Knowledge, Attitude and Practice of Community Pharmacists Regarding Antibiotic Use and Infectious Diseases: A Cross-Sectional Survey in Hungary (KAPPhA-HU)
Abstract
1. Introduction
2. Results
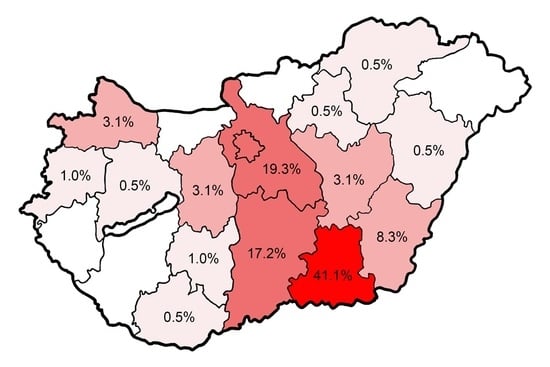
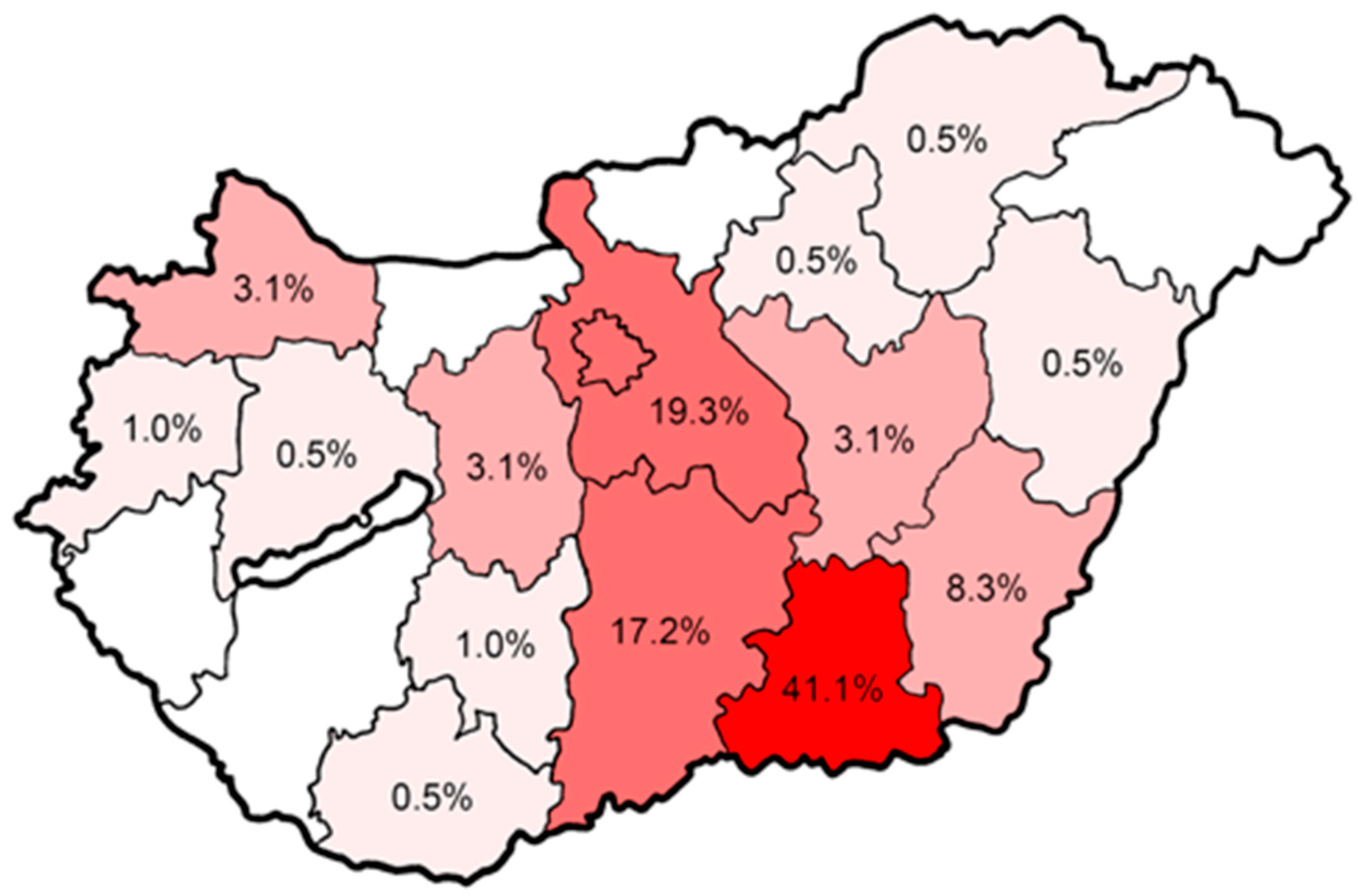
2.1. Demographic Characteristics
2.2. Self-Perceived Knowledge-Level of CPs Regarding ABs and Infectious Diseases
2.3. AB Utilization
2.4. Theoretical Attitude
2.5. Practical Attitude
2.6. Attitude Towards Prevention
2.7. Professional Attitude and Role Expansion
2.8. Correlational Analysis between Self-Perceived Knowledge and Certain Attitudes
3. Discussion
3.1. Knowledge-Level of CPs
3.2. Non-Prescription AB Use
3.3. Role of CPs in Patient Education
3.4. Potential Expansion of Professional Role of Pharmacists
3.5. Influence of Personal and