The Significance of Utilizing A Corticotomy on Periodontal and Orthodontic Outcomes: A Systematic Review and Meta-Analysis
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Population, Intervention, Comparison, Outcome (PICO) Question
2.2. Selection Criteria
2.3. Screening Process
2.4. Data Extraction
2.5. Data Analyses
2.6. Risk of Bias Assessment
3. Results
3.1. Features of the Included Studies
3.1.1. Study Design and Participant Features
3.1.2. Outcome Measurements
3.1.3. Anatomic Location of the Study Sites
3.1.4. Active Treatment Time for Patients Receiving Anterior CAOT or PAOO
3.1.5. Bone Grafting Materials
3.1.6. Type of Localized Corticotomy
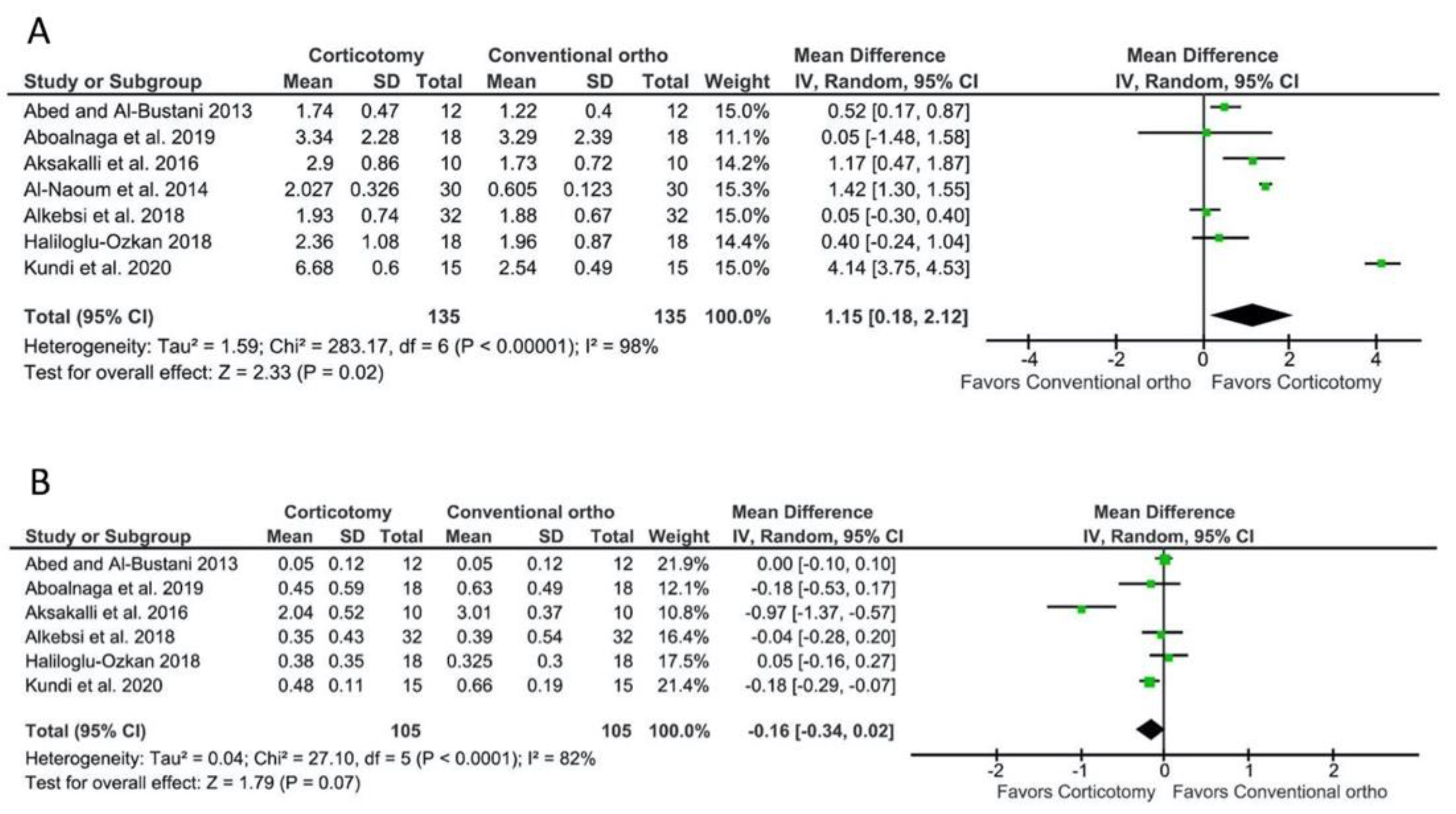
3.2. Meta-Analyses for the Outcomes of a Localized Corticotomy Compared to a Conventional Orthodontic Treatment
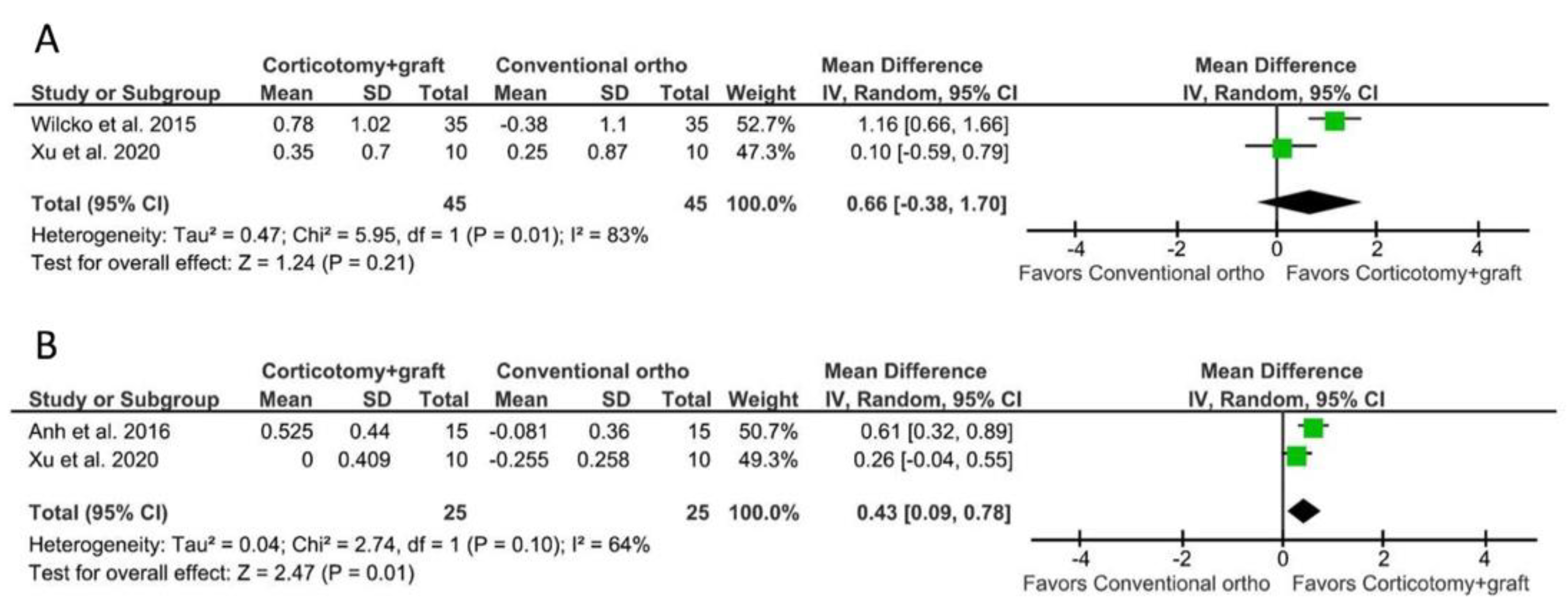
3.3. Meta-Analyses for the Outcomes of PAOO Compared to a Conventional Orthodontic Treatment
3.4. Meta-Analyses for the Outcomes of Anterior CAOT Compared to PAOO
3.5. Risk of Bias Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Study | Random Sequence Generation | Allocation Concealment | Blinding of Participants and Personnel | Blinding of Outcome Assessment | Incomplete Outcome Data Addressed | Selective Reporting | Other Bias |
|---|---|---|---|---|---|---|---|
| Al-Naoum et al., 2014 [32] | Low | Low | Uncertain | Uncertain | Low | Low | Low |
