Abstract
Fixed restorations are now among the most common restorations in modern dental prosthodontics. The current view in prosthodontics of maximum preparation economy is causing an increased interest in the mechanical properties of cements. Among the most important properties of materials used for indirect cementation are mechanical properties, i.e., hardness and compressive strength. These properties can change as a result of changes in physical factors. The purpose of this study was to analyze the available literature on the effect of conditioning temperature of cements used for cementation of indirect fixed restorations on the durability of their bonding to dental tissues and their mechanical and physical properties. The following databases were used: Mendeley, PubMed, ResearchGate, National Library of Medicine, and Google Scholar. Analysis of the available literature was carried out according to the Prisma diagram program. Forty-eight articles were selected, which were the following types of studies: clinical reports, research article, and review articles. Some studies indicated that mechanical properties, such as flexural strength, polymerization shrinkage, and conversion factor, did not change after heating the composite material. According to some researchers, preheating the composite material increased its conversion degree, which consequently led to an increase in hardness and fracture toughness, an increase in flexural strength and an increase in elastic modulus, and an increase in abrasion resistance. Studies on changes in the mechanical and physical properties of composite materials, as well as composite cements, have not always provided clear answers, as there are still no laboratory and clinical studies that fully confirm the benefits of heating composite cements. Conducting studies evaluating the effect of elevated storage temperature on the strength parameters of cements, in conjunction with the type of material and its composition, could provide answers to many clinical questions that are still unresolved. If the benefits of heating cements were unequivocally confirmed in laboratory studies, this could open up many possibilities for improving the retention of fixed prosthetic restorations.
1. Introduction
Fixed prosthetic restorations are currently one of the most commonly performed restorations in dental prosthodontics. The durability of these types of restorations is dependent among others on one of the most important forces called retention. Retention, as the force that holds the restoration on the prosthetic pillar, is determined by the geometric configuration of the pillar tooth walls created during preparation, which directly translates into the size of the bonding area, between the tooth’s own tissues and the prosthetic restoration. The most important factor influencing the retention of a fixed prosthetic restoration is the strength of cement adhesion to the tooth surface and prosthetic restoration. The mechanical properties of the cement, such as hardness and compressive strength, are the factors that determine proper retention of the fixed prosthetic restoration. Among the cements currently and most widely used in prosthodontics, composite cements seems to be the most popular. Composite cements can be divided according to the method of tooth surface preparation and according to the method of initiation of the polymerization process. The preferably clinical classification of composite cements is based on the method of surface preparation. According to this classification, cements are divided into resin, self-etch, and self-adhesive. Currently, self-adhesive cements are the most commonly used cements by clinicians, and their popularity is due to the simplified application procedure, which significantly saves time spent on the cementing procedure [1,2].
Self-adhesive cements are modified resin cements that bond to hard tissue in two stages. In the first step, the superficial layers of hard tissue are demineralized by the action of acidic monomer groups, which leads to the formation of a bond between the methacrylates and the enamel and dentin. Later, metal ions from the fillers are released and further bonding to enamel and dentin occurs [1,2]. These cements do not require acid conditioning of the tooth surface or application of a bonding agent prior to cementation [3]. According to the manufacturers, the functional monomers are able to chemically bond calcium to hydroxyapatite, which in the case of this group of cements is one of the bonding mechanisms responsible for the retention of the restoration [4,5,6]. Of the many analyses and conclusions regarding composite cements in the literature, the most noteworthy are those that translate significantly to clinical work. It has been concluded that if the grinding limit is in the enamel and dentin, conventional composite cements should be the materials of choice because of their strong bond to the enamel. It was also noted that the use of selective enamel etching prior to the use of resin and highly recommended for self-etch cements. It has also been shown that the strength of self-etch cements with dentin, compared to conventional composite cements, is higher. Additionally, it is known that despite the lack of clear recommendations for bonding systems, in the case of self-adhesive cements, the additional use of phosphoric acid is necessary to develop the enamel surface. Studies show that selective etching of the enamel significantly improves the bonding of the cement to this tissue [7,8].
From a clinical point of view, it is necessary to take into account the possible influence of modifiable factors, such as the type of activation method, the quality and method of mixing, or finally, the storage temperature. Most composite cements in use today have the manufacturer’s storage temperature specified as room temperature. According to the American Haritage Dictionary of the English Language, room temperature is 20–22 °C (68–72 °F). Merriam-Webster defines room temperature as a range of 15 °C to 25 °C (59–77 °F) as suitable for long-term human habitation and laboratory experiments. Room temperature is usually lower in winter and higher in summer. The World Health Organization (WHO) indicates a trend that women often prefer warmer temperatures than men, and this is due to the higher metabolism in women and the hormonal economy. Some current research agencies refer to room temperature as normal temperature. The International Union of Pure and Applied Chemistry (IUPAC) defines standard temperature as 25 °C (77 °F, 298 °K). The U.S. Environmental Protection Agency (EPA) defines normal temperature as 25 °C (77 °F). In scientific guilds, room temperature should be recorded and reported because it may differ from ideal or standard values. The storage temperature may exceed the manufacturer’s recommended range of room temperature in the event of a situation related to improper conditions of transport of materials and the occurrence of artificial temperature fluctuations caused by storing materials in the vicinity of devices that change room temperature, such as air conditioners or heaters. Variations in the storage conditions of dental materials can also be caused by the lack of clear procedures and algorithms for dealing with the storage of materials in the dental office environment. This can perhaps contribute to unconscious negligence leading to irregularities. It is believed that the human factor is the main factor initiating storage irregularities of dental materials, which can lead to changes in the strength parameters of these materials [9,10].
Hence the aim of this study was to analyze the available literature on the effect of conditioning the temperature of cements used for cementation of indirect fixed restorations on the durability of their bond with the tooth’s own tissues and their mechanical and physical properties. The authors of the paper were particularly interested in how ambient temperature can contribute to changes in the mechanical properties of composite cements, in the range of room temperature as well as temperatures beyond room temperature.
