Whole-Genome Sequencing and Drug-Susceptibility Analysis of Serial Mycobacterium abscessus Isolates from Thai Patients
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Clinical Mycobacterium abscessus Isolates
2.1.1. Mycobacterium abscessus Collection and Study Setting
2.1.2. Bacterial Culture and DNA Extraction
2.2. Identifying Recurrent Infection of M. abscessus
2.2.1. Whole-Genome Sequencing
2.2.2. Analysis Pipeline for WGS
2.2.3. Phylogenetic Analysis
2.3. Mutation Rate Analysis
2.3.1. Mutation Rate Estimation
2.3.2. Statistical Comparisons of Mutation Rates
2.4. Drug-Resistance Analysis
2.4.1. Drug-Susceptibility Testing Using the Broth-Microdilution Method
2.4.2. Known Mutations Related to Drug Resistance
3. Results
3.1. Study Population and Study Setting
3.2. Distinguishing between Persistent and Re-infection Cases in Recurrent M. abscessus Infection and Cluster Analysis
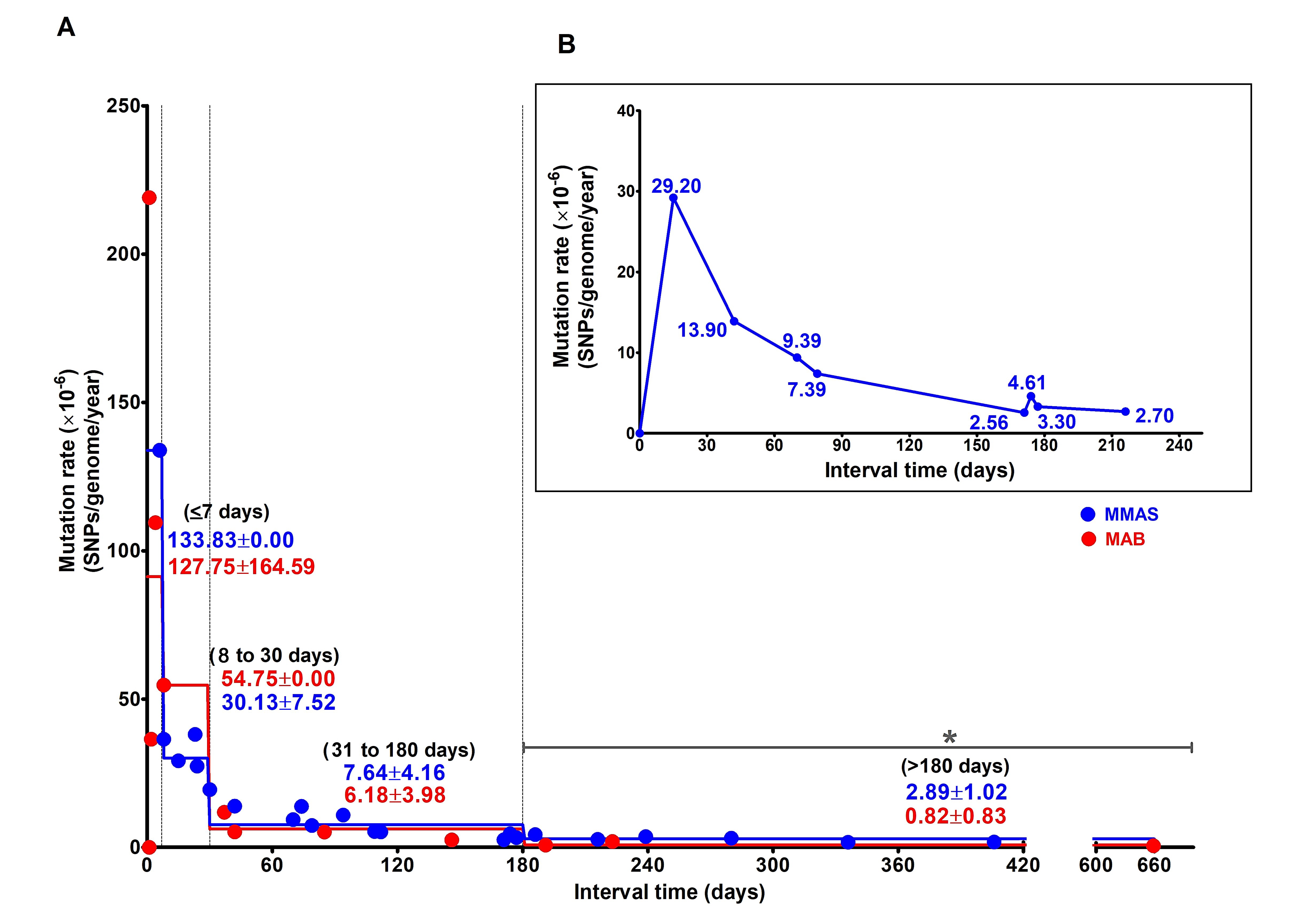
3.3. Estimation of Mutation Rate of M. abscessus during Persistent Infection (PI) and Persistent Colonization
3.4. Drug Resistance-Conferring Mutations Related to MIC Valuese
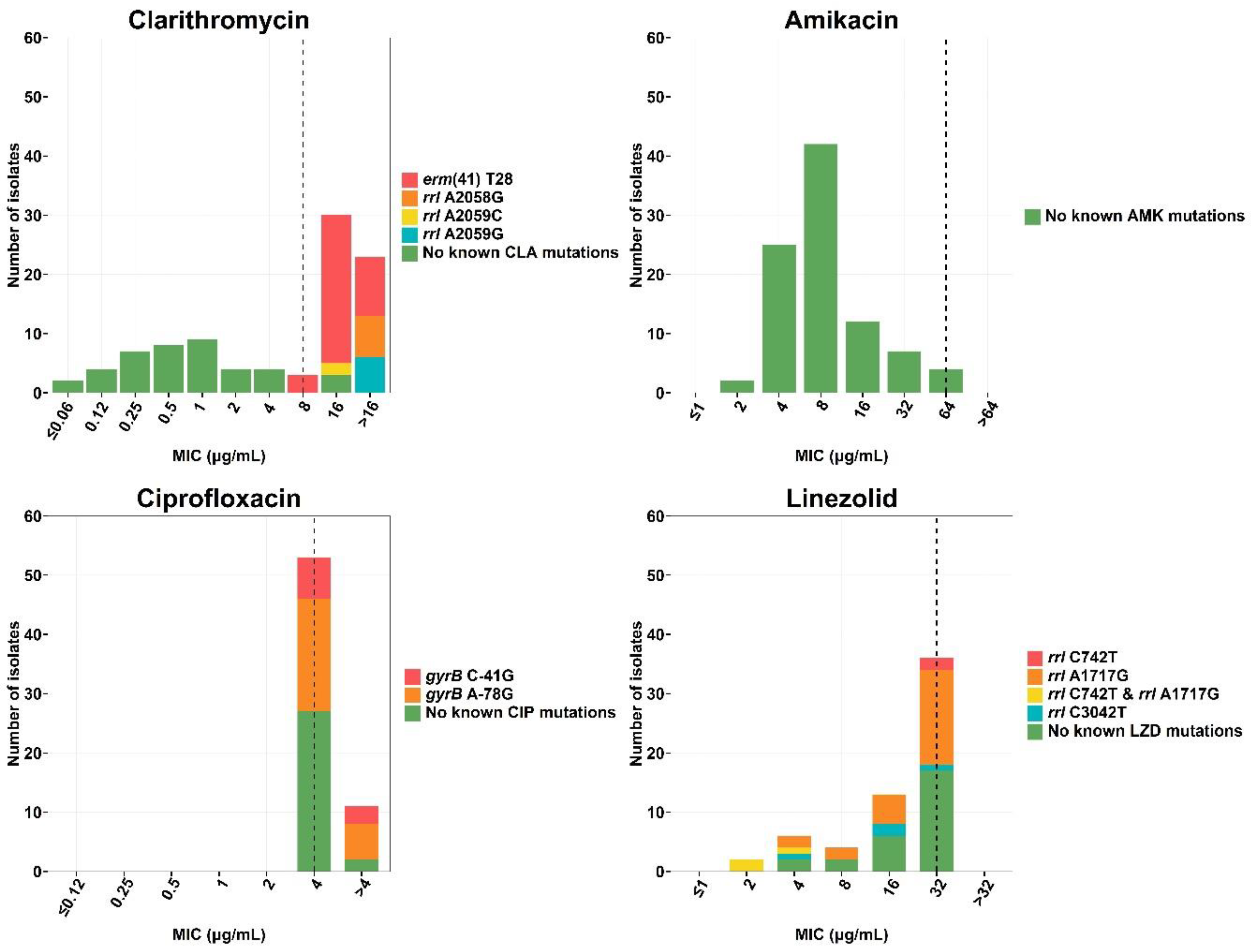
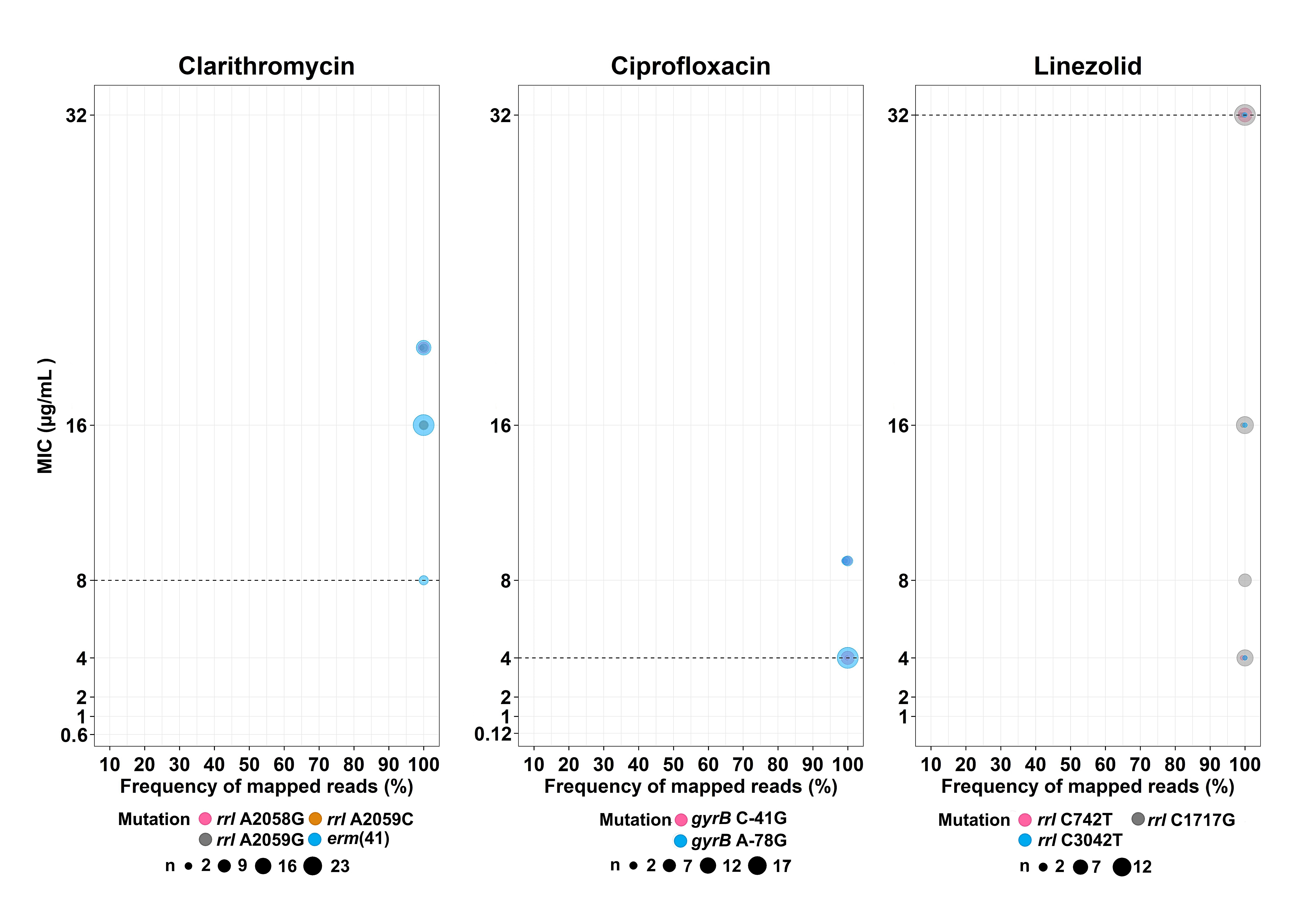
3.4.1. Clarithromycin
