4.1. Repeatability and Feasibility
While Mode3 (3D reconstructions with anaglyph glasses) was the best viewing modality within observer 1, the agreement between the two observers on that modality was only moderate. This could point to personal aptitude to use anaglyph glasses, based on individual eyesight. Observer 1 as a habitual spectacle wearer could have handled anaglyph glasses differently from observer 2, who does not habitually wear glasses. In fact, observer 2 reported some degree of dizziness after the observations while wearing anaglyph glasses. This could explain the relatively low degree of agreement between both observers in this mode, especially since Mode1 (2D slices) and Mode2 (3D reconstructions without anaglyph glasses) resulted in perfect agreement between them. Before introducing anaglyph glasses into forensic casework, future observers could thus be advised to test their personal affinity for this modality, considering their eyesight.
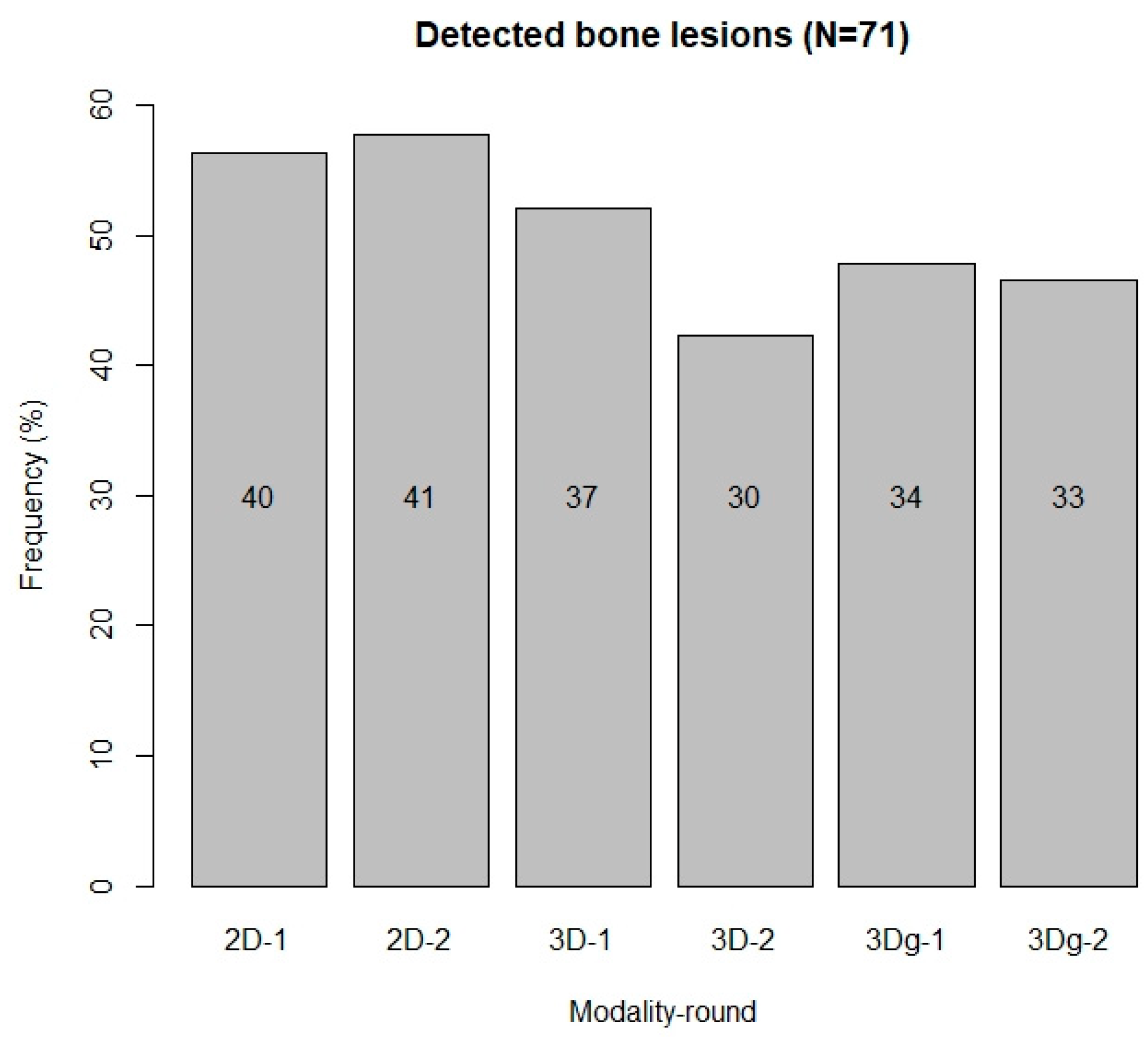
The generally superior performance of Mode1 in the direct comparison of detected bone lesions with the forensic reports is surprising. We expected a superiority of the 3D reconstructions with the ability to rotate and zoom. However, minute bone lesions were more obvious on the 2D slices, while on the 3D reconstructions, due to contrast issues, we faced greater challenges spotting them. Furthermore, on the 2D slices, the observer’s view is limited to the expanse of the present slice, while on the 3D reconstructions, the observer needs a clear focus on bone lesions. Hence, while Mode1 and Mode2 performed best between observers and Mode3 was superior in the agreement within observer 1, Mode1 was superior in the direct comparison with the forensic reports.
