Development of a Tailored, Complex Intervention for Clinical Reflection and Communication about Suspected Urinary Tract Infections in Nursing Home Residents
Abstract
1. Introduction
2. Results
2.1. Organizational Challenges of Diagnosing UTIs in Nursing Homes
2.2. From the Original Idea to the Final Intervention
2.3. The Dialogue Tool
2.3.1. The Reflection Tool
Early Draft
Barriers to Implementation of the Reflection Tool
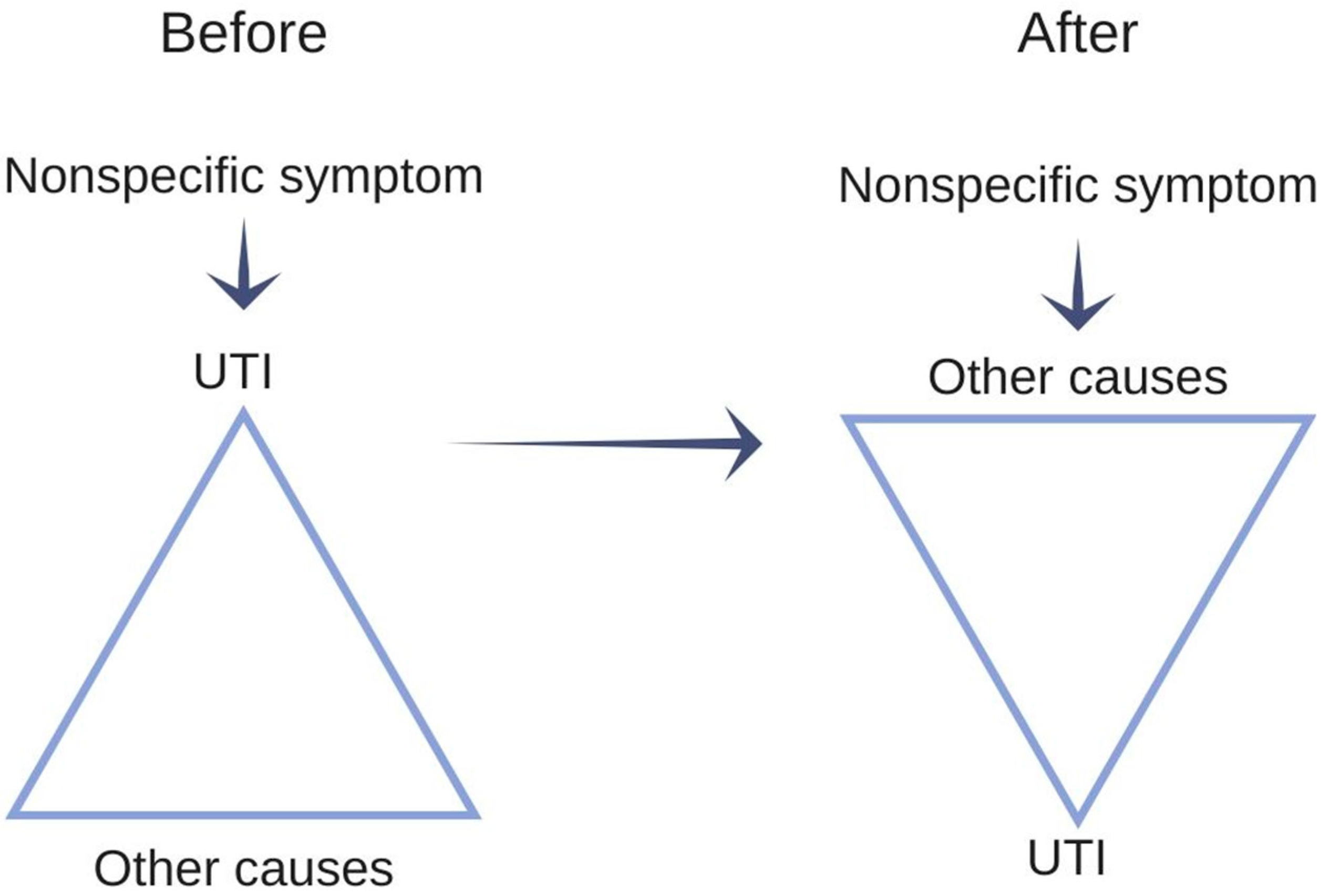
- The Staff’s Intuitive Reasoning Led to Inappropriate Suspicion of UTIs
“But I don’t think you can do that. I don’t think you can… because… no but this is the reason you need to be careful with this… Because they are a little confused, and then you have the lady here, who has foul smelling urine and she has nitrite and leucocytes, so you can’t exclude that there is something there or something coming, and therefore of course I would give her lots of fluids and then observe her and send a (urine sample for, red) culture and resistance, because ehm, she could develop something. Especially, when she is a little more confused than usual. You can’t exclude it you know…”
“Because I wouldn’t say that the symptoms she has are acute. So, I would like to have a space where I could state something like ‘general’ (symptoms, red).”
