Demographic Factors Predict Risk of Lymph Node Involvement in Patients with Endometrial Adenocarcinoma
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
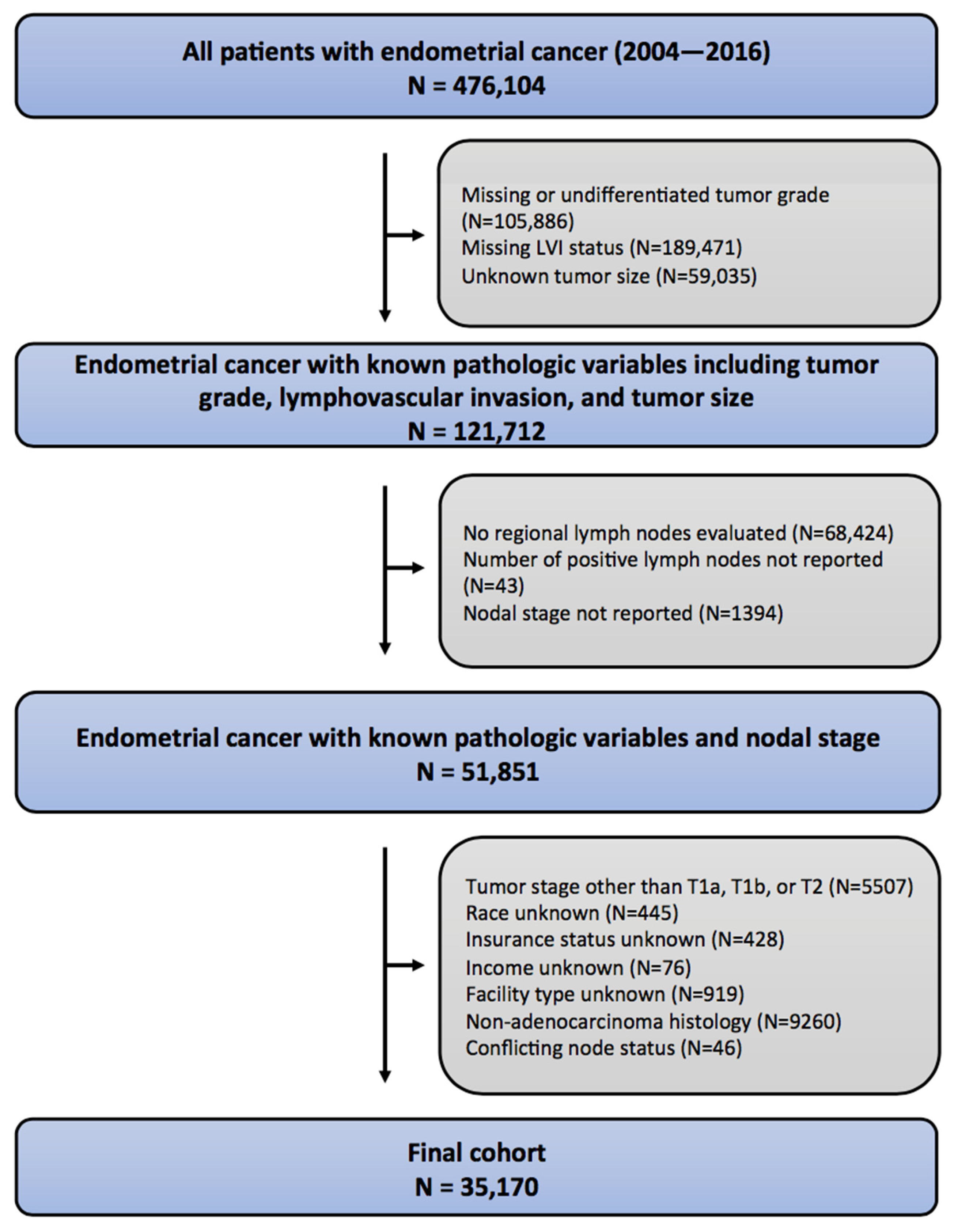
2.1. Patient Selection
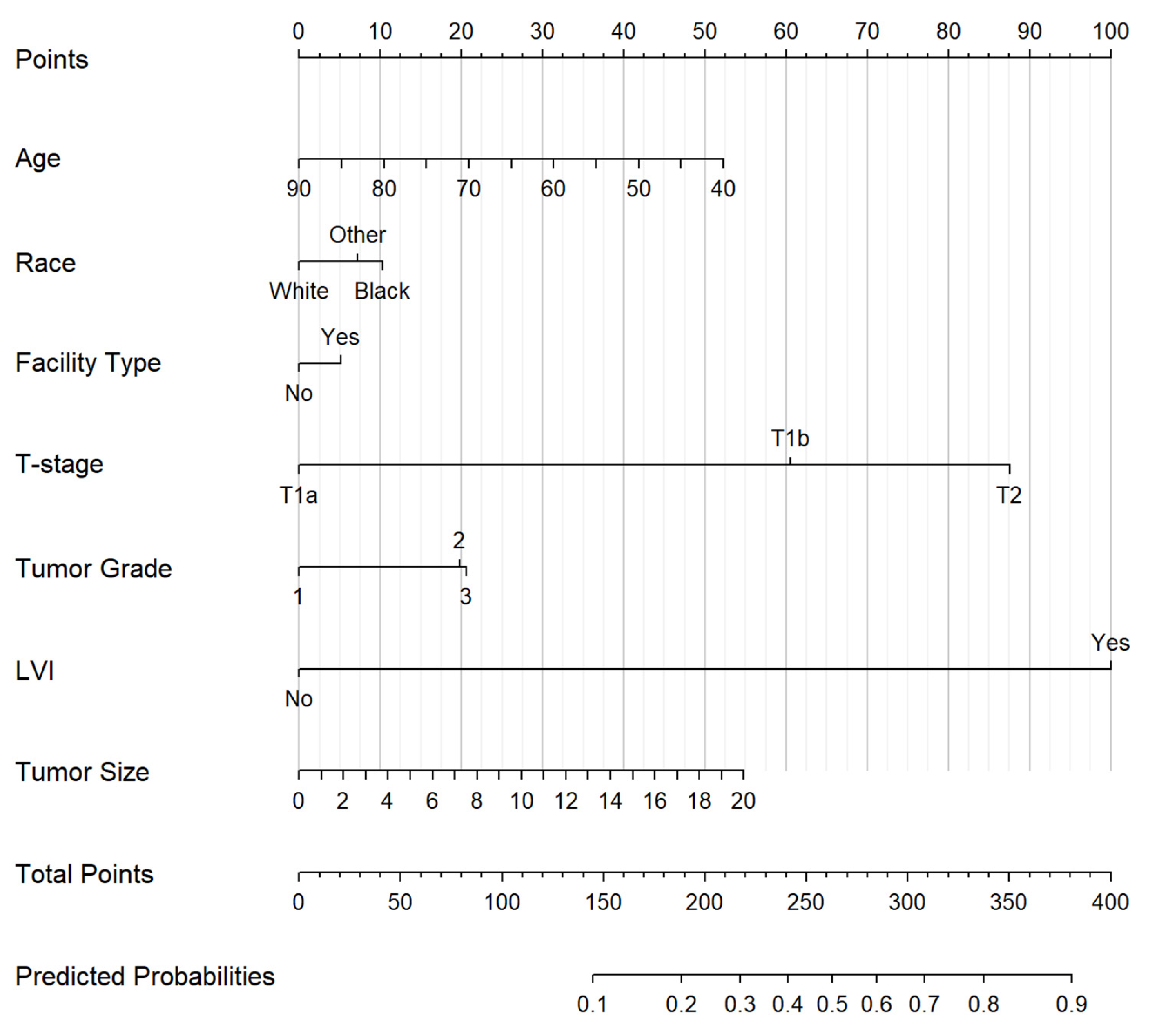
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brooks, R.A.; Fleming, G.F.; Lastra, R.R.; Lee, N.K.; Moroney, J.W.; Son, C.H.; Tatebe, K.; Veneris, J.L. Current recommendations and recent progress in endometrial cancer. CA Cancer J. Clin. 2019, 69, 258–279. [Google Scholar] [CrossRef] [PubMed]
- Bogani, G.; Dowdy, S.C.; Cliby, W.A.; Ghezzi, F.; Rossetti, D.; Mariani, A. Role of pelvic and para-aortic lymphadenectomy in endometrial cancer: Current evidence. J. Obs. Obstet. Gynaecol. Res. 2014, 40, 301–311. [Google Scholar] [CrossRef] [PubMed]
- Daraï, E.; Dubernard, G.; Bats, A.S.; Heitz, D.; Mathevet, P.; Marret, H.; Querleu, D.; Golfier, F.; Leblanc, E.; Rouzier, R.; et al. Sentinel node biopsy for the management of early stage endometrial cancer: Long-term results of the SENTI-ENDO study. Gynecol. Oncol. 2015, 136, 54–59. [Google Scholar] [CrossRef]
- Rossi, E.C.; Kowalski, L.D.; Scalici, J.; Cantrell, L.; Schuler, K.; Hanna, R.K.; Method, M.; Ade, M.; Ivanova, A.; Boggess, J.F.; et al. A comparison of sentinel lymph node biopsy to lymphadenectomy for endometrial cancer staging (FIRES trial): A multicentre, prospective, cohort study. Lancet Oncol. 2017, 18, 384–392. [Google Scholar] [CrossRef]
- Panici, P.B.; Basile, S.; Maneschi, F.; Lissoni, A.A.; Signorelli, M.; Scambia, G.; Angioli, R.; Tateo, S.; Mangili, G.; Katsaros, D.; et al. Systematic pelvic lymphadenectomy vs. no lymphadenectomy in early-stage endometrial carcinoma: Randomized clinical trial. J. Natl. Cancer Inst. 2008, 100, 1707–1716. [Google Scholar] [CrossRef]
- Kitchener, H.; Swart, A.M.; Qian, Q.; Amos, C.; Parmar, M.K. Efficacy of systematic pelvic lymphadenectomy in endometrial cancer (MRC ASTEC trial): A randomised study. Lancet 2009, 373, 125–136. [Google Scholar]