2. Materials and Methods
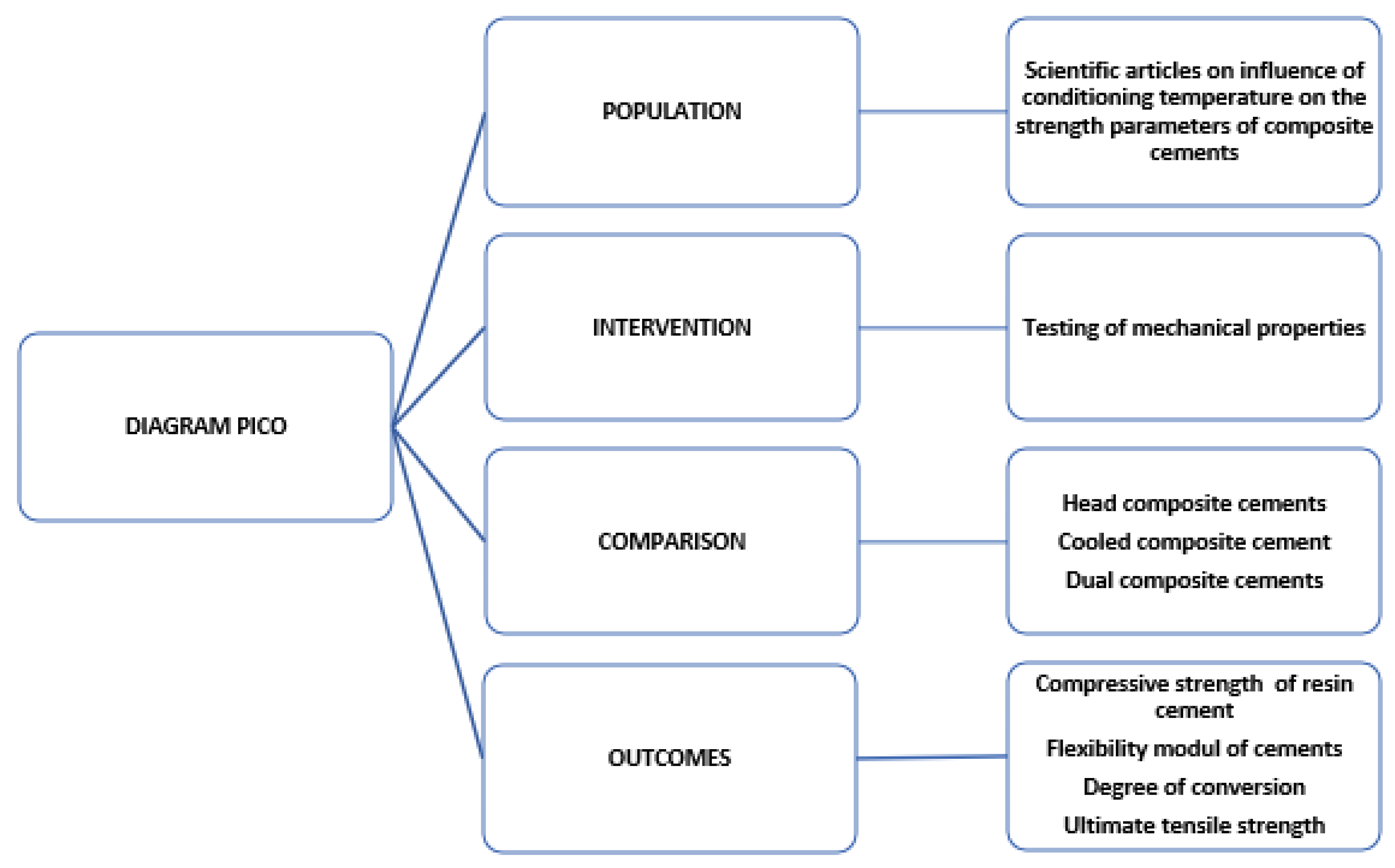
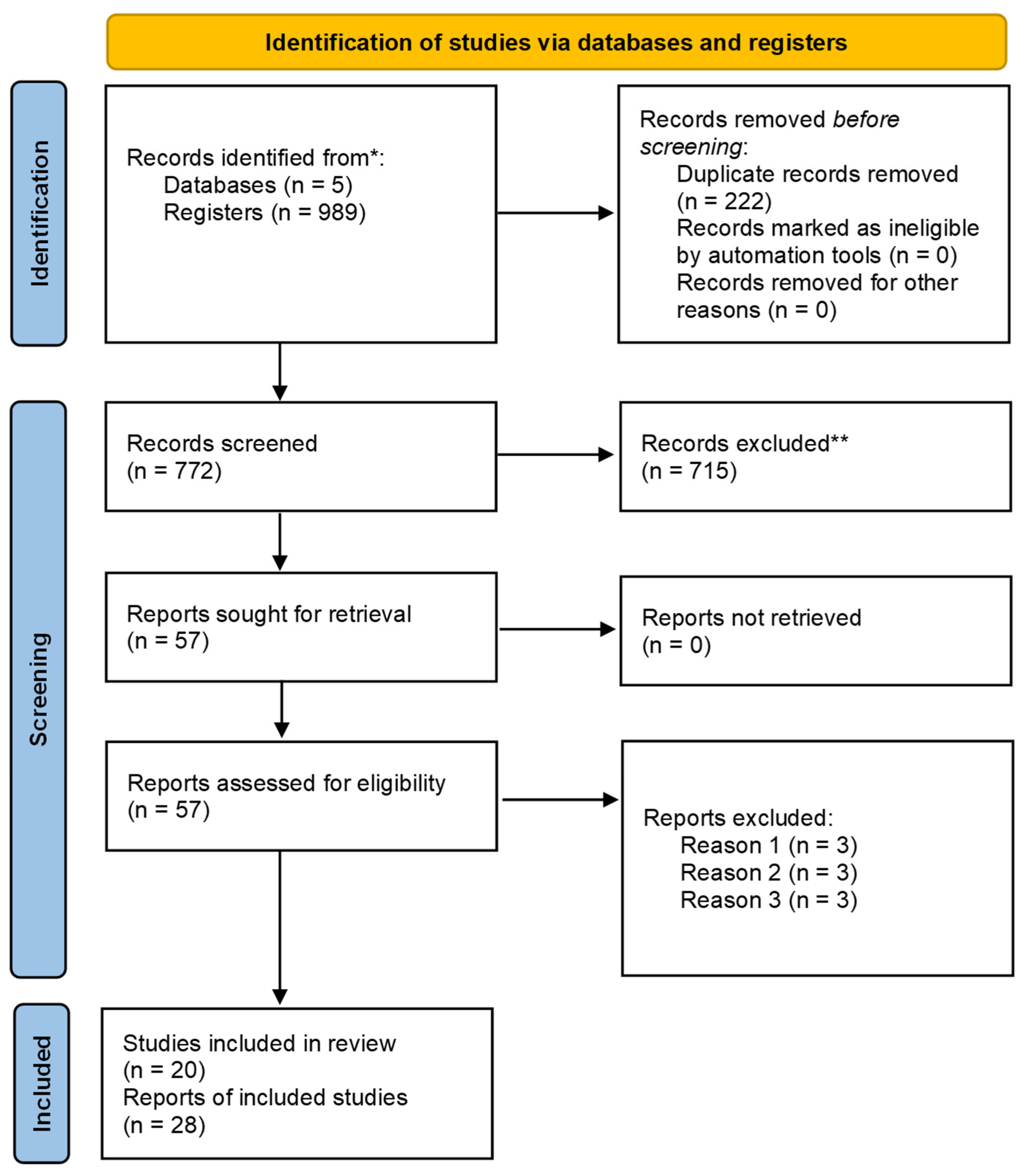
The following databases were used: Mendeley, PubMed, ResaerchGate, National Library of Medicine, and Google Scholar. Analysis of the available literature was performed according to PICO diagram (Figure 1) and Prisma diagram (Figure 2). The PICO diagram was designed to formulate a clinical question, according to evidence-based medicine. It allows to explicitly formulate the right clinical questions using an expansion from the PICO acronym (P-population, I-intervention, C-comparison, O-outcome) [11,12]. PRISMA stands for preferred reporting items for systematic reviews and meta-analyses. It is an evidence-based minimum set of items for reporting in systematic reviews and meta-analyses [13]. It includes a checklist and flow diagram for planning a systematic review. Seventy-eight articles were eligible for the presented review. Inclusion criteria adopted in this review are in vitro studies, articles that focus on the mechanical properties of composite cements or dental composites, indirect prosthetic restorations, and available full-text article. Exclusion criteria were studies applied in permanent dentition that evaluated the hardness in indirect restorations and then evaluated the compressive strength in indirect restoration. Used search terms included: heated composite cement, cooled composite cement, dual composite cement and mechanical properties, hardness, compressive strength and mechanical properties of composite cements, and strength parameters of composite cements.
