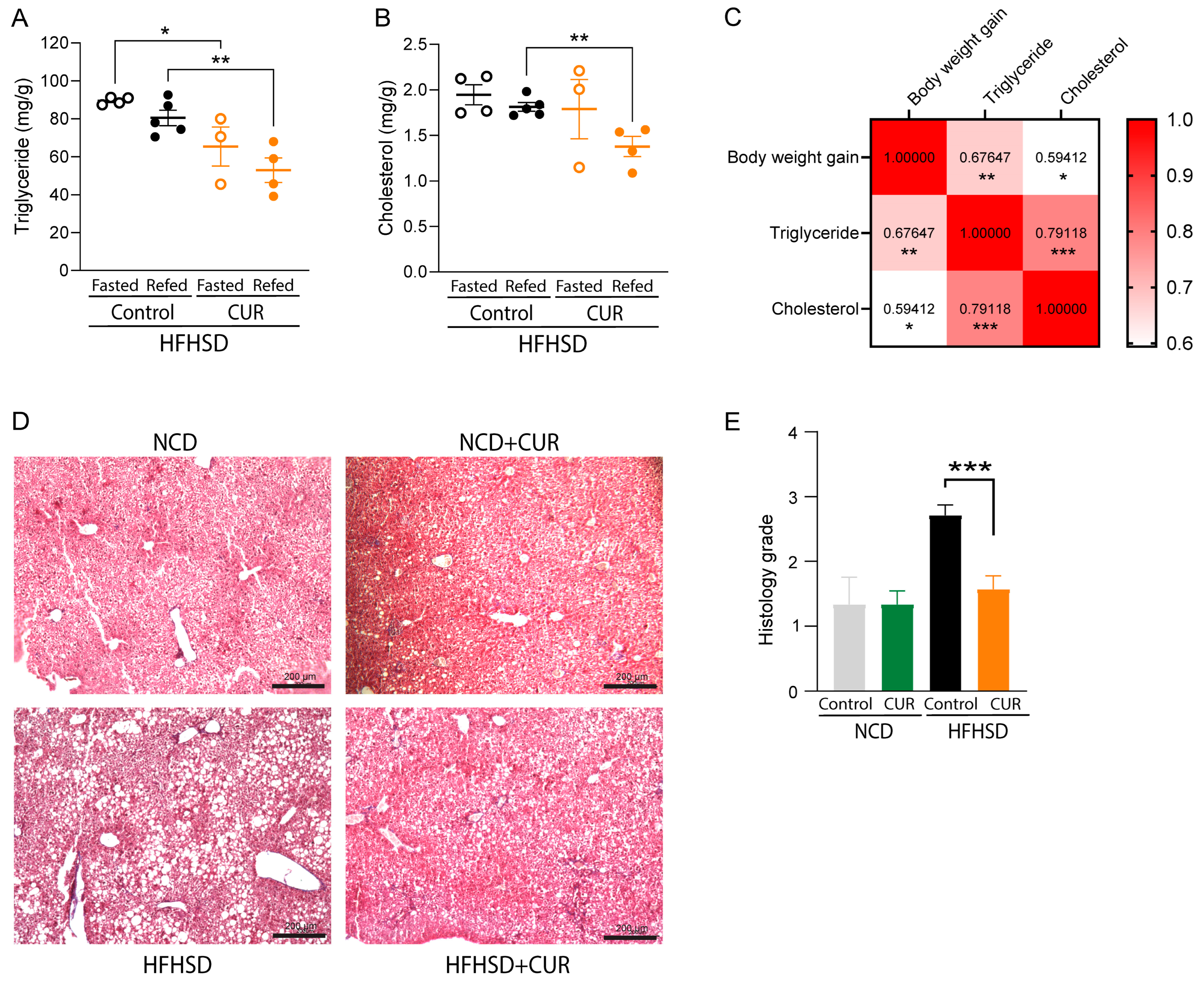
3.3. Curcumin Ameliorated Triglyceride and Cholesterol Deposition in the Liver of HFHSD-Fed Mice
3.4. Curcumin Ameliorated HFHSD-Induced Hepatic Steatosis in Mice
3.5. Curcumin Downregulated Adipogenesis- and Lipogenesis-Related Genes in white Adipose Tissues of Mice
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 14 February 2024).