| Aksakalli et al., 2016 [31] | Uncertain | Uncertain | Low | Low | Low | Low | Low |
| Alkebsi et al., 2018 [33] | Low | Low | High | Low | Low | Uncertain | Low |
| Haliloglu-Ozkan et al., 2018 [35] | Uncertain | Uncertain | Low | Low | High | High | Low |
| Aboalnaga et al., 2019 [30] | Low | Low | Low | Low | Low | Low | Low |
| Kundi et al., 2020 [36] | Uncertain | Uncertain | Low | Low | Low | Low | Low |
| Shoreibah et al., 2012 [37] | Uncertain | Uncertain | Uncertain | Uncertain | Low | Uncertain | Low |
| Bahamman 2016 [34] | Uncertain | Uncertain | Low | Low | Low | Uncertain | Low |
References
- Wilcko, W.M.; Wilcko, T.; Bouquot, J.E.; Ferguson, D.J. Rapid orthodontics with alveolar reshaping: Two case reports of decrowding. Int. J. Periodontics Restor. Dent. 2001, 21, 9–19. [Google Scholar]
- Amit, G.; Jps, K.; Pankaj, B.; Suchinder, S.; Parul, B. Periodontally accelerated osteogenic orthodontics (PAOO)—A review. J. Clin. Exp. Dent. 2012, 4, e292–e296. [Google Scholar] [CrossRef]
- Wilcko, M.T.; Wilcko, W.M.; Pulver, J.J.; Bissada, N.F.; Bouquot, J.E. Accelerated Osteogenic Orthodontics Technique: A 1-Stage Surgically facilitated rapid orthodontic technique with alveolar augmentation. J. Oral Maxillofac. Surg. 2009, 67, 2149–2159. [Google Scholar] [CrossRef] [PubMed]
- Frost, H.M. The regional acceleratory phenomenon: A review. Henry Ford Hosp. Med. J. 1983, 31, 3–9. [Google Scholar] [PubMed]