- de Boer, S.M.; Powell, M.E.; Mileshkin, L.; Katsaros, D.; Bessette, P.; Haie-Meder, C.; Ottevanger, P.B.; Ledermann, J.A.; Khaw, P.; D’Amico, R.; et al. Adjuvant chemoradiotherapy versus radiotherapy alone in women with high-risk endometrial cancer (PORTEC-3): Patterns of recurrence and post-hoc survival analysis of a randomised phase 3 trial. Lancet Oncol. 2019, 20, 1273–1285. [Google Scholar] [CrossRef] [PubMed]
- Matei, D.; Filiaci, V.; Randall, M.E.; Mutch, D.; Steinhoff, M.M.; DiSilvestro, P.A.; Moxley, K.M.; Kim, Y.M.; Powell, M.A.; O’Malley, D.M.; et al. Adjuvant Chemotherapy plus Radiation for Locally Advanced Endometrial Cancer. N. Engl. J. Med. 2019, 380, 2317–2326. [Google Scholar] [CrossRef]
- Creasman, W.T.; Ali, S.; Mutch, D.G.; Zaino, R.J.; Powell, M.A.; Mannel, R.S.; Backes, F.J.; DiSilvestro, P.A.; Argenta, P.A.; Pearl, M.L.; et al. Surgical-pathological findings in type 1 and 2 endometrial cancer: An NRG Oncology/Gynecologic Oncology Group study on GOG-210 protocol. Gynecol. Oncol. 2017, 145, 519–525. [Google Scholar] [CrossRef]
- Fox, J.; Weisberg, S. An R Companion to Applied Regression, 3rd ed.; Sage Publications: Thousand Oaks, CA, USA, 2018. [Google Scholar]
- Frank, E.H. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis; Springer: Berlin, Germany, 2015. [Google Scholar]
- Creasman, W.T.; Morrow, C.P.; Bundy, B.N.; Homesley, H.D.; Graham, J.E.; Heller, P.B. Surgical pathologic spread patterns of endometrial cancer. A Gynecologic Oncology Group Study. Cancer 1987, 60, 2035–2041. [Google Scholar] [CrossRef]
- Creutzberg, C.L.; van Putten, W.L.; Koper, P.C.; Lybeert, M.L.; Jobsen, J.J.; Wárlám-Rodenhuis, C.C.; De Winter, K.A.; Lutgens, L.C.; van den Bergh, A.C.; van de Steen-Banasik, E.; et al. Surgery and postoperative radiotherapy versus surgery alone for patients with stage-1 endometrial carcinoma: Multicentre randomised trial. Lancet 2000, 355, 1404–1411. [Google Scholar] [CrossRef] [PubMed]
- Creutzberg, C.L.; van Putten, W.L.; Koper, P.C.; Lybeert, M.L.; Jobsen, J.J.; Wárlám-Rodenhuis, C.C.; De Winter, K.A.; Lutgens, L.C.; van den Bergh, A.C.; van de Steen-Banasik, E.; et al. Nomograms for prediction of outcome with or without adjuvant radiation therapy for patients with endometrial cancer: A pooled analysis of PORTEC-1 and PORTEC-2 trials. Int. J. Radiat. Oncol. Biol. Phys. 2015, 91, 530–539. [Google Scholar] [CrossRef]
