Comparisons of the Oral Microbiota from Seven Species of Wild Venomous Snakes in Taiwan Using the High-Throughput Amplicon Sequencing of the Full-Length 16S rRNA Gene
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
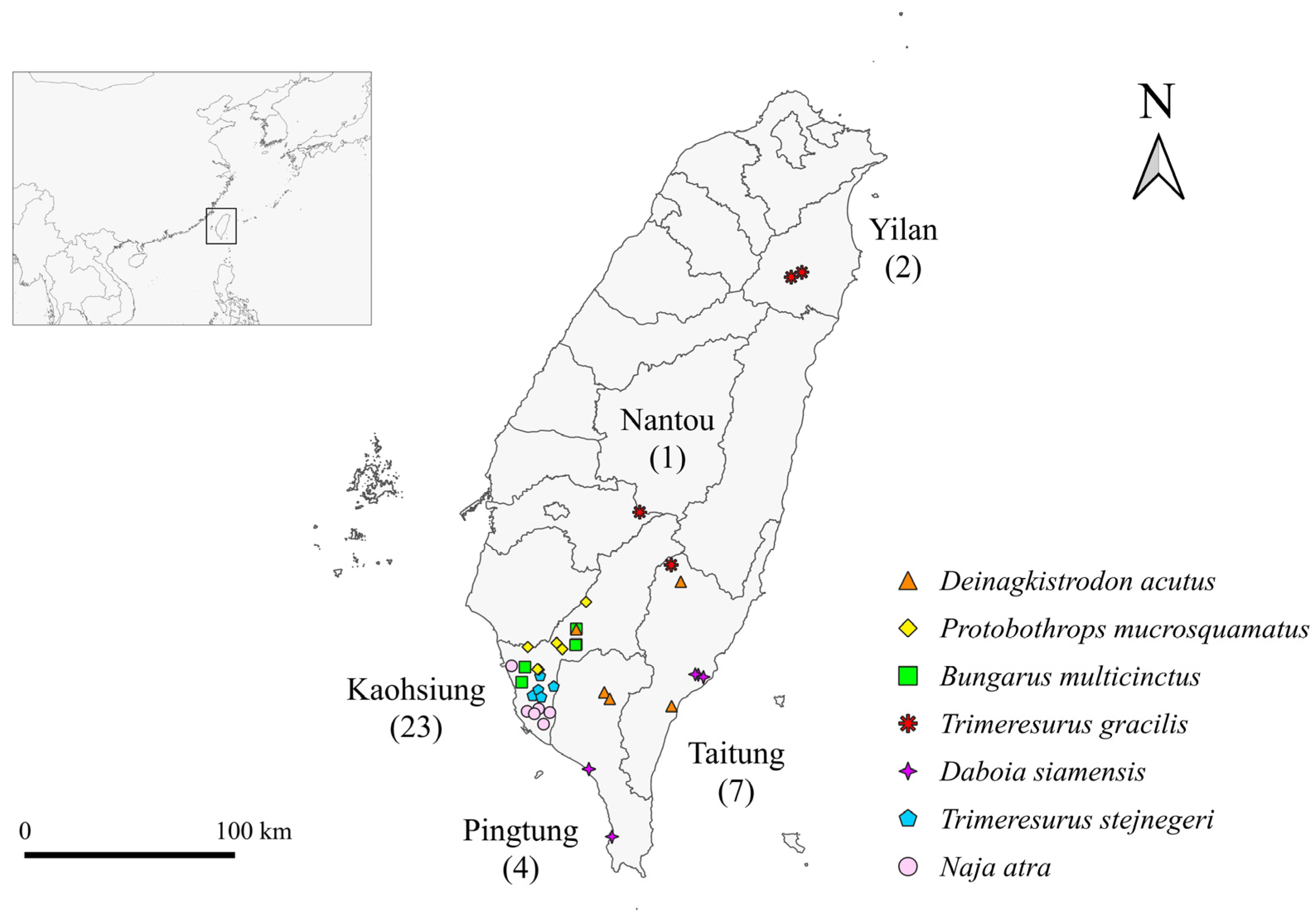
2.1. Sample Collection
2.2. DNA Extraction, PCR Amplification, and Purification
2.3. SMRTbell Library Construction and Sequencing
2.4. Data Analysis
3. Results
3.1. Sequence Analysis
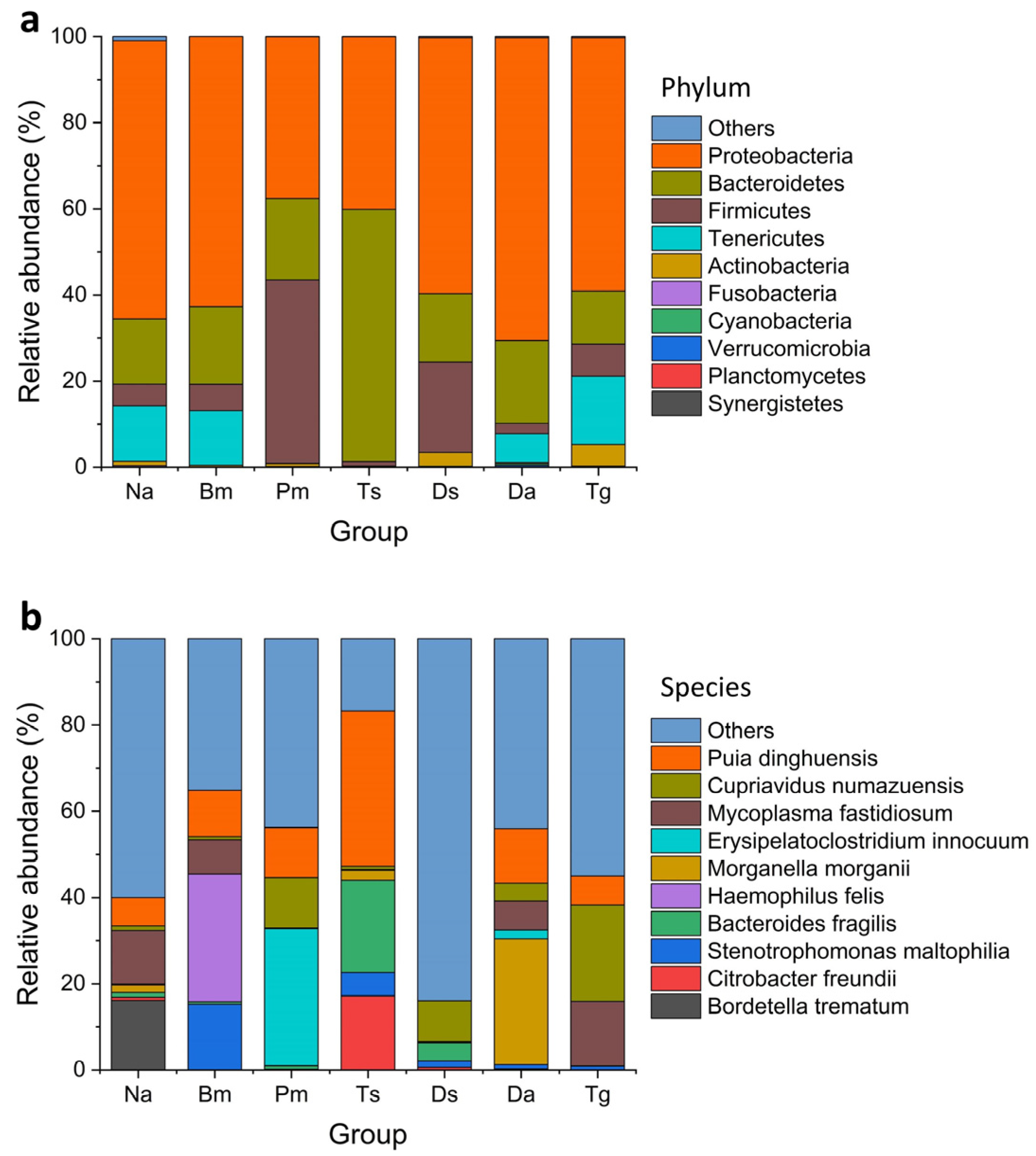
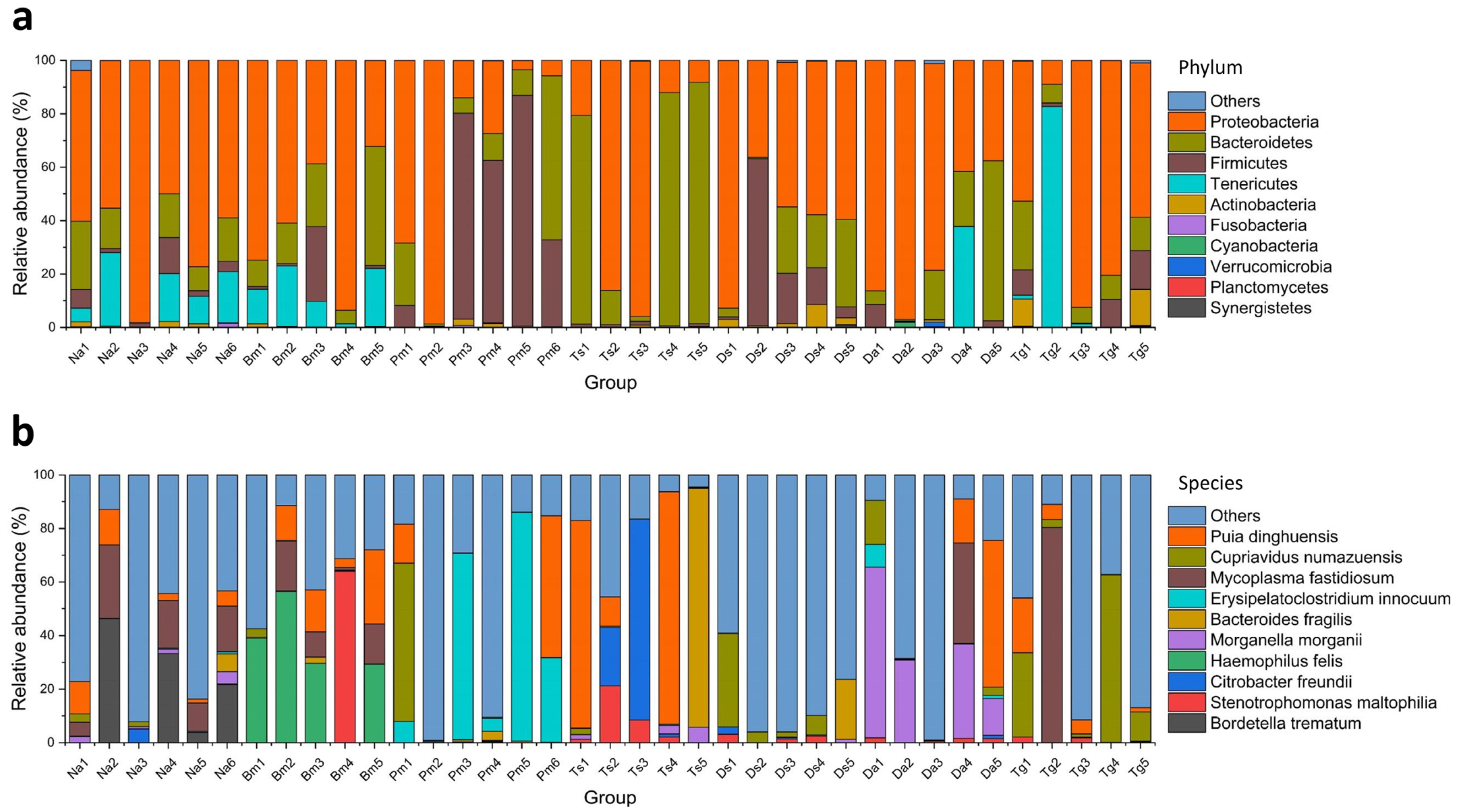
3.2. Taxonomic Profiling of Metagenomic Sequences
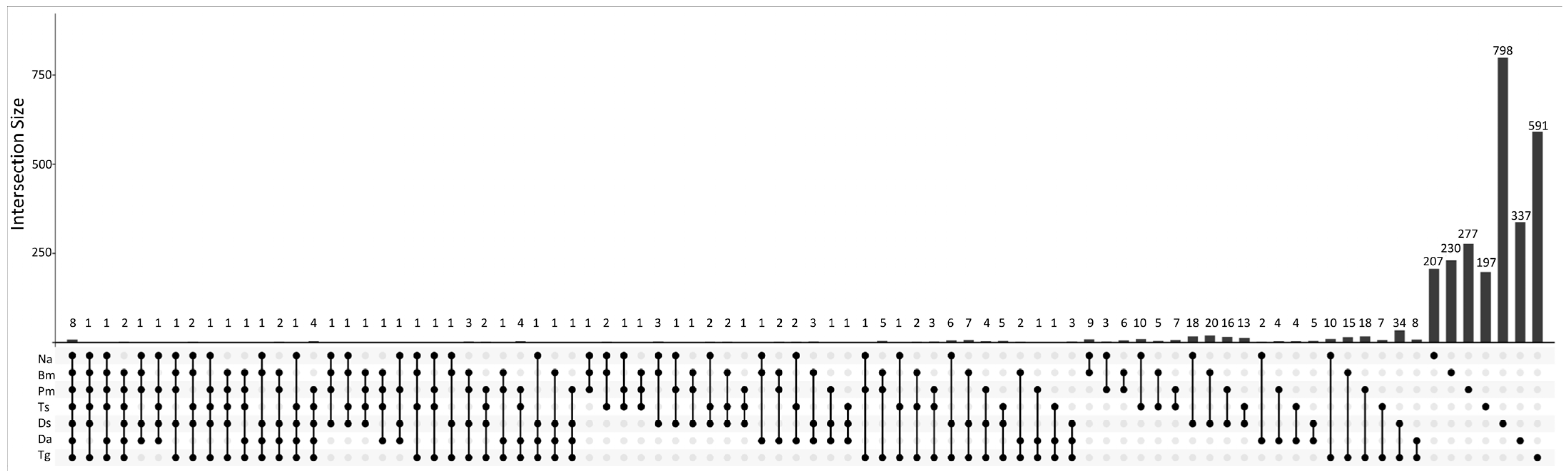
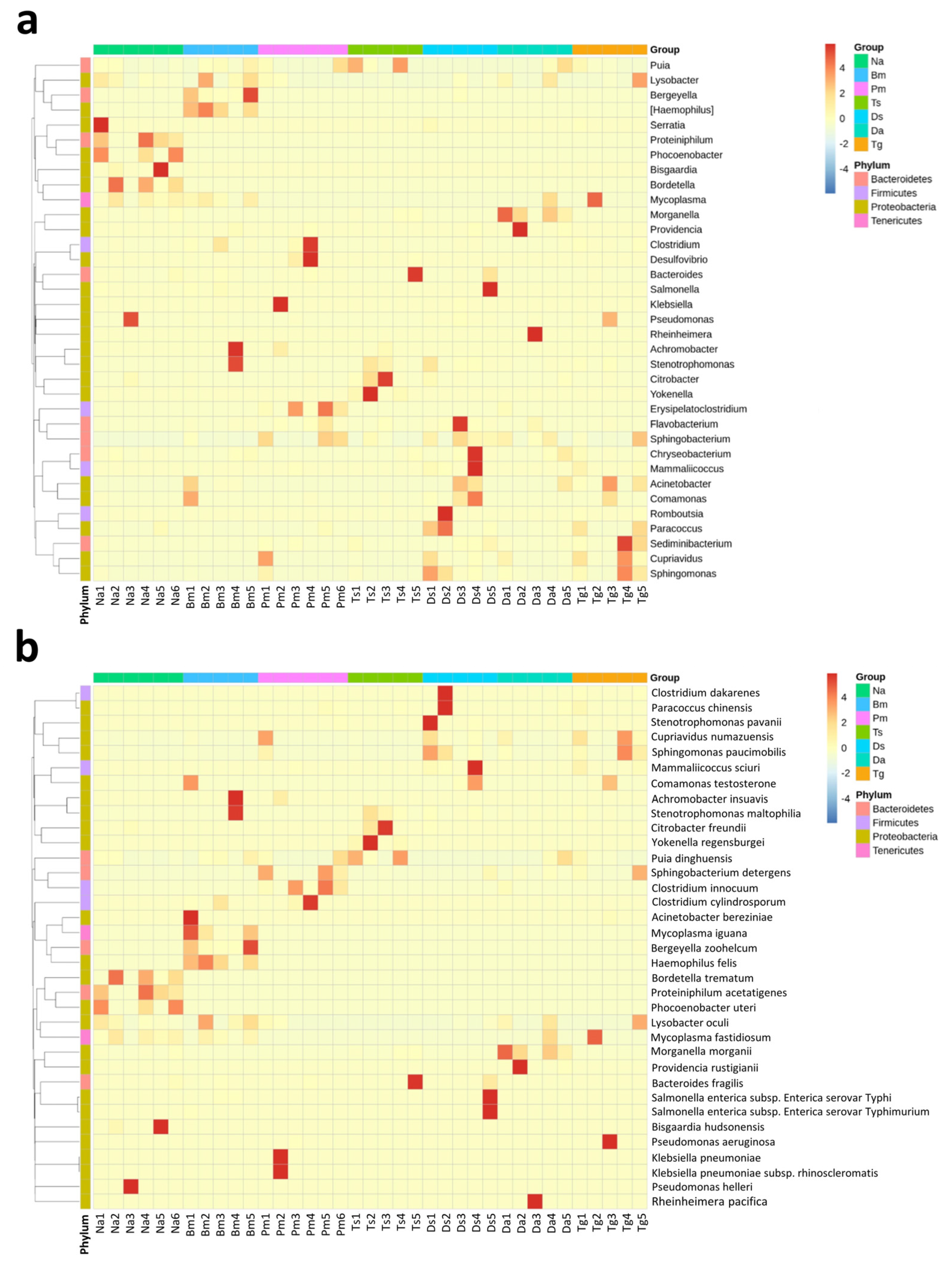
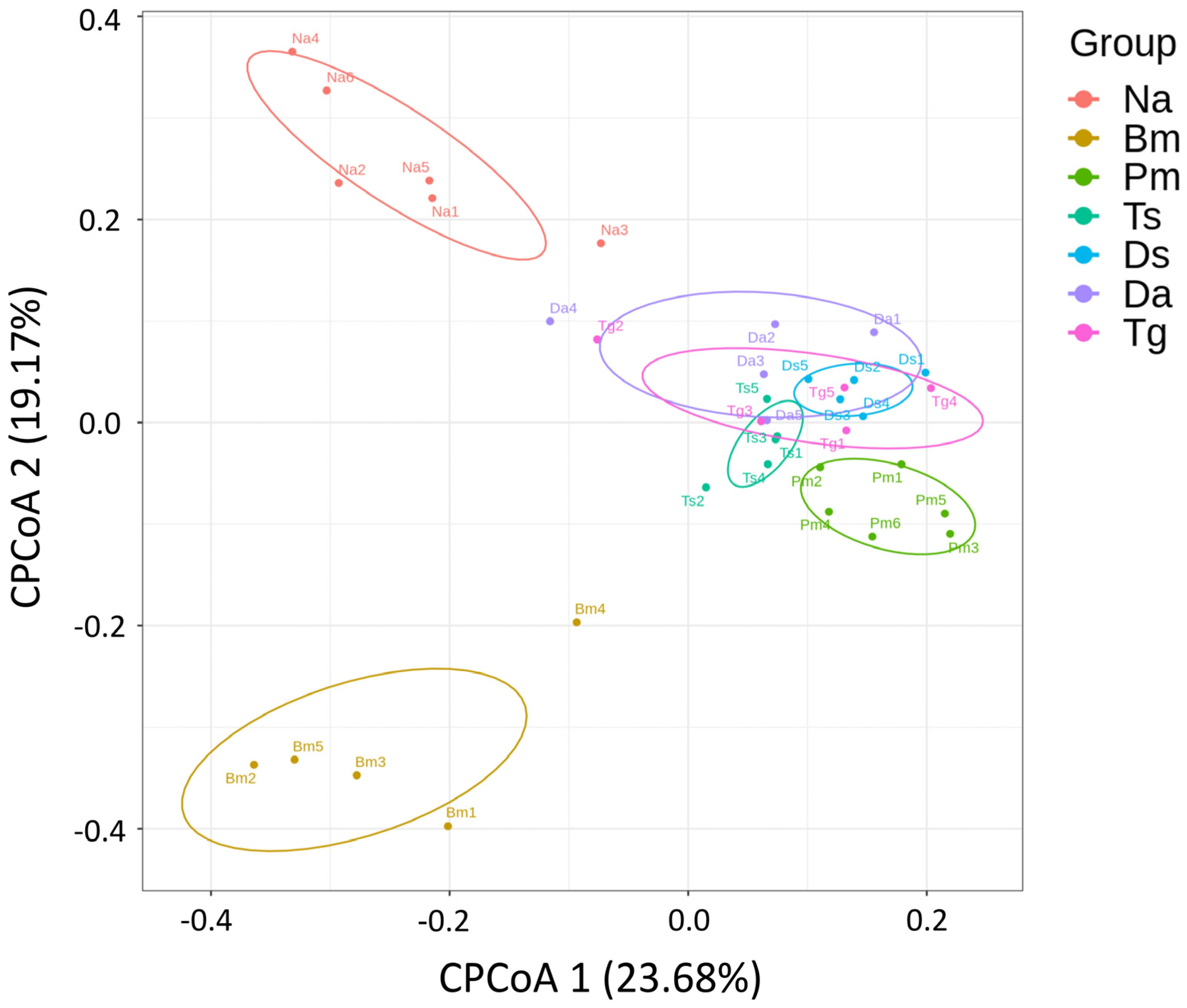
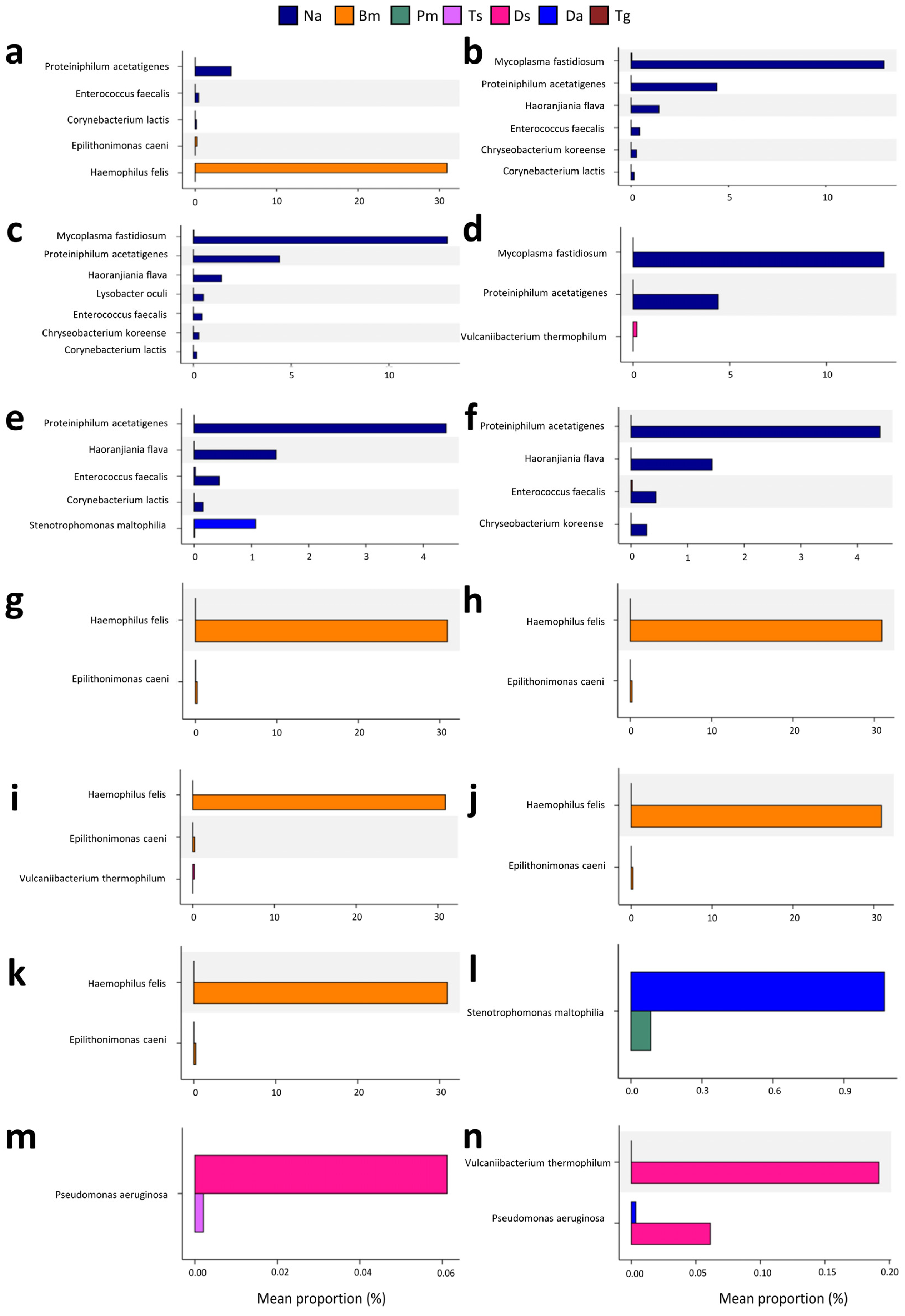
3.3. Comparison of Bacterial Community Structure
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Noutsos, T.; Currie, B.J.; Wijewickrama, E.S.; Isbister, G.K. Snakebite associated thrombotic microangiopathy and recommendations for clinical practice. Toxins 2022, 14, 57. [Google Scholar] [CrossRef]
- Chippaux, J.P. Snake-bites: Appraisal of the global situation. Bull. World Health Organ. 1998, 76, 515–524. [Google Scholar]
- Sminkey, L. World report on child injury prevention. Inj. Prev. 2008, 14, 69. [Google Scholar] [CrossRef]
- Ulima, A.T.; Fawzy, A. Complication in neglected non-venomous snake bite in rural area; what we need to anticipate. Int. J. Med. Sci. Clin. Res. 2022, 2, 1038–1043. [Google Scholar] [CrossRef]
- Gutiérrez, J.M.; Theakston, R.D.G.; Warrell, D.A. Confronting the neglected problem of snake bite envenoming: The need for a global partnership. PLoS Med. 2006, 3, e150. [Google Scholar] [CrossRef]
- Suchithra, N.; Pappachan, J.; Sujathan, P. Snakebite envenoming in Kerala, South India: Clinical profile and factors involved in adverse outcomes. Emerg. Med. J. 2008, 25, 200–204. [Google Scholar] [CrossRef]
- Shaikh, I.K.; Dixit, P.P.; Pawade, B.S.; Potnis-Lele, M.; Kurhe, B.P. Assessment of cultivable oral bacterial flora from important venomous snakes of India and their antibiotic susceptibilities. Curr. Microbiol. 2017, 74, 1278–1286. [Google Scholar] [CrossRef]
- Goldstein, E.; Agyare, E.; Vagvolgyi, A.; Halpern, M. Aerobic bacterial oral flora of garter snakes: Development of normal flora and pathogenic potential for snakes and humans. J. Clin. Microbiol. 1981, 13, 954–956. [Google Scholar] [CrossRef]
- Padhi, L.; Panda, S.K.; Mohapatra, P.P.; Sahoo, G. Antibiotic susceptibility of cultivable aerobic microbiota from the oral cavity of Echis carinatus from Odisha (India). Microb. Pathog. 2020, 143, 104121. [Google Scholar] [CrossRef]
- Gold, B.S.; Dart, R.C.; Barish, R.A. Bites of venomous snakes. N. Engl. J. Med. 2002, 347, 347–356. [Google Scholar] [CrossRef]
- Abubakar, S.; Habib, A.; Mathew, J. Amputation and disability following snakebite in Nigeria. Trop. Dr. 2010, 40, 114–116. [Google Scholar] [CrossRef]
- Lam, K.K.; Crow, P.; Ng, K.H.; Shek, K.C.; Fung, H.T.; Ades, G.; Grioni, A.; Tan, K.S.; Yip, K.T.; Lung, D.C.; et al. A cross-sectional survey of snake oral bacterial flora from Hong Kong, SAR, China. Emerg. Med. J. 2011, 28, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Theakston, R.; Phillips, R.; Looareesuwan, S.; Echeverria, P.; Makin, T.; Warrell, D. Bacteriological studies of the venom and mouth cavities of wild Malayan pit vipers (Calloselasma rhodostoma) in southern Thailand. Trans. R. Soc. Trop. Med. Hyg. 1990, 84, 875–879. [Google Scholar] [CrossRef]
- Gilmore, M.S.; Ferretti, J.J. The thin line between gut commensal and pathogen. Science 2003, 299, 1999–2002. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-M.; Wu, K.-G.; Chen, C.-J.; Wang, C.-M. Bacterial infection in association with snakebite: A 10-year experience in a northern Taiwan medical center. J. Microbiol. Immunol. Infect. 2011, 44, 456–460. [Google Scholar] [CrossRef]