- Wang, C.; Yu, S.; Mandelaris, G.A.; Wang, H. Is periodontal phenotype modification therapy beneficial for patients receiving orthodontic treatment? An american academy of periodontology best evidence review. J. Periodontol. 2020, 91, 299–310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kao, R.T.; Curtis, D.A.; Kim, D.M.; Lin, G.; Wang, C.; Cobb, C.M.; Hsu, Y.; Kan, J.; Velasquez, D.; Avila-Ortiz, G.; et al. American Academy of Periodontology best evidence consensus statement on modifying periodontal phenotype in preparation for orthodontic and restorative treatment. J. Periodontol. 2020, 91, 289–298. [Google Scholar] [CrossRef] [Green Version]
- Zimmo, N.; Sal, M.H.A.; Sinjab, K.; Wang, C.-W.; Mandelaris, G.; Wang, H.-L. Corticotomy-Assisted Orthodontics for Canine Distalization: A systematic review and meta-analysis of clinical controlled trials. J. Int. Acad. Periodontol. 2018, 20, 153–162. [Google Scholar]
- Ahn, H.-W.; Seo, D.-H.; Kim, S.-H.; Park, Y.-G.; Chung, K.-R.; Nelson, G. Morphologic evaluation of dentoalveolar structures of mandibular anterior teeth during augmented corticotomy-assisted decompensation. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 659–669. [Google Scholar] [CrossRef] [PubMed]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inform. Decis. Mak. 2007, 7, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (Updated February, 2021). Available online: www.training.cochrane.org/handbook (accessed on 30 June 2021).