Regarding the comparison with the combined forensic reports, observer 1 did not detect between 30 and 38 of the 71 bone lesions (42.2% to 53.5%), depending on the modality. These findings demonstrate the difficulty to interpret skeletal lesions from tomographic data, even in the presence of sound anatomical knowledge and previous experience with radiographic data. This difficulty could partly be due to the specific challenge with the brittle and usually fragmented ribs in forensic casework, depriving forensic anthropologists of experience with intact thoracic bones. Although to our knowledge, no other studies analyzed the detectability of bone lesions in sharp force trauma on CT data, our outcomes are comparable to those from Spies and colleagues [
11]. This recent experimental study analyzed blunt force fractures in piglets on different imaging modalities and compared the observations to the macerated remains of the piglets, assuming the latter as the standard. Although results obtained from experimental vs. cases from non-controlled environment studies may differ considerably [
58], we concur that the detection of fractures on virtual images can be challenging for forensic anthropologists. The authors [
11] found that the difficulties of trauma detection on tomographic data decreased with radiological training and experience. This highlights the need for specific training in radiological analysis to strengthen the skills of experts in this field [
11].
While the above reported results on the detectability of bone lesions for forensic anthropologists are sobering, we need to relativize the discrepancy between our observations and the forensic reports. The in-depth analysis of the twelve most detailed cases showed that the differences between the three investigations (autopsy, radiology and our observations) was not divergent, with each investigation leaving five to six bone lesions undetected. The discrepancy between the reports and our observations appears greater since we are using the autopsy and the radiology reports combined as a baseline. The error is less obvious if we compare our observations to the autopsy or the radiology report individually. This stresses the benefit of multimodal investigations in forensics. Nonetheless, as pointed out in previous work [
11,
12], our findings highlight the importance of radiological training for the ability to detect perimortem trauma on postmortem tomographic data.
4.2. Further Analyses
Analyzing the anatomical distribution of soft tissue injuries and bone lesions as well as other parameters relating to the manner of death can help distinguish between suicide and homicide [
8]. It is worthwhile to relate the location of soft tissue injuries to bone lesions, as a general pattern could emerge.
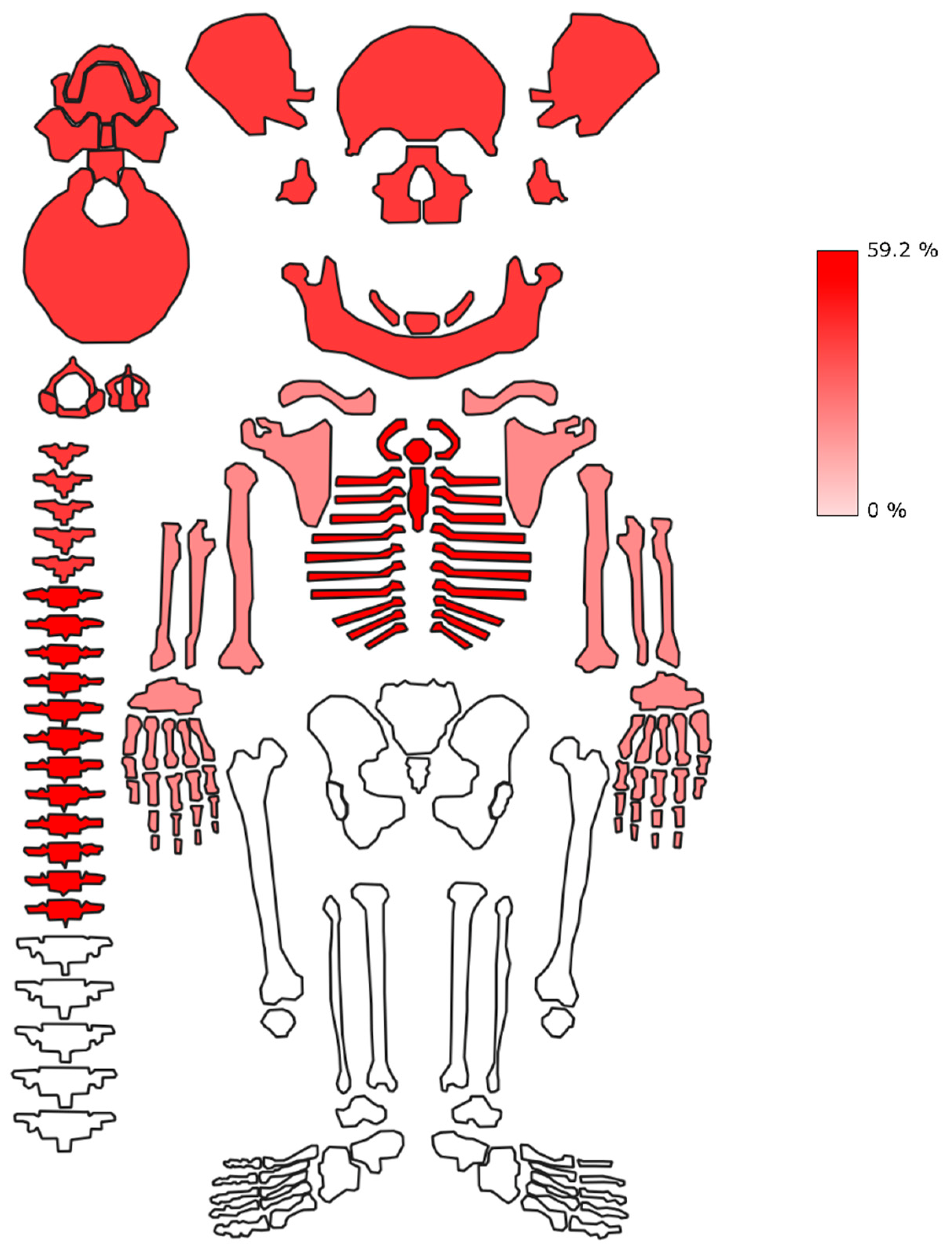
