Retinol-Binding Protein-4—A Predictor of Insulin Resistance and the Severity of Coronary Artery Disease in Type 2 Diabetes Patients with Coronary Artery Disease
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Sample Size Calculation
2.3. Aim and Hypotheses
2.4. Demographic and Clinical Information, and Anthropometric Measurements
2.5. Biochemical Parameters
2.6. RBP-4 Assay Protocol
2.7. Statistical Analysis
2.8. Operational Definitions
3. Results
3.1. Demographic and Clinical Factors of Study Population
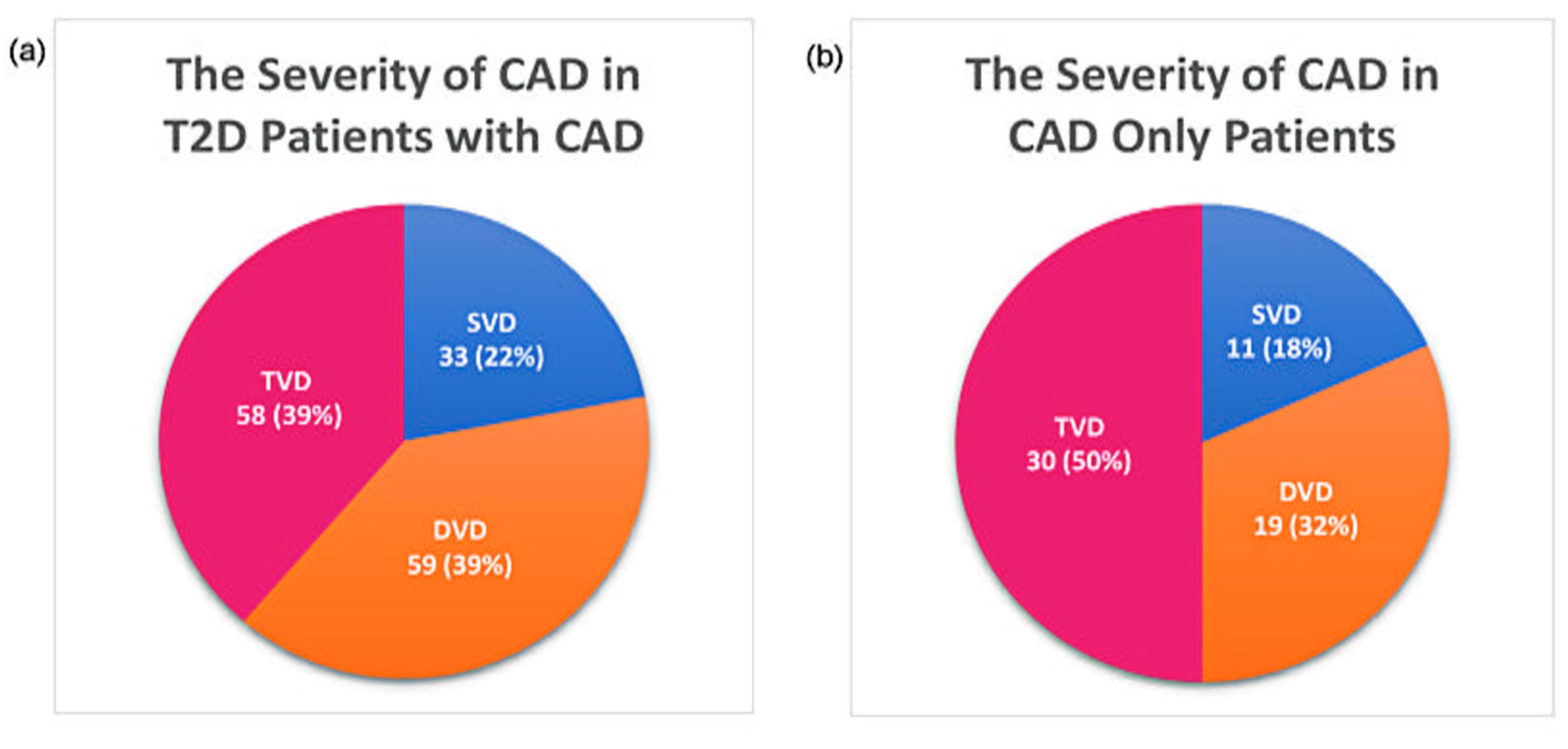
3.2. The Severity of CAD
3.3. Association of Clinical Factors with RBP-4
3.4. Association of Clinical Factors with IR
3.5. Association of Clinical Factors with the Severity of CAD
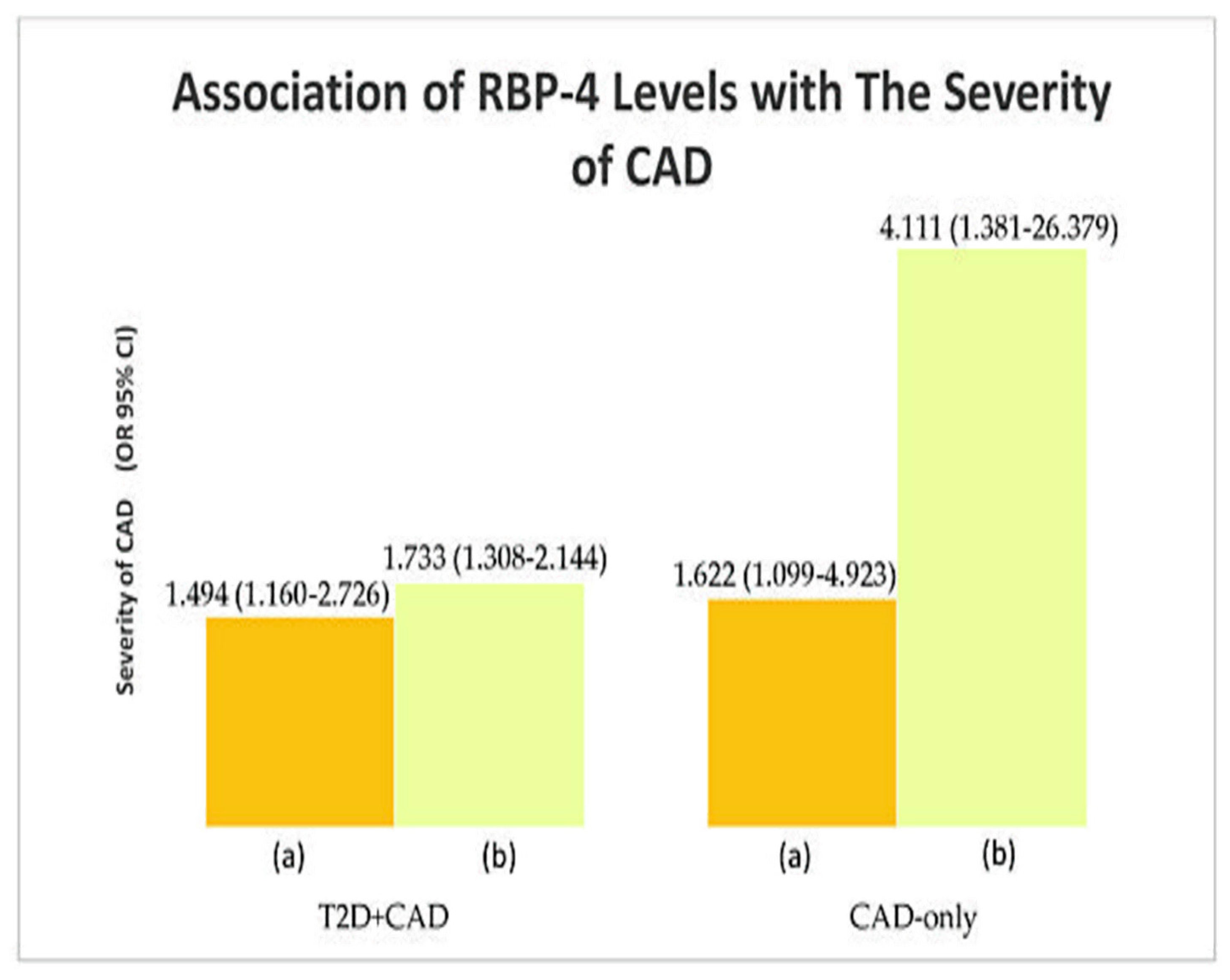
3.6. Association of RBP-4 Levels with IR and the Severity of CAD
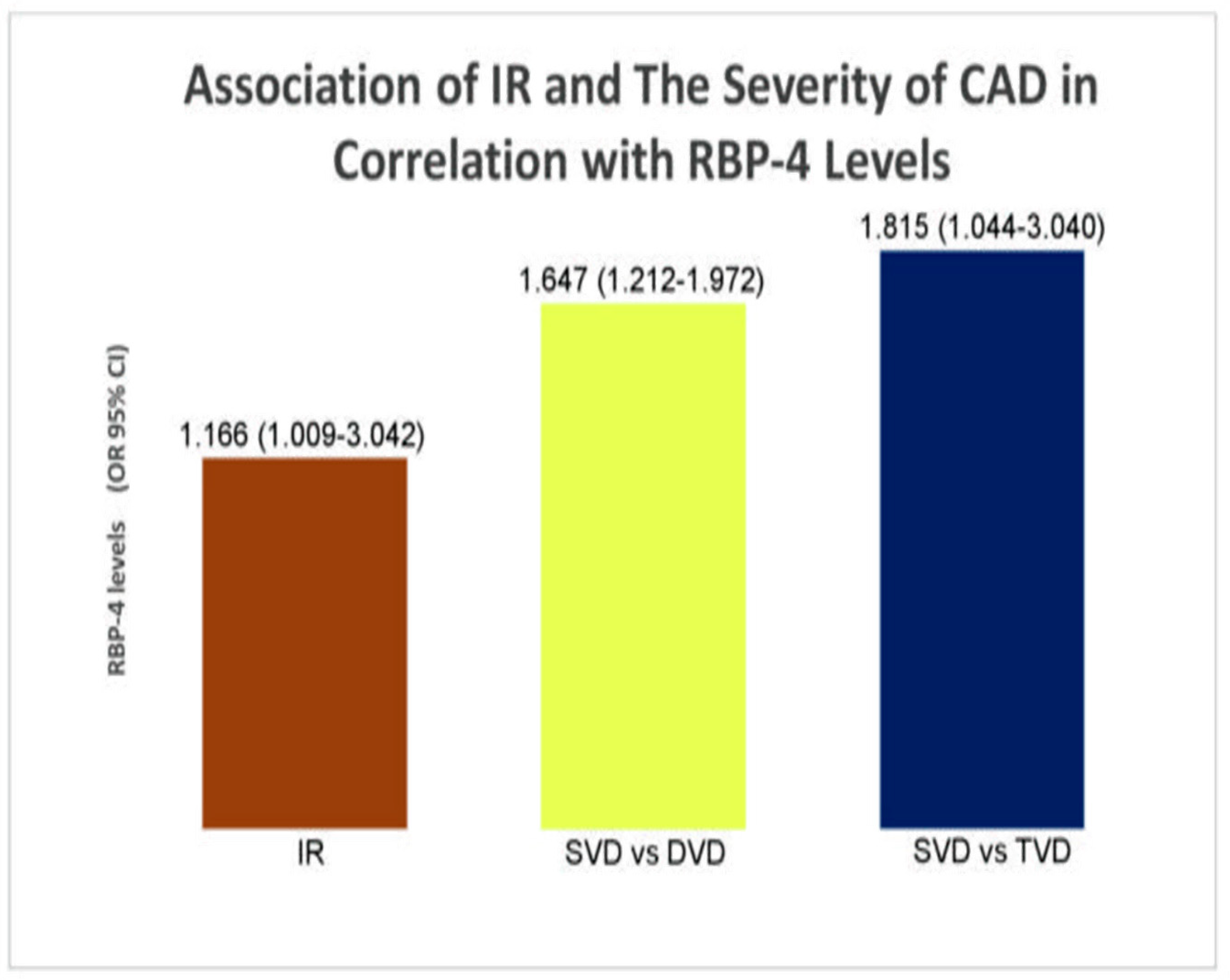
3.7. Association of IR and the Severity of CAD in Correlation with RBP-4 Levels and Clinical Factors (Secondary Analysis)
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Association of RBP-4 with Clinical Factors | ||
|---|---|---|
| Group | Parameter | p-Value |
| T2D + CAD | A1C | 0.034 |
| hs-CRP | <0.001 | |
| LDL-c | <0.001 | |
| HDL-c | 0.001 | |
| TG | 0.028 | |
| Bi + I | <0.001 | |
| Bi + SGLT2 + I | 0.001 | |
| Bi + SU | <0.001 | |
| Bi | <0.001 | |
| SU | <0.001 | |
| Nitrates | 0.008 | |
| Diuretics | 0.002 | |
| Cardiac glycosides | <0.001 | |
| T2D-only | FPI | 0.032 |
| TC | 0.031 | |
| CAD-only | – | – |
| Association of clinical factors with IR and the severity of CAD | ||
| Group | Factor | p-value |
| T2D + CAD | ||
| IR | FPG | 0.011 |
| FPI | <0.001 | |
| hs-CRP | 0.025 | |
| Bi + DPP4i + I | 0.008 | |
| Antiplatelet agents | 0.003 | |
| ACEI | 0.026 | |
| Severity of CAD | FPG | a 0.007 b 0.012 |
| FPI | a 0.045 | |
| DPP4i | a <0.001 b <0.001 | |
| SU + DPP4i | a 0.011 b 0.016 | |
| Bi + DPP4i + I | a <0.001 b 0.003 | |
| ACEI | a 0.032 b 0.029 | |
| AB | a 0.008 b 0.020 | |
| Fibrates | b <0.001 | |
| Statins | b 0.018 | |
| Hematinic agents | a 0.011 b 0.016 | |
| T2D-only | ||
| IR | FPI | <0.001 |
| Severity of CAD | – | – |
| CAD-only | ||
| IR | FPG | 0.048 |
| FPI | <0.001 | |
| Severity of CAD | FPG | a <0.001 |
| FPI | b <0.001 | |
| A1C | b <0.001 | |
| LDL-c | b 0.004 | |
| HDL-c | a <0.001 | |
| TG | b 0.001 | |
| Association of RBP-4 with IR and the severity of CAD | ||
| Group | Factor | p-value |
| T2D + CAD | ||
| IR | RBP-4 | 0.002 |
| Severity of CAD | a 0.017 b 0.022 | |
| T2D-only | ||
| IR | RBP-4 | 0.042 |
| Severity of CAD | – | |
| CAD-only | ||
| IR | RBP-4 | 0.031 |
| Severity of CAD | a 0.002 b 0.001 | |
References
- Zhang, Y.; Pan, X.F.; Chen, J.; Xia, L.; Cao, A.; Zhang, Y.; Wang, J.; Li, H.; Yang, K.; Guo, K.; et al. Combined lifestyle factors and risk of incident type 2 diabetes and prognosis among individuals with type 2 diabetes: A systematic review and meta-analysis of prospective cohort studies. Diabetologia 2019, 63, 21–33. [Google Scholar] [CrossRef]
- Taylor, R. Insulin Resistance and Type 2 Diabetes. Diabetes 2012, 61, 778–779. [Google Scholar] [CrossRef]