- Wen, L.; Chen, C.; Zhou, K. Relationship between Abdominal Obesity and Insulin Resistance, Growth Hormone, and Insulin-like Growth Factor-1 in Individuals with Type 2 Diabetes. Cell Mol. Biol. 2022, 68, 36–41. [Google Scholar] [CrossRef]
- Kohrt, W.M.; Kirwan, J.P.; Staten, M.A.; Bourey, R.E.; King, D.S.; Holloszy, J.O. Insulin Resistance in Aging Is Related to Abdominal Obesity. Diabetes 1993, 42, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Suorsa, K.; Gupta, N.; Leskinen, T.; Andersen, L.L.; Pasanen, J.; Hettiarachchi, P.; Johansson, P.J.; Pentti, J.; Vahtera, J.; Stenholm, S. Modifications of 24-h Movement Behaviors to Prevent Obesity in Retirement: A Natural Experiment Using Compositional Data Analysis. Int. J. Obes. 2023, 47, 922–930. [Google Scholar] [CrossRef] [PubMed]
- Kelley, J.A.; Thorpe, R.J. Chapter 11—The Interplay of Age, Period, and Cohort Effects on Obesity and Metabolic Diseases in Later Life. In Handbook of Aging and the Social Sciences, 9th ed.; Ferraro, K.F., Carr, D., Eds.; Handbooks of Aging; Academic Press: Cambridge, MA, USA, 2021; pp. 165–177. ISBN 978-0-12-815970-5. [Google Scholar]
- Pi-Sunyer, X. The Medical Risks of Obesity. Postgrad. Med. 2009, 121, 21–33. [Google Scholar] [CrossRef]
- Friedman, S.L.; Neuschwander-Tetri, B.A.; Rinella, M.; Sanyal, A.J. Mechanisms of NAFLD Development and Therapeutic Strategies. Nat. Med. 2018, 24, 908–922. [Google Scholar] [CrossRef]
- Rinella, M.E.; Sanyal, A.J. Management of NAFLD: A Stage-Based Approach. Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 196–205. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, S.A.; Schattenberg, J.M. NAFLD in the Elderly. Clin. Interv. Aging 2021, 16, 1633–1649. [Google Scholar] [CrossRef]
- Desroches-Castan, A.; Tillet, E.; Ricard, N.; Ouarné, M.; Mallet, C.; Belmudes, L.; Couté, Y.; Boillot, O.; Scoazec, J.-Y.; Bailly, S.; et al. Bone Morphogenetic Protein 9 Is a Paracrine Factor Controlling Liver Sinusoidal Endothelial Cell Fenestration and Protecting Against Hepatic Fibrosis. Hepatology 2019, 70, 1392. [Google Scholar] [CrossRef]
- Park, S.H.; Jeon, W.K.; Kim, S.H.; Kim, H.J.; Park, D.I.; Cho, Y.K.; Sung, I.K.; Sohn, C.I.; Keum, D.K.; Kim, B.I. Prevalence and Risk Factors of Non-Alcoholic Fatty Liver Disease among Korean Adults. J. Gastroenterol. Hepatol. 2006, 21, 138–143. [Google Scholar] [CrossRef]
- Wong, V.W.-S.; Chu, W.C.-W.; Wong, G.L.-H.; Chan, R.S.-M.; Chim, A.M.-L.; Ong, A.; Yeung, D.K.-W.; Yiu, K.K.-L.; Chu, S.H.-T.; Woo, J.; et al. Prevalence of Non-Alcoholic Fatty Liver Disease and Advanced Fibrosis in Hong Kong Chinese: A Population Study Using Proton-Magnetic Resonance Spectroscopy and Transient Elastography. Gut 2012, 61, 409–415. [Google Scholar] [CrossRef]