- Reported Symptoms Were often Known and Insignificant Changes
“Well, we often go on home visits where we think ‘why were we called? There wasn’t anything new here?’”
2.3.2. The Communication Tool
Early Draft
Barriers to Implementation of the Communication Tool
“…We sometimes receive emails, where it says ‘the patient is ill, what should we do?’. And then we would like to, then we would like to go through some stuff, we need to have that specified.”
“…We are quickly influenced by the cause of enquiry… if an experienced nurse calls and tells us a lot of things from this box (points “new onset urinary tract symptoms”, red), well, then we don’t bother so much about this (points to “symptoms from other organs and other findings”, red)”
2.4. The Case-Based Education Session
2.4.1. Content of the Case-Based Education
“And so the urinary dipstick says nitrite and leucocytes and that’s what’s supposed to be there… This is what usually indicates an infection.”
“Here it says significantly confused, and it is very typical for someone who has a UTI that she becomes confused and unsettled, like it says here, right. So that is very… I would say that this is straight by the book, right. But how people respond differs a lot.”
2.4.2. Adjustment to the Case-Based Education Session
3. Discussion
3.1. Discussion of Findings
3.2. Limitations and Strengths
4. Materials and Methods
4.1. The Original Understanding of the Field
4.2. The Planned and Executed Developmental Stages
4.3. Interviews during the Tailoring Process and the Pilot
4.4. Ethical Approval
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ricchizzi, E.; Latour, K.; Kärki, T.; Buttazzi, R.; Jans, B.; Moro, M.L.; Nakitanda, O.A.; Plachouras, D.; Monnet, D.L.; Suetens, C.; et al. Antimicrobial use in european long-term care facilities: Results from the third point prevalence survey of healthcare-associated infections and antimicrobial use, 2016 to 2017. Eurosurveillance 2018, 23. [Google Scholar] [CrossRef] [PubMed]
- van Buul, L.W.; Veenhuizen, R.B.; Achterberg, W.P.; Schellevis, F.G.; Essink, R.T.G.M.; de Greeff, S.C.; Natsch, S.; van der Steen, J.T.; Hertogh, C.M.P.M. Antibiotic prescribing in dutch nursing homes: How appropriate is it? J. Am. Med. Dir. Assoc. 2015, 16, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Daneman, N.; Gruneir, A.; Newman, A.; Fischer, H.D.; Bronskill, S.E.; Rochon, P.A.; Anderson, G.M.; Bell, C.M. Antibiotic use in long-term care facilities. J. Antimicrob. Chemother. 2011, 66, 2856–2863. [Google Scholar] [CrossRef] [PubMed]
- Daneman, N.; Bronskill, S.E.; Gruneir, A.; Newman, A.M.; Fischer, H.D.; Rochon, P.A.; Anderson, G.M.; Bell, C.M. Variability in Antibiotic Use Across Nursing Homes and the Risk of Antibiotic-Related Adverse Outcomes for Individual Residents. JAMA Intern. Med. 2015, 175, 1331–1339. [Google Scholar] [CrossRef]
- Costelloe, C.; Metcalfe, C.; Lovering, A.; Mant, D.; Hay, A.D. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: Systematic review and meta-analysis. BMJ 2010, 340, c2096. [Google Scholar] [CrossRef]