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [Green Version]
- Aboul-Ela, S.M.B.E.-D.; El-Beialy, A.; El-Sayed, K.F.; Selim, E.M.N.; El-Mangoury, N.H.; Mostafa, Y.A. Miniscrew implant-supported maxillary canine retraction with and without corticotomy-facilitated orthodontics. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 252–259. [Google Scholar] [CrossRef]
- Alfawal, A.M.H.; Hajeer, M.Y.; Ajaj, M.A.; Hamadah, O.; Brad, B. Evaluation of piezocision and laser-assisted flapless corticotomy in the acceleration of canine retraction: A randomized controlled trial. Head Face Med. 2018, 14, 4. [Google Scholar] [CrossRef]
- Alikhani, M.; Raptis, M.; Zoldan, B.; Sangsuwon, C.; Lee, Y.B.; Alyami, B.; Corpodian, C.; Barrera, L.M.; Alansari, S.; Khoo, E.; et al. Effect of micro-osteoperforations on the rate of tooth movement. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 639–648. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, P.; Bhattacharya, H.; Anjum, A.; Bhandari, R.; Agarwal, D.; Gupta, A.; Ansar, J. Assessment of corticotomy facilitated tooth movement and changes in alveolar bone thickness—A CT scan study. J. Clin. Diagn. Res. 2014, 8, ZC26–ZC30. [Google Scholar] [CrossRef] [PubMed]
- Charavet, C.; Lecloux, G.; Jackers, N.; Maes, N.; Lambert, F. Patient-reported outcomes measures (PROMs) following a piezocision-assisted versus conventional orthodontic treatments: A randomized controlled trial in adults. Clin. Oral Investig. 2019, 23, 4355–4363. [Google Scholar] [CrossRef]
- Feizbakhsh, M.; Zandian, D.; Heidarpour, M.; Farhad, S.Z.; Fallahi, H.R. The use of micro-osteoperforation concept for accelerating differential tooth movement. J. World Fed. Orthod. 2018, 7, 56–60. [Google Scholar] [CrossRef]
- Gibreal, O.; Hajeer, M.Y.; Brad, B. Evaluation of the levels of pain and discomfort of piezocision-assisted flapless corticotomy when treating severely crowded lower anterior teeth: A single-center, randomized controlled clinical trial. BMC Oral Health 2019, 19, 57. [Google Scholar] [CrossRef]
- Heidbuchel, K.L.; Kuijpers-Jagtman, A.M.; Freihofer, H.P.M. An orthodontic and cephalometric study on the results of the combined surgical-orthodontic approach of the protruded premaxilla in bilateral clefts. J. Cranio Maxillofac. Surg. 1993, 21, 60–66. [Google Scholar] [CrossRef]
- Lee, J.-K.; Chung, K.-R.; Baek, S.-H. Treatment outcomes of orthodontic treatment, corticotomy-assisted orthodontic treatment, and anterior segmental osteotomy for bimaxillary dentoalveolar protrusion. Plast. Reconstr. Surg. 2007, 120, 1027–1036. [Google Scholar] [CrossRef]
- Makki, L.; Ferguson, D.J.; Wilcko, M.T.; Wilcko, W.M.; Bjerklin, K.; Stapelberg, R.; Al-Mulla, A. Mandibular irregularity index stability following alveolar corticotomy and grafting: A 10-year preliminary study. Angle Orthod. 2014, 85, 743–749. [Google Scholar] [CrossRef]
- Medeiros, R.B.; Pires, F.R.; Kantarci, A.; Capelli, J. Tissue repair after selective alveolar corticotomy in orthodontic patients. Angle Orthod. 2017, 88, 179–186. [Google Scholar] [CrossRef] [Green Version]
- Salman, L.H.; Ali, F.A. Acceleration of canine movement by laser assisted flapless corticotomy: An innovative approach in clinical orthodontics. J. Baghdad Coll. Dent. 2014, 26, 133–137. [Google Scholar] [CrossRef]