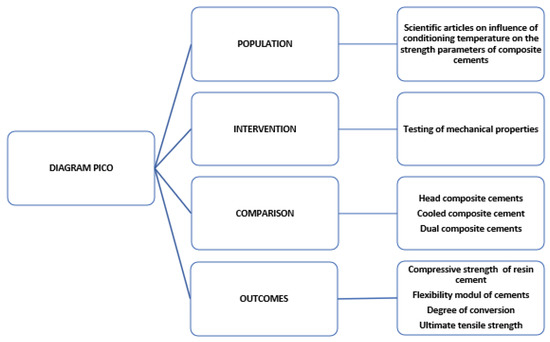
Figure 1.
The PICO diagram implemented in this review [11,12].
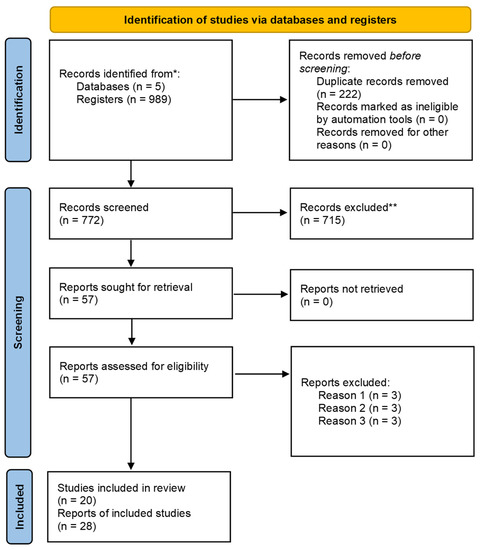
Figure 2.
The PRISMA flowchart of the study selection [13].
Taking into account the above inclusion and exclusion criteria, a total of 989 articles was identified. Duplicate articles and those that did not meet the above criteria were not considered. Of the remaining studies, 48 articles, which were original papers or literature reviews, were left, for detailed evaluation. The articles left for evaluation were evaluated in terms of studies describing the bond strength of cements, modulus of elasticity of the degree of conversion, compressive strength, and tensile strength in indirect restorations. The list of properties abbreviations used in this review is in Table 1.

Table 1.
The list of abbreviations used in this review.
3. Results and Discussion
There are reports indicating that storage conditions of composite cements can significantly affect their bond strength. Ozer F. et al. [14] conducted a comparison of the bonding performance of three different self-adhesive resin cements to human dentin after storage under two different temperature conditions. The test cements used in both study groups were: Clearfil SA (CSA), G-Cem (GC), and Bis-Cem (BC). The cements of the first group were stored in a refrigerator at 6 ± 2 °C for 3 months and the cements of the second group were stored at a constant room temperature of 19 ± 2 °C for an additional 3 months. Each group consisted of 6 teeth and 24 dentin scrapings, and cementation was performed in both storage groups according to the manufacturer’s recommendations. After determining the shear bond strength (SBS), bond forces were calculated and translated into values expressed in MPa. The bond strength values in the two storage groups were significantly different from each other. The bond forces decreased significantly after storage at room temperature, and this was true for all cements in this storage group (Table 2) [14].

Table 2.
The bond strengths (BS) between resin cements and human dentin [MPa] presented in [14].
The compressive strength of composite cements was measured by other investigators in water at 37 °C and at 0.5, 1, 5, and 60 min after removal from the water bath. All of the cements tested showed a very rapid decrease in temperature after removal from the water bath, and a marked increase in strength of all cements was shown within the first minutes after removal from the water bath [15].
There are also reports on the use of heated composite material for cementing intermediate works. The idea of using restorative materials after they have been preheated has been used for almost 40 years, and the material that was used first after preheating was a regular composite resin [16]. In light of current research, it is even believed that this preheated composite material can compete with dual-cure composite cements when cementing indirect restorations. In fact, studies have shown that preheating the composite material used for cavity filling can find application in the adhesive cementation procedure. The heated composite material has higher fluidity, elastic modulus, and microhardness. The higher fluidity can reduce the viscosity of the material, which can directly affect the application method and improve marginal tightness [17,18,19].