The observed frequency of soft tissue injuries versus bone lesions is interesting since it can be cautiously used as an approximation of the relative informativity of different anatomical regions in documenting traumatic events. Our data strongly confirm the intuitive relationship between the amount of soft tissue layers and presence of bone lesions. This is clearly demonstrated by the absence of bone lesions in the abdominal area and, by contrast, by the high frequency of bone lesions at the level of the head and neck region and the thorax. Although not surprising, this pattern is of a general interest, being relevant in the context of both forensic examinations and osteoarchaeological analyses. The total frequency of skeletally unobservable traumatic events (ca. 89%) is quite impressive and calls for caution when trying to base forensic and paleopathological reconstructions based solely on skeletal data. Clearly, one needs to consider the likely bias on these data played by the variable typology of used sharp objects, as well as in the dynamic of applied trauma (e.g., force, direction). Moreover, our sample is relatively small, features a biased sex ratio and contains individuals from a first world context. These are the unavoidable limitations of any forensic dataset, but should be carefully considered using the results of this study while discussing findings from different cultural, social and chronological settings.
The anatomical distribution of soft tissue injuries in our sample corresponds to the findings from a comprehensive review article [
5], with one difference in the most common location of injuries. The greatest number of soft tissue lesions in our suicide subsample (including and excluding case no. 15) was to the head and neck, which is slightly different from the thorax as the most frequently affected body part reported by De Giorgio and colleagues [
5]. In the homicide subsample, the thorax was the most frequent location for soft tissue injuries caused by sharp force, corresponding to the reports in De Giorgio and colleagues [
5]. The number of soft tissue injuries in our sample (excluding suicide case no. 15) was significantly higher in homicides as opposed to suicides.
A third of the suicide cases in our sample presented with a single soft tissue injury, the average number of injuries per suicide was 4.6 ± 4.3, excluding case no. 15. This corroborates the findings in literature, reporting a frequency of a third of the suicide cases with a single injury [
4] and an average of 2.4 injuries per case [
5]. The average of 4.6 in our sample would increase to 13.2 ± 32.3 if we added suicide case no. 15. We found only 19.2% of homicides with a single soft tissue injury, while literature reports about 40% [
4]. The average number of homicidal soft tissue injuries was 16.3 ± 17.6, while literature mentions an average of 3.8 injuries [
5]. Our homicide sample thus features a greater number of cases with multiple injuries resulting in the higher mean value compared to literature. While we need to consider the very large dataset of De Giorgio et al. [
5], the sample size of 65 cases in the study by Karger and colleagues [
4] is similar to ours. Hence, sample size alone does not explain the considerable differences in injury frequency; we may simply face a series of homicidal overkill cases in our sample.