- Eguchi, Y.; Hyogo, H.; Ono, M.; Mizuta, T.; Ono, N.; Fujimoto, K.; Chayama, K.; Saibara, T. JSG-NAFLD Prevalence and Associated Metabolic Factors of Nonalcoholic Fatty Liver Disease in the General Population from 2009 to 2010 in Japan: A Multicenter Large Retrospective Study. J. Gastroenterol. 2012, 47, 586–595. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Xu, M.; Hu, Z.; Hultström, M.; Lai, E. Sex-Specific Prevalence of Fatty Liver Disease and Associated Metabolic Factors in Wuhan, South Central China. Eur. J. Gastroenterol. Hepatol. 2014, 26, 1015. [Google Scholar] [CrossRef] [PubMed]
- Long, M.T.; Pedley, A.; Massaro, J.M.; Hoffmann, U.; Ma, J.; Loomba, R.; Chung, R.T.; Benjamin, E.J. A Simple Clinical Model Predicts Incident Hepatic Steatosis in a Community-Based Cohort: The Framingham Heart Study. Liver Int. 2018, 38, 1495–1503. [Google Scholar] [CrossRef] [PubMed]
- Govaere, O.; Hasoon, M.; Alexander, L.; Cockell, S.; Tiniakos, D.; Ekstedt, M.; Schattenberg, J.M.; Boursier, J.; Bugianesi, E.; Ratziu, V.; et al. A Proteo-Transcriptomic Map of Non-Alcoholic Fatty Liver Disease Signatures. Nat. Metab. 2023, 5, 572–578. [Google Scholar] [CrossRef] [PubMed]
- Forlano, R.; Sigon, G.; Mullish, B.H.; Yee, M.; Manousou, P. Screening for NAFLD—Current Knowledge and Challenges. Metabolites 2023, 13, 536. [Google Scholar] [CrossRef]
- Masoodi, M.; Gastaldelli, A.; Hyötyläinen, T.; Arretxe, E.; Alonso, C.; Gaggini, M.; Brosnan, J.; Anstee, Q.M.; Millet, O.; Ortiz, P.; et al. Metabolomics and Lipidomics in NAFLD: Biomarkers and Non-Invasive Diagnostic Tests. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 835–856. [Google Scholar] [CrossRef] [PubMed]
- Zuo, Q.; Park, N.H.; Lee, J.K.; Santaliz-Casiano, A.; Madak-Erdogan, Z. Navigating Nonalcoholic Fatty Liver Disease (NAFLD): Exploring the Roles of Estrogens, Pharmacological and Medical Interventions, and Life Style. Steroids 2024, 203, 109330. [Google Scholar] [CrossRef] [PubMed]
- Karimi, R.; Cleven, A.; Elbarbry, F.; Hoang, H. The Impact of Fasting on Major Metabolic Pathways of Macronutrients and Pharmacokinetics Steps of Drugs. Eur. J. Drug Metab. Pharmacokinet. 2021, 46, 25–39. [Google Scholar] [CrossRef] [PubMed]
- Fahed, G.; Aoun, L.; Bou Zerdan, M.; Allam, S.; Bou Zerdan, M.; Bouferraa, Y.; Assi, H.I. Metabolic Syndrome: Updates on Pathophysiology and Management in 2021. Int. J. Mol. Sci. 2022, 23, 786. [Google Scholar] [CrossRef]
- Wu, H.; Ballantyne, C.M. Metabolic Inflammation and Insulin Resistance in Obesity. Circ. Res. 2020, 126, 1549–1564. [Google Scholar] [CrossRef]
- Shou, J.; Chen, P.-J.; Xiao, W.-H. Mechanism of Increased Risk of Insulin Resistance in Aging Skeletal Muscle. Diabetol. Metab. Syndr. 2020, 12, 14. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, B.; Sultana, R.; Greene, M.W. Adipose Tissue and Insulin Resistance in Obese. Biomed. Pharmacother. 2021, 137, 111315. [Google Scholar] [CrossRef]