Skąpska A et al. [20] conducted a pilot study to compare selected mechanical properties of a heated composite material and a self-adhesive composite cement. The aim of their work was to compare selected mechanical properties, compressive strength, and modulus of elasticity of the heated composite material Enamel Plus Hri (Micerium) and dual composite cement RelyX U200 (3M). For the test, specimens of each material type were prepared in the shape of a 5 × 3 mm cylinder, using silicone molds. The material temperature (50 °C) was obtained using an Ena-Heat heating device (Micerium). The test was performed using an Instron 8501 hydraulic pulse oximeter, which is a universal testing machine. The compressive strength test was used, and the modulus of elasticity was calculated. Analysis of the results showed that the average compressive strength the heated composite material was 530 or 327 MPa, depending of the material (Table 3). The study also showed that the heated composite material has a higher modulus of elasticity (7.9 ± 1.48 GPa) and thus is more rigid compared to the self-adhesive composite cement (5.9 ± 0.35 GPa). This study proved that a heated composite material has better mechanical properties compared to a self-adhesive cement. The different values of compressive strength and modulus of elasticity can be explained by the difference in the composition of the different materials (Table 3) [20]. Enamel Plus Hri has a higher value of inorganic filler (53% by volume) compared to RelyX U200 cement (43% by volume). The increased amount of filler may result in increased mechanical strength. The compressive strength of Enamel Plus Hri, as a referential value, amounts 340 MPa [21].

Table 3.
Flexibility module E [GPa] and average compressive strength CS [MPa] of two studied cement before and after heating from [20].
In another study, Skąpska et al. conducted a study to compare composite cements with preheated composite materials. Enamel Plus Hri (Micerium) composite material and RelyX U200 Automix (3M) dual composite cement were tested for microhardness, compressive strength, flexural strength, diametric compressive strength, and modulus of elasticity. The composite materials were heated to 50 °C before polymerization. Higher values of microhardness (by 67.36%), compressive strength (by 41.84%), elastic modulus (by 17.75%), flexural strength (by 36.03%), and diametral tensile strength (by 45.52%) were obtained using heated Enamel Plus Hri composite material compared to RelyX U200 adhesive cement [22].
Additionally, it has also been shown that heating can increase the fluidity of composites characterized by a regular consistency, which can translate into improved adaptation of the material to the walls of the prepared cavity. In the study of Sanjukta Deb at al. [23], the preheating of the resin composites exhibited a significant decrease in film thickness after preheating, so it can be crucial from the clinical point of view [23]. The authors suggested that enhancing flow is resulted from thermal energy that translates to higher molecular motion [23]. The heated material showed less viscosity, which consequently translated into a better fit to the edges of the cavity. This resulted in better adhesion at the border of the material with the tooth’s own tissues and reduced marginal microleakage. Minimizing marginal microleakage resulted in a lower tendency for secondary cavity caries and resulted in clinical success in terms of long-term bonding of the material to the tooth’s own tissues [24,25,26]. Studies on the modulus of elasticity have shown that similar values of the modulus of elasticity of dentin and cement result in proper functioning of the prosthetic restoration in the stomatognathic system, and in this context, it should be mentioned that the average value of the modulus of elasticity for dentin is considered to be 19 GPa [27]. Based on the assumption that, since the dual composite cement contains filler in its composition, such as the composite material, only in a smaller amount, because the filler constitutes 30%–75% of the volume in the case of the adhesive cement and the composite material contains 60%–80% of this component, it could be hypothesized that even minimal heating of the composite cement alone could improve its mechanical properties.
Morais et al. [28] performed a study to evaluate the effect of preheated, dual-cured resin cements on the bond strength of indirect restorations to dentin. The research hypothesis was that preheating the dual composite cement provided greater bond strength to dentin, compared to using the cement at room temperature, regardless of the activation mode. The study was conducted on forty freshly extracted and erupted human molars. Composite discs mimicking indirect composite restorations and three dual composite cements Variolink II (Esthetic DC), Calibra (Dentsply Sirona), and Excite (Ivoclar) were used. Previously prepared teeth were assigned to eight groups depending on the cement temperature (25 or 50 °C), the type of cement among the three selected for the study, and the activation mode (dual bond or self-curing mode). The specimens were cut to obtain multiple bonded beams with a cross-sectional area of 1 mm2 for tensile strength testing and then tested using a universal testing machine. In conclusion, it was found that elevated temperature before polymerization may promote higher tensile strength over dentin in indirect restorations. The increase in microtensile bond strength (µTBS) values at 50 °C (from 33.38 to 47.12 MPa) was due to the presence of the self-curing component of benzoyl peroxide (BPO) in Variolink II [28]. This component is activated by heat and decomposes faster into free radicals at higher temperatures compared to room temperature. As a consequence of this, it may contribute to an increase in µTBS values. However, the effectiveness of heating the composite dual cement on µTBS was product dependent, as the greatest effect in terms of increased µTBS was observed for cements with low self-curing components. For Variolink II cement, significant differences were found for temperature and activation mode factors in µTBS results. For Calibra cement, no significant difference was found in µTBS values as a function of temperature and activation mode [28].
Some researchers have observed that the use of elevated temperature in glass ionomer cements improves marginal adhesion, reduces working time, and increases surface microhardness up to the 4 mm level [29,30]. Resin-based materials, such as hybrid composite resins, resin cements, and siloranes, have also been subjected to laboratory studies to evaluate the effects on their physical and photoactivation properties. It was found that the average heating temperature of these materials found in the literature is 54–68 °C and considered safe for pulp in the study conducted [31,32,33]. According to a study by Knezevic et al., the limiting safety temperature for pulp in the context of heating composite materials is 68 °C [34]. Some researchers believe that the harmful threshold for living dental pulp tissue is a 5.5 °C increase in dental pulp temperature [35]. There are also reports confirming that heating composite cement to 60 °C prior to polymerization reduced viscosity and allowed for increased free radical mobility [23,36]. As a consequence, these materials achieved higher monomer conversion at elevated temperatures than when used at room temperature [37,38,39,40,41]. When free monomers are present (lower degree of conversion), it is important to note that they can cause severe allergic reactions, and their occurrence is a highly undesirable phenomenon. The incompletely reacted monomers may also leach into the oral environment, into saliva, and consequently reduce the mechanical strength of the restorations, alter their color, and create the possibility of the development of unfavorable bacterial flora in the oral environment [23].