- Singh, S.; Jayan, B. Comparative evaluation of periodontally accelerated osteogenic orthodontics (PAOO) versus conventional orthodontic tooth movement in adult patients with bimaxillary dentoalveolar protrusion. Int. J. Periodontics Restor. Dent. 2019, 39, 571–577. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Yuan, L.; Wang, B.; Zhang, L.; Shen, G.; Fang, B. Changes of alveolar bone dehiscence and fenestration after augmented corticotomy-assisted orthodontic treatment: A CBCT evaluation. Prog. Orthod. 2019, 20, 7. [Google Scholar] [CrossRef]
- Wang, B.; Shen, G.; Fang, B.; Yu, H.; Wu, Y.; Sun, L. Augmented Corticotomy-Assisted Surgical Orthodontics Decompensates Lower Incisors in Class III Malocclusion Patients. J. Oral Maxillofac. Surg. 2014, 72, 596–602. [Google Scholar] [CrossRef]
- Wu, J.; Jiang, J.-H.; Xu, L.; Liang, C.; Bai, Y.; Zou, W. A pilot clinical study of Class III surgical patients facilitated by improved accelerated osteogenic orthodontic treatments. Angle Orthod. 2015, 85, 616–624. [Google Scholar] [CrossRef] [Green Version]
- Abed, S.S.; Al-Bustani, A.I. Corticotomy Assisted Orthodontic Canine Retraction. J. Baghdad Coll. Dent. 2013, 25, 160–166. [Google Scholar] [CrossRef]
- Aboalnaga, A.; Fayed, M.M.S.; El-Ashmawi, N.A.; Soliman, S.A. Effect of micro-osteoperforation on the rate of canine retraction: A split-mouth randomized controlled trial. Prog. Orthod. 2019, 20, 21. [Google Scholar] [CrossRef]
- Aksakalli, S.; Calik, B.; Kara, B.; Ezirganli, S. Accelerated tooth movement with piezocision and its periodontal-transversal effects in patients with Class II malocclusion. Angle Orthod. 2015, 86, 59–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Naoum, F.; Hajeer, M.Y.; Al-Jundi, A. does alveolar corticotomy accelerate orthodontic tooth movement when retracting upper canines? a split-mouth design randomized controlled trial. J. Oral Maxillofac. Surg. 2014, 72, 1880–1889. [Google Scholar] [CrossRef] [PubMed]
- Alkebsi, A.; Al-Maaitah, E.; Al-Shorman, H.; Abu Alhaija, E. Three-dimensional assessment of the effect of micro-osteoperforations on the rate of tooth movement during canine retraction in adults with Class II malocclusion: A randomized controlled clinical trial. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 771–785. [Google Scholar] [CrossRef]
- Bahammam, M.A. Effectiveness of bovine-derived xenograft versus bioactive glass with periodontally accelerated osteogenic orthodontics in adults: A randomized, controlled clinical trial. BMC Oral Health 2016, 16, 126. [Google Scholar] [CrossRef] [Green Version]
- Haliloglu-Ozkan, T.; Arici, N.; Arici, S. In-vivo effects of flapless osteopuncture-facilitated tooth movement in the maxilla and the mandible. J. Clin. Exp. Dent. 2018, 10, e761–e767. [Google Scholar] [CrossRef]
- Kundi, I.; Alam, M.K.; Shaheed, S. Micro-osteo perforation effects as an intervention on canine retraction. Saudi Dent. J. 2020, 32, 15–20. [Google Scholar] [CrossRef]
- Shoreibah, E.A.; Ibrahim, S.A.; Attia, M.S.; Diab, M.M.N. Clinical and radiographic evaluation of bone grafting in corticotomy-facilitated orthodontics in adults. J. Int. Acad. Periodontol. 2012, 14, 105–113. [Google Scholar] [PubMed]