- Wondmkun, Y.T. Obesity, Insulin Resistance, and Type 2 Diabetes: Associations and Therapeutic Implications. Diabetes Metab. Syndr. Obes. 2020, 13, 3611–3616. [Google Scholar] [CrossRef] [PubMed]
- Koutoukidis, D.A.; Koshiaris, C.; Henry, J.A.; Noreik, M.; Morris, E.; Manoharan, I.; Tudor, K.; Bodenham, E.; Dunnigan, A.; Jebb, S.A.; et al. The Effect of the Magnitude of Weight Loss on Non-Alcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis. Metabolism 2021, 115, 154455. [Google Scholar] [CrossRef] [PubMed]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 8. Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes: Standards of Care in Diabetes—2023. Diabetes Care 2022, 46, S128–S139. [Google Scholar] [CrossRef]
- Li, H.-Y.; Gan, R.-Y.; Shang, A.; Mao, Q.-Q.; Sun, Q.-C.; Wu, D.-T.; Geng, F.; He, X.-Q.; Li, H.-B. Plant-Based Foods and Their Bioactive Compounds on Fatty Liver Disease: Effects, Mechanisms, and Clinical Application. Oxidative Med. Cell. Longev. 2021, 2021, e6621644. [Google Scholar] [CrossRef]
- Sharifi-Rad, J.; Rayess, Y.E.; Rizk, A.A.; Sadaka, C.; Zgheib, R.; Zam, W.; Sestito, S.; Rapposelli, S.; Neffe-Skocińska, K.; Zielińska, D.; et al. Turmeric and Its Major Compound Curcumin on Health: Bioactive Effects and Safety Profiles for Food, Pharmaceutical, Biotechnological and Medicinal Applications. Front. Pharmacol. 2020, 11, 01021. [Google Scholar] [CrossRef]
- Devkota, H.P.; Adhikari-Devkota, A.; Bhandari, D.R. Chapter4.7—Curcumin. In Antioxidants Effects in Health; Nabavi, S.M., Silva, A.S., Eds.; Elsevier: Amsterdam, The Netherlands, 2022; pp. 341–352. ISBN 978-0-12-819096-8. [Google Scholar]
- Lamichhane, G.; Liu, J.; Lee, S.-J.; Lee, D.-Y.; Zhang, G.; Kim, Y. Curcumin Mitigates the High-Fat High-Sugar Diet-Induced Impairment of Spatial Memory, Hepatic Metabolism, and the Alteration of the Gut Microbiome in Alzheimer’s Disease-Induced (3xTg-AD) Mice. Nutrients 2024, 16, 240. [Google Scholar] [CrossRef]
- Lee, S.-J.; Chandrasekran, P.; Mazucanti, C.H.; O’Connell, J.F.; Egan, J.M.; Kim, Y. Dietary Curcumin Restores Insulin Homeostasis in Diet-Induced Obese Aged Mice. Aging 2022, 14, 225. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.-Y.; Lee, S.-J.; Chandrasekaran, P.; Lamichhane, G.; O’Connell, J.F.; Egan, J.M.; Kim, Y. Dietary Curcumin Attenuates Hepatic Cellular Senescence by Suppressing the MAPK/NF-κB Signaling Pathway in Aged Mice. Antioxidants 2023, 12, 1165. [Google Scholar] [CrossRef]
- Plevkova, J.; Brozmanova, M.; Harsanyiova, J.; Sterusky, M.; Honetschlager, J.; Buday, T. Various Aspects of Sex and Gender Bias in Biomedical Research. Physiol. Res. 2020, 69, S367–S378. [Google Scholar] [CrossRef]
- Zucker, I.; Beery, A.K. Males Still Dominate Animal Studies. Nature 2010, 465, 690. [Google Scholar] [CrossRef] [PubMed]