3.4.2. Amikacin
3.4.3. Ciprofloxacin
3.4.4. Linezolid
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, M.R.; Sheng, W.H.; Hung, C.C.; Yu, C.J.; Lee, L.N.; Hsueh, P.R. Mycobacterium abscessus Complex Infections in Humans. Emerg. Infect. Dis. 2015, 21, 1638–1646. [Google Scholar] [CrossRef]
- Hurst-Hess, K.; Rudra, P.; Ghosh, P. Mycobacterium abscessus WhiB7 Regulates a Species-Specific Repertoire of Genes to Confer Extreme Antibiotic Resistance. Antimicrob. Agents Chemother. 2017, 61, e01347-17. [Google Scholar] [CrossRef] [PubMed]
- Pryjma, M.; Burian, J.; Kuchinski, K.; Thompson, C.J. Antagonism between Front-Line Antibiotics Clarithromycin and Amikacin in the Treatment of Mycobacterium abscessus Infections Is Mediated by the whiB7 Gene. Antimicrob. Agents Chemother. 2017, 61, e01353-17. [Google Scholar] [CrossRef] [PubMed]
- Kham-Ngam, I.; Chetchotisakd, P.; Ananta, P.; Chaimanee, P.; Reechaipichitkul, W.; Lulitanond, V.; Namwat, W.; Faksri, K. Differentiation between persistent infection/colonization and re-infection/re-colonization of Mycobacterium abscessus isolated from patients in Northeast Thailand. Infect. Genet. Evol. J. Mol. Epidemiol. Evol. Genet. Infect. Dis. 2019, 68, 35–42. [Google Scholar] [CrossRef] [PubMed]