- Jho, Y.-S.; Park, D.-H.; Lee, J.-H.; Cha, S.-Y.; Han, J.S. Identification of bacteria from the oral cavity and cloaca of snakes imported from Vietnam. Lab. Anim. Res. 2011, 27, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Artavia-Leon, A.; Romero-Guerrero, A.; Sancho-Blanco, C.; Rojas, N.; Umana-Castro, R. Diversity of aerobic bacteria isolated from oral and cloacal cavities from free-living snakes species in Costa Rica rainforest. Int. Sch. Res. Notices 2017, 2017, 8934285. [Google Scholar] [CrossRef]
- Liu, P.Y.; Weng, L.L.; Tseng, S.Y.; Huang, C.C.; Cheng, C.C.; Mao, Y.C.; Tung, K.C. Colistin resistance of Pseudomonas aeruginosa isolated from snakes in Taiwan. Can. J. Infect. Dis. Med. Microbiol. 2017, 2017, 7058396. [Google Scholar] [CrossRef]
- Sadeghi, M.; Barazandeh, M.; Zakariaei, Z.; Davoodi, L.; Tabaripour, R.; Fakhar, M.; Zakariaei, A. Massive cutaneous complications due to snakebite: A case report and literature review. Clin. Case Rep. 2021, 9, e04129. [Google Scholar] [CrossRef]
- Blaylock, R. Normal oral bacterial flora from some southern African snakes. Onderstepoort J. Vet. Res. 2001, 68, 175–182. [Google Scholar]
- Janda, J.M.; Abbott, S.L. The genus Aeromonas: Taxonomy, pathogenicity, and infection. Clin. Microbiol. Rev. 2010, 23, 35–73. [Google Scholar] [CrossRef] [PubMed]
- Mehler, S.J.; Bennett, R.A. Oral, dental, and beak disorders of reptiles. Vet. Clin. N. Am. Exot. Anim. Pract. 2003, 6, 477–503. [Google Scholar] [CrossRef]
- Mehler, S.; Bennett, R. Chapter 72—Upper Alimentary Tract Disease. In Reptile Medicine and Surgery, 2nd ed.; Mader, D.R., Ed.; Saunders Elsevier: St. Louis, MI, USA, 2006; pp. 924–930. [Google Scholar]
- Hedley, J. Anatomy and disorders of the oral cavity of reptiles and amphibians. Vet. Clin. N. Am. Exot. Anim. Pract. 2016, 19, 689–706. [Google Scholar] [CrossRef]
- Schumacher, J. Selected infectious diseases of wild reptiles and amphibians. J. Exot. Pet Med. 2006, 15, 18–24. [Google Scholar] [CrossRef]
- Mitchell, M.; Tully, T.N. Manual of Exotic Pet Practice; Elsevier Health Sciences: Saint Louis, MI, USA, 2008; pp. 136–163. [Google Scholar]
- Abba, Y.; Ilyasu, Y.M.; Noordin, M.M. Isolation and identification of bacterial populations of zoonotic importance from captive non-venomous snakes in Malaysia. Microb. Pathog. 2017, 108, 49–54. [Google Scholar] [CrossRef]
- Blaylock, R. The identification and syndromic management of snakebite in South Africa. S. Afr. Fam. Pract. 2005, 47, 46–53. [Google Scholar] [CrossRef]
- Fonseca, M.G.; Moreira, W.; Cunha, K.; Ribeiro, A.; Almeida, M. Oral microbiota of Brazilian captive snakes. J. Venom. Anim. Toxins Incl. Trop. Dis. 2009, 15, 54–60. [Google Scholar] [CrossRef]
- Su, H.Y.; Hussain, B.; Hsu, B.M.; Lee, K.H.; Mao, Y.C.; Chiang, L.C.; Chen, J.S. Bacterial community analysis identifies Klebsiella pneumoniae as a native symbiotic bacterium in the newborn Protobothrops mucrosquamatus. BMC Microbiol. 2023, 23, 213. [Google Scholar] [CrossRef]
- Greay, T.L.; Gofton, A.W.; Paparini, A.; Ryan, U.M.; Oskam, C.L.; Irwin, P.J. Recent insights into the tick microbiome gained through next-generation sequencing. Parasit. Vectors 2018, 11, 12. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Porchas, M.; Villalpando-Canchola, E.; Vargas-Albores, F. Significant loss of sensitivity and specificity in the taxonomic classification occurs when short 16S rRNA gene sequences are used. Heliyon 2016, 2, e00170. [Google Scholar] [CrossRef] [PubMed]
- Mao, Y.C.; Chuang, H.N.; Shih, C.H.; Hsieh, H.H.; Jiang, Y.H.; Chiang, L.C.; Lin, W.L.; Hsiao, T.H.; Liu, P.Y. An investigation of conventional microbial culture for the Naja atra bite wound, and the comparison between culture-based 16S Sanger sequencing and 16S metagenomics of the snake oropharyngeal bacterial microbiota. PLoS Negl. Trop. Dis. 2021, 15, e0009331. [Google Scholar] [CrossRef]