In the study by Franca et al. [42], the degree of conversion (DC) and tensile strength due to preheating to 50 °C before and during polymerization of dual-cured resin cements were analyzed [43]. Disc-shaped and hourglass-shaped samples were prepared from Rely X ARC (3M) and Variolink II cements using silicone adhesion molds. The samples were subjected to temperatures of 25 °C and 50 °C, three curing conditions, and light activation through a glass slide and through a pre-cured 2-mm-thick resin composite disc and then allowed to self-cure. The samples were stored dry in the dark for 15 days. For DC analysis, the resin cements were placed in a mold located at the center of a horizontal rhombus, on an attenuated total reflectance element, and in the optical bench of a Fourier transform infrared spectrometer. Infrared spectra (n = 6) were collected in the range 1680–1500 nm. The degree of conversion was calculated by standard methods using changes in the ratio of aliphatic to aromatic C=C absorption peaks in the cured and uncured states. The specimens (n = 10) were subjected to tensile testing in a universal testing machine at a crosshead speed of 1 mm/min until failure. Both cements showed higher conversion degree value at 50 °C than at 25 °C in all curing conditions. However, there was no significant difference in tensile strength values between the light-activated groups at 25 °C and the groups at 50 °C. In summary, it was found that an increase in temperature led to an increase in the conversion rate, but the effect of increased temperature on tensile strength depended on the curing conditions. Such a result confirms previous reports and can be attributed to the increased mobility of radicals and the frequency of collisions between unreacted active groups and radicals, resulting from the reduced viscosity promoted by the increased temperature [23]. Some researchers indicate that preheating the resin composite even to 60 °C still increases its conversion rate [36,37]. This results in increased hardness and fracture toughness, increased flexural strength and modulus, and increased abrasion resistance [43,44].
When monomer conversion is closely related to the mechanical properties of the contained polymer, improved bond strength of indirect restorations to dentin can be expected, even if the polymerization of the dual-bond composite cement is based solely on self-curing components in a chemical reaction [45,46,47].
Studies of microtensile bond strength and resin-dentin adhesive bonding have shown that preheating composite resin for cementing procedures may not improve microtensile bond strength, although it can be used to reduce material viscosity and improve adhesive bonding strength. Ten experimental groups were set up using human molars with three different composite materials. These included Rely X ARC resin cement and Venus and Z250 XT composite resins. The composite resins were tested both at room temperature and when heated to 64 °C. The filling depth was tested using intermediate composite restorations with a height of 2 or 4 mm, previously fabricated on cylindrical molds. Adhesive and luting procedures were performed under simulated pulp pressure. After cementation, teeth were cut into beams with a cross-sectional area of 1 mm2 at the adhesive interface and subjected to tensile testing at 0.5 mm/min. The characteristics of the adhesive interfaces were evaluated under a scanning electron microscope (SEM). When cementing 2 mm restorations, Z250 XT composite resin preheated or at room temperature achieved significantly higher microtensile bond strength than RelyX ARC cement. At this depth, Venus composite resin did not differ from the resin cement, and for 4 mm restorations only, preheated Venus exhibited significantly higher microtensile bond strengths than RelyX ARC. Preheating the composite resin resulted in a thinner luting bond, with a more intimate interaction between the luting agent and the adhesive layer [48].
In addition to the temperature factor of preheating itself, the time required to achieve the desired fluidity and thus improve the properties of the filler material is equally important. From the available studies, it appears that there is a very wide variation in heating times. The most common time used to anneal the material was 15 min, and the time span for annealing composite materials, among the available studies, ranged from 40 s to 24 h. In the oral cavity, the action of a constant temperature stimulus affects the maturity of dental materials and improves their properties. High temperatures, reached above the glass transition temperature, can cause irreversible deformation and changes in properties, even over a short period of time [49,50,51,52].
An important consideration regarding the storage conditions of composite cements is the recommendation for storage at or below room temperature. Some composite materials require manufacturer-recommended refrigerated storage, but researchers recommend removing them from the refrigerator just before use. This is attributed to the disruption of some of the properties of the composite resin under reduced temperature conditions, related to the significant dynamics of the composite temperature drop after removal from the heater. A 50% drop in temperature was recorded within 2 min. The best monomer conversion results were achieved when the heated composite was dispensed and used as quickly as possible. Neither repeated nor prolonged heating of the composite significantly affected monomer conversion [39].
From the collected studies, composite resins when heated show significant improvement in physical and strength properties [53,54,55,56,57,58,59,60,61,62,63], such as an increase in conversion rate and a decrease in polymerization shrinkage [61,62,63,64,65,66,67].
Significant differences in the mechanical properties of dual composite cements have been found with chemical activation alone than with light curing alone [68]. It has been noted that dual cements also exhibit the greatest fault tolerance during earning compared to resin matrix cements, which are among the most demanding and complicated cements in terms of cementing procedure [69,70].
There is very concrete evidence of a positive correlation of heating cements on the potential for improved mechanical properties. The clinical success of composite restorations is closely related to material characteristics, such as polymerization shrinkage, conversion rate, and mechanical properties [71,72,73]. Improvements in these properties consequently may yield improved retention of fixed restorations, which can clearly translate into long-term clinical success. Numerous studies demonstrate that there is a clear relationship between increasing the temperature of composite materials, both restorative materials and dental cements, and the benefits of improving their physical and mechanical properties (Table 4). However, studies on the exchange of mechanical and physical properties of composite materials as well as composite cements do not always provide clear answers, as there is still a lack of clinical studies that conclusively confirm the benefits of heating composite materials. There is also a lack of comprehensive studies of dental resin materials mechanical properties in wide range of conditioning temperature. In the collected literature, the strength values of the bonding of teeth to dental cements vary considerably. This may probably be due to the fact that the tests were conducted under different physical and chemical conditions, and the polymerization process may have differed, and in addition, the tested samples may have been stored in water for different times. Unification of these studies could bring answers to many nagging questions and unequivocally give an answer to the question: how can storage conditions affect the strength parameters of composite cements used in dental prosthetics? Deepening these studies could provide answers to many clinical problems.

Table 4.
Summary table of mechanical properties of materials relevant for this review.
4. Conclusions and Recommendations
After analysis, 48 articles were selected. The studies in them indicate that preheating composite materials can have both positive and negative effects on some physical and mechanical properties. On the basis of presented articles, it follows that an increase in temperature led to an increase in the conversion degree, but the tensile strength of material is rather dependent on the curing conditions. In turn, the increase in microtensile bond strength with temperature is a material-dependent phenomenon. Some studies indicate that mechanical properties, such as flexural strength, polymerization shrinkage, and conversion rate, did not change when the composite material was heated. According to some researchers, preheating the composite material increased its conversion rate, which consequently led to increased hardness and fracture toughness, increased flexural strength and increased elastic modulus, and increased abrasion resistance.
Studies on the changes in the mechanical and physical properties of composite materials as well as composite cements do not always give clear answers because there are still no clinical trials that would fully confirm the benefits of heating composite cements.