- La Rosa, R.; Johansen, H.K.; Molin, S. Persistent Bacterial Infections, Antibiotic Treatment Failure, and Microbial Adaptive Evolution. Antibiotics 2022, 11, 419. [Google Scholar] [CrossRef] [PubMed]
- Davidson, R.M.; Hasan, N.A.; Reynolds, P.R.; Totten, S.; Garcia, B.; Levin, A.; Ramamoorthy, P.; Heifets, L.; Daley, C.L.; Strong, M. Genome sequencing of Mycobacterium abscessus isolates from patients in the United States and comparisons to globally diverse clinical strains. J. Clin. Microbiol. 2014, 52, 3573–3582. [Google Scholar] [CrossRef] [PubMed]
- Shaw, L.P.; Doyle, R.M.; Kavaliunaite, E.; Spencer, H.; Balloux, F.; Dixon, G.; Harris, K.A. Children with Cystic Fibrosis Are Infected with Multiple Subpopulations of Mycobacterium abscessus With Different Antimicrobial Resistance Profiles. Clin. Infect. Dis. 2019, 69, 1678–1686. [Google Scholar] [CrossRef] [PubMed]
- Bryant, J.M.; Grogono, D.M.; Greaves, D.; Foweraker, J.; Roddick, I.; Inns, T.; Reacher, M.; Haworth, C.S.; Curran, M.D.; Harris, S.R.; et al. Whole-genome sequencing to identify transmission of Mycobacterium abscessus between patients with cystic fibrosis: A retrospective cohort study. Lancet 2013, 381, 1551–1560. [Google Scholar] [CrossRef]
