Impact of Multidisciplinary Team Management on Survival and Recurrence in Stage I–III Colorectal Cancer: A Population-Based Study in Northern Italy
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Multidisciplinary Team
2.3. Statistical Analysis
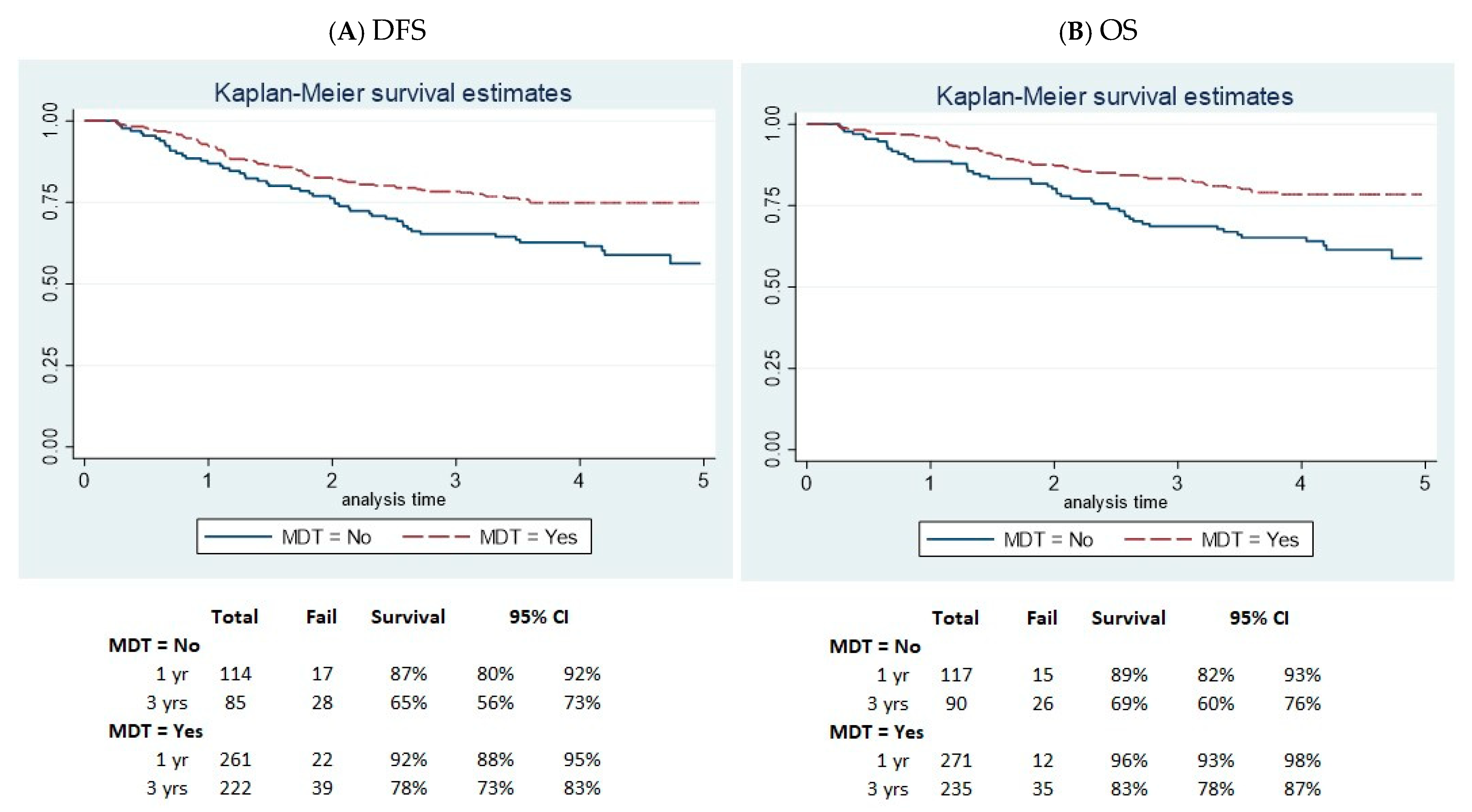
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef] [PubMed]
- Brenner, H.; Chen, C. The colorectal cancer epidemic: Challenges and opportunities for primary, secondary and tertiary prevention. Br. J. Cancer 2018, 119, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Rossi, P.G.; Vicentini, M.; Sacchettini, C.; Di Felice, E.; Caroli, S.; Ferrari, F.; Mangone, L.; Pezzarossi, A.; Roncaglia, F.; Campari, C.; et al. Impact of Screening Program on Incidence of Colorectal Cancer: A Cohort Study in Italy. Am. J. Gastroenterol. 2015, 110, 1359–1366. [Google Scholar] [CrossRef] [PubMed]
- Adigun, A.O.; Adebile, T.M.; Okoye, C.; Ogundipe, T.I.; Ajekigbe, O.R.; Mbaezue, R.N.; Okobi, O.E. Causes and Prevention of Early-Onset Colorectal Cancer. Cureus 2023, 15, e45095. [Google Scholar] [CrossRef] [PubMed]
- Mangone, L.; Marinelli, F.; Bisceglia, I.; Braghiroli, M.B.; Damato, A.; Pinto, C. Five-year relative survival by stage of breast and colon cancers in northern Italy. Front. Oncol. 2022, 12, 982461. [Google Scholar] [CrossRef]
- Majek, O.; Gondos, A.; Jansen, L.; Emrich, K.; Holleczek, B.; Katalinic, A.; Nennecke, A.; Eberle, A.; Brenner, H.; GEKID Cancer Survival Working Group. Survival from colorectal cancer in Germany in the early 21st century. Br. J. Cancer 2012, 106, 1875–1880. [Google Scholar] [CrossRef]
- Bekaii-Saab, T. A decade of progress: Advances in the third-line treatment of patients with metastatic colorectal cancer. Am. J. Manag. Care 2024, 30 (Suppl. S2), S23–S30. [Google Scholar] [CrossRef]
- Gmeiner, W.H. Recent Advances in Therapeutic Strategies to Improve Colorectal Cancer Treatment. Cancers 2024, 16, 1029. [Google Scholar] [CrossRef] [PubMed]
- Dulskas, A.; Gaizauskas, V.; Kildusiene, I.; Samalavicius, N.E.; Smailyte, G. Improvement of Survival over Time for Colorectal Cancer Patients: A Population-Based Study. J. Clin. Med. 2020, 9, 4038. [Google Scholar] [CrossRef]