- AlHilli, M.M.; Podratz, K.C.; Dowdy, S.C.; Bakkum-Gamez, J.N.; Weaver, A.L.; McGree, M.E.; Keeney, G.L.; Cliby, W.A.; Mariani, A. Risk-scoring system for the individualized prediction of lymphatic dissemination in patients with endometrioid endometrial cancer. Gynecol. Oncol. 2013, 131, 103–108. [Google Scholar] [CrossRef]
- Dong, Y.; Cheng, Y.; Tian, W.; Zhang, H.; Wang, Z.; Li, X.; Shan, B.; Ren, Y.; Wei, L.; Wang, H.; et al. An Externally Validated Nomogram for Predicting Lymph Node Metastasis of Presumed Stage I and II Endometrial Cancer. Front. Oncol. 2019, 9, 1218. [Google Scholar] [CrossRef] [PubMed]
- Pollom, E.L.; Conklin, C.M.; von Eyben, R.; Folkins, A.K.; Kidd, E.A. Nomogram to Predict Risk of Lymph Node Metastases in Patients With Endometrioid Endometrial Cancer. Int. J. Gynecol. Pathol. 2016, 35, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Numanoglu, C.; Corbacioglu Esmer, A.; Ulker, V.; Goksedef, B.C.; Han, A.; Akbayir, O.; Guraslan, B. The prediction of para-aortic lymph node metastasis in endometrioid adenocarcinoma of endometrium. J. Obs. Obstet. Gynaecol. 2014, 34, 177–181. [Google Scholar] [CrossRef]
- Sari, M.E.; Yalcin, İ.; Sahin, H.; Meydanli, M.M.; Gungor, T. Risk factors for paraaortic lymph node metastasis in endometrial cancer. Int. J. Clin. Oncol. 2017, 22, 937–944. [Google Scholar] [CrossRef]
- Mahdi, H.; Jernigan, A.; Nutter, B.; Michener, C.; Rose, P.G. Lymph node metastasis and pattern of recurrence in clinically early stage endometrial cancer with positive lymphovascular space invasion. J. Gynecol. Oncol. 2015, 26, 208–213. [Google Scholar] [CrossRef]
- Jorge, S.; Hou, J.Y.; Tergas, A.I.; Burke, W.M.; Huang, Y.; Hu, J.C.; Ananth, C.V.; Neugut, A.I.; Hershman, D.L.; Wright, J.D. Magnitude of risk for nodal metastasis associated with lymphvascular space invasion for endometrial cancer. Gynecol. Oncol. 2016, 140, 387–393. [Google Scholar] [CrossRef]
- Chambers, L.M.; Jia, X.; Rose, P.G.; AlHilli, M. Impact of treatment modality on overall survival in women with advanced endometrial cancer: A National Cancer Database analysis. Gynecol. Oncol. 2021, 160, 405–412. [Google Scholar] [CrossRef]