Regarding the 71 bone lesions in our sample, we obtained statistical significance for the number of bone lesions per manner of death, corroborating the results of Banasr et al. [
6]. The thorax was the most commonly affected anatomical region for bone lesions in suicides as well as homicides in our study. This differs slightly from another study [
8], which describes the head and neck region as the most common site for homicidal sharp force trauma, followed by the thorax, but it corroborates the findings of Banasr and colleagues [
6]. The number of anatomical regions affected by bone lesions did not differ significantly between the manners of death in our sample. However, we consider the number of affected anatomical regions a relevant parameter for future forensic casework, even if statistical significance was not obtained [
59].
The suicidal bone lesions in our sample to the sternum (
n = 2) and the ribs (
n = 4) corroborate the findings reported in previous work [
60]. Although bone lesions in sharp force suicides are rarer than in homicides, they are not exceptional [
61]. Rare cases of aggressive sharp force suicides have been reported in literature and usually point to serious mental disorders [
62,
63,
64]. Such cases can complicate the distinction between suicide and homicide [
63], making the careful analysis of the circumstances of death and of the crime scene even more important [
64]. In this context, we need to mention suicide case no. 15 in our sample, presenting with 133 superficial stab wounds to the neck as well as the thorax. Although none of the injuries penetrated to the bone, it is an example of an unusual suicide.
In several analyses of sharp force suicide and homicide cases [
7,
65], bone and cartilage lesions were recorded in 50% and 56%, respectively, of all cases. These frequencies are similar to 58.5% in our sample. Brunel et al. [
7] as well as Teifel and Rothschild [
65] reported bone and/or cartilage lesions in 14.6% and 29.8%, respectively, of sharp force suicide cases, which stands in stark contrast to 40% in our study. This high frequency could indicate a greater degree of self-directed aggression in our sample. In the 70 homicide cases, the authors [
7] reported bone or cartilage lesions in 52 cases (74.3%), which is slightly higher than 69.2% in our sample. Other studies from Frankfurt (Germany) [
8] and from Paris (France) [
6] found 66.3% and 53%, respectively, of sharp force homicides with bone lesions.
The inclusion of cartilaginous lesions could account for the slightly higher percentage in the study by Brunel et al. [
7]. Due to the general absence of cartilage in skeletonized human remains, we did not consider cartilaginous lesions (for instance between ribs and sternum) by default. Unfortunately, the study [
7] does not discriminate between bone and cartilage lesions in terms of the anatomical location and quantity, thus limiting a direct comparison with our results. However, we can relate to their finding that bone lesions are a predictor for homicide [
7]. Even if the presence or absence of bone lesions was not significant for the manner of death in our study, the calculated odds ratio indicates a 3.269 times higher chance of presenting with bone lesions in a homicide. Moreover, our number of bone lesions per manner of death did yield a significant result. This could imply that a perpetrator intending to stab a person ignores the location of bones and thus more likely generates bone lesions than a person committing suicide, who might avoid skeletal elements [
7]. In our study, all suicidal bone lesions were caused with a category 4bα tool (blade length >15 cm, blade width >2 cm, smooth edge). The tools causing homicidal bone lesions, in contrast, included categories 2 and 4, with unspecified or serrated edges. No smooth-edged tools were described for the homicide tools. Although the choice of sharp force tools in our sample might have been coincidental, we point to the difference in pressure needed to penetrate skin with varying blades. Smooth knife blades slice through the skin at a pressure of at least 1900 g, while a serrated blade takes considerably less pressure (700 g) to penetrate skin, due to the higher energy density and the relative ease with which a serrated blade tears into skin [
66].
Apart from injury patterns and tool dimensions, we analyzed age-at-death as another parameter to discern possible differences between suicide and homicide. Mean age-at-death in sharp force suicides is often higher than in homicides [
5]. Indeed, we found a significantly higher age-at-death in suicides than in homicides. Sex, in contrast, was not a significant predictor of the manner of death. However, we found an odds ratio indicating a 0.3 higher time to be male in a suicide case, even if the result was not significant. This corresponds to the findings of a study from Japan, noting that 75.4% of sharp force suicide victims were males.
Potential limitations of our study relate to the relatively small size of the analyzed sample and the confined geographical origin of the specimens. The completeness of our sample, however, allows some cautious statements, even though we do not wish to venture into other forensic fields. Forensic cases may present with a combination of different trauma, which, however, was not the focus of the present study.