- Bryant, J.M.; Grogono, D.M.; Rodriguez-Rincon, D.; Everall, I.; Brown, K.P.; Moreno, P.; Verma, D.; Hill, E.; Drijkoningen, J.; Gilligan, P.; et al. Emergence and spread of a human-transmissible multidrug-resistant nontuberculous mycobacterium. Science 2016, 354, 751–757. [Google Scholar] [CrossRef]
- Crow, J.F. The high spontaneous mutation rate: Is it a health risk? Proc. Natl. Acad. Sci. USA 1997, 94, 8380–8386. [Google Scholar] [CrossRef] [Green Version]
- Araten, D.J. Mutation Rate. In Encyclopedia of Cancer; Schwab, M., Ed.; Springer: Berlin/Heidelberg, Germany, 2011; pp. 2412–2416. [Google Scholar]
- Wielgoss, S.; Barrick, J.E.; Tenaillon, O.; Wiser, M.J.; Dittmar, W.J.; Cruveiller, S.; Chane-Woon-Ming, B.; Médigue, C.; Lenski, R.E.; Schneider, D. Mutation rate dynamics in a bacterial population reflect tension between adaptation and genetic load. Proc. Natl. Acad. Sci. USA 2013, 110, 222–227. [Google Scholar] [CrossRef]
- Howard, S.T. Recent progress towards understanding genetic variation in the Mycobacterium abscessus complex. Tuberculosis 2013, 93, S15–S20. [Google Scholar] [CrossRef]
- Band, V.I.; Weiss, D.S. Heteroresistance: A cause of unexplained antibiotic treatment failure? PLoS Pathog. 2019, 15, e1007726. [Google Scholar] [CrossRef]