- Horne, Z.D.; Teterichko, S.R.; Glaser, S.M.; Wegner, R.E.; Hasan, S.; Crafton, S.M.; Miller, E.M.; Krivak, T.C.; Viswanathan, A.; Olawaiye, A.B.; et al. Race-driven survival differential in women diagnosed with endometrial cancers in the USA. Int. J. Gynecol. Cancer 2020, 30, 1893–1901. [Google Scholar] [CrossRef] [PubMed]
- Mukerji, B.; Baptiste, C.; Chen, L.; Tergas, A.I.; Hou, J.Y.; Ananth, C.V.; Neugut, A.I.; Hershman, D.L.; Wright, J.D. Racial disparities in young women with endometrial cancer. Gynecol. Oncol. 2018, 148, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Sun, X.; Bai, W. Nomograms for Predicting Cancer-Specific and Overall Survival Among Patients With Endometrial Carcinoma: A SEER Based Study. Front. Oncol. 2020, 10, 269. [Google Scholar] [CrossRef] [PubMed]
- Bendifallah, S.; Canlorbe, G.; Laas, E.; Huguet, F.; Coutant, C.; Hudry, D.; Graesslin, O.; Raimond, E.; Touboul, C.; Collinet, P.; et al. A Predictive Model Using Histopathologic Characteristics of Early-Stage Type 1 Endometrial Cancer to Identify Patients at High Risk for Lymph Node Metastasis. Ann. Surg. Oncol. 2015, 22, 4224–4232. [Google Scholar] [CrossRef]
- Taşkın, S.; Şükür, Y.E.; Varlı, B.; Koyuncu, K.; Seval, M.M.; Ateş, C.; Yüksel, S.; Güngör, M.; Ortaç, F. Nomogram with potential clinical use to predict lymph node metastasis in endometrial cancer patients diagnosed incidentally by postoperative pathological assessment. Arch. Gynecol. Obs. 2017, 296, 803–809. [Google Scholar] [CrossRef]
| Full Cohort | White | Black | Other Race | p | |
|---|---|---|---|---|---|
| N = 35,170 | N = 31,274 | N = 2329 | N = 1567 | ||
| Age, years | |||||
| Median (IQR) | 62.0 (56.0; 69.0) | 62.0 (57.0; 69.0) | 62.0 (56.0; 68.0) | 59.0 (53.0; 66.0) | <0.001 |
| Mean (SD) | 62.7 (9.47) | 63.0 (9.47) | 62.0 (8.95) | 59.4 (9.57) | <0.001 |
| Charlson–Deyo Comorbidity Score | <0.001 | ||||
| 0 | 26,430 (75.1%) | 23,680 (75.7%) | 1597 (68.8%) | 1153 (73.6%) | |
| 1 | 7168 (20.4%) | 6262 (20%) | 571 (24.5%) | 335 (21.4%) | |
| 2 | 1278 (3.6%) | 1083 (3.5%) | 130 (5.6%) | 65 (4.2%) | |
| 3 | 294 (0.8%) | 249 (0.8%) | 31 (1.3%) | 14 (0.9%) | |
| Insurance Status | <0.001 | ||||