- Ormazabal, V.; Nair, S.; Elfeky, O.; Aguayo, C.; Salomon, C.; Zuñiga, F.A. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc. Diabetol. 2018, 17, 122. [Google Scholar] [CrossRef] [PubMed]
- Rafieian-Kopaei, M.; Setorki, M.; Doudi, M.; Baradaran, A.; Nasri, H. Atherosclerosis: Process, indicators, risk factors and new hopes. Int. J. Prev. Med. 2014, 5, 927–946. [Google Scholar]
- Perumalsamy, S.; Wan Ahmad, W.A.; Zaman Huri, H. Single Nucleotide Polymorphism rs17173608 in the Chemerin Encoding Gene: Is It a Predictor of Insulin Resistance and Severity of Coronary Artery Disease in Non-Obese Type 2 Diabetes? Healthcare 2021, 9, 623. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Guo, X.; Gao, Y.; Guo, Q.; Zhang, J.; Fang, B.; Yan, B. Impact of right coronary dominance on triple-vessel coronary artery disease: A cross-sectional study. Medicine 2018, 97, e11685. [Google Scholar] [CrossRef] [PubMed]
- Naito, R.; Kasai, T. Coronary artery disease in type 2 diabetes mellitus: Recent treatment strategies and future perspectives. World J. Cardiol. 2015, 7, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Einarson, T.R.; Acs, A.; Ludwig, C.; Panton, U.H. Prevalence of cardiovascular disease in type 2 diabetes: A systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc. Diabetol. 2018, 17, 83. [Google Scholar] [CrossRef] [PubMed]
- Tsalamandris, S.; Antonopoulos, A.S.; Oikonomou, E.; Papamikroulis, G.A.; Vogiatzi, G.; Papaioannou, S.; Deftereos, S.; Tousoulis, D. The Role of Inflammation in Diabetes: Current Concepts and Future Perspectives. Eur. Cardiol. 2019, 14, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Noy, N.; Li, L.; Abola, M.V.; Berger, N.A. Is retinol binding protein 4 a link between adiposity and cancer? Horm. Mol. Biol. Clin. Investig. 2015, 23, 39–46. [Google Scholar] [CrossRef]
- Chang, X.; Yan, H.; Bian, H.; Xia, M.; Zhang, L.; Gao, J.; Gao, X. Serum retinol binding protein 4 is associated with visceral fat in human with nonalcoholic fatty liver disease without known diabetes: A cross-sectional study. Lipids Health Dis. 2015, 14, 28. [Google Scholar] [CrossRef][Green Version]
- Liu, Y.; Albrecht, E.; Dannenberger, D.; Hammon, H.M.; Kuehn, C.; Sauerwein, H.; Yang, R.; Zhao, Z.; Maak, S. Retinol binding protein 4 abundance in plasma and tissues is related to body fat deposition in cattle. Sci. Rep. 2019, 9, 8056. [Google Scholar] [CrossRef]
- Zabetian-Targhi, F.; Mahmoudi, M.J.; Rezaei, N.; Mahmoudi, M. Retinol binding protein 4 in relation to diet, inflammation, immunity, and cardiovascular diseases. Adv. Nutr. 2015, 6, 748–762. [Google Scholar] [CrossRef] [PubMed]
- Bobbert, T.; Raila, J.; Scharz, F.; Mai, K.; Henze, A.; Pfeiffer, A.F.; Schweigert, F.J.; Spranger, J. Relation between retinol, retinol-binding protein 4, transthyretin and carotid intima media thickness. Atherosclerosis 2010, 213, 549–551. [Google Scholar] [CrossRef] [PubMed]
- Takebayashi, K.; Sohma, R.; Aso, Y.; Inukai, T. Effects of retinol binding protein-4 on vascular endothelial cells. Biochem. Biophys. Res. Commun. 2011, 408, 58–64. [Google Scholar] [CrossRef]