Analysis of available studies of the effect of temperature changes on the strength properties of cements and composite materials has provided inconclusive results. Different properties were studied, and the studies themselves were conducted on a limited number of materials. The studies analyzed in the review indicate the unavailability of sufficient resources to formulate unambiguous conclusions and the small size of the research sample, all of which we can describe in research as a limitation of the study. Conducting studies evaluating the effects of storage temperatures (wider range of temperature) on the strength parameters of cements, in connection with material type and composition, could provide answers to many clinical questions still unresolved. If the benefits of heating cements were confirmed in laboratory tests, then it could open up many possibilities for improving the retention of fixed prosthetic restorations. It also seems reasonable to add specific information about storage and manipulate temperature of cement rather than only “room temperature”.
Author Contributions
Conceptualization, J.G. and K.B.; investigation, K.B. and J.G.; methodology, K.B. and J.G.; project administration, J.G.; resources, J.S.; supervision, B.D. and J.S.; writing—original draft, J.G. and K.B.; writing—review and editing, J.G., K.B., B.D. and J.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Pryliński, M. Vademecum Materiałoznawstwa Protetycznego; Med Tour Press International: Otwock, Poland, 2020; pp. 124–129. [Google Scholar]
- Albert, F.E.; El-Mowafy, O.M. Marginal adaptation and microleage of Procera AllCeram crowns with four cements. Int. J. Prosthodont. 2004, 17, 529–553. [Google Scholar] [CrossRef] [PubMed]
- Bosso Andre, C.; Agular, T.R.; Ayres, A.P.; Bovi Ambrosano, G.M.; Giannini, M. Bond strength of self-adhesive resincements to dry and moist dentin. Braz. Oral Res. 2013, 27, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Aguiar, T.R.; Di Francescantonino, M.; Ambrosano, G.M.B.; Giannini, M. Effect of curing mode on bond strength of self-adhesive resin luting cements to dentin. J. Biomed. Mater. Res. B Appl. Biomater. 2010, 93, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Pisani-Proenca, J.; Erhard, M.C.; Amaral, R.; Valandro, L.F.; Bottino, M.A.; Del Castillo-Salmerón, R. Influence of different surface conditioning protocols on microtensile bond strength of self-adhesive resin cements to dentin. J. Prosthet. Dent. 2011, 105, 227–235. [Google Scholar] [CrossRef]
- Vaz, R.R.; Hipólito, V.D.; D’Alpino, P.H.; Goes, M.F. Bond strength and interfacial micromorphology of etch-and-rinse and self-adhesive resin cements to dentin. J. Prosthodont. 2012, 21, 101–111. [Google Scholar] [CrossRef]
- Duarte, S., Jr.; Botta, A.C.; Meire, M.; Sadan, A. Microtensil bond strengths and scanning electron microscopic evaluation of self-adhesive and self-etch resin cements so intact and etched enamel. J. Prosthet. Dent. 2008, 10, 203–210. [Google Scholar] [CrossRef]
- Marzec-Gawron, M.; Michalska, S.; Dejak, B. Properties of contemporary resin cements and their adhesion to enamel and dentin. Prosthodontics 2012, LXII, 173–180. [Google Scholar] [CrossRef]
- Kuhn, H.J.; Braslovsky, S.E.; Schmidt, R. Chemical actinometry (IUPAC Technical Report). Pure Appl. Chem. 2004, 76, 2105–2146. [Google Scholar] [CrossRef]
- Karjalainen, S. Gender differences in thermal comfort and use of thermostats in everyday thermal environments. Build. Environ. 2007, 4, 1594–1603. [Google Scholar] [CrossRef]
- Richardson, W.S.; Wilson, M.C.; Nishikawa, J.; Hayward, R.S.A. The well-bulit clinical question: A key to evidence-based decisions. ACP J. Club 1995, 123, A12. [Google Scholar] [CrossRef]
- Nishikawa-Pacher, A. Research Questions with PICO: A Universal Mnemonic. Publications 2022, 10, 21. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamsheer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Ozer, F.; Ovecoglu, H.S.; Deneshmehr, L.; Sinmazisik, G.; Kashyap, K.; Iriboz, E.; Blatz, M.B. Effect of storage temperature on the shelf life of self-adhesive resin cements. J. Adhes. Dent. 2015, 17, 545–550. [Google Scholar] [CrossRef]
- Øllo, G.; Ørstavik, D. The temperature of cement specimens and its influence on measured strength. Dent. Mater. 1985, 1, 71–73. [Google Scholar] [CrossRef] [PubMed]
- Bausch, J.R.; de Lange, C.; Davidson, C.L. The influence of the temperature on some physical properties of dental composites. J. Oral Rehabil. 1981, 8, 309–317. [Google Scholar] [CrossRef]
- Żuławnik, A.; Cierech, M.; Rączkiewicz, M. Effect of temperature increase of composite materials on the quality of adhesive cementation—Review of literature. Prosthodontics 2019, 69, 437–443. [Google Scholar] [CrossRef]
- Naumova, E.A.; Ernst, S.; Schaper, K.; Arnold, W.H.; Piwowarczyk, A. Adhesion of different resin cements to enamel and dentin. Dent. Mater. J. 2016, 35, 345–352. [Google Scholar] [CrossRef]
- Rohr, N.; Fischer, J. Tooth surface treatment strategie for adhesive cementation. J. Adv. Prosthodont. 2017, 9, 85–92. [Google Scholar] [CrossRef]
- Skąpska, A.; Sochacka, A.; Ziopaja, A.; Komorek, Z.; Cierech, M. Comparative analysis of selected mechanical properties of preheated composite material and self-adhesive composite cement—Pilot study. Prosthodontics 2020, 70, 281–288. [Google Scholar] [CrossRef]
- Moldovan, M.; Balazsi, R.; Soanca, A.; Roman, A.; Sarosi, C.; Prodan, D.; Cojocaru, I.; Saceleanu, V.; Cristescu, I. Evaluation of degree of conversion, residual monomers and mechanical properties of some light-cured dental resin composites. Materials 2019, 12, 2109. [Google Scholar] [CrossRef]