- Shin, S.S.; Modongo, C.; Baik, Y.; Allender, C.; Lemmer, D.; Colman, R.E.; Engelthaler, D.M.; Warren, R.M.; Zetola, N.M. Mixed Mycobacterium tuberculosis-Strain Infections Are Associated With Poor Treatment Outcomes Among Patients With Newly Diagnosed Tuberculosis, Independent of Pretreatment Heteroresistance. J. Infect. Dis. 2018, 218, 1974–1982. [Google Scholar] [CrossRef]
- Bouzinbi, N.; Marcy, O.; Bertolotti, T.; Chiron, R.; Bemer, P.; Pestel-Caron, M.; Peuchant, O.; Guet-Revillet, H.; Fangous, M.S.; Héry-Arnaud, G.; et al. Evaluation of the GenoType NTM-DR assay performance for the identification and molecular detection of antibiotic resistance in Mycobacterium abscessus complex. PLoS ONE 2020, 15, e0239146. [Google Scholar] [CrossRef]
- Larsen, M.H.; Biermann, K.; Tandberg, S.; Hsu, T.; Jacobs, W.R., Jr. Genetic Manipulation of Mycobacterium tuberculosis. Curr. Protoc. Microbiol. 2007, 6, 10A.2.1–10A.2.21. [Google Scholar] [CrossRef]
- Simon, A. FastQC: A Quality Control Tool for High Throughput Sequence Data 2010. Available online: http://www.bioinformatics.babraham.ac.uk/projects/fastqc/ (accessed on 7 December 2018).