- Hu, T.; Chitnis, N.; Monos, D.; Dinh, A. Next-generation sequencing technologies: An overview. Hum. Immunol. 2021, 82, 801–811. [Google Scholar] [CrossRef]
- Tse, T.-C.; Tsai, I.-H.; Chan, Y.-Y.; Tsai, T.-S. Venom proteomics of Trimeresurus gracilis, a Taiwan-endemic pitviper, and comparison of its venom proteome and VEGF and CRISP sequences with those of the most related species. Toxins 2023, 15, 408. [Google Scholar] [CrossRef]
- Krishnankutty, S.P.; Muraleedharan, M.; Perumal, R.C.; Michael, S.; Benny, J.; Balan, B.; Kumar, P.; Manazhi, J.; Kumar, B.D.; Santhosh, S.; et al. Next-generation sequencing analysis reveals high bacterial diversity in wild venomous and non-venomous snakes from India. J. Venom. Anim. Toxins Incl. Trop. Dis. 2018, 24, 41. [Google Scholar] [CrossRef]
- McKiernan, H.; Danielson, P. Chapter 21—Molecular diagnostic applications in forensic science. In Molecular Diagnostics, 3rd ed.; Patrinos, G.P., Ansorge, W., Danielson, P.B., Eds.; Elsevier: San Diego, CA, USA, 2017; pp. 371–394. [Google Scholar]
- Callahan, B.J.; McMurdie, P.J.; Rosen, M.J.; Han, A.W.; Johnson, A.J.A.; Holmes, S.P. DADA2: High-resolution sample inference from Illumina amplicon data. Nat. Methods 2016, 13, 581–583. [Google Scholar] [CrossRef] [PubMed]
- Quin, C.; Estaki, M.; Vollman, D.; Barnett, J.; Gill, S.; Gibson, D. Probiotic supplementation and associated infant gut microbiome and health: A cautionary retrospective clinical comparison. Sci. Rep. 2018, 8, 8283. [Google Scholar] [CrossRef] [PubMed]
- Bokulich, N.A.; Kaehler, B.D.; Rideout, J.R.; Dillon, M.; Bolyen, E.; Knight, R.; Huttley, G.A.; Gregory Caporaso, J. Optimizing taxonomic classification of marker-gene amplicon sequences with QIIME 2′s q2-feature-classifier plugin. Microbiome 2018, 6, 90. [Google Scholar] [CrossRef] [PubMed]
- Rognes, T.; Flouri, T.; Nichols, B.; Quince, C.; Mahé, F. VSEARCH: A versatile open source tool for metagenomics. PeerJ 2016, 4, e2584. [Google Scholar] [CrossRef]
- Bolyen, E.; Rideout, J.R.; Dillon, M.R.; Bokulich, N.A.; Abnet, C.C.; Al-Ghalith, G.A.; Alexander, H.; Alm, E.J.; Arumugam, M.; Asnicar, F. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat. Biotechnol. 2019, 37, 852–857. [Google Scholar] [CrossRef]
- Katoh, K.; Standley, D.M. MAFFT multiple sequence alignment software version 7: Improvements in performance and usability. Mol. Biol. Evol. 2013, 30, 772–780. [Google Scholar] [CrossRef] [PubMed]
- Balvočiūtė, M.; Huson, D.H. SILVA, RDP, Greengenes, NCBI and OTT—How do these taxonomies compare? BMC Genom. 2017, 18, 114. [Google Scholar] [CrossRef] [PubMed]
- Gyarmati, P.; Kjellander, C.; Aust, C.; Song, Y.; Öhrmalm, L.; Giske, C. Metagenomic analysis of bloodstream infections in patients with acute leukemia and therapy-induced neutropenia. Sci. Rep. 2016, 6, 23532. [Google Scholar] [CrossRef] [PubMed]
- Hong, X.; Chen, J.; Liu, L.; Wu, H.; Tan, H.; Xie, G.; Xu, Q.; Zou, H.; Yu, W.; Wang, L. Metagenomic sequencing reveals the relationship between microbiota composition and quality of Chinese Rice Wine. Sci. Rep. 2016, 6, 26621. [Google Scholar] [CrossRef] [PubMed]
- Whittaker, R.H. Evolution and measurement of species diversity. Taxon 1972, 21, 213–251. [Google Scholar] [CrossRef]
- Lozupone, C.; Knight, R. UniFrac: A new phylogenetic method for comparing microbial communities. Appl. Environ. Microbiol. 2005, 71, 8228–8235. [Google Scholar] [CrossRef] [PubMed]
- Lozupone, C.; Lladser, M.E.; Knights, D.; Stombaugh, J.; Knight, R. UniFrac: An effective distance metric for microbial community comparison. ISME J. 2011, 5, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Legendre, P.; Anderson, M.J. Distance-based redundancy analysis: Testing multispecies responses in multifactorial ecological experiments. Ecol. Monogr. 1999, 69, 1–24. [Google Scholar] [CrossRef]