| Uninsured | 1213 (3.5%) | 1001 (3.2%) | 123 (5.3%) | 89 (5.7%) | |
| Private Insurance | 18,339 (52.1%) | 16,429 (52.5%) | 1036 (44.5%) | 874 (55.8%) | |
| Medicaid | 1660 (4.7%) | 1241 (4.0%) | 225 (9.7%) | 194 (12.4%) | |
| Medicare | 13,513 (38.4%) | 12,227 (39.1%) | 923 (39.6%) | 363 (23.2%) | |
| Other Insurance | 445 (1.3%) | 376 (1.2%) | 22 (0.9%) | 47 (3.0%) | |
| Income | <0.001 | ||||
| <$48,000 | 13,496 (38.4%) | 11,630 (37.2%) | 1450 (62.3%) | 416 (26.5%) | |
| ≥$48,000 | 21,674 (61.6%) | 19,644 (62.8%) | 879 (37.7%) | 1151 (73.5%) | |
| Education | <0.001 | ||||
| Low | 13,841 (39.4%) | 11,568 (37.0%) | 1576 (67.7%) | 697 (44.5%) | |
| High | 21,329 (60.6%) | 19,706 (63%) | 753 (32.3%) | 870 (55.5%) | |
| Practice Type | <0.001 | ||||
| Non-Academic | 27,557 (78.4%) | 24,713 (79%) | 1497 (64.3%) | 1347 (86%) | |
| Academic | 7613 (21.6%) | 6561 (21%) | 832 (35.7%) | 220 (14%) | |
| Pathologic Tumor Stage | <0.001 | ||||
| 1a | 22,240 (63.2%) | 19,618 (62.7%) | 1566 (67.2%) | 1056 (67.4%) | |
| 1b | 10,067 (28.6%) | 9172 (29.3%) | 511 (21.9%) | 384 (24.5%) | |
| 2 | 2863 (8.1%) | 2484 (7.9%) | 252 (10.8%) | 127 (8.1%) | |
| Pathologic Nodal Stage | <0.001 | ||||
| 0 | 32,306 (91.9%) | 28,781 (92%) | 2097 (90%) | 1428 (91.1%) | |
| IIIC1 | 2027 (5.8%) | 1797 (5.8%) | 145 (6.2%) | 85 (5.4%) | |
| IIIC2 | 837 (2.4%) | 696 (2.2%) | 87 (3.7%) | 54 (3.5%) | |
| Pathologic Tumor Grade | <0.001 | ||||
| 1 | 15,324 (43.6%) | 13,834 (44.2%) | 796 (34.2%) | 694 (44.3%) | |
| 2 | 14,011 (39.8%) | 12,530 (40.1%) | 890 (38.2%) | 591 (37.7%) | |
| 3 | 5835 (16.6%) | 4910 (15.7%) | 643 (27.64%) | 282 (18%) | |
| LVI | 0.88 | ||||
| Absent | 28,125 (80%) | 25,005 (80%) | 1871 (80.3%) | 1249 (79.7%) | |
| Present | 7045 (20%) | 6269 (20%) | 458 (19.7%) | 318 (20.3%) | |
| Tumor Size (cm) | |||||
| Mean (SD) | 3.94 (2.86) | 3.9 (2.87) | 4.53 (2.7) | 3.86 (2.64) | <0.001 |
| Covariates | Univariate | Multivariable | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age | 0.995 (0.991 to 0.999) | 0.02 | 0.98 (0.98 to 0.99) | <0.001 |
| Race | ||||
| White | 1.000 | - | 1.000 | - |
| Black | 1.28 (1.11 to 1.45) | <0.001 | 1.19 (1.01 to 1.40) | 0.04 |