- Cardoso, R.; Guo, F.; Heisser, T.; De Schutter, H.; Van Damme, N.; Nilbert, M.C.; Christensen, J.; Bouvier, A.-M.; Bouvier, V.; Launoy, G.; et al. Overall and stage-specific survival of patients with screen-detected colorectal cancer in European countries: A population-based study in 9 countries. Lancet Reg. Health Eur. 2022, 21, 100458. [Google Scholar] [CrossRef]
- Luu, X.Q.; Lee, K.; Jun, J.K.; Suh, M.; Jung, K.; Choi, K.S. Effect of colorectal cancer screening on long-term survival of colorectal cancer patients: Results of the Korea National Cancer Screening Program. Int. J. Cancer 2022, 150, 1958–1967. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhao, L.; Güngör, C.; Tan, F.; Zhou, Z.; Li, C.; Song, X.; Wang, D.; Pei, Q.; Liu, W. The main contributor to the upswing of survival in locally advanced colorectal cancer: An analysis of the SEER database. Ther. Adv. Gastroenterol. 2019, 12, 1756284819862154. [Google Scholar] [CrossRef] [PubMed]
- Alese, O.B.; Wu, C.; Chapin, W.J.; Ulanja, M.B.; Zheng-Lin, B.; Amankwah, M.; Eads, J. Update on Emerging Therapies for Advanced Colorectal Cancer. Am. Soc. Clin. Oncol. Educ. Book 2023, 43, e389574. [Google Scholar] [CrossRef] [PubMed]
- Layfield, D.M.; Flashman, K.G.; Benitez Majano, S.; Senapati, A.; Ball, C.; Conti, J.A.; Khan, J.S.; O’Leary, D.P. Changing patterns of multi-disciplinary team treatment, early mortality, and survival in colorectal cancer. BJS Open. 2022, 6, zrac098. [Google Scholar] [CrossRef]
- Zhang, H.; Yu, J.; Wei, Z.; Wu, W.; Zhang, C.; He, Y. The Effect of Multidisciplinary Team Discussion Intervention on the Prognosis of Advanced Colorectal Cancer. J. Cancer 2021, 12, 3307–3314. [Google Scholar] [CrossRef]
- Peng, D.; Cheng, Y.X.; Cheng, Y. Improved Overall Survival of Colorectal Cancer under Multidisciplinary Team: A Meta-Analysis. Biomed Res. Int. 2021, 2021, 5541613. [Google Scholar] [CrossRef]
- Fehervari, M.; Hamrang-Yousefi, S.; Fadel, M.G.; Mills, S.C.; Warren, O.J.; Tekkis, P.P.; Kontovounisios, C. A systematic review of colorectal multidisciplinary team meetings: An international comparison. BJS Open 2021, 5, zrab044. [Google Scholar] [CrossRef]