- Zgadzaj, R.; Garrido-Oter, R.; Jensen, D.B.; Koprivova, A.; Schulze-Lefert, P.; Radutoiu, S. Root nodule symbiosis in Lotus japonicus drives the establishment of distinctive rhizosphere, root, and nodule bacterial communities. Proc. Natl. Acad. Sci. USA 2016, 113, E7996–E8005. [Google Scholar] [CrossRef]
- Paulson, J.N.; Stine, O.C.; Bravo, H.C.; Pop, M. Differential abundance analysis for microbial marker-gene surveys. Nat. Methods 2013, 10, 1200–1202. [Google Scholar] [CrossRef]
- Hyde, E.R.; Navas-Molina, J.A.; Song, S.J.; Kueneman, J.G.; Ackermann, G.; Cardona, C.; Humphrey, G.; Boyer, D.; Weaver, T.; Mendelson, J.R., 3rd; et al. The oral and skin microbiomes of captive Komodo dragons are significantly shared with their habitat. mSystems 2016, 1, e00046-16. [Google Scholar] [CrossRef]
- Qin, Z.; Wang, S.; Guo, D.; Zhu, J.; Chen, H.; Bai, L.; Luo, X.; Yin, Y. Comparative analysis of intestinal bacteria among venom secretion and non-secrection snakes. Sci. Rep. 2019, 9, 6335. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Ren, J.; Yang, D.; Liu, S.; Gong, X. Comparative analysis and characterization of the gut microbiota of four farmed snakes from southern China. PeerJ 2019, 7, e6658. [Google Scholar] [CrossRef] [PubMed]
- Tang, W.; Zhu, G.; Shi, Q.; Yang, S.; Ma, T.; Mishra, S.K.; Wen, A.; Xu, H.; Wang, Q.; Jiang, Y.; et al. Characterizing the microbiota in gastrointestinal tract segments of Rhabdophis subminiatus: Dynamic changes and functional predictions. Microbiologyopen 2019, 8, e00789. [Google Scholar] [CrossRef]
- Zhong, J.; Guo, K.; Liao, Z.-L.; Hu, S.-C.; Du, Y.; Ji, X. Comparative analysis of the gut microbiota composition between two sea snakes, Hydrophis curtus, and Hydrophis cyanocinctus. Coral Reefs 2022, 41, 53–62. [Google Scholar] [CrossRef]
- Huang, L.-W.; Wang, J.-D.; Huang, J.-A.; Hu, S.-Y.; Wang, L.-M.; Tsan, Y.-T. Wound infections secondary to snakebite in central Taiwan. J. Venom. Anim. Toxins Incl. Trop. Dis. 2011, 18, 272–276. [Google Scholar] [CrossRef]
- Yeh, H.; Gao, S.-Y.; Lin, C.-C. Wound infections from Taiwan Cobra (Naja atra) bites: Determining bacteriology, antibiotic susceptibility, and the use of antibiotics-a cobra BITE study. Toxins 2021, 13, 183. [Google Scholar] [CrossRef]
- Mao, Y.-C.; Liu, P.-Y.; Hung, D.-Z.; Lai, W.-C.; Huang, S.-T.; Hung, Y.-M.; Yang, C.-C. Bacteriology of Naja atra snakebite wound and its implications for antibiotic therapy. Am. J. Trop. Med. Hyg. 2016, 94, 1129. [Google Scholar] [CrossRef]
- Mao, Y.-C.; Liu, P.-Y.; Chiang, L.-C.; Lai, C.-S.; Lai, K.-L.; Ho, C.-H.; Wang, T.-H.; Yang, C.-C. Naja atra snakebite in Taiwan. Clin. Toxicol. 2018, 56, 273–280. [Google Scholar] [CrossRef]
- Yeh, H.; Gao, S.Y.; Lin, C.C. Wound infection of snakebite from venomous Protobothrops mucrosquamatus, Viridovipera stejnegeri and Naja atra in Taiwan: Validation of BITE and cobra BITE scoring systems and their bacteriological differences in wound cultures. Toxins 2023, 15, 78. [Google Scholar] [CrossRef]
- Lin, C.-C.; Chen, Y.-C.; Goh, Z.N.L.; Seak, C.-K.; Seak, J.C.-Y.; Shi-Ying, G.; Seak, C.-J.; Investigators, S. Wound infections of snakebites from the venomous Protobothrops mucrosquamatus and Viridovipera stejnegeri in taiwan: Bacteriology, antibiotic susceptibility, and predicting the need for antibiotics—A bite study. Toxins 2020, 12, 575. [Google Scholar] [CrossRef]
- Chuang, P.C.; Lin, W.H.; Chen, Y.C.; Chien, C.C.; Chiu, I.M.; Tsai, T.S. Oral bacteria and their antibiotic susceptibilities in Taiwanese venomous snakes. Microorganisms 2022, 10, 951. [Google Scholar] [CrossRef] [PubMed]
- Rampini, S.K.; Bloemberg, G.V.; Keller, P.M.; Büchler, A.C.; Dollenmaier, G.; Speck, R.F.; Böttger, E.C. Broad-range 16S rRNA gene polymerase chain reaction for diagnosis of culture-negative bacterial infections. Clin. Infect. Dis. 2011, 53, 1245–1251. [Google Scholar] [CrossRef]