- Liu, C.; Zhou, X.R.; Ye, M.Y.; Xu, X.Q.; Zhang, Y.W.; Liu, H.; Huang, X.Z. RBP4 Is Associated With Insulin Resistance in Hyperuricemia-Induced Rats and Patients With Hyperuricemia. Front. Endocrinol. 2021, 12, 653819. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Chen, H.; Liu, Y.; Zhou, W.; Sun, R.; Xia, M. Retinol binding protein 4 induces mitochondrial dysfunction and vascular oxidative damage. Atherosclerosis 2015, 240, 335–344. [Google Scholar] [CrossRef]
- Bengal, E.; Aviram, S.; Hayek, T. p38 MAPK in Glucose metabolism of skeletal muscle: Beneficial or harmful? Int. J. Mol. Sci. 2020, 21, 6480. [Google Scholar] [CrossRef]
- Inoue, E.; Yamashita, A.; Inoue, H.; Sekiguchi, M.; Shiratori, A.; Yamamoto, Y.; Tadokoro, T.; Ishimi, Y.; Yamauchi, J. Identification of glucose transporter 4 knockdown-dependent transcriptional activation element on the retinol binding protein 4 gene promoter and requirement of the 20 S proteasome subunit for transcriptional activity. J. Biol. Chem. 2010, 285, 25545–25553. [Google Scholar] [CrossRef]
- Chadt, A.; Al-Hasani, H. Glucose transporters in adipose tissue, liver, and skeletal muscle in metabolic health and disease. Pflügers Arch. -Eur. J. Physiol. 2020, 472, 1273–1298. [Google Scholar] [CrossRef]
- Naji, M.T.; Sami, O.M.; Shams, H.A.; Abdul-Hadi, M.H.; Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Al-Harchan, N.A.A. The associations between retinol binding protein-4 and cardiometabolic profile: Intertwined-intricate relationship. Biomed. Biotechnol. Res. J. (BBRJ) 2020, 4, 95. [Google Scholar]
- Fan, J.; Yin, S.; Lin, D.; Liu, Y.; Chen, N.; Bai, X.; Ke, Q.; Shen, J.; You, L.; Lin, X.; et al. Association of serum retinol-binding protein 4 levels and the risk of incident type 2 diabetes in subjects with prediabetes. Diabetes Care 2019, 42, 1574–1581. [Google Scholar] [CrossRef]
- Sun, H.X.; Ji, H.H.; Chen, X.L.; Wang, L.; Wang, Y.; Shen, X.Y.; Lu, X.; Gao, W.; Wang, L.S. Serum retinol-binding protein 4 is associated with the presence and severity of coronary artery disease in patients with subclinical hypothyroidism. Aging 2019, 11, 4510–4520. [Google Scholar] [CrossRef]
- Baingana, R.K.; Matovu, D.K.; Garrett, D. Application of Retinol-Binding Protein Enzyme Immunoassay to Dried Blood Spots to Assess Vitamin A Deficiency in a Population-Based Survey: The Uganda Demographic and Health Survey 2006. Food Nutr. Bull. 2008, 29, 297–305. [Google Scholar] [CrossRef]
- Su, Y.; Huang, Y.; Jiang, Y.; Zhu, M. The Association between Serum retinol-binding protein 4 levels and cardiovascular events in patients with chronic kidney disease. Lab. Med. 2020, 51, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Wessel, H.; Saeed, A.; Heegsma, J.; Connelly, M.A.; Faber, K.N.; Dullaart, R.P.F. Plasma levels of retinol binding protein 4 relate to large VLDL and small LDL particles in subjects with and without type 2 diabetes. J. Clin. Med. 2019, 8, 1792. [Google Scholar] [CrossRef] [PubMed]
- Ruijgrok, C.; Dekker, J.M.; Beulens, J.W.; Brouwer, I.A.; Coupé, V.M.H.; Heymans, M.W.; Sijtsma, F.P.C.; Mela, D.J.; Zock, P.L.; Olthof, M.R.; et al. Size and shape of the associations of glucose, HbA1c, insulin and HOMA-IR with incident type 2 diabetes: The Hoorn Study. Diabetologia 2017, 61, 93–100. [Google Scholar] [CrossRef]
- Abdul-Ghani, M.A.; Matsuda, M.; Balas, B.; DeFronzo, R.A. Muscle and Liver Insulin Resistance Indexes Derived From the Oral Glucose Tolerance Test. Diabetes Care 2006, 30, 89–94. [Google Scholar] [CrossRef]