- Wilcko, M.T.; Ferguson, D.J.; Makki, L.; Wilcko, W.M. Keratinized gingiva height increases after alveolar corticotomy and augmentation bone grafting. J. Periodontol. 2015, 86, 1107–1115. [Google Scholar] [CrossRef] [Green Version]
- Xu, X.; Wu, J.-Q.; Jiang, J.-H.; Liang, C.; Wang, X.-E.; Jing, W.-D.; Xu, L. Periodontal effect of periodontally accelerated osteogenic orthodontics in skeletal angle class III: A Nonrandomized, Controlled Trial. Int. J. Periodontics Restor. Dent. 2020, 40, e169–e177. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [Green Version]
- El-Beialy, A.; Abou-El-Ezz, A.M.; Attia, K.; El-Bialy, A.M.; Mostafa, Y.A. Loss of anchorage of miniscrews: A 3-dimensional assessment. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 700–707. [Google Scholar] [CrossRef]
- Wu, J.; Jiang, J.; Xu, L.; Liang, C.; Li, C.; Xu, X. Alveolar bone thickness and root length changes in the treatment of skeletal Class III patients facilitated by improved corticotomy: A cone-beam CT analysis. Zhonghua kou qiang yi xue za zhi = Zhonghua kouqiang yixue zazhi = Chin. J. Stomatol. 2015, 50, 223–227. [Google Scholar]


| Reason for Exclusion | Author (Year) |
|---|---|
| No data on comparing groups with and without corticotomy procedures. | Heidbuchel et al., 1993 [20] |
| Makki et al., 2015 [22] | |
| Medeiros et al., 2018 [23] | |
| Singh and Jayan 2019 [25] | |
| Wang et al., 2014 [27] | |
| No control group | Alfawal et al., 2018 [14] |
| Inadequate data to be pooled in meta-analyses | Aboul-Ela et al., 2011 [13] |
| Alikhani et al., 2013 [15] | |
| Bhattacharya et al., 2014 [16] | |
| Charavet et al., 2019 [17] | |
| Feizbakhsh et al., 2018 [18] | |
| Gibreal et al., 2019 [19] | |
| Lee et al., 2007 [21] | |
| Salman and Ali 2014 [24] | |
| Sun et al., 2019 [26] | |
| Wu et al., 2015 [28] |
| Localized Corticotomy (Limited to Distal of the Canine) Compared to Conventional Orthodontic Treatment | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Author/Year | Study Design | Duration; Gender; Age Range | Case Type | Treatment Groups (sample size) | Treatment Location | Outcomes | Conclusions | ||||
| Canine Distalization Mean (SD) | Loss of Anchorage Mean (SD) | Canine Tipping Mean (SD) | Active Treatment Time | ||||||||
| Abed and Al-Bustani 2013 [29] | Case-Control Study | 1 month post-surgery; 8f, 4m; average 21.7 | Class II | T: Flap Corticotomy (12) C: Conventional orthodontics (12) | Distal aspect of canine | T: 1.74 (0.47) C: 1.22 (0.40) | T: 0.05 (0.12) C: 0.05 (0.12) | Not reported | 1 month | Flap corticotomy is effective in accelerating orthodontic tooth movement with no harmful effects on surrounding vital structures and/or pulp vitality. | |
| Al-Naoum et al. 2014 [32] | RCT | 3 months post-surgery; 15f, 15m; 20.04 (3.63) | Class II | T: Flap Corticotomy (30) C: Conventional orthodontics (30) | Distal aspect of canine | T: 2.027 (0.326) C: 0.605 (0.123) | Not reported | Not reported | 3 months | Flap corticotomy increased orthodontic tooth movement. Velocities after corticotomies were 2 to 4 times faster in the test group compared to control. | |