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef]
- Li, H. Aligning sequence reads, clone sequences and assembly contigs with BWA-MEM. arXiv 2013, arXiv:1303.3997v2. [Google Scholar]
- Li, H.; Handsaker, B.; Wysoker, A.; Fennell, T.; Ruan, J.; Homer, N.; Marth, G.; Abecasis, G.; Durbin, R. The Sequence Alignment/Map format and SAMtools. Bioinformatics 2009, 25, 2078–2079. [Google Scholar] [CrossRef]
- McKenna, A.; Hanna, M.; Banks, E.; Sivachenko, A.; Cibulskis, K.; Kernytsky, A.; Garimella, K.; Altshuler, D.; Gabriel, S.; Daly, M.; et al. The Genome Analysis Toolkit: A MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010, 20, 1297–1303. [Google Scholar] [CrossRef]
- Kumar, S.; Stecher, G.; Tamura, K. MEGA7: Molecular Evolutionary Genetics Analysis Version 7.0 for Bigger Datasets. Mol. Biol. Evol. 2016, 33, 1870–1874. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Letunic, I.; Bork, P. Interactive tree of life (iTOL) v3: An online tool for the display and annotation of phylogenetic and other trees. Nucleic Acids Res. 2016, 44, W242–W245. [Google Scholar] [CrossRef] [PubMed]
- Kaewprasert, O.; Tongsima, S.; Ong, R.T.; Faksri, K. Optimized analysis parameters of variant calling for whole genome-based phylogeny of Mycobacteroides abscessus. Arch. Microbiol. 2022, 204, 190. [Google Scholar] [CrossRef] [PubMed]
- Ford, C.B.; Lin, P.L.; Chase, M.R.; Shah, R.R.; Iartchouk, O.; Galagan, J.; Mohaideen, N.; Ioerger, T.R.; Sacchettini, J.C.; Lipsitch, M.; et al. Use of whole genome sequencing to estimate the mutation rate of Mycobacterium tuberculosis during latent infection. Nat. Genet. 2011, 43, 482–486. [Google Scholar] [CrossRef] [PubMed]
- Lopeman, R.C.; Harrison, J.; Desai, M.; Cox, J.A.G. Mycobacterium abscessus: Environmental Bacterium Turned Clinical Nightmare. Microorganisms 2019, 7, 90. [Google Scholar] [CrossRef]
- Tan, J.L.; Ng, K.P.; Ong, C.S.; Ngeow, Y.F. Genomic Comparisons Reveal Microevolutionary Differences in Mycobacterium abscessus Subspecies. Front. Microbiol. 2017, 8, 2042. [Google Scholar] [CrossRef]
- Bohr, L.L.; Youngblom, M.A.; Eldholm, V.; Pepperell, C.S. Genome reorganization during emergence of host-associated Mycobacterium abscessus. Microb. Genom. 2021, 7, 000706–000720. [Google Scholar] [CrossRef]
- Lewin, A.; Kamal, E.; Semmler, T.; Winter, K.; Kaiser, S.; Schäfer, H.; Mao, L.; Eschenhagen, P.; Grehn, C.; Bender, J.; et al. Genetic diversification of persistent Mycobacterium abscessus within cystic fibrosis patients. Virulence 2021, 12, 2415–2429. [Google Scholar] [CrossRef]
- Tröbner, W.; Piechocki, R. Selection against hypermutability in Escherichia coli during long term evolution. Mol. Gen. Genet. MGG 1984, 198, 177–178. [Google Scholar] [CrossRef]
- Eyre-Walker, A.; Keightley, P.D. The distribution of fitness effects of new mutations. Nat. Rev. Genet. 2007, 8, 610–618. [Google Scholar] [CrossRef]