- Lv, Y.Y.; Gao, Z.H.; Xia, F.; Chen, M.H.; Qiu, L.H. Puia dinghuensis gen. nov., sp. nov., isolated from monsoon evergreen broad-leaved forest soil. Int. J. Syst. Evol. Microbiol. 2017, 67, 4639–4645. [Google Scholar] [CrossRef]
- Shin, S.; Choi, J.; Ko, K. Four cases of possible human infections with Delftia lacustris. Infection 2012, 40, 709–712. [Google Scholar] [CrossRef] [PubMed]
- Sohn, K.M.; Baek, J.-Y.; Cheon, S.; Kim, Y.-S.; Koo, S.H. Ocular infection associated with Delftia lacustris: First report. Braz. J. Infect. Dis. 2015, 19, 449–450. [Google Scholar] [CrossRef]
- Jørgensen, N.O.; Brandt, K.K.; Nybroe, O.; Hansen, M. Delftia lacustris sp. nov., a peptidoglycan-degrading bacterium from fresh water, and emended description of Delftia tsuruhatensis as a peptidoglycan-degrading bacterium. Int. J. Syst. Evol. Microbiol. 2009, 59, 2195–2199. [Google Scholar] [CrossRef]
- Kane, S.R.; Chakicherla, A.Y.; Chain, P.S.; Schmidt, R.; Shin, M.W.; Legler, T.C.; Scow, K.M.; Larimer, F.W.; Lucas, S.M.; Richardson, P.M. Whole-genome analysis of the methyl tert-butyl ether-degrading beta-proteobacterium Methylibium petroleiphilum PM1. J. Bacteriol. 2007, 189, 1931–1945. [Google Scholar] [CrossRef]
- Nakatsu, C.H.; Hristova, K.; Hanada, S.; Meng, X.-Y.; Hanson, J.R.; Scow, K.M.; Kamagata, Y. Methylibium petroleiphilum gen. nov., sp. nov., a novel methyl tert-butyl ether-degrading methylotroph of the Betaproteobacteria. Int. J. Syst. Evol. Microbiol. 2006, 56, 983–989. [Google Scholar] [CrossRef]
- Moore, G.M.; Gitai, Z. Both clinical and environmental Caulobacter species are virulent in the Galleria mellonella infection model. PLoS ONE 2020, 15, e0230006. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Fletcher, B.; Scott, D.C.; Ely, B. Genome sequence and phenotypic characterization of Caulobacter segnis. Curr. Microbiol. 2015, 70, 355–363. [Google Scholar] [CrossRef]
- Derichs, J.; Kämpfer, P.; Lipski, A. Pedobacter nutrimenti sp. nov., isolated from chilled food. Int. J. Syst. Evol. Microbiol. 2014, 64, 1310–1316. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Aguilar, L.; Caballero-Mellado, J.; Estrada-De Los Santos, P. Transfer of Wautersia numazuensis to the genus Cupriavidus as Cupriavidus numazuensis comb. nov. Int. J. Syst. Evol. Microbiol. 2013, 63, 208–211. [Google Scholar] [CrossRef] [PubMed]
- Almuzara, M.N.; Barberis, C.M.; Rodríguez, C.H.; Famiglietti, A.M.; Ramirez, M.S.; Vay, C.A. First report of an extensively drug-resistant VIM-2 metallo-β-lactamase-producing Brevundimonas diminuta clinical isolate. J. Clin. Microbiol. 2012, 50, 2830–2832. [Google Scholar] [CrossRef] [PubMed]
- Lupande-Mwenebitu, D.; Tshiyongo, R.K.; Lunguya-Metila, O.; Lavigne, J.-P.; Rolain, J.-M.; Diene, S.M. First isolation and clinical case of Brevundimonas diminuta in a newborn with low birth weight, in Democratic Republic of Congo: A case report. Medicina 2021, 57, 1227. [Google Scholar] [CrossRef]
- Cherny, K.E.; Muscat, E.B.; Reyna, M.E.; Kociolek, L.K. Clostridium innocuum: Microbiological and clinical characteristics of a potential emerging pathogen. Anaerobe 2021, 71, 102418. [Google Scholar] [CrossRef]
- Kim, J.H.; Cho, C.R.; Um, T.H.; Rhu, J.Y.; Kim, E.S.; Jeong, J.W.; Lee, H.R. Morganella morganii sepsis with massive hemolysis. J. Korean Med. Sci. 2007, 22, 1082–1084. [Google Scholar] [CrossRef][Green Version]
- Liu, H.; Zhu, J.; Hu, Q.; Rao, X. Morganella morganii, a non-negligent opportunistic pathogen. Int. J. Infect. Dis. 2016, 50, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.-T.; Chang, S.-C.; Chen, Y.-C.; Luh, K.-T. Comparison of antimicrobial susceptibility of Citrobacter freundii isolates in two different time periods. J. Microbiol. Immunol. Infect. 2000, 33, 258–262. [Google Scholar]