- Reboux, N.; Cadieu, E.; Pruvost-Couvreur, M.; Cariou, M.; Kermarrec, M.; Kermarrec, T.; Bouzeloc, S.; Nousbaum, J.-B.; Robaszkiewicz, M.; Quénéhervé, L. Factors associated with non-presentation in a multidisciplinary team meeting for colon cancer: A matched retrospective cohort study in a French area. Clin. Res. Hepatol. Gastroenterol. 2022, 46, 101950. [Google Scholar] [CrossRef]
- Carvello, M.; Bellato, V.; Maroli, A.; Hart, A.; Danese, S.; Warusavitarne, J.; Spinelli, A. A Multidisciplinary Approach to Rectal Cancer Treatment in Ulcerative Colitis Results in High Rate of Restorative Minimally Invasive Surgery. J. Crohn’s Colitis 2022, 16, 244–250. [Google Scholar] [CrossRef]
- Chen, Y.; Xu, M.; Ye, Q.; Xiang, J.; Xue, T.; Yang, T.; Liu, L.; Yan, B. Irregular delay of adjuvant chemotherapy correlated with poor outcome in stage II-III colorectal cancer. BMC Cancer 2022, 22, 670. [Google Scholar] [CrossRef]
- MacDermid, E.; Hooton, G.; MacDonald, M.; McKay, G.; Grose, D.; Mohammed, N.; Porteous, C. Improving patient survival with the colorectal cancer multi-disciplinary team. Color. Dis. 2009, 11, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Munro, A.; Brown, M.; Niblock, P.; Steele, R.; Carey, F. Do Multidisciplinary Team (MDT) processes influence survival in patients with colorectal cancer? A population-based experience. BMC Cancer 2015, 15, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Segelman, J.; Singnomklao, T.; Hellborg, H.; Martling, A. Differences in multidisciplinary team assessment and treatment between patients with stage IV colon and rectal cancer. Color. Dis. 2009, 11, 768–774. [Google Scholar] [CrossRef] [PubMed]
- Rollet, Q.; Bouvier, V.; Moutel, G.; Launay, L.; Bignon, A.-L.; Bouhier-Leporrier, K.; Launoy, G.; Lièvre, A. Multidisciplinary team meetings: Are all patients presented and does it impact quality of care and survival—A registry-based study. BMC Health Serv. Res. 2021, 21, 1032. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.oncomel.org/fichs/11085.pdf (accessed on 21 August 2024).