- Uemura, H.; Katsuura-Kamano, S.; Yamaguchi, M.; Bahari, T.; Ishizu, M.; Fujioka, M.; Arisawa, K. Relationships of serum high-sensitivity C-reactive protein and body size with insulin resistance in a Japanese cohort. PLoS ONE 2017, 12, e0178672. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Khan, A.H.; Adnan, A.S.; Sulaiman, S.A.S.; Mushtaq, S.; Ahmad, N.; Khan, I. Hypertension control among euvolemic hypertensive hemodialysis patients in Malaysia: A prospective follow-up study. J. Pharm. Policy Pract. 2019, 12, 10. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, M.; Kamath, P.; Bhat, N.; Pai, N.; Bhat, R.; Shah, T.; Manjrekar, P.; Mahabala, C. Basal hyperinsulinemia beyond a threshold predicts major adverse cardiac events at 1 year after coronary angiogram in type 2 diabetes mellitus: A retrospective cohort study. Diabetol. Metab. Syndr. 2017, 9, 38. [Google Scholar] [CrossRef]
- Dai, W.; Zhang, Z.; Zhao, S. Baseline levels of serum high sensitivity C reactive protein and lipids in predicting the residual risk of cardiovascular events in Chinese population with stable coronary artery disease: A prospective cohort study. Lipids Health Dis. 2018, 17, 273. [Google Scholar] [CrossRef] [PubMed]
- Toth, P.P.; Granowitz, C.; Hull, M.; Liassou, D.; Anderson, A.; Philip, S. High triglycerides are associated with increased cardiovascular events, medical costs, and resource use: A real-world administrative claims analysis of statin-treated patients with high residual cardiovascular risk. J. Am. Heart Assoc. 2018, 7, e008740. [Google Scholar] [CrossRef] [PubMed]
- Kim-Mitsuyama, S.; Soejima, H.; Yasuda, O.; Node, K.; Jinnouchi, H.; Yamamoto, E.; Sekigami, T.; Ogawa, H.; Matsui, K. Reduction in hsCRP levels is associated with decreased incidence of cardiovascular events in Japanese hypertensive women but not in men. Sci. Rep. 2020, 10, 17040. [Google Scholar] [CrossRef] [PubMed]
- Razban, M.M.; Eslami, M.; Bagherzadeh, A. The relationship between serum levels of Hs-CRP and coronary lesion severity. Med. Pharm. Rep. 2016, 89, 352–364. [Google Scholar] [CrossRef] [PubMed]
- Ou, H.T.; Chang, K.C.; Li, C.Y.; Wu, J.S. Comparative cardiovascular risks of dipeptidyl peptidase 4 inhibitors with other second- and third-line antidiabetic drugs in patients with type 2 diabetes. Br. J. Clin. Pharmacol. 2017, 83, 1556–1570. [Google Scholar] [CrossRef]
- Arnold, S.V.; Bhatt, D.L.; Barsness, G.W.; Beatty, A.L.; Deedwania, P.C.; Inzucchi, S.E.; Kosiborod, M.; Leiter, L.A.; Lipska, K.J.; Newman, J.D.; et al. Clinical management of stable coronary artery disease in patients with type 2 diabetes mellitus: A scientific statement from the American Heart Association. Circulation 2020, 141, e779–e806. [Google Scholar] [CrossRef]
- Elam, M.B.; Ginsberg, H.N.; Lovato, L.C.; Corson, M.; Largay, J.; Leiter, L.A.; Lopez, C.; O’Connor, P.J.; Sweeney, M.E.; Weiss, D.; et al. Association of fenofibrate therapy with long-term cardiovascular risk in statin-treated patients with type 2 diabetes. JAMA Cardiol. 2017, 2, 370. [Google Scholar] [CrossRef] [PubMed]