- Liu, H.; Zhao, Z.; Xue, Y.; Ding, K.; Xue, Q. Fatal cases of Citrobacter freundii septicemia and encephalitis in sheep. J. Vet. Diagn. Invest. 2018, 30, 245–248. [Google Scholar] [CrossRef]
- Denton, M.; Kerr, K.G. Microbiological and clinical aspects of infection associated with Stenotrophomonas maltophilia. Clin. Microbiol. Rev. 1998, 11, 57–80. [Google Scholar] [CrossRef]
- Garcia Paez, J.; Tengan, F.; Barone, A.; Levin, A.; Costa, S. Factors associated with mortality in patients with bloodstream infection and pneumonia due to Stenotrophomonas maltophilia. Eur. J. Clin. Microbiol. 2008, 27, 901–906. [Google Scholar] [CrossRef]
- Vandamme, P.; Heyndrickx, M.; Vancanneyt, M.; Hoste, B.; De Vos, P.; Falsen, E.; Kersters, K.; Hinz, K.-H. Bordetella trematum sp. nov., isolated from wounds and ear infections in humans, and reassessment of Alcaligenes denitrificans Rüger and Tan 1983. Int. J. Syst. Evol. Microbiol. 1996, 46, 849–858. [Google Scholar] [CrossRef] [PubMed]
- Kukla, R.; Svarc, M.; Bolehovska, R.; Ryskova, L.; Paterova, P.; Fajfr, M.; Malisova, L.; Zemlickova, H. Isolation of Bordetella trematum from the respiratory tract of a patient with lung cancer: A case report. Folia Microbiol. 2020, 65, 623–627. [Google Scholar] [CrossRef]
- Mao, Y.C.; Liu, P.Y.; Chiang, L.C.; Liao, S.C.; Su, H.Y.; Hsieh, S.Y.; Yang, C.C. Bungarus multicinctus multicinctus snakebite in Taiwan. Am. J. Trop. Med. Hyg. 2017, 96, 1497–1504. [Google Scholar] [CrossRef]
- Lai, C.S.; Liu, P.Y.; Lee, C.H.; Ho, C.H.; Chen, W.L.; Lai, K.L.; Su, H.Y.; Lin, W.L.; Chung, K.C.; Yang, Y.Y.; et al. The development of surgical risk score and evaluation of necrotizing soft tissue infection in 161 Naja atra envenomed patients. PLoS Negl. Trop. Dis. 2022, 16, e0010066. [Google Scholar] [CrossRef]
- Chen, Y.-W.; Chen, M.-H.; Chen, C.-K.; Lee, C.-H.; Hung, D.-Z.; Huang, C.-I.; Yang, C.-C.; Chen, Y.-C.; Yen, D.H.-T.; Wang, L.-M. Differences in clinical profiles of patients with Protobothrops mucrosquamatus and Viridovipera stejnegeri envenoming in Taiwan. Am. J. Trop. Med. Hyg. 2009, 80, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.S.; Chan, Y.Y.; Huang, S.M.; Chuang, P.C. Case report: Symptoms and prognosis of Trimeresurus gracilis envenomation. Am. J. Trop. Med. Hyg. 2022, 106, 1281–1284. [Google Scholar] [CrossRef] [PubMed]
- Su, H.Y.; Huang, S.W.; Mao, Y.C.; Liu, M.W.; Lee, K.H.; Lai, P.F.; Tsai, M.J. Clinical and laboratory features distinguishing between Deinagkistrodon acutus and Daboia siamensis envenomation. J. Venom. Anim. Toxins Incl. Trop. Dis. 2018, 24, 43. [Google Scholar] [CrossRef]
- Tsai, T.S.; Liu, C.C.; Chuang, P.C. Personal experience of Daboia siamensis envenomation. Case Rep. Med. 2021, 2021, 3396373. [Google Scholar] [CrossRef]
- Ho, C.H.; Chiang, L.C.; Mao, Y.C.; Lan, K.C.; Tsai, S.H.; Shih, Y.J.; Tzeng, Y.S.; Lin, C.S.; Lin, W.L.; Fang, W.H.; et al. Analysis of the necrosis-inducing components of the venom of Naja atra and assessment of the neutralization ability of freeze-dried antivenom. Toxins 2021, 13, 619. [Google Scholar] [CrossRef]
- Chiang, L.C.; Chien, K.Y.; Su, H.Y.; Chen, Y.C.; Mao, Y.C.; Wu, W.G. Comparison of protein variation in Protobothrops mucrosquamatus venom between northern and southeast Taiwan and association with human envenoming effects. Toxins 2022, 14, 643. [Google Scholar] [CrossRef] [PubMed]
- Zaher, H.; Murphy, R.W.; Arredondo, J.C.; Graboski, R.; Machado-Filho, P.R.; Mahlow, K.; Montingelli, G.G.; Quadros, A.B.; Orlov, N.L.; Wilkinson, M. Large-scale molecular phylogeny, morphology, divergence-time estimation, and the fossil record of advanced caenophidian snakes (Squamata: Serpentes). PLoS ONE 2019, 14, e0216148. [Google Scholar] [CrossRef]

| Sample Name | Raw HiFi Reads | Remove Primers | Filtered Reads | Denoised Reads | Non-Chimeric Reads |