| Other | 1.12 (0.94 to 1.34) | 0.20 | 1.14 (0.93 to 1.38) | 0.21 |
| Charlson–Deyo Comorbidity Score | ||||
| 0 | 1.000 | - | 1.000 | - |
| 1 | 0.94 (0.86 to 1.04) | 0.24 | 0.99 (0.88 to 1.10) | 0.97 |
| 2 | 1.05 (0.86 to 1.28) | 0.60 | 1.04 (0.83 to 1.30) | 0.72 |
| 3 | 1.27 (0.85 to 1.83) | 0.21 | 1.28 (0.82 to 1.93) | 0.25 |
| Insurance Status | ||||
| Uninsured | 1.000 | - | 1.000 | - |
| Private Insurance | 0.81 (0.67 to 0.99) | 0.04 | 1.13 (0.91 to 1.42) | 0.28 |
| Medicaid | 1.29 (1.01 to 1.64) | 0.04 | 1.42 (1.09 to 1.88) | 0.01 |
| Medicare | 0.83 (0.68 to 1.02) | 0.07 | 1.19 (0.94 to 1.51) | 0.16 |
| Other Insurance | 0.87 (0.58 to 1.26) | 0.47 | 1.12 (0.72 to 1.71) | 0.61 |
| Income | ||||
| <$48,000 | 1.000 | - | 1.000 | - |
| ≥$48,000 | 0.92 (0.85 to 0.997) | 0.04 | 0.94 (0.85 to 1.04) | 0.23 |
| Education | ||||
| Low | 1.000 | - | 1.000 | - |
| High | 0.92 (0.85 to 0.99) | 0.03 | 1.03 (0.93 to 1.14) | 0.53 |
| Practice Type | ||||
| Non-Academic | 1.000 | - | 1.000 | - |
| Academic | 1.01 (0.92 to 1.11) | 0.78 | 1.11 (0.995 to 1.22) | 0.06 |
| Year of Diagnosis | 1.03 (1.007 to 1.05) | 0.01 | 1.01 (0.99 to 1.04) | 0.42 |
| Pathologic Tumor Stage | ||||
| 1a | 1.000 | - | 1.000 | - |
| 1b | 5.36 (4.88 to 5.90) | <0.001 | 3.08 (2.78 to 3.42) | <0.001 |
| 2 | 10.66 (9.52 to 11.94) | <0.001 | 5.10 (4.50 to 5.78) | <0.001 |
| Pathologic Tumor Grade | ||||
| 1 | 1.000 | - | 1.000 | - |
| 2 | 2.22 (2.02 to 2.44) | <0.001 | 1.45 (1.31 to 1.61) | <0.001 |
| 3 | 3.48 (3.13 to 3.86) | <0.001 | 1.47 (1.30 to 1.65) | <0.001 |
| LVI | ||||
| Absent | 1.000 | - | 1.000 | - |
| Present | 10.44 (9.61 to 11.35) | <0.001 | 6.44 (5.88 to 7.05) | <0.001 |
| Tumor size (cm) | 1.15 (1.14 to 1.17) | <0.001 | 1.05 (1.04 to 1.06) | <0.001 |
| Covariates | Pelvic | Paraaortic | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age | 0.98 (0.98 to 0.99) | <0.001 | 0.97 (0.96 to 0.98) | <0.001 |
| Race | ||||
| White | 1.000 | - | 1.000 | - |
| Black | 1.05 (0.86 to 1.26) | 0.65 | 1.64 (1.27 to 2.09) | <0.001 |
| Other | 0.98 (0.76 to 1.24) | 0.85 | 1.54 (1.12 to 2.07) | 0.006 |
| Charlson–Deyo Comorbidity Score | ||||
| 0 | 1.000 | - | 1.000 | - |