- Vafaeimanesh, J.; Parham, M.; Norouzi, S.; Hamednasimi, P.; Bagherzadeh, M. Insulin resistance and coronary artery disease in non-diabetic patients: Is there any correlation? Casp. J. Intern. Med. 2018, 9, 121–126. [Google Scholar] [CrossRef]
- Majerczyk, M.; Kocełak, P.; Choręza, P.; Arabzada, H.; Owczarek, A.J.; Bożentowicz-Wikarek, M.; Brzozowska, A.; Szybalska, A.; Puzianowska-Kuźnicka, M.; Grodzicki, T.; et al. Components of metabolic syndrome in relation to plasma levels of retinol binding protein 4 (RBP4) in a cohort of people aged 65 years and older. J. Endocrinol. Investig. 2018, 41, 1211–1219. [Google Scholar] [CrossRef] [PubMed]
- McInnes, K.J.; Smith, L.B.; Hunger, N.I.; Saunders, P.T.; Andrew, R.; Walker, B.R. Deletion of the androgen receptor in adipose tissue in male mice elevates retinol binding protein 4 and reveals independent effects on visceral fat mass and on glucose homeostasis. Diabetes 2012, 61, 1072–1081. [Google Scholar] [CrossRef]
- Jin, Y.; Cao, J.N.; Wang, C.X.; Feng, Q.T.; Ye, X.H.; Xu, X.; Yang, C.J. High serum YKL-40 level positively correlates with coronary artery disease. Biomark. Med. 2017, 11, 133–139. [Google Scholar] [CrossRef]
- Li, X.; Zhang, K.; Yan, J.; Wang, L.; Wang, Y.; Shen, X.; Sun, H.; Liu, L.; Zhao, C.; He, H.; et al. Serum retinol-binding protein 4 as a predictor of cardiovascular events in elderly patients with chronic heart failure. ESC Heart Fail. 2020, 7, 542–550. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, D.; Chen, H.; Xia, M. Circulating retinol binding protein 4 is associated with coronary lesion severity of patients with coronary artery disease. Atherosclerosis 2015, 238, 45–51. [Google Scholar] [CrossRef] [PubMed]

| Parameter | OR (95% CI) | ||
|---|---|---|---|
| T2D + CAD (n = 150) | T2D-Only (n = 90) | CAD-Only (n = 60) | |
| FPG (mmol/L) | 1.088 (0.983–1.204) | 0.937 (0.825–1.065) | 0.943 (0.328–2.707) |
| FPI (pmol/L) | 0.995 (0.987–1.002) | 1.220 (1.041–1.430) | 0.936 (0.846–1.036) |
| A1C (%) | 0.797 (0.654–0.970) | 1.048 (0.856–1.283) | 0.869 (0.268–2.820) |
| hs-CRP (mg/L) | 1.317 (1.052–1.632) | 1.728 (0.776–3.845) | 1.214 (0.248–5.939) |
| TC (mmol/L) | 1.017 (0.783–1.230) | 1.345 (1.033–1.589) | 1.476 (0.715–3.047) |
| LDL-c (mmol/L) | 2.918 (1.428–3.385) | 0.602 (0.339–1.069) | 1.261 (0.533–2.986) |
| HDL-c (mmol/L) | 0.490 (0.300–0.800) | 1.181 (0.265–5.264) | 0.965 (0.750–2.455) |
| TG (mmol/L) | 1.402 (1.201–1.702) | 0.740 (0.437–1.255) | 0.983 (0.435–2.218) |
| Hypertension | 0.244 (0.040–1.251) | 1.102 (0.175–6.940) | 3.062 (0.248–7.879) |
| Dyslipidemia | 2.336 (0.708–7.708) | 2.800 (0.548–14.311) | 0.557 (0.096–3.244) |
| Peripheral neuropathy | 0.635 (0.325–1.240) | 1.021 (0.440–2.368) | 5.667 (0.239–19.655) |
| Chronic kidney disease (CKD) | 1.615 (0.691–3.778) | 1.483 (0.526–4.183) | 0.160 (0.009–2.823) |
| Retinopathy | 0.547 (0.255–1.173) | 0.839 (0.338–2.083) | 5.667 (0.778–10.661) |
| Anemia | 0.783 (0.048–12.760) | 0.731 (0.050–2.065) | 4.076 (0.421–40.755) |
| Gastritis | 0.786 (0.333–1.546) | 4.371 (0.437–43.763) | 0.327 (0.026–4.034) |
| Biguanides | 6.400 (2.024–20.237) | 0.613 (0.220–1.705) | – |
| Sulphonylureas | 17.714 (5.812–53.993) | 1.482 (0.590–3.722) | – |
| DPP4i | 8.400 (0.056–34.855) | 1.005 (0.399–2.529) | – |