- Muscogiuri, G.; Verde, L.; Vetrani, C.; Barrea, L.; Savastano, S.; Colao, A. Obesity: A Gender-View. J. Endocrinol. Investig. 2024, 47, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Peng, X.-G.; Ju, S.; Qin, Y.; Fang, F.; Cui, X.; Liu, G.; Nicholson, Y.; Teng, G.-J.T. Quantification of Liver Fat in Mice: Comparing Dual-Echo Dixon Imaging, Chemical Shift Imaging, and 1H-MR Spectroscopy. J. Lipid Res. 2011, 52, 1847–1855. [Google Scholar] [CrossRef]
- Sethunath, D.; Morusu, S.; Tuceryan, M.; Cummings, O.W.; Zhang, H.; Yin, X.-M.; Vanderbeck, S.; Chalasani, N.; Gawrieh, S. Automated Assessment of Steatosis in Murine Fatty Liver. PLoS ONE 2018, 13, e0197242. [Google Scholar] [CrossRef]
- Guilherme, A.; Rowland, L.A.; Wetoska, N.; Tsagkaraki, E.; Santos, K.B.; Bedard, A.H.; Henriques, F.; Kelly, M.; Munroe, S.; Pedersen, D.J.; et al. Acetyl-CoA Carboxylase 1 Is a Suppressor of the Adipocyte Thermogenic Program. Cell Rep. 2023, 42, 112488. [Google Scholar] [CrossRef] [PubMed]
- Stamatikos, A.D.; da Silva, R.P.; Lewis, J.T.; Douglas, D.N.; Kneteman, N.M.; Jacobs, R.L.; Paton, C.M. Tissue Specific Effects of Dietary Carbohydrates and Obesity on ChREBPα and ChREBPβ Expression. Lipids 2016, 51, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Phillips, C.M.; Goumidi, L.; Bertrais, S.; Field, M.R.; Cupples, L.A.; Ordovas, J.M.; McMonagle, J.; Defoort, C.; Lovegrove, J.A.; Drevon, C.A.; et al. ACC2 Gene Polymorphisms, Metabolic Syndrome, and Gene-Nutrient Interactions with Dietary Fat. J. Lipid Res. 2010, 51, 3500–3507. [Google Scholar] [CrossRef] [PubMed]
- Jeninga, E.H.; Gurnell, M.; Kalkhoven, E. Functional Implications of Genetic Variation in Human PPARγ. Trends Endocrinol. Metab. 2009, 20, 380–387. [Google Scholar] [CrossRef]
- Xie, C.; Wang, Z.C.; Liu, X.F.; Yang, M.S. The Common Biological Basis for Common Complex Diseases: Evidence from Lipoprotein Lipase Gene. Eur. J. Hum. Genet. 2010, 18, 3–7. [Google Scholar] [CrossRef]
- Han, T.S.; Lean, M.E. A Clinical Perspective of Obesity, Metabolic Syndrome and Cardiovascular Disease. JRSM Cardiovasc. Dis. 2016, 5, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Odermatt, A. The Western-Style Diet: A Major Risk Factor for Impaired Kidney Function and Chronic Kidney Disease. Am. J. Physiol.-Ren. Physiol. 2011, 301, F919–F931. [Google Scholar] [CrossRef] [PubMed]
- De Paoli, M.; Zakharia, A.; Werstuck, G.H. The Role of Estrogen in Insulin Resistance: A Review of Clinical and Preclinical Data. Am. J. Pathol. 2021, 191, 1490–1498. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Rodrigo, C.; Gianzo Citores, M.; Hervás Bárbara, G.; Aranceta-Bartrina, J. Prevalence of Obesity and Abdominal Obesity in Spanish Population Aged 65 Years and over: ENPE Study. Med. Clínica 2022, 158, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Freemantle, N.; Holmes, J.; Hockey, A.; Kumar, S. How Strong Is the Association between Abdominal Obesity and the Incidence of Type 2 Diabetes? Int. J. Clin. Pract. 2008, 62, 1391–1396. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Bhupathiraju, S.N.; de Koning, L.; Hu, F.B. Duration of Obesity and Overweight and Risk of Type 2 Diabetes among US Women. Obesity 2014, 22, 2267–2273. [Google Scholar] [CrossRef]