- Skąpska, A.; Komorek, Z.; Cierech, M.; Mierzwińska-Nastalska, E. Comparison of mechanical properties of self-adhesive composite cement and heated composite material. Polymers 2022, 14, 2686. [Google Scholar] [CrossRef] [PubMed]
- Deb, S.; Di Silvio, L.; Mackler, H.E.; Millar, B.J. Pre-warming of dental composites. Dent. Mater. 2011, 27, e51–e59. [Google Scholar] [CrossRef] [PubMed]
- Ayub, K.V.; Santos GCIr Rizkalla, A.S.; Bohay, R.; Pegoraro, L.F.; Rubo, J.H.; Santos, M.J. Effect of preheating on microhardness and viscosity of four resin composites. J. Can. Dent. Assoc. 2014, 80, e12. [Google Scholar]
- Mufnoz, C.A.; Bond, P.R.; Sy-Munoz, J.; Tan, D.; Peterson, J. Effect of pre-heating on depth of cure and surface hardness of light polymerized resin composites. Am. J. Dent. 2008, 21, 215–222. [Google Scholar]
- Wagner, W.; Asku, M.; Neme, A.M.L.; Linger, J.B.; Pink, F.E.; Walker, S. Effect of pre-haeting resin composite on restoration microleakage. Oper. Dent. 2008, 33, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.R.; Du, W.; Zhou, X.D.; Yu, H.Y. Review of research on the mechanical properties of the human tooth. Int. J. Oral Sci. 2014, 6, 61–69. [Google Scholar] [CrossRef]
- Morais, A.; Santos, A.; Giannini, M.; Reis, A.F.; Rodrigues, J.A.; Arrais, C.A. Effect of pre-heated dual-cured resin cements on the bond strength of indirect restorations to dentin. Bras. Oral Res. 2012, 26, 170–176. [Google Scholar] [CrossRef]
- Shoja-Assadi, F.T.; Lea, S.C.; Burke, F.J.; Palin, W.M. Extrinsic energy sources affect hardness through depth during set of a glass-ionomer cement. J. Dent. 2010, 38, 490–495. [Google Scholar] [CrossRef]
- Khoroushi, M.; Karvandi, T.M.; Sadeghi, R. Effect of prewarming and/or delayed light activation on resin-modified glass ionomer bond strength to tooth structures. Oper. Dent. 2012, 37, 54–62. [Google Scholar] [CrossRef]
- Gavic, L.; Gorseta, K.; Glavina, D.; Czrnecka, B.; Nicholson, J.W. Heat transfer properties and thermal cure glass-ionomer dental cements. J. Mater. Sci. Mater. Med. 2015, 26, 249. [Google Scholar] [CrossRef]
- El-Deeb, H.A.; Abd El-Azis, S.; Mobarak, E.H. Effect of preheating low shrinking resin composite on intrapulpal temperature and microtensile bond strength to dentin. J. Adv. Res. 2015, 6, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Karacan, A.O.; Ozyurt, P. Effect of preheated bulk-fill composite temperature on intrapulpal temperature increase in vitro. J. Esthet. Restor. Dent. 2019, 31, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Knezevic, A.; Zaljezic, D.; Kopjar, N.; Duarte, S., Jr.; Par, M.; Tarle, Z. Toxicity of pre-heated composites polymerized directly and through CAD/CAM overlay. Acta Stomatol. Croat. 2018, 52, 203–217. [Google Scholar] [CrossRef] [PubMed]
- Gross, D.J.; Davila-Sanchez, A.; Runnacles, P.; Zarpellon, D.C.; Kiratcz, F.; Campagnoli, E.B.; Alegria-Acevedo, L.F.; Coelho, U.; Rueggeberg, F.A.; Arrais, C. In vivo temperature rise and acute inflammatory response in anesthetized human pulp tissue of premolars having Class V preparations after exposure to Polywave® LED light curing inits. Dent. Mater. 2020, 36, 1201–1213. [Google Scholar] [CrossRef]
- Froes-Salgado, N.R.; Silva, L.M.; Kawano, Y.; Francci, C.; Reis, A.; Loguercio, A.D. Composite pre-heating: Effects on marginal adaptation, degree of conversion and mechanical properties. Dent. Mater. 2010, 26, 908–914. [Google Scholar] [CrossRef] [PubMed]
- Daronch, M.; Rueggeberg, F.A.; De Goes, M.F. Monomer conversion of pre-heated composite. J. Dent. Res. 2005, 84, 663–667. [Google Scholar] [CrossRef] [PubMed]
- Daronch, M.; Rueggeberg, F.A.; De Goes, M.F.; Giudici, R. Plymerization kinetics of pre-heated composite. J. Dent. Res. 2006, 85, 38–43. [Google Scholar] [CrossRef]
- Daronch, M.; Rueggeberg, F.A.; Moss, L.; de Goes, M.F. Clinically relevant issues related to preheating composites. J. Esthet. Restor. Dent. 2006, 18, 340–350. [Google Scholar] [CrossRef]
- Blalock, J.S.; Holmes, R.G.; Rueggeberg, F.A. Effect of temperature on unpolymerized composite resin film thickness. J. Prosthet. Dent. 2006, 96, 424–432. [Google Scholar] [CrossRef]
- Daronch, M.; Rueggeberg, F.A.; Hall De Goes, M.F. Effect of composite temperature on in vitro intrapulpal temperature rise. Dent. Mater. 2007, 23, 1283–1288. [Google Scholar] [CrossRef]
- Franca, F.A.; de Oliveira, M.; Rodriges, J.A.; Arrals, C.A. Pre-heated dual-cured resin cements: Analysis of the degree of conversion and ultimate tensile strength. Braz. Oral Res. 2011, 25, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Ruyter, I.E. Methacrylate-based polymeric denetal materials: Conversion and related properties. Summary and review. Acta Odontol. Scan. 1982, 40, 359–376. [Google Scholar] [CrossRef] [PubMed]
- Mileding, P.; Ortengren, U.; Karlsson, S. Ceramic inlay systems: Some clinical aspects. J. Oral Rehabil. 1995, 22, 571–580. [Google Scholar] [CrossRef]
- Ferracane, J.L. Correlation between hardness and degree of conversion during the setting reaction of unfilled dental restorative resins. Dent. Mater. 1985, 1, 11–14. [Google Scholar] [CrossRef]
- Ferracane, J.L.; Berge, H.X.; Condon, J.R. In vitro aging of dental composites in water—Effect of degree of conversion, filler volume, and filler/matrix coupling. J. Biomed. Mater. Res. 1998, 42, 465–472. [Google Scholar] [CrossRef]
- Peutzfeldt, A. Dual-cure resin cements: In vitro wear and effect of quantity of remaining double bonds, filler volume and light curing. Acta Odontol. Scand. 1995, 53, 29–34. [Google Scholar] [CrossRef]