| AGI | 0.786 (0.045–1.433) | 0.731 (0.088–4.033) | – |
| Meglitinides | 0.786 (0.088–2.113) | 1.031 (0.326–3.264) | – |
| Biguanide + SU | 10.000 (3.240–30.866) | 1.360 (0.539–3.432) | – |
| SU + DPP4i | 9.056 (0.076–65.877) | 0.907 (0.144–5.715) | – |
| Biguanide + insulin | 1.206 (1.093–1.458) | – | – |
| Biguanide + SU + insulin | 1.290 (0.310–5.365) | – | – |
| Biguanide + DPP4i + insulin | 0.021 (0.006–0.043) | – | – |
| Biguanide + SGLT2 + insulin | 1.161 (1.053–1.493) | – | – |
| SGLT2 + insulin | 0.308 (0.034–2.821) | – | – |
| Antiplatelet agents | 4.114 (0.469–36.102) | – | 0.008 (0.002–0.015) |
| ACEI | 0.847 (0.443–1.619) | 0.724 (0.268–1.951) | 0.429 (0.090–2.043) |
| ARB II | 0.530 (0.237–1.187) | 1.052 (0.429–2.579) | 2.909 (0.666–12.708) |
| Calcium channel blockers | 1.041 (0.496–2.182) | 1.235 (0.534–2.859) | 1.818 (0.390–8.466) |
| Beta blockers | 1.106 (0.578–2.114) | 1.029 (0.445–2.377) | 0.318 (0.064–1.574) |
| Alpha blockers | 9.664 (0.099–45.123) | 0.731 0.045–3.912) | – |
| Nitrates | 2.657 (1.331–5.303) | – | 2.629 (0.425–16.263) |
| Fibrates | 7.690 (0.065–33.878) | – | – |
| Statins | 0.040 (0.012–0.077) | 7.760 (0.013–27.112) | – |
| Diuretics | 1.297 (1.141–1.624) | 1.283 (0.522–3.153) | 2.629 (0.425–16.263) |
| Antianginal drugs | 1.983 (0.935–4.205) | – | 0.500 (0.046–5.423) |
| Hematinic agents | 3.925 (0.402–38.903) | 0.676 (0.059–7.735) | 0.380 (0.061–2.354) |
| Cardiac glycosides | 18.444 (2.331–145.961) | – | – |
| Parameter | HOMA-IR, OR (95% CI) | ||
|---|---|---|---|
| T2D + CAD (n = 150) | T2D-Only (n = 90) | CAD-Only (n = 60) | |
| FPG (mmol/L) | 1.160 (1.031–1.306) | 1.010 (0.894–1.142) | 2.570 (1.097–5.773) |
| FPI (pmol/L) | 1.233 (1.146–1.327) | 1.376 (1.197–1.581) | 1.368 (1.167–1.603) |
| A1C (%) | 1.102 (0.913–1.331) | 1.098 (0.896–1.344) | 2.122 (0.759–5.932) |
| hs-CRP (mg/L) | 2.378 (1.155–4.899) | 1.394 (0.636–3.057) | 3.502 (0.909–13.493) |
| TC (mmol/L) | 0.813 (0.622–1.063) | 1.159 (0.809–1.660) | 0.775 (0.443–1.356) |
| LDL-c (mmol/L) | 0.942 (0.650–1.366) | 1.119 (0.675–1.855) | 0.806 (0.405–1.606) |
| HDL-c (mmol/L) | 0.738 (0.500–1.089) | 0.702 (0.159–3.100) | 0.524 (0.053–5.140) |
| TG (mmol/L) | 0.973 (0.673–1.407) | 0.799 (0.482–1.324) | 0.627 (0.292–1.342) |
| Hypertension | 0.614 (0.147–2.556) | 1.687 (0.268–10.617) | 6.304 (0.044–19.030) |
| Dyslipidemia | 0.515 (0.176–1.505) | 1.951 (0.456–8.341) | 0.684 (0.149–3.134) |
| Peripheral neuropathy | 0.633 (0.319–1.258) | 0.980 (0.426–2.253) | – |
| Chronic kidney disease (CKD) | 0.990 (0.415–2.359) | 2.645 (0.893–7.831) | 2.867 (0.169–48.744) |
| Retinopathy | 1.319 (0.629–2.768) | 0.879 (0.360–2.147) | – |
| Anemia | 1.596 (0.098–26.032) | – | – |
| Gastritis | – | 1.098 (0.148–8.152) | – |
| Biguanides | 0.750 (0.365–1.540) | 0.689 (0.254–1.870) | – |
| Sulphonylureas | 1.076 (0.496–2.332) | 0.714 (0.292–1.747) | – |
| DPP4i | 0.006 (0.002–0.010) | 1.133 (0.455–2.822) | – |
| AGI | 1.586 (0.066–2.887) | 0.915 (0.052–4.835) | – |
| Biguanide + SU | 1.201 (0.509–2.835) | 0.413 (0.163–1.046) | – |
| SU + DPP4i | 0.012 (0.006–0.030) | 4.718 (0.506–43.984) | – |
| Biguanide + insulin | 0.681 (0.333–1.394) | – | – |
| Biguanide + SU + insulin | 1.630 (0.391–6.787) | – | – |