- Gajdács, M. The concept of an ideal antibiotic: Implications for drug design. Molecules 2019, 24, 892. [Google Scholar] [CrossRef]
- Nace, D.A.; Drinka, P.J.; Crnich, C.J. Clinical Uncertainties in the Approach to Long Term Care Residents With Possible Urinary Tract Infection. J. Am. Med. Dir. Assoc. 2014, 15, 133–139. [Google Scholar] [CrossRef]
- D’Agata, E.D.; Loeb, M.B.; Mitchell, S.L. Challenges in assessing nursing home residents with advanced dementia for suspected urinary tract infections. J. Am. Geriatr. Soc. 2013, 61, 62–66. [Google Scholar] [CrossRef]
- Nicolle, L.E.; Gupta, K.; Bradley, S.F.; Colgan, R.; DeMuri, G.P.; Drekonja, D.; Eckert, L.O.; Geerlings, S.E.; Köves, B.; Hooton, T.M.; et al. Clinical practice guideline for the management of asymptomatic bacteriuria: 2019 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2019, 68, E75–E83. [Google Scholar] [CrossRef]
- Mayne, S.; Bowden, A.; Sundvall, P.D.; Gunnarsson, R. The scientific evidence for a potential link between confusion and urinary tract infection in the elderly is still confusing—A systematic literature review. BMC Geriatr. 2019, 19. [Google Scholar] [CrossRef]
- Jorgensen, S.C.J.; Yeung, S.L.; Zurayk, M.; Terry, J.; Dunn, M.; Nieberg, P.; Pallares, J.; Wong-Beringer, A. Leveraging antimicrobial stewardship in the emergency department to improve the quality of urinary tract infection management and outcomes. Open Forum Infect. Dis. 2018, 5, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Zalmanovici Trestioreanu, A.; Lador, A.; Sauerbrun-Cutler, M.-T.; Leibovici, L. Antibiotics for asymptomatic bacteriuria. Cochrane database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Biggel, M.; Heytens, S.; Latour, K.; Bruyndonckx, R.; Goossens, H.; Moons, P. Asymptomatic bacteriuria in older adults: The most fragile women are prone to long-term colonization. BMC Geriatr. 2019, 19, 1–11. [Google Scholar] [CrossRef]
- Ninan, S.; Walton, C.; Barlow, G. Investigation of suspected urinary tract infection in older people. BMJ 2014, 4070, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Kistler, C.E.; Beeber, A.S.; Zimmerman, S.; Ward, K.; Farel, C.E.; Chrzan, K.; Wretman, C.J.; Boynton, M.H.; Pignone, M.; Sloane, P.D. Nursing Home Clinicians’ Decision to Prescribe Antibiotics for a Suspected Urinary Tract Infection: Findings From a Discrete Choice Experiment. J. Am. Med. Dir. Assoc. 2020, 21, 675–682. [Google Scholar] [CrossRef] [PubMed]
- Sundheds- og ældreministeriet. National Undersøgelse af Forholdene på Plejecentre [National Investigation into the Conditions at Nursing Homes]; Sundheds- og ældreministeriet: Copenhagen, Denmark, 2016.
- Central Enhed for Infektionshygiejne. Overvågning af sundhedssektorerhvervede infektioner og antibiotikaaudit på plejehjem HALT 3. [Survailance of Health Sector Acquired Infections and Antibiotics Audit at Nursing Homes HALT 3.]; Central Enhed for Infektionshygiejne: Copenhagen, Denmark, 2018.