- Bouvier, A.-M.; Bauvin, E.; Danzon, A.; Grosclaude, P.; Delafosse, P.; Buémi, A.; Trétarre, B.; Raverdy, N.; Maarouf, N.; Velten, M.; et al. Place of multidisciplinary consulting meetings and clinical trials in the management of colorectal cancer in France in 2000. Gastroenterol. Clin. Biol. 2007, 31, 286–291. [Google Scholar] [CrossRef]
- Mangone, L.; Borciani, E.; Michiara, M.; Vicentini, M.; Carrozzi, G.; Mancuso, P.; Sacchettini, C.; Giorgi Rossi, P. I Tumori Nelle Province Dell’area Vasta Emilia Nord: Piacenza, Parma, Reggio Emilia e Modena: Anni 2013–2014; I Registri Tumori: Modena, Italy, 2015. [Google Scholar]
- Fritz, A.; Percy, C.; Jack, A.; Shanmugaratnam, K.; Sobin, L.; Parkin, D.M.; Whelan, S. International Classification of Disease for Oncology, 3rd ed.; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Sobin, L.; Gospodarowicz, M.; Wittekind, C. TNM Classification of Malignant Tumours. In UICC, 8th ed.; Raffaello Cortina Editore: Milano, Italy, 2017. [Google Scholar]
- Siriwardena, A.K.; Serrablo, A.; Fretland, Å.A.; Wigmore, S.J.; Ramia-Angel, J.M.; Malik, H.Z.; Stättner, S.; Søreide, K.; Zmora, O.; Meijerink, M.; et al. Multisocietal European consensus on the terminology, diagnosis, and management of patients with synchronous colorectal cancer and liver metastases: An E-AHPBA consensus in partnership with ESSO, ESCP, ESGAR, and CIRSE. Br. J. Surg. 2023, 110, 1161–1170. [Google Scholar] [CrossRef]
- Lin, W.-L.; Sun, J.-L.; Chang, S.-C.; Tsai, T.-C.; Wu, P.-H.; Huang, W.-T.; Tsao, C.-J.; Lin, C.-L. Effectiveness of the Multidisciplinary Team Model in Treating Colorectal Cancer. Gastroenterol. Nurs. 2018, 41, 491–496. [Google Scholar] [CrossRef]
- Harji, D.P.; Houston, F.; Cutforth, I.; Hawthornthwaite, E.; McKigney, N.; Sharpe, A.; Coyne, P.; Griffiths, B. The impact of multidisci-plinary team decision-making in locally advanced and recurrent rectal cancer. Ann. R. Coll. Surg. Engl. 2022, 104, 611–617. [Google Scholar] [CrossRef]
- Whitehouse, M. A policy framework commissioning cancer services. BMJ 1995, 310, 22293. [Google Scholar] [CrossRef]
- Kelly, M.J.; Lloyd, T.D.R.; Marshall, D.; Garcea, G.; Sutton, C.D.; Beach, M. A snapshot of MDT working and patient mapping in the UK colorectal cancer centres in 2002. Color. Dis. 2003, 5, 577–581. [Google Scholar] [CrossRef]
- Taylor, C.; Sippitt, J.M.; Collins, G.; McManus, C.; Richardson, A.; Dawson, J.; Richards, M.; Ramirez, A.J. A pre-post test evaluation of the impact of the PELICAN MDT-TME Development Programme on the working lives of colorectal cancer team members. BMC Health Serv. Res. 2010, 10, 187. [Google Scholar] [CrossRef] [PubMed]
- OECD. Health at a Glance. 2019. Available online: https://www.oecdilibrary.org/content/publication/4dd50c09-en (accessed on 21 August 2024).