- Sniegowski, P.D.; Gerrish, P.J.; Johnson, T.; Shaver, A. The evolution of mutation rates: Separating causes from consequences. BioEssays News Rev. Mol. Cell. Dev. Biol. 2000, 22, 1057–1066. [Google Scholar] [CrossRef]
- Sturtevant, A.H. Essays on evolution. I. On the effects of selection on mutation rate. Q. Rev. Biol. 1937, 12, 464–467. [Google Scholar] [CrossRef]
- Stout, J.E.; Floto, R.A. Treatment of Mycobacterium abscessus: All macrolides are equal, but perhaps some are more equal than others. Am. J. Respir. Crit. Care Med. 2012, 186, 822–823. [Google Scholar] [CrossRef]
- Jeong, S.H.; Kim, S.Y.; Huh, H.J.; Ki, C.S.; Lee, N.Y.; Kang, C.I.; Chung, D.R.; Peck, K.R.; Shin, S.J.; Koh, W.J. Mycobacteriological characteristics and treatment outcomes in extrapulmonary Mycobacterium abscessus complex infections. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2017, 60, 49–56. [Google Scholar] [CrossRef]
- Wilson, J.W.; Estes, L.L. Mayo clinic antimicrobial therapy: Quick guide. In Nontuberculosis Mycobacteria Management Pearls; Mayo Clinic Scientific Press/Oxford University Press: Cary, NC, USA, 2018. [Google Scholar]
- Nash, K.A.; Brown-Elliott, B.A.; Wallace, R.J., Jr. A novel gene, erm(41), confers inducible macrolide resistance to clinical isolates of Mycobacterium abscessus but is absent from Mycobacterium chelonae. Antimicrob. Agents Chemother. 2009, 53, 1367–1376. [Google Scholar] [CrossRef]
- Bastian, S.; Veziris, N.; Roux, A.L.; Brossier, F.; Gaillard, J.L.; Jarlier, V.; Cambau, E. Assessment of clarithromycin susceptibility in strains belonging to the Mycobacterium abscessus group by erm(41) and rrl sequencing. Antimicrob. Agents Chemother. 2011, 55, 775–781. [Google Scholar] [CrossRef]
- Li, B.; Yang, S.; Chu, H.; Zhang, Z.; Liu, W.; Luo, L.; Ma, W.; Xu, X. Relationship between Antibiotic Susceptibility and Genotype in Mycobacterium abscessus Clinical Isolates. Front. Microbiol. 2017, 8, 1739. [Google Scholar] [CrossRef]
- Carneiro, M.D.S.; Nunes, L.S.; David, S.M.M.; Barth, A.L. Lack of association between rrl and erm(41) mutations and clarithromycin resistance in Mycobacterium abscessus complex. Mem. Do Inst. Oswaldo Cruz 2017, 112, 775–778. [Google Scholar] [CrossRef]
- Vester, B.; Douthwaite, S. Macrolide resistance conferred by base substitutions in 23S rRNA. Antimicrob. Agents Chemother. 2001, 45, 1–12. [Google Scholar] [CrossRef]
- Lipworth, S.; Hough, N.; Leach, L.; Morgan, M.; Jeffery, K.; Andersson, M.; Robinson, E.; Smith, E.G.; Crook, D.; Peto, T.; et al. Whole-Genome Sequencing for Predicting Clarithromycin Resistance in Mycobacterium Abscessus. Antimicrob. Agents Chemother. 2019, 63. [Google Scholar] [CrossRef]
- Monego, F.; Duarte, R.S.; Biondo, A.W. gyrA and gyrB gene mutation in ciprofloxacin-resistant Mycobacterium massiliense clinical isolates from Southern Brazil. Microb. Drug Resist. 2012, 18, 1–6. [Google Scholar] [CrossRef]