- McClean, P.; Tunney, M.; Gilpin, D.; Parsons, C.; Hughes, C. Antimicrobial prescribing in residential homes. J. Antimicrob. Chemother. 2012, 67, 1781–1790. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lim, C.J.; Kwong, M.W.L.; Stuart, R.L.; Buising, K.L.; Deborah Friedman, N.; Bennett, N.J.; Cheng, A.C.; Peleg, A.; Marshall, C.; Kong, D.C.M. Antibiotic prescribing practice in residential aged care facilities - Health care providers’ perspectives. Med. J. Aust. 2014, 201, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Crnich, C.J.; Jump, R.; Trautner, B.; Sloane, P.D.; Mody, L. Optimizing Antibiotic Stewardship in Nursing Homes: A Narrative Review and Recommendations for Improvement. Drugs Aging 2015, 32, 699–716. [Google Scholar] [CrossRef]
- Van Buul, L.W.; Van Der Steen, J.T.; Doncker, S.M.; Achterberg, W.P.; Schellevis, F.G.; Veenhuizen, R.B.; Hertogh, C.M. Factors influencing antibiotic prescribing in long-term care facilities: A qualitative in-depth study. BMC Geriatr. 2014, 14, 1–11. [Google Scholar] [CrossRef]
- Feldstein, D.; Sloane, P.D.; Feltner, C. Antibiotic Stewardship Programs in Nursing Homes: A Systematic Review. J. Am. Med. Dir. Assoc. 2018, 19, 110–116. [Google Scholar] [CrossRef]
- Saha, S.K.; Kong, D.C.M.; Thursky, K.; Mazza, D. A Nationwide Survey of Australian General Practitioners on Antimicrobial Stewardship: Awareness, Uptake, Collaboration with Pharmacists and Improvement Strategies. Antibiotics 2020, 9, 310. [Google Scholar] [CrossRef] [PubMed]
- Raban, M.Z.; Gasparini, C.; Li, L.; Baysari, M.T.; Westbrook, J.I. Effectiveness of interventions targeting antibiotic use in long-term aged care facilities: A systematic review and meta-analysis. BMJ Open 2020, 10. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.; Gillies, C.; Ej, S.; Cheater, F.; Flottorp, S.; Robertson, N.; Wensing, M.; Fiander, M.; Mp, E.; J, V.L.; et al. Tailored interventions to address determinants of practice. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Craig, P.; Dieppe, P.; Macintyre, S.; Mitchie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical research council guidance. BMJ 2008, 337, 979–983. [Google Scholar] [CrossRef]
- Pothier, D.; Monteiro, P.; Mooktiar, M.; Shaw, A. Pilot study to show the loss of important data in nursing handover. Br. J. Nurs. 2005, 14, 1090–1093. [Google Scholar] [CrossRef]
- Bhabra, G.; Mackeith, S.; Monteiro, P.; Pothier, D.D. An experimental comparison of handover methods. Ann. R. Coll. Surg. Engl. 2007, 89, 298–300. [Google Scholar] [CrossRef]
- Loeb, M.; Brazil, K.; Lohfeld, L.; McGeer, A.; Simor, A.; Stevenson, K.; Zoutman, D.; Smith, S.; Liu, X.; Walter, S.D. Effect of a multifaceted intervention on number of antimicrobial prescriptions for suspected urinary tract infections in residents of nursing homes: Cluster randomised controlled trial. BMJ 2005, 331, 669. [Google Scholar] [CrossRef]
- Mcmaughan, D.K.; Nwaiwu, O.; Zhao, H.; Frentzel, E.; Mehr, D.; Imanpour, S.; Garfinkel, S.; Phillips, C.D. Impact of a decision-making aid for suspected urinary tract infections on antibiotic overuse in nursing homes. BMC Geriatr. 2016, 16. [Google Scholar] [CrossRef]
- Ydemann, M. Kommunikation på hospitalet ved hjælp af en standardiseret metode. [Communication in a hospital by means of a standardised method]. Ugeskr. Laeger 2012, 174, 1798–1801. [Google Scholar]
- Arnold, S.H.; Jensen, J.N.; Kousgaard, M.B.; Siersma, V.; Bjerrum, L.; Holm, A. Reducing Antibiotic Prescriptions for Urinary Tract Infection in Nursing Homes Using a Complex Tailored Intervention Targeting Nursing Home Staff: Protocol for a Cluster Randomized Controlled Trial. JMIR Res. Protoc. 2020, 9, e17710. [Google Scholar] [CrossRef]