- Carinci, F.; Van Gool, K.; Mainz, J.; Veillard, J.; Pichora, E.C.; Januel, J.M.; Arispe, I.; Kim, S.M.; Klazinga, N.; OECD Health Care Quality Indicators Expert Group. Towards actionable international comparisons of health system performance: Expert revision of the OECD framework and quality indicators. Int. J. Qual. Health Care 2015, 27, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Mangone, L.; Marinelli, F.; Bisceglia, I.; Braghiroli, M.B.; Mastrofilippo, V.; Pezzarossi, A.; Morabito, F.; Aguzzoli, L.; Mandato, V.D. Optimizing Outcomes through a Multidisciplinary Team Approach in Endometrial Cancer. Healthcare 2023, 12, 64. [Google Scholar] [CrossRef] [PubMed]
- Taberna, M.; Gil Moncayo, F.; Jané-Salas, E.; Antonio, M.; Arribas, L.; Vilajosana, E.; Torres, E.P.; Mesía, R. The Multidisciplinary Team (MDT) Approach and Quality of Care. Front. Oncol. 2020, 10, 85. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.M.; Hong, Y.S.; Kim, T.W.; Park, J.; Kim, J.H.; Park, S.H.; Kim, A.Y.; Lim, S.; Lee, Y.; Yu, C.S. Impact of a Multidisciplinary Team Approach for Managing Advanced and Recurrent Colorectal Cancer. World J. Surg. 2018, 42, 2227–2233. [Google Scholar] [CrossRef] [PubMed]
- Viñal, D.; Martinez-Recio, S.; Martinez-Perez, D.; Ruiz-Gutierrez, I.; Jimenez-Bou, D.; Peña-Lopez, J.; Alameda-Guijarro, M.; Martin-Montalvo, G.; Rueda-Lara, A.; Gutierrez-Sainz, L.; et al. Clinical Score to Predict Recurrence in Patients with Stage II and Stage III Colon Cancer. Cancers 2022, 14, 5891. [Google Scholar] [CrossRef]
- Nors, J.; Iversen, L.H.; Erichsen, R.; Gotschalck, K.A.; Andersen, C.L. Incidence of Recurrence and Time to Recurrence in Stage I to III Colorectal Cancer: A Nationwide Danish Cohort Study. JAMA Oncol. 2024, 10, 54–62. [Google Scholar] [CrossRef]
- Paik, J.-H.; Ryu, C.-G.; Hwang, D.-Y. Risk factors of recurrence in TNM stage I colorectal cancer. Ann. Surg. Treat. Res. 2023, 104, 281–287. [Google Scholar] [CrossRef]
- Qaderi, S.M.; Galjart, B.; Verhoef, C.; Slooter, G.D.; Koopman, M.; Verhoeven, R.H.A.; de Wilt, J.H.W.; van Erning, F.N. Disease recurrence after colorectal cancer surgery in the modern era: A population-based study. Int. J. Color. Dis. 2021, 36, 2399–2410. [Google Scholar] [CrossRef]
- Nikolic, N.; Radosavljevic, D.; Gavrilovic, D.; Nikolic, V.; Stanic, N.; Spasic, J.; Cacev, T.; Castellvi-Bel, S.; Cavic, M.; Jankovic, G. Prognostic Factors for Post-Recurrence Survival in Stage II and III Colorectal Carcinoma Patients. Medicina 2021, 57, 1108. [Google Scholar] [CrossRef]
- Kaprio, T.; Hansen, T.F.; Glimelius, B.; Böckelman, C.; Engelmann, B.E. Risk of recurrence in patients with colon cancer stage II and III: A systematic review and meta-analysis of recent literature. Acta Oncol. 2015, 54, 5–16. [Google Scholar] [CrossRef]