| Biguanide + DPP4i + insulin | 1.860 (1.043–2.027) | – | – |
| Biguanide + SGLT2 + insulin | 1.033 (0.445–2.395) | – | – |
| SGLT2 + insulin | 2.455 (0.398–15.155) | – | – |
| Antiplatelet agents | 1.454 (1.032–1.895) | – | 6.011 (0.042–36.772) |
| ACEI | 1.444 (1.227–1.868) | 2.353 (0.872–6.351) | 3.800 (1.006–14.351) |
| ARB II | 1.829 (0.845–3.961) | 0.524 (0.214–1.285) | 0.429 (0.123–1.495) |
| Calcium channel blockers | 0.662 (0.303–1.446) | 0.644 (0.280–1.481) | 1.768 (0.488–6.397) |
| Beta blockers | 0.824 (0.426–1.594) | 1.318 (0.575–3.024) | 2.111 (0.509–8.751) |
| Alpha blockers | 2.702 (0.038–16.806) | – | 0.364 (0.033–1.452) |
| Nitrates | 0.768 (0.382–1.544) | – | 0.433 (0.086–2.196) |
| Fibrates | 2.607 (0.028–6.442) | – | – |
| Statins | 0.009 (0.004–0.014) | 15.436 (0.078–66.022) | – |
| Diuretics | 1.699 (0.853–3.384) | 0.750 (0.305–1.843) | 0.433 (0.086–2.195) |
| Antianginal drugs | 0.594 (0.267–1.320) | – | 9.923 (0.950–33.701) |
| Hematinic agents | 1.607 (0.220–11.735) | 0.536 (0.047–6.128) | 2.308 (0.456–11.690) |
| Cardiac glycosides | 0.263 (0.058–1.232) | – | – |
| Parameter | Severity of CAD, OR (95% CI) | |
|---|---|---|
| T2D + CAD (n = 150) | CAD-Only (n = 60) | |
| FPG (mmol/L) | a 1.815 (1.710–1.935) b 1.875 (1.771–1.992) | a1.651 (1.201–2.110) b 0.458 (0.151–1.388) |
| FPI (pmol/L) | a 1.011 (0.997–1.026) b 1.015 (1.001–1.030) | a 0.984 (0.885–1.094) b 1.553 (1.054–2.105) |
| A1C (%) | a 0.898 (0.712–1.133) b 0.939 (0.747–1.179) | a 0.626 (0.161–2.444) b 1.318 (1.087–1.858) |
| hs-CRP (mg/L) | a 0.652 (0.369–1.154) b 0.801 (0.518–1.237) | a 3.229 (0.548–19.036) b 2.726 (0.526–14.473) |
| TC (mmol/L) | a 0.880 (0.632–1.227) b 0.772 (0.546–1.092) | a 0.685 (0.314–1.492) b 1.424 (0.712–2.848) |
| LDL-c (mmol/L) | a 1.169 (0.722–1.895) b 0.901 (0.543–1.494) | a 0.510 (0.197–1.321) b 1.722 (1.296–2.538) |
| HDL-c (mmol/L) | a 1.007 (0.602–1.686) b 1.059 (0.635–1.764) | a3.754 (1.185–76.172) b 2.218 (0.130–3.789) |
| TG (mmol/L) | a 1.090 (0.689–1.724) b 0.726 (0.437–1.207) | a 0.736 (0.285–1.899) b 1.299 (1.007–1.523) |
| Hypertension | a 2.963 (0.331–26.504) b 1.143 (0.100–13.105) | a 4.144 (0.349–20.714) b 5.329 (0.957–29.532) |
| Dyslipidemia | a 0.926 (0.207–4.147) b 1.373 (0.330–5.711) | a 1.875 (0.171–20.609) b 2.000 (0.207–19.336) |
| Peripheral neuropathy | a 0.783 (0.320–1.912) b 0.660 (0.271–1.609) | – – |
| Chronic kidney disease (CKD) | a 0.875 (0.272–2.818) b 0.763 (0.240–2.424 | a 0.055 (0.015–0.368) b 0.976 (0.843–1.280) |
| Retinopathy | a 0.791 (0.298–2.097) b 1.006 (0.371–2.728) | – – |
| Anemia | a 1.006 (0.954–1.087) b 1.014 (0.076–1.632) | a 1.065 (0.045–2.060) b 0.063 (0.036–0.123) |
| Gastritis | – – | a 1.800 (0.101–31.988) b 2.900 (0.166–50.815) |
| Biguanides | a 1.203 (0.491–2.945) b 1.500 (0.602–3.740) | – – |
| Sulphonylureas | a 1.008 (0.387–2.625) b 1.800 (0.646–5.018) | – – |
| DPP4i | a 1.269 (1.008–1.865) b 2.149 (1.320–3.326) | – – |
| Biguanide + SU | a 1.319 (0.450–3.872) b 1.466 (0.490–4.387) | – – |
| SU + DPP4i | a 1.654 (1.054–2.022) b 1.754 (1.132–2.503) | – – |
| Biguanide + insulin | a 0.525 (0.194–1.418) b 0.441 (0.164–1.184) | – – |
| Biguanide + SU + insulin | a 2.850 (0.451–17.999) b 1.833 (0.348–9.652) | – – |