- van Buul, L.W.; Vreeken, H.L.; Bradley, S.F.; Crnich, C.J.; Drinka, P.J.; Geerlings, S.E.; Jump, R.L.P.; Mody, L.; Mylotte, J.J.; Loeb, M.; et al. The Development of a Decision Tool for the Empiric Treatment of Suspected Urinary Tract Infection in Frail Older Adults: A Delphi Consensus Procedure. J. Am. Med. Dir. Assoc. 2018, 19, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Arinzon, Z.; Peisakh, A.; Shuval, I.; Shabat, S.; Berner, Y.N. Detection of urinary tract infection (UTI) in long-term care setting: Is the multireagent strip an adequate diagnostic tool? Arch. Gerontol. Geriatr. 2009, 48, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Sundvall, P.D.; Elm, M.; Ulleryd, P.; Mölstad, S.; Rodhe, N.; Jonsson, L.; Andersson, B.; Hahn-Zoric, M.; Gunnarsson, R. Interleukin-6 concentrations in the urine and dipstick analyses were related to bacteriuria but not symptoms in the elderly: A cross sectional study of 421 nursing home residents. BMC Geriatr. 2014, 14, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Midthun, S.J.; Paur, R.; Lindseth, G. Urinary tract infections. Does the smell really tell? J. Gerontol. Nurs. 2004, 30, 4–9. [Google Scholar] [CrossRef]
- Heneghan, C.; Spencer, E. Catalogue of Bias. Available online: https://catalogofbias.org/biases/previous-opinion-bias/ (accessed on 13 May 2020).
- Public Health England. Diagnosis of Urinary Tract Infections: Quick Reference Tool for Primary Care for Consultation and Local Adaptation Diagnosis of Urinary Tract Infections: Quick Reference Tool for Primary Care; Public Health England: London, UK, 2019.
- Boockvar, K.S.; Lachs, M.S. Predictive value of nonspecific symptoms for acute illness in nursing home residents. J. Am. Geriatr. Soc. 2003, 51, 1111–1115. [Google Scholar] [CrossRef]
- Hunskår, S. Almen Medicin [Family Medicine], 1st ed.; Bjerrum, L., Maagaard, R., Jensen, M.B., Kristensen, J.K., Jarbøl, D.E., Ertmann, R.K., Rosendal, M., Christensen, K.S., Lange, P., Eds.; Munksgaard: Copenhagen, Denmark, 2014; ISBN 9788762812079. [Google Scholar]
- Kahneman, D. Maps of bounded rationality: A perspective on intuitive judgment and choice. Sveriges Riksbank Prize Econ. Sci. Mem. Alfred Nobel 2002, 106, 1248–1299. [Google Scholar]
- Pelaccia, T.; Tardif, J.; Triby, E.; Charlin, B. An analysis of clinical reasoning through a recent and comprehensive approach: The dual-process theory. Med. Educ. Online 2011, 16, 1–9. [Google Scholar] [CrossRef]
- Festinger, L. A theory of Cognitive Dissonance; Standford University Press: Standford, CA, USA, 1957. [Google Scholar]
- Lipman, T.H.; Deatrick, J.A. Preparing advanced practice nurses for clinical decision making in specialty practice. Nurse Educ. 1997, 22, 47–50. [Google Scholar] [CrossRef]
- Durham, C.O.; Fowler, T.; Kennedy, S. Teaching dual-process diagnostic reasoning to doctor of nursing practice students: Problem-based learning and the illness script. J. Nurs. Educ. 2014, 53, 646–650. [Google Scholar] [CrossRef]
- Grigoryan, L.; Naik, A.D.; Horwitz, D.; Cadena, J.; Patterson, J.E.; Zoorob, R.; Trautner, B.W. Survey finds improvement in cognitive biases that drive overtreatment of asymptomatic bacteriuria after a successful antimicrobial stewardship intervention. Am. J. Infect. Control 2016, 44, 1544–1548. [Google Scholar] [CrossRef]
- Schweizer, A.K.; Hughes, C.M.; Macauley, D.C.; O’Neill, C. Managing urinary tract infections in nursing homes: A qualitative assessment. Pharm. World Sci. 2005, 27, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Healthcare in Denmark; Ministry of Health: Copenhagen, Denmark, 2017.