| Aksakalli et al. 2016 [31] | RCT | 3.5 months post-surgery; 6f, 4m; 16.3 (2.4) | Class II | T: MOP with piezocision (10) C: Conventional orthodontics (10) | Distal aspect of canine | T: 2.90 (0.86) C: 1.73 (0.72) | T: 2.04 (0.52) C: 3.01 (0.37) | Not reported | 3.5 months | MOP with piezocision-assisted distalization accelerates tooth movement, decreases the anchorage loss for posterior teeth, and does not induce any maxillary transversal change or adverse effects on periodontal heath. | |
| Alkebsi et al. 2018 [33] | RCT | 3 months post-surgery; 24f, 8m; 19.26 (2.48) | Class II | T: MOP with mini-screw (32) C: Conventional orthodontics (32) | Distal aspect of canine | T: 1.93 (0.74) C: 1.88 (0.67) | T: 0.35 (0.43) C: 0.39 (0.54) | T: 0.25 (0.23) C: 0.25 (0.26) Data in mm | 3 months | MOP was not effective in accelerating tooth movement at any time point. There was no significant difference between test and control at any time points. | |
| Haliloglu-Ozkan et al. 2018 [35] | RCT | 2 months post-surgery; 13f, 19m; T: 15.27 (1.62), C: 16.13 (1.28) | Not reported | T: MOP corticotomy with mini-screw (18) C: Conventional orthodontics (18) | Distal aspect of canine | T: 2.36 (1.08) C: 1.96 (0.87) | T: 0.38 (0.35) C: 0.325 (0.30) | T: 7.57 (2.67) C: 4.545 (2.05) Data in degree | 2 months | MOP did not facilitate accelerated canine distalization or loss of molar anchorage. Canine tipping was significant in the treatment group. | |
| Aboalnaga et al. 2019 [30] | RCT | 4 months post-surgery; 18f; 16–25 | Not reported | T: MOP corticotomy with mini-screw (18) C: Conventional orthodontics (18) | Distal aspect of canine | T: 3.34 (2.28) C: 3.29 (2.39) | T: 0.45 (0.59) C: 0.63 (0.49) | The canine cusp tips moved a greater distance than the apices in both sides | 4 months | MOP did not facilitate accelerate canine distalization. Also, it did not reduce molar anchorage compared to the control group. | |
| Kundi et al. 2020 [36] | RCT | 16 months post-surgery; 16f, 14m; 20–36 | Class II | T: MOP corticotomy with standardized needle gun (15) C: Conventional orthodontics (15) | Distal aspect of canine | T: 6.68 (0.60) C: 2.54 (0.49) | T: 0.48 (0.11) C: 0.66 (0.19) | Not reported | 4–5 months | MOP accelerated canine distalization. There was no significant difference in anchorage loss between treatment and control group. | |
| PAOO (Anterior Corticotomy + Graft) Compared to Conventional Orthodontic Treatment | |||||||||||
| Author/Year | Study Design | Duration; Gender; Age Range | Case Type | Treatment Groups (sample size) | Treatment Location | Outcomes | Conclusions | ||||
| Keratinized Tissue Gain Mean (SD) | Bone Thickness Gain Mean (SD) | Active Treatment Time | |||||||||
| Wilcko et al. 2015 [38] | Case-Control Study | T: 19.4 months post-treatment, C: 15.9 months post-treatment; 48f, 22m; 12.1–61.5 | Not reported; no open bites included | T (PAOO): Corticotomy + DFDBA and bovine xenograft (35) C: Conventional orthodontics (35) | Mand ant | T: 0.78 (1.02)C: −0.38 (1.10) | Not reported | T: 7.1 (1.7) monthsC: 22.1 (6.8) months | PAOO helps in increasing keratinized tissue surrounding dentition compared to conventional orthodontic treatment. | ||
| Ahn et al. 2016 [8] | Case-Control Study | T: 8.7 months C: 10.9 months pre-orthognathic; 16f, 14m; T: 23.06 (6.16) C: 21.51 (3.34) | Class III | T (PAOO): Corticotomy + bovine xenograft (15) C: Conventional orthodontics (15) | Mand ant | Not reported | T: 0.525 (0.44) C: −0.081 (0.36) | T: 8.7 months C: 10.9 months | PAOO provided a favorable decompensation pattern for mandibular incisors and preserved the periodontal structures surrounding mandibular anteriors. | ||