| Biguanide + DPP4i + insulin | a 1.545 (1.008–1.967) b 1.877 (1.210–3.116) | – – |
| Biguanide + SGLT2 + insulin | a 1.778 (0.612–5.165) b 1.367 (0.487–3.837) | – – |
| SGLT2 + insulin | a 0.891 (0.078–10.210) b 0.875 (0.076–10.033) | – – |
| Antiplatelet agents | a 1.123 (0.098–12.872) b 1.745 (0.174–17.492) | a 4.647 (0.077–8.945) b 0.945 (0.768–1.490) |
| ACEI | a 1.487 (1.085–3.532) b 1.166 (1.032–2.890) | a 0.833 (0.126–5.504) b 0.889 (0.151–5.241) |
| ARB II | a 1.253 (0.453–3.468) b 1.006 (0.371–2.728) | a 1.607 (0.255–10.132) b 1.636 (0.289–9.255) |
| Calcium channel blockers | a 0.567 (0.209–1.537) b 1.032 (0.362–2.946) | a 1.200 (0.182–7.926) b 1.636 (0.289–9.255) |
| Beta blockers | a 0.703 (0.299–1.654) b 0.548 (0.231–1.299) | a 0.375 (0.036–3.865) b 0.500 (0.052–4.834) |
| Alpha blockers | a 1.795 (1.076–4.644) b 1.900 (1.056–3.012) | – – |
| Nitrates | a 1.153 (0.485–2.742) b 2.112 (0.853–5.230) | a 1.875 (0.171–20.609) b 1.111 (0.103–11.965) |
| Fibrates | a 0.029 (0.006–0.144) b 1.056 (1.008–1.768) | – – |
| Statins | a 25.265 (0.122–46.004) b 1.087 (1.004–1.255) | – – |
| Diuretics | a 0.975 (0.395–2.404) b 0.950 (0.385–2.346) | a 16.240 (3.209–57.778) b 13.325 (1.620–25.921) |
| Antianginal drugs | a 0.729 (0.276–1.923) b 1.367 (0.487–3.837) | – – |
| Hematinic agents | a 1.540 (1.021–2.006) b 1.444 (1.058–2.244) | a 0.533 (0.049–5.862) b 0.900 (0.084–9.692) |
| Cardiac glycosides | a 1.025 (0.277–3.797) b 3.862 (0.667–22.350) | – – |
| Parameter | OR (95% CI) | ||
|---|---|---|---|
| T2D + CAD (n = 150) | T2D-Only (n = 90) | CAD-Only (n = 60) | |
| Insulin resistance | 1.667 (1.341–1.303) * | 1.594 (1.255–1.880) * | 1.385 (1.089–1.665) * |
| Severity of CAD | a 1.494 (1.160–2.726) ¥ b 1.733 (1.308–2.144) ¥ | – | a 1.622 (1.099–4.923) ¥ b 4.111 (1.381–26.379) ¥ |
| Parameter | OR (95% CI) | p-Value |
|---|---|---|
| Insulin resistance | 1.166 (1.009–3.042) * | 0.030 |
| Severity of CAD | a 1.647 (1.212–1.972) ¥ b 1.815 (1.044–3.040) ¥ | 0.044 0.036 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perumalsamy, S.; Ahmad, W.A.W.; Huri, H.Z. Retinol-Binding Protein-4—A Predictor of Insulin Resistance and the Severity of Coronary Artery Disease in Type 2 Diabetes Patients with Coronary Artery Disease. Biology 2021, 10, 858. https://doi.org/10.3390/biology10090858
Perumalsamy S, Ahmad WAW, Huri HZ. Retinol-Binding Protein-4—A Predictor of Insulin Resistance and the Severity of Coronary Artery Disease in Type 2 Diabetes Patients with Coronary Artery Disease. Biology. 2021; 10(9):858. https://doi.org/10.3390/biology10090858
Chicago/Turabian StylePerumalsamy, Sangeetha, Wan Azman Wan Ahmad, and Hasniza Zaman Huri. 2021. "Retinol-Binding Protein-4—A Predictor of Insulin Resistance and the Severity of Coronary Artery Disease in Type 2 Diabetes Patients with Coronary Artery Disease" Biology 10, no. 9: 858. https://doi.org/10.3390/biology10090858
APA StylePerumalsamy, S., Ahmad, W. A. W., & Huri, H. Z. (2021). Retinol-Binding Protein-4—A Predictor of Insulin Resistance and the Severity of Coronary Artery Disease in Type 2 Diabetes Patients with Coronary Artery Disease. Biology, 10(9), 858. https://doi.org/10.3390/biology10090858