|---|---|---|---|---|---|
| Na 1 | 20,241 | 19,179 | 18,345 | 17,940 | 17,910 |
| Na 2 | 12,779 | 11,293 | 10,983 | 10,850 | 10,850 |
| Na 3 | 13,112 | 11,003 | 10,559 | 10,285 | 9955 |
| Na 4 | 11,740 | 11,070 | 10,800 | 10,709 | 10,709 |
| Na 5 | 11,535 | 10,936 | 10,707 | 10,607 | 10,607 |
| Na 6 | 13,057 | 12,333 | 11,975 | 11,817 | 11,817 |
| Bm 1 | 13,652 | 12,611 | 12,226 | 11,951 | 11,940 |
| Bm 2 | 10,806 | 10,388 | 10,135 | 10,029 | 10,029 |
| Bm 3 | 12,306 | 11,213 | 10,882 | 10,607 | 10,607 |
| Bm 4 | 15,043 | 13,337 | 13,048 | 12,915 | 12,915 |
| Bm 5 | 10,436 | 9241 | 8990 | 8837 | 8837 |
| Pm 1 | 15,813 | 14,108 | 13,732 | 13,690 | 13,690 |
| Pm 2 | 14,113 | 12,000 | 11,405 | 11,252 | 11,039 |
| Pm 3 | 12,350 | 10,178 | 9804 | 9763 | 9763 |
| Pm 4 | 13,039 | 12,315 | 11,893 | 11,643 | 11,643 |
| Pm 5 | 13,771 | 11,941 | 11,611 | 11,488 | 11,488 |
| Pm 6 | 13,372 | 11,610 | 11,327 | 11,197 | 11,197 |
| Ts 1 | 24,256 | 23,659 | 22,684 | 22,589 | 22,589 |
| Ts 2 | 13,490 | 12,723 | 12,349 | 12,269 | 12,269 |
| Ts 3 | 15,999 | 15,147 | 14,739 | 14,605 | 14,605 |
| Ts 4 | 12,484 | 11,839 | 11,568 | 11,507 | 11,507 |
| Ts 5 | 21,205 | 19,912 | 19,379 | 19,225 | 19,225 |
| Ds 1 | 13,793 | 12,318 | 11,983 | 11,854 | 11,852 |
| Ds 2 | 15,176 | 13,649 | 13,229 | 13,175 | 13,175 |
| Ds 3 | 13,422 | 13,166 | 12,739 | 12,433 | 12,298 |
| Ds 4 | 14,308 | 13,084 | 12,734 | 12,558 | 12,546 |
| Ds 5 | 12,141 | 11,740 | 11,429 | 11,334 | 11,334 |
| Da 1 | 13,651 | 12,426 | 11,964 | 11,819 | 11,816 |
| Da 2 | 13,395 | 13,032 | 12,657 | 12,619 | 12,606 |
| Da 3 | 13,200 | 12,489 | 12,058 | 11,655 | 11,655 |
| Da 4 | 11,583 | 10,217 | 9996 | 9910 | 9910 |
| Da 5 | 11,517 | 10,151 | 9949 | 9890 | 9890 |
| Tg 1 | 13,637 | 12,419 | 12,044 | 11,886 | 11,886 |
| Tg 2 | 12,071 | 10,967 | 10,690 | 10,535 | 10,535 |
| Tg 3 | 12,850 | 11,453 | 11,149 | 10,827 | 10,827 |
| Tg 4 | 13,424 | 11,993 | 11,712 | 11,549 | 11,549 |
| Tg 5 | 13,913 | 12,609 | 12,320 | 12,039 | 12,039 |
| Na | Bm | Pm | Ts | Ds | Da | Tg | |
|---|---|---|---|---|---|---|---|
| Reads | 71,848 | 54,328 | 68,820 | 80,195 | 61,205 | 55,877 | 56,836 |
| Phylum | 8 | 8 | 6 | 7 | 8 | 9 | 13 |
| Class | 22 | 20 | 21 | 21 | 23 | 24 | 30 |
| Order | 39 | 37 | 37 | 42 | 45 | 45 | 55 |
| Family | 69 | 70 | 72 | 69 | 95 | 81 | 103 |
| Genus | 115 | 115 | 124 | 121 | 226 | 155 | 246 |
| Species | 163 | 207 | 204 | 192 | 478 | 253 | 471 |
| Order | Na | Bm | Pm | Ts | Ds | Da | Tg |
|---|---|---|---|---|---|---|---|
| 1 | Bordetella trematum (16.11%) 1 | Haemophilus felis (29.60%) | Clostridium innocuum (31.73%) | Puia dinghuensis (36.04%) | Clostridium dakarense (10.71%) | Morganella morganii (29.12%) | Cupriavidus numazuensis (22.37%) |
| 2 | Mycoplasma fastidiosum (12.43%) | Stenotrophomonas maltophilia (15.23%) | Cupriavidus numazuensis (11.77%) | Bacteroides fragilis (21.40%) | Cupriavidus numazuensis (9.47%) | Providencia rustigianii (14.96%) | Mycoplasma fastidiosum (14.90%) |
| 3 | Phocoenobacter uteri (12.21%) | Puia dinghuensis (10.74%) | Puia dinghuensis (11.58%) | Citrobacter freundii (17.14%) | Salmonella enterica enterica serovar Typhimurium (4.63%) | Puia dinghuensis (12.63%) | Pseudomonas aeruginosa (9.39%) |
| 4 | Pseudomonas helleri (11.83%) | Mycoplasma fastidiosum (7.93%) | Klebsiella pneumoniae (9.89%) | Yokenella regensburgei (6.13%) | Sphingomonas paucimobilis (4.34%) | Mycoplasma fastidiosum (6.68%) | Puia dinghuensis (6.69%) |
| 5 | Bisgaardia hudsonensis (11.21%) | Mycoplasma iguana (4.82%) | Clostridium cylindrosporum (8.14%) | Stenotrophomonas maltophilia (5.46%) | Bacteroides fragilis (4.20%) | Rheinheimera pacifica (5.33%) | Sphingomonas paucimobilis (4.50%) |
| 6 | Puia dinghuensis (6.58%) | Bergeyella zoohelcum (4.56%) | Sphingobacterium detergens (2.88%) | Morganella morganii (2.29%) | Paracoccus chinensis (3.90%) | Cupriavidus numazuensis (4.14%) | Sediminibacterium lactis (2.45%) |