- Rosander, E.; Holm, T.; Sjövall, A.; Hjern, F.; Weibull, C.; Nordenvall, C. Preoperative multidisciplinary team assessment is associated with improved survival in patients with locally advanced colon cancer; a nationwide cohort study in 3157 patients. Eur. J. Surg. Oncol. 2021, 47, 2398–2404. [Google Scholar] [CrossRef] [PubMed]
- AIOM; AIRTUM; Fondazione AIOM; PASSI. I Numeri del Cancro in Italia, 2018; Intermedia Editore: Brescia, Italy, 2018. [Google Scholar]
- Campari, C.; Sassatelli, R.; Paterlini, L.; Camellini, L.; Menozzi, P.; Cattani, A. Sensibilità del test immunochimico e del programma nello screening del cancro del colon retto nella provincia di Reggio Emilia [Test and programme sensitivities of screening for colorectal cancer in Reggio Emilia]. Epidemiol. Prev. 2011, 35, 118–124. (In Italian) [Google Scholar] [PubMed]
| MDT | p-Value | ||||||
|---|---|---|---|---|---|---|---|
| Yes | No | ||||||
| n | % | n | % | n | % | ||
| Overall | 460 | 100 | 300 | 65.2 | 160 | 34.8 | |
| Age at diagnosis (group) | |||||||
| <50 | 25 | 5.4 | 19 | 6.3 | 6 | 3.8 | |
| 50–69 | 149 | 32.4 | 100 | 33.4 | 49 | 30.6 | 0.37 |
| 70+ | 286 | 62.2 | 181 | 60.3 | 105 | 65.6 | |
| Year | |||||||
| 2017 | 244 | 53.0 | 136 | 45.3 | 108 | 67.5 | <0.01 |
| 2018 | 216 | 47.0 | 164 | 54.7 | 52 | 32.5 | |
| Gender | |||||||
| Male | 263 | 57.2 | 171 | 57.0 | 92 | 57.5 | 0.92 |
| Female | 197 | 42.8 | 129 | 43.0 | 68 | 42.5 | |
| Site | |||||||
| Colon | 337 | 73.3 | 208 | 69.3 | 129 | 80.6 | <0.01 |
| Rectum | 123 | 26.7 | 92 | 30.7 | 31 | 19.4 | |
| Stage | |||||||
| I | 146 | 31.7 | 110 | 36.6 | 36 | 22.5 | <0.01 |
| II | 166 | 36.1 | 101 | 33.7 | 65 | 40.6 | |
| III | 148 | 32.2 | 89 | 29.7 | 59 | 36.9 | |
| Surgery | |||||||
| Yes | 342 | 74.4 | 235 | 78.3 | 107 | 66.9 | <0.05 |
| No | 85 | 18.5 | 44 | 14.7 | 41 | 25.6 | |
| Unknown | 33 | 7.1 | 21 | 7.0 | 12 | 7.5 | |
| Chemotherapy | |||||||
| Yes | 124 | 27.0 | 89 | 29.7 | 35 | 21.9 | 0.20 |
| No | 303 | 65.9 | 190 | 63.3 | 113 | 70.6 | |
| Unknown | 33 | 7.1 | 21 | 7.0 | 12 | 7.5 | |
| MDT | |||||
|---|---|---|---|---|---|
| Yes (n = 282) | No (n = 132) | p-Value | |||
| n | % | n | % | ||
| Age at diagnosis (group) | |||||
| <50 | 18 | 6.4 | 6 | 4.5 | 0.71 |
| 50–69 | 99 | 35.1 | 45 | 34.1 | |
| 70+ | 165 | 58.5 | 81 | 61.4 | |
| Gender | |||||
| Male | 162 | 57.5 | 72 | 54.5 | 0.58 |
| Female | 120 | 42.5 | 60 | 45.5 | |
| Stage | |||||
| I | 108 | 38.3 | 31 | 23.5 | <0.05 |
| II | 96 | 34.0 | 59 | 44.7 | |
| III | 78 | 27.7 | 42 | 31.8 | |
| Recurrences | |||||
| Yes | 24 | 8.5 | 13 | 9.9 | 0.56 |
| No | 255 | 90.4 | 116 | 87.9 | |
| Unknown | 3 | 1.1 | 3 | 2.3 | |
| Only patients with recurrence | Yes (n = 24) | No (n = 13) | p-value | ||
| n | % | n | % | ||
| Stage | |||||