- Ye, M.; Xu, L.; Zou, Y.; Li, B.; Guo, Q.; Zhang, Y.; Zhan, M.; Xu, B.; Yu, F.; Zhang, Z.; et al. Molecular Analysis of Linezolid-Resistant Clinical Isolates of Mycobacterium abscessus. Antimicrob. Agents Chemother. 2019, 63, e01842-18. [Google Scholar] [CrossRef]
- Abdelaal, H.F.M.; Chan, E.D.; Young, L.; Baldwin, S.L.; Coler, R.N. Mycobacterium abscessus: It’s Complex. Microorganisms 2022, 10, 1454. [Google Scholar] [CrossRef]
- Yagi, K.; Ishii, M.; Namkoong, H.; Asami, T.; Iketani, O.; Asakura, T.; Suzuki, S.; Sugiura, H.; Yamada, Y.; Nishimura, T.; et al. The efficacy, safety, and feasibility of inhaled amikacin for the treatment of difficult-to-treat non-tuberculous mycobacterial lung diseases. BMC Infect. Dis. 2017, 17, 558–566. [Google Scholar] [CrossRef]
- Schmalstig, A.A.; Zorn, K.M.; Murcia, S.; Robinson, A.; Savina, S.; Komarova, E.; Makarov, V.; Braunstein, M.; Ekins, S. Mycobacterium abscessus drug discovery using machine learning. Tuberculosis 2022, 132, 102168–102175. [Google Scholar] [CrossRef]
- Thomas, S.E.; McCarthy, W.J.; El Bakali, J.; Brown, K.P.; Kim, S.Y.; Blaszczyk, M.; Mendes, V.; Abell, C.; Floto, R.A.; Coyne, A.G.; et al. Structural Characterization of Mycobacterium abscessus Phosphopantetheine Adenylyl Transferase Ligand Interactions: Implications for Fragment-Based Drug Design. Front. Mol. Biosci. 2022, 9, 1–12. [Google Scholar] [CrossRef]
- Richter, A.; Strauch, A.; Chao, J.; Ko, M.; Av-Gay, Y. Screening of Preselected Libraries Targeting Mycobacterium abscessus for Drug Discovery. Antimicrob. Agents Chemother. 2018, 62, e00828-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Infection Status | M. abscessusa | |
|---|---|---|
| MAB | MMAS | |
| Persistent infection (PI) | ≤7 SNPs (n = 9) | ≤14 SNPs (n = 11) |
| Re-infection (RI) | NA | ≥102 SNPs (n = 2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaewprasert, O.; Nonghanphithak, D.; Chetchotisakd, P.; Namwat, W.; Ong, R.T.-H.; Faksri, K. Whole-Genome Sequencing and Drug-Susceptibility Analysis of Serial Mycobacterium abscessus Isolates from Thai Patients. Biology 2022, 11, 1319. https://doi.org/10.3390/biology11091319
Kaewprasert O, Nonghanphithak D, Chetchotisakd P, Namwat W, Ong RT-H, Faksri K. Whole-Genome Sequencing and Drug-Susceptibility Analysis of Serial Mycobacterium abscessus Isolates from Thai Patients. Biology. 2022; 11(9):1319. https://doi.org/10.3390/biology11091319
Chicago/Turabian StyleKaewprasert, Orawee, Ditthawat Nonghanphithak, Ploenchan Chetchotisakd, Wises Namwat, Rick Twee-Hee Ong, and Kiatichai Faksri. 2022. "Whole-Genome Sequencing and Drug-Susceptibility Analysis of Serial Mycobacterium abscessus Isolates from Thai Patients" Biology 11, no. 9: 1319. https://doi.org/10.3390/biology11091319
APA StyleKaewprasert, O., Nonghanphithak, D., Chetchotisakd, P., Namwat, W., Ong, R. T.-H., & Faksri, K. (2022). Whole-Genome Sequencing and Drug-Susceptibility Analysis of Serial Mycobacterium abscessus Isolates from Thai Patients. Biology, 11(9), 1319. https://doi.org/10.3390/biology11091319