- Wilding, J.P.H. The Importance of Weight Management in Type 2 Diabetes Mellitus. Int. J. Clin. Pract. 2014, 68, 682–691. [Google Scholar] [CrossRef] [PubMed]
- Home, P.D.; Pacini, G. Hepatic Dysfunction and Insulin Insensitivity in Type 2 Diabetes Mellitus: A Critical Target for Insulin-Sensitizing Agents. Diabetes Obes. Metab. 2008, 10, 699–718. [Google Scholar] [CrossRef]
- Yao, J.; Liu, X.; Sun, Y.; Dong, X.; Liu, L.; Gu, H. Curcumin-Alleviated Osteoarthritic Progression in Rats Fed a High-Fat Diet by Inhibiting Apoptosis and Activating Autophagy via Modulation of MicroRNA-34a. J. Inflamm. Res. 2021, 14, 2317–2331. [Google Scholar] [CrossRef]
- Bideyan, L.; Nagari, R.; Tontonoz, P. Hepatic Transcriptional Responses to Fasting and Feeding. Genes Dev. 2021, 35, 635–657. [Google Scholar] [CrossRef]
- Shao, W.; Yu, Z.; Chiang, Y.; Yang, Y.; Chai, T.; Foltz, W.; Lu, H.; Fantus, I.G.; Jin, T. Curcumin Prevents High Fat Diet Induced Insulin Resistance and Obesity via Attenuating Lipogenesis in Liver and Inflammatory Pathway in Adipocytes. PLoS ONE 2012, 7, e28784. [Google Scholar] [CrossRef]
- Pan, Q.; Ai, W.; Chen, Y.; Kim, D.M.; Shen, Z.; Yang, W.; Jiang, W.; Sun, Y.; Safe, S.; Guo, S. Reciprocal Regulation of Hepatic TGF-Β1 and Foxo1 Controls Gluconeogenesis and Energy Expenditure. Diabetes 2023, 72, 1193–1206. [Google Scholar] [CrossRef]
- Kim, Y.; Rouse, M.; González-Mariscal, I.; Egan, J.M.; O’Connell, J.F. Dietary Curcumin Enhances Insulin Clearance in Diet-Induced Obese Mice via Regulation of Hepatic PI3K-AKT Axis and IDE, and Preservation of Islet Integrity. Nutr. Metab. 2019, 16, 48. [Google Scholar] [CrossRef]
- Meneses, M.J.; Sousa-Lima, I.; Jarak, I.; Raposo, J.F.; Alves, M.G.; Macedo, M.P. Distinct Impacts of Fat and Fructose on the Liver, Muscle, and Adipose Tissue Metabolome: An Integrated View. Front. Endocrinol. 2022, 13, 898471. [Google Scholar] [CrossRef]
- López-Otín, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. The Hallmarks of Aging. Cell 2013, 153, 1194–1217. [Google Scholar] [CrossRef]
- Kim, C.-W.; Moon, Y.-A.; Park, S.W.; Cheng, D.; Kwon, H.J.; Horton, J.D. Induced Polymerization of Mammalian Acetyl-CoA Carboxylase by MIG12 Provides a Tertiary Level of Regulation of Fatty Acid Synthesis. Proc. Natl. Acad. Sci. USA 2010, 107, 9626–9631. [Google Scholar] [CrossRef]
- Iizuka, K.; Takao, K.; Yabe, D. ChREBP-Mediated Regulation of Lipid Metabolism: Involvement of the Gut Microbiota, Liver, and Adipose Tissue. Front. Endocrinol. 2020, 11, 587189. [Google Scholar] [CrossRef]
- Janani, C.; Ranjitha Kumari, B.D. PPAR Gamma Gene—A Review. Diabetes Metab. Syndr. Clin. Res. Rev. 2015, 9, 46–50. [Google Scholar] [CrossRef]