| 1 | 0.99 (0.88 to 1.12) | 0.93 | 0.99 (0.82 to 1.18) | 0.88 |
| 2 | 1.14 (0.89 to 1.44) | 0.31 | 0.84 (0.54 to 1.26) | 0.43 |
| 3 | 1.28 (0.77 to 2.03) | 0.31 | 1.26 (0.58 to 2.43) | 0.53 |
| Insurance Status | ||||
| Uninsured | 1.000 | - | 1.000 | - |
| Private Insurance | 1.29 (0.99 to 1.70) | 0.06 | 0.88 (0.63 to 1.25) | 0.45 |
| Medicaid | 1.62 (1.18 to 2.25) | 0.003 | 1.10 (0.72 to 1.68) | 0.66 |
| Medicare | 1.35 (1.02 to 1.81) | 0.04 | 0.93 (0.65 to 1.35) | 0.67 |
| Other Insurance | 1.37 (0.83 to 2.20) | 0.21 | 0.78 (0.34 to 1.60) | 0.52 |
| Income | ||||
| <$48,000 | 1.000 | - | 1.000 | - |
| ≥$48,000 | 0.92 (0.82 to 1.04) | 0.17 | 0.98 (0.82 to 1.16) | 0.79 |
| Education | ||||
| Low | 1.000 | - | 1.000 | - |
| High | 1.06 (0.94 to 1.19) | 0.34 | 0.98 (0.82 to 1.16) | 0.8 |
| Practice Type | ||||
| Non-Academic | 1.000 | - | 1.000 | - |
| Academic | 1.13 (1.002 to 1.27) | 0.04 | 1.01 (0.85 to 1.21) | 0.88 |
| Year of Diagnosis | 1.01 (0.98 to 1.04) | 0.51 | 1.01 (0.97 to 1.06) | 0.61 |
| Pathologic Tumor Stage | ||||
| 1a | 1.000 | - | 1.000 | - |
| 1b | 2.91 (2.58 to 3.28) | <0.001 | 3.52 (2.91 to 4.27) | <0.001 |
| 2 | 5.00 (4.34 to 5.76) | <0.001 | 5.33 (4.28 to 6.65) | <0.001 |
| Pathologic Tumor Grade | ||||
| 1 | 1.000 | - | 1.000 | - |
| 2 | 1.47 (1.31 to 1.65) | <0.001 | 1.38 (1.15 to 1.66) | <0.001 |
| 3 | 1.45 (1.27 to 1.67) | <0.001 | 1.40 (1.14 to 1.72) | 0.001 |
| Lymphovascular Invasion | ||||
| Absent | 1.000 | - | 1.000 | - |
| Present | 5.77 (5.20 to 6.39) | <0.001 | 8.64 (7.32 to 10.24) | <0.001 |
| Tumor Size (cm) | 1.04 (1.03 to 1.06) | <0.001 | 1.05 (1.03 to 1.07) | <0.001 |
| Covariates | Black | White | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age | 0.98 (0.96 to 0.998) | 0.03 | 0.98 (0.97 to 0.99) | <0.001 |
| Charlson–Deyo Comorbidity Score | ||||
| 0 | 1.000 | - | 1.000 | - |
| 1 | 1.25 (0.86 to 1.79) | 0.23 | 0.96 (0.85 to 1.08) | 0.47 |
| 2 | 0.65 (0.28 to 1.36) | 0.28 | 1.07 (0.84 to 1.35) | 0.57 |
| 3 | 0.96 (0.20 to 3.40) | 0.95 | 1.26 (0.78 to 1.96) | 0.32 |
| Insurance Status | ||||
| Uninsured | 1.000 | - | 1.000 | - |
| Private Insurance | 0.96 (0.49 to 1.96) | 0.86 | 1.14 (0.90 to 1.47) | 0.3 |