- Goulart, M.; Borges Veleda, B.; Damin, D.; Bovi Ambrosano, G.M.; Coelho de Souza, F.H.; Guilherme Erhardt, M.C. Preheated composite resin used as a luting agent for indirect restorations: Effects on bond strength and resin-dentin interfaces. Int. J. Esthet. Dent. 2018, 13, 86–97. [Google Scholar]
- Mohammadi, M.; Jafari-Navimipour, E.; Kimyai, S.; Ajami, A.A.; Bahari, M.; Ansarin, M. Effect of preheating on the mechanical properties of silorane-based and methacrylate-based composites. J. Clin. Exp. Dent. 2016, 8, e373–e378. [Google Scholar] [CrossRef][Green Version]
- Lucey, S.; Lynch, C.D.; Ray, N.J.; Burke, F.M.; Hannigan, A. Effect of pre-heating on the viscosity and microhardness of a resin composite. J. Oral Rehabil. 2010, 37, 278–282. [Google Scholar] [CrossRef]
- Marcinkowska, A.; Gauza-Włodarczyk, M.; Kubisz, L.; Hędzelek, W. The electrical properties and glass transition of some dental materials after temperature exposure. J. Mater. Sci. Mater. Med. 2017, 28, 186. [Google Scholar] [CrossRef]
- Sharafeddin, F.; Motamedi, M.; Fattah, Z. Effect of preheating and precooling on the flexural strength and modulus of elasticity of nanohybrid and silorane-based composite. J. Dent. 2015, 16, 224–229. [Google Scholar]
- Davari, A.; Daneshkazemi, A.; Behniafar, B.; Sheshmani, M. Effect of pre-heating on microtensile bond, strength of composite resin to dentin. J. Dent. 2014, 11, 569–575. [Google Scholar]
- da Costa, J.; Mcpharlin, R.; Hilton, T.; Ferracane, J. Effect of heat on the flow of commercial composites. Am. J. Dent. 2009, 22, 92–96. [Google Scholar]
- Kramer, M.R.; Edelhoff, D.; Stawarczyk, B. Flexural strength of preheated resin composites and bonding properties to glass-ceramic and dentin. Materials 2016, 9, 83. [Google Scholar] [CrossRef] [PubMed]
- Choudhary, N.; Kamat, S.; Mangala, T.M.; Thomas, M. Effect of pre-heating composite resin on gap formation at three different temperatures. J. Conserv. Dent. 2011, 14, 191–195. [Google Scholar] [CrossRef]
- Jongsma, L.A.; Kleveraan, C.J. Influence of temperature on volumetric shrinkage and constraction stress of dental composites. Dent. Mater. 2015, 31, 721–725. [Google Scholar] [CrossRef]
- Ahn, K.H.; Lim, S.; Kum, K.Y.; Chang, S.W. Effect of preheating on the viscoelastic properties of dental composite under different deformation conditions. Dent. Mater. J. 2015, 34, 702–706. [Google Scholar] [CrossRef]
- Staansbury, J.W. Curing dental resin and composites by photopolymerization. J. Esthet. Dent. 2020, 12, 300–308. [Google Scholar] [CrossRef]
- Cheung, K.C.; Darvell, B.W. Sintering of dental porcelain: Effect of time and temperature on appearance and porosity. Dent. Mater. 2002, 18, 163–173. [Google Scholar] [CrossRef]
- Theobaldo, J.D.; Aguiar, F.H.B.; Pini, N.I.P.; Lima, D.A.N.L.; Liporoni, P.C.S.; Catelan, A. Effect of preheating and light-curing unit on physicochemical properties of a bulk-fill composite. Clin. Cosmet. Investig. Dent. 2017, 16, 39–43. [Google Scholar] [CrossRef]
- El-Korashy, D.I. Post-gel shrinkage strain and degree oh conversion of preheated resin composite cured using different regimens. Oper. Dent. 2010, 35, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Prasanna, N.; Pallavi, R.Y.; Kavitha, S.; Lakshmi Narayanan, L. Degree of conversion and residual stress of preheated and room-temperature composites. Indian J. Dent. Res. 2007, 18, 173–176. [Google Scholar] [CrossRef]
- Silva, J.C.; Rogerio Vieira, R.; Rege, I.C.; Cruz, C.A.; Vaz, L.G.; Estrela, C.; Castro, F.L. Pre-heating mitigates composite degradation. J. Appl. Oral Sci. 2015, 23, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Trujillo, M.; Newman, S.M.; Stansbury, J.W. Use of near-IR to monitor the influence of external heating on dental composite photopolymerization. Dent. Mater. 2004, 20, 766–777. [Google Scholar] [CrossRef] [PubMed]
- da Silva-Junior, M.E.; de Fz, L.R.; Bagnato, V.S.; Tonetto Mr Simoes, F.; Borges, A.H.; Bandeca, M.C.; de Andrade, M.F. Effect of the curing temperature of dental composites evaluated with a fluorescent dye. J. Contemp. Dent. Pract. 2018, 19, 3–12. [Google Scholar] [CrossRef]
- Taubock, T.T.; Tarle, Z.; Marovic, D.; Attin, T. Pre-heating of high-viscosity bulk-fill resin composites: Effects on shrinkage force and monomer conversion. J. Dent. 2015, 43, 1358–1364. [Google Scholar] [CrossRef]
- Behr, M.; Rosentritt, M.; Loher, H.; Kolbeck, C.; Trempler, C.; Stemplinger, B.; Kopzon, V.; Handel, G. Changes of cement properties by mixing errors: The therapeutic range of different cement types. Dent. Mater. 2008, 24, 1187–1193. [Google Scholar] [CrossRef]
- Vrohari, A.D.; Eliades, G.; Hellwig, E.; Wrbas, K.T. Curing efficiency of four self-etching, self adhesive resin cements. Dent. Mater. 2009, 25, 1104–1108. [Google Scholar] [CrossRef]
- Bocci, A.; Dobson, A.; Ferracane, J.L.; Consani, R.; Pfeifer, C.S. Thio-urethanes improve properties of dual-cured composite cements. J. Dent. Res. 2014, 93, 1320–1325. [Google Scholar] [CrossRef]
- Yoon, T.H.; Lee, Y.K.; Lim, B.S.; Kim, C.W. Degree of polymerization of resin composites by different light sources. J. Oral Rehabil. 2002, 29, 1165–1173. [Google Scholar] [CrossRef]
- Silikas, N.; Eliades, G.; Watts, D.C. Light intensity effects on resin-composite degree of conversion and shrinkage strain. Dent. Mater. 2000, 16, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Lohbauer, U.; Rahiotis, C.; Kramer, N.; Petschelt, A.; Eliades, G. The effect of different light-curing units on fatique behavior and degree of conversion of resin composite. Dent. Mater. 2005, 21, 608–615. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).