| I | 4 | 3.7 | 0 | 0.0 | 0.28 |
| II–III | 20 | 11.5 | 13 | 12.9 | |
| Site | |||||
| Liver | 8 | 33.3 | 6 | 46.2 | 0.73 |
| Lung | 5 | 20.8 | 3 | 23.1 | |
| Lymph nodes | 3 | 12.5 | 0 | 0.0 | |
| Peritoneum | 8 | 33.3 | 4 | 30.7 | |
| Months | |||||
| 6–12 | 11 | 45.8 | 4 | 30.8 | 0.38 |
| 12+ | 13 | 54.2 | 9 | 69.2 | |
| Characteristics | Disease-Free Survival | Overall Survival | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Stage | ||||||
| I | 1.00 | Ref. | 1.00 | Ref. | ||
| II | 1.30 | 0.79–2.14 | 0.30 | 1.16 | 0.69–1.97 | 0.57 |
| III | 2.79 | 1.74–4.49 | <0.01 | 2.50 | 1.52–4.10 | <0.01 |
| Age at diagnosis | ||||||
| <50 | 1.00 | Ref. | 1.00 | Ref. | ||
| 50–69 | 1.36 | 0.40–4.57 | 0.62 | 1.52 | 0.35–6.61 | 0.58 |
| 70+ | 4.09 | 1.29–12.98 | <0.05 | 5.23 | 1.28–21.35 | <0.05 |
| Gender | ||||||
| Female | 1.00 | Ref. | 1.00 | Ref. | ||
| Male | 1.14 | 0.80–1.64 | 0.47 | 1.06 | 0.72–1.56 | 0.77 |
| MDT | ||||||
| Yes | 1.00 | Ref. | 1.00 | Ref. | ||
| No | 1.66 | 1.14–2.41 | <0.01 | 1.96 | 1.31–2.91 | <0.01 |
| Year | ||||||
| 2017 | 1.00 | Ref. | 1.00 | Ref. | ||
| 2018 | 1.19 | 0.82–1.75 | 0.36 | 1.32 | 0.88–1.98 | 0.19 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mangone, L.; Zizzo, M.; Nardecchia, M.; Marinelli, F.; Bisceglia, I.; Braghiroli, M.B.; Banzi, M.C.; Damato, A.; Cerullo, L.; Pellegri, C.; et al. Impact of Multidisciplinary Team Management on Survival and Recurrence in Stage I–III Colorectal Cancer: A Population-Based Study in Northern Italy. Biology 2024, 13, 928. https://doi.org/10.3390/biology13110928
Mangone L, Zizzo M, Nardecchia M, Marinelli F, Bisceglia I, Braghiroli MB, Banzi MC, Damato A, Cerullo L, Pellegri C, et al. Impact of Multidisciplinary Team Management on Survival and Recurrence in Stage I–III Colorectal Cancer: A Population-Based Study in Northern Italy. Biology. 2024; 13(11):928. https://doi.org/10.3390/biology13110928
Chicago/Turabian StyleMangone, Lucia, Maurizio Zizzo, Melissa Nardecchia, Francesco Marinelli, Isabella Bisceglia, Maria Barbara Braghiroli, Maria Chiara Banzi, Angela Damato, Loredana Cerullo, Carlotta Pellegri, and et al. 2024. "Impact of Multidisciplinary Team Management on Survival and Recurrence in Stage I–III Colorectal Cancer: A Population-Based Study in Northern Italy" Biology 13, no. 11: 928. https://doi.org/10.3390/biology13110928
APA StyleMangone, L., Zizzo, M., Nardecchia, M., Marinelli, F., Bisceglia, I., Braghiroli, M. B., Banzi, M. C., Damato, A., Cerullo, L., Pellegri, C., Morabito, F., Neri, A., Fabozzi, M., Pinto, C., & Giorgi Rossi, P. (2024). Impact of Multidisciplinary Team Management on Survival and Recurrence in Stage I–III Colorectal Cancer: A Population-Based Study in Northern Italy. Biology, 13(11), 928. https://doi.org/10.3390/biology13110928