| 7 | Proteiniphilum acetatigenes (4.63%) | Achromobacter insuavis (4.00%) | Luteibacter anthropic (2.39%) | Phyllobacterium myrsinacearum (1.86%) | Stenotrophomonas pavanii (3.86%) | Clostridium innocuum (2.09%) | Latilactobacillus curvatus (1.50%) |
| 8 | Serratia marcescens (2.33%) | Acinetobacter bereziniae (3.13%) | Desulfovibrio desulfuricans (2.18%) | Beijerinckia fluminensis (1.71%) | Chryseobacterium salipaludis (3.24%) | Rheinheimera hassiensis (1.90%) | Comamonas testosterone (1.45%) |
| 9 | Morganella morganii (1.74%) | Clostridium cylindrosporum (2.78%) | Epilithonimonas lactis (2.01%) | Cupriavidus numazuensis (0.80%) | Mammaliicoccus sciuri (2.70%) | Acinetobacter proteolyticus (1.85%) | Paracoccus suum (1.35%) |
| 10 | Haoranjiania flava (1.64%) | Comamonas testosterone (2.12%) | Oceanisphaera ostreae (0.94%) | Tepidimonas aquatica (0.77%) | Acinetobacter variabilis (2.35%) | Rheinheimera aquimaris (1.61%) | Paenarthrobacter nitroguajacolicus (1.35%) |
| Pathogen Bacterial Species | Non-Pathogen Bacterial Species |
|---|---|
| Achromobacter insuavis (G−) | Beijerinckia fluminensis (G−) |
| Acinetobacter bereziniae (G−) | Chryseobacterium salipaludis (G−) |
| Acinetobacter proteolyticus (G−) | Clostridium cylindrosporum (G+, An) |
| Acinetobacter variabilis (G−) | Clostridium dakarense (G+, An) |
| Bacteroides fragilis (G−, An) 1 | Cupriavidus numazuensis (G−) 1 |
| Bergeyella zoohelcum (G−) | Epilithonimonas lactis (G−) |
| Bisgaardia hudsonensis (G−) | Haemophilus felis (G−) 1 |
| Citrobacter freundii (G−) 1 | Haoranjiania flava (G−) |
| Clostridium innocuum (G+, An) 1 | Latilactobacillus curvatus (G+, An) |
| Comamonas testosterone (G−) | Mycoplasma fastidiosum (G−) 1 |
| Desulfovibrio desulfuricans (G−, An) | Mycoplasma iguana (G−) |
| Klebsiella pneumoniae (G−) | Oceanisphaera ostreae (G−) |
| Morganella morganii (G−) 1 | Paracoccus chinensis (G−) |
| Pseudomonas aeruginosa (G−) | Phocoenobacter uter (G−) |
| Serratia marcescens (G−) | Proteiniphilum acetatigenes (G−, An) |
| Luteibacter anthropi (G−) | Pseudomonas helleri (G−) |
| Mammaliicoccus sciuri (G+) | Puia dinghuensis (G−) 1 |
| Paenarthrobacter nitroguajacolicus (G+) | Rheinheimera aquimaris (G−) |
| Phyllobacterium myrsinacearum (G−) | Rheinheimera hassiensis (G−) |
| Providencia rustigianii (G−) | Rheinheimera pacifica (G−) |
| Salmonella enterica enterica serovar Typhimurium (G−) | Sediminibacterium lactis (G−) |
| Sphingomonas paucimobilis (G−) | Sphingobacterium detergens (G−) |
| Stenotrophomonas maltophilia (G−) 1 | Stenotrophomonas pavanii (G−) |
| Yokenella regensburgei (G−) | Tepidimonas aquatica (G−) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, W.-H.; Tsai, T.-S. Comparisons of the Oral Microbiota from Seven Species of Wild Venomous Snakes in Taiwan Using the High-Throughput Amplicon Sequencing of the Full-Length 16S rRNA Gene. Biology 2023, 12, 1206. https://doi.org/10.3390/biology12091206
Lin W-H, Tsai T-S. Comparisons of the Oral Microbiota from Seven Species of Wild Venomous Snakes in Taiwan Using the High-Throughput Amplicon Sequencing of the Full-Length 16S rRNA Gene. Biology. 2023; 12(9):1206. https://doi.org/10.3390/biology12091206
Chicago/Turabian StyleLin, Wen-Hao, and Tein-Shun Tsai. 2023. "Comparisons of the Oral Microbiota from Seven Species of Wild Venomous Snakes in Taiwan Using the High-Throughput Amplicon Sequencing of the Full-Length 16S rRNA Gene" Biology 12, no. 9: 1206. https://doi.org/10.3390/biology12091206
APA StyleLin, W.-H., & Tsai, T.-S. (2023). Comparisons of the Oral Microbiota from Seven Species of Wild Venomous Snakes in Taiwan Using the High-Throughput Amplicon Sequencing of the Full-Length 16S rRNA Gene. Biology, 12(9), 1206. https://doi.org/10.3390/biology12091206