- Eldridge, S.M.; Lancaster, G.A.; Campbell, M.J.; Thabane, L.; Hopewell, S.; Coleman, C.L.; Bond, C.M. Defining feasibility and pilot studies in preparation for randomised controlled trials: Development of a conceptual framework. PLoS ONE 2016, 11, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Boren, M.T.; Ramey, J. Thinking aloud: Reconciling theory and practice. IEEE Trans. Prof. Commun. 2000, 43, 261–278. [Google Scholar] [CrossRef]


| Components | Original Idea | Final Intervention |
|---|---|---|
| Diagnostic component | Decision aid by Loeb et al. [29] | Reflection (observations of signs and symptoms, flowchart and discussion) |
| Communication component | Communication tool by McMaughan et al. and Ydemann [30,31] | ISBAR (Identification, Situation, Background, Assessment, and Recommendation) |
| POC-test | CRP test | Discarded |
| Educational component | (1) Educational session to introduce decision aid and communication tool to all nursing home staff (2) Educational session to introduce CRP testing to selected staff | Case-based education to introduce dialogue tool and bridge knowledge gaps |
| Developmental Stage | Initial Draft | Tailoring | Nonrandomised Pilot | ||||
|---|---|---|---|---|---|---|---|
| Phases | - | Phase 1 | Phase 2 | Phase 3 | Phase 4 | Phase 5 | - |
| Date | April 2017–May 2018 | June 2018 | June 2018 | June 2018 | July 2018 | July 2018 | September 2018 |
| Method(s) | Literature search Participatory observations Interviews Survey | Focus group interview | Double interview | Double interview | Single interview | Single interview | Two single interviews Four short telephone interviews during the pilot |
| Perspective | All | Nursing home | General practice | Patients and relatives | Nursing home | Nursing home | Nursing home |
| Informants background | Nursing home residents, all groups of nursing home staff, GPs, general practice staff | Three healthcare helpers, two healthcare assistants | One GP, one medical secretary | Two Senior Citizens’ Council Members | One nurse | One nurse | One head nurse, one nurse |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arnold, S.H.; Olesen, J.A.; Jensen, J.N.; Bjerrum, L.; Holm, A.; Kousgaard, M.B. Development of a Tailored, Complex Intervention for Clinical Reflection and Communication about Suspected Urinary Tract Infections in Nursing Home Residents. Antibiotics 2020, 9, 360. https://doi.org/10.3390/antibiotics9060360
Arnold SH, Olesen JA, Jensen JN, Bjerrum L, Holm A, Kousgaard MB. Development of a Tailored, Complex Intervention for Clinical Reflection and Communication about Suspected Urinary Tract Infections in Nursing Home Residents. Antibiotics. 2020; 9(6):360. https://doi.org/10.3390/antibiotics9060360
Chicago/Turabian StyleArnold, Sif H., Julie A. Olesen, Jette N. Jensen, Lars Bjerrum, Anne Holm, and Marius B. Kousgaard. 2020. "Development of a Tailored, Complex Intervention for Clinical Reflection and Communication about Suspected Urinary Tract Infections in Nursing Home Residents" Antibiotics 9, no. 6: 360. https://doi.org/10.3390/antibiotics9060360
APA StyleArnold, S. H., Olesen, J. A., Jensen, J. N., Bjerrum, L., Holm, A., & Kousgaard, M. B. (2020). Development of a Tailored, Complex Intervention for Clinical Reflection and Communication about Suspected Urinary Tract Infections in Nursing Home Residents. Antibiotics, 9(6), 360. https://doi.org/10.3390/antibiotics9060360