- Altalebi, R.R.; Al-hussaniy, H.A.; Al-tameemi, Z.S.; AL-Zobaidy, M.A.-H.; Albu-Rghaif, A.H.; Alkuraishy, H.M.; Hedeab, G.M.; Azam, F.; Al-Samydai, A.M.; Naji, M.A. Non-Alcoholic Fatty Liver Disease: Relation to Juvenile Obesity, Lipid Profile, and Hepatic Enzymes. J. Med. Life 2023, 16, 42–47. [Google Scholar] [CrossRef]
- Azzu, V.; Vacca, M.; Virtue, S.; Allison, M.; Vidal-Puig, A. Adipose Tissue-Liver Cross Talk in the Control of Whole-Body Metabolism: Implications in Nonalcoholic Fatty Liver Disease. Gastroenterology 2020, 158, 1899–1912. [Google Scholar] [CrossRef]
- Wang, L.; Yi, J.; Guo, J.; Ren, X. Weigh Change across Adulthood Is Related to the Presence of NAFLD: Results from NHANES III. J. Transl. Med. 2023, 21, 142. [Google Scholar] [CrossRef]
- Li, S.; You, J.; Wang, Z.; Liu, Y.; Wang, B.; Du, M.; Zou, T. Curcumin Alleviates High-Fat Diet-Induced Hepatic Steatosis and Obesity in Association with Modulation of Gut Microbiota in Mice. Food Res. Int. 2021, 143, 110270. [Google Scholar] [CrossRef]
- Voshol, P.J.; Haemmerle, G.; Ouwens, D.M.; Zimmermann, R.; Zechner, R.; Teusink, B.; Maassen, J.A.; Havekes, L.M.; Romijn, J.A. Increased Hepatic Insulin Sensitivity Together with Decreased Hepatic Triglyceride Stores in Hormone-Sensitive Lipase-Deficient Mice. Endocrinology 2003, 144, 3456–3462. [Google Scholar] [CrossRef][Green Version]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lamichhane, G.; Lee, D.-Y.; Franks, R.; Olawale, F.; Jin, J.-B.; Egan, J.M.; Kim, Y. Curcumin-Rich Diet Mitigates Non-Alcoholic Fatty Liver Disease (NAFLD) by Attenuating Fat Accumulation and Improving Insulin Sensitivity in Aged Female Mice under Nutritional Stress. Biology 2024, 13, 472. https://doi.org/10.3390/biology13070472
Lamichhane G, Lee D-Y, Franks R, Olawale F, Jin J-B, Egan JM, Kim Y. Curcumin-Rich Diet Mitigates Non-Alcoholic Fatty Liver Disease (NAFLD) by Attenuating Fat Accumulation and Improving Insulin Sensitivity in Aged Female Mice under Nutritional Stress. Biology. 2024; 13(7):472. https://doi.org/10.3390/biology13070472
Chicago/Turabian StyleLamichhane, Gopal, Da-Yeon Lee, Rienna Franks, Femi Olawale, Jong-Beom Jin, Josephine M. Egan, and Yoo Kim. 2024. "Curcumin-Rich Diet Mitigates Non-Alcoholic Fatty Liver Disease (NAFLD) by Attenuating Fat Accumulation and Improving Insulin Sensitivity in Aged Female Mice under Nutritional Stress" Biology 13, no. 7: 472. https://doi.org/10.3390/biology13070472
APA StyleLamichhane, G., Lee, D.-Y., Franks, R., Olawale, F., Jin, J.-B., Egan, J. M., & Kim, Y. (2024). Curcumin-Rich Diet Mitigates Non-Alcoholic Fatty Liver Disease (NAFLD) by Attenuating Fat Accumulation and Improving Insulin Sensitivity in Aged Female Mice under Nutritional Stress. Biology, 13(7), 472. https://doi.org/10.3390/biology13070472