| Medicaid | 1.16 (0.53 to 2.62) | 0.71 | 1.45 (1.07 to 1.97) | 0.02 |
| Medicare | 0.98 (0.48 to 2.11) | 0.96 | 1.21 (0.94 to 1.59) | 0.15 |
| Other Insurance | 0.56 (0.07 to 2.83) | 0.52 | 1.17 (0.73 to 1.86) | 0.5 |
| Income | ||||
| <$48,000 | 1.000 | - | 1.000 | - |
| ≥$48,000 | 0.83 (0.56 to 1.22) | 0.34 | 0.94 (0.84 to 1.05) | 0.25 |
| Education | ||||
| Low | 1.000 | - | 1.000 | - |
| High | 1.05 (0.70 to 1.57) | 0.81 | 1.04 (0.93 to 1.15) | 0.52 |
| Practice Type | ||||
| Non-Academic | 1.000 | - | 1.000 | - |
| Academic | 1.19 (0.86 to 1.65) | 0.28 | 1.07 (0.96 to 1.20) | 0.22 |
| Year of Diagnosis | 0.96 (0.49 to 1.96) | 0.4 | 1.009 (0.98 to 1.04) | 0.49 |
| Pathologic Tumor Stage | ||||
| 1a | 1.000 | - | 1.000 | - |
| 1b | 2.40 (1.65 to 3.52) | <0.001 | 3.09 (2.77 to 3.45) | <0.001 |
| 2 | 4.99 (3.31 to 7.54) | <0.001 | 5.07 (4.42 to 5.80) | <0.001 |
| Pathologic Tumor Grade | ||||
| 1 | 1.000 | - | 1.000 | - |
| 2 | 2.40 (1.46 to 4.09) | 0.001 | 1.41 (1.27 to 1.57) | <0.001 |
| 3 | 4.01 (2.46 to 6.78) | <0.001 | 1.37 (1.21 to 1.56) | 0.003 |
| Lymphovascular Invasion | ||||
| Absent | 1.000 | - | 1.000 | - |
| Present | 5.48 (3.95 to 7.65) | <0.001 | 6.56 (5.96 to 7.22) | <0.001 |
| Tumor Size (cm) | 1.07 (1.01 to 1.13) | 0.01 | 1.05 (1.04 to 1.06) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anderson, E.M.; Luu, M.; Kamrava, M. Demographic Factors Predict Risk of Lymph Node Involvement in Patients with Endometrial Adenocarcinoma. Biology 2023, 12, 982. https://doi.org/10.3390/biology12070982
Anderson EM, Luu M, Kamrava M. Demographic Factors Predict Risk of Lymph Node Involvement in Patients with Endometrial Adenocarcinoma. Biology. 2023; 12(7):982. https://doi.org/10.3390/biology12070982
Chicago/Turabian StyleAnderson, Eric M., Michael Luu, and Mitchell Kamrava. 2023. "Demographic Factors Predict Risk of Lymph Node Involvement in Patients with Endometrial Adenocarcinoma" Biology 12, no. 7: 982. https://doi.org/10.3390/biology12070982
APA StyleAnderson, E. M., Luu, M., & Kamrava, M. (2023). Demographic Factors Predict Risk of Lymph Node Involvement in Patients with Endometrial Adenocarcinoma. Biology, 12(7), 982. https://doi.org/10.3390/biology12070982