| Xu et al. 2020 [39] | Case-Control Study | 6 months post-treatment; 14f, 6m; 18–30 | Class III | T (PAOO): Corticotomy + tricalcium phosphate bone substitute (10) C: Conventional orthodontics (10) | Max ant | T: 0.35 (0.77) C: 0.25 (0.87) | T: 0 (0.409) C: −0.255 (0.258) | Not reported | PAOO does not negatively affect periodontium and alveolar bone based on the findings of bone from the trial. | ||
| PAOO (Anterior Corticotomy + Graft) Compared to CAOT (Anterior Corticotomy) | |||||||||||
| Author/Year | Study Design | Duration; Gender; Age Range | Case Type | Treatment Groups (sample size) | Treatment Location | Outcomes | Conclusions | ||||
| Pocket Depth Reduction Mean (SD) | Root Length Reduction Mean (SD) | Bone Density Change Gray Value (SD) | Active Treatment Time | ||||||||
| Shoreibah et al. 2012 [37] | RCT | 6 months post-treatment; 16f, 4m; average 24.5 | Class I | T (PAOO): Corticotomy + Bioactive glass (10) C (CAOT): Corticotomy only (10) | Mand ant | T: 1.559 (0.614) C: 1.427 (0.237) | T: 0.050 (0.026) C: 0.056 (0.025) | T: 25.849 (15.644) C: −17.596 (5.774) | T: 16.67 weeks C: 17 weeks | Performing corticotomy significantly reduced the total time of treatment. The incorporation of bone grafting material with corticotomy increased the alveolar bone density significantly. | |
| Bahamman 2016 [34] | RCT | 9 months post-treatment; 23f, 10m; 18–27 | Class I | T1 (PAOO): Corticotomy + Bioactive glass (11) T2 (PAOO): Corticotomy + Bovine xenograft (11) C (CAOT): Corticotomy only (11) | Mand ant | T1: 0.37 (0.08) T2: 0.37 (0.08) T1/T2 combined: 0.37 (0.08) C: 0.36 (0.09) | T1: 0.03 (0.50) T2: 0.04 (0.58) T1/T2 combined: 0.035 (0.528) C: 0.03 (0.67) | T1: 13.71 (14.33) T2: 31.99 (14.45) T1/T2 combined: 22.85 (16.874) C: 0.87 (15.28) | T1: 14.4 weeks T2: 16.8 weeks C: 15 weeks | Combination of orthodontic treatment and corticotomy decreased the duration of active treatment. Use of PAOO approach provided superior benefits in terms of increased bone density. | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gao, J.; Nguyen, T.; Oberoi, S.; Oh, H.; Kapila, S.; Kao, R.T.; Lin, G.-H. The Significance of Utilizing A Corticotomy on Periodontal and Orthodontic Outcomes: A Systematic Review and Meta-Analysis. Biology 2021, 10, 803. https://doi.org/10.3390/biology10080803
Gao J, Nguyen T, Oberoi S, Oh H, Kapila S, Kao RT, Lin G-H. The Significance of Utilizing A Corticotomy on Periodontal and Orthodontic Outcomes: A Systematic Review and Meta-Analysis. Biology. 2021; 10(8):803. https://doi.org/10.3390/biology10080803
Chicago/Turabian StyleGao, Jonathan, Trung Nguyen, Snehlata Oberoi, Heesoo Oh, Sunil Kapila, Richard T. Kao, and Guo-Hao Lin. 2021. "The Significance of Utilizing A Corticotomy on Periodontal and Orthodontic Outcomes: A Systematic Review and Meta-Analysis" Biology 10, no. 8: 803. https://doi.org/10.3390/biology10080803
APA StyleGao, J., Nguyen, T., Oberoi, S., Oh, H., Kapila, S., Kao, R. T., & Lin, G.-H. (2021). The Significance of Utilizing A Corticotomy on Periodontal and Orthodontic Outcomes: A Systematic Review and Meta-Analysis. Biology, 10(8), 803. https://doi.org/10.3390/biology10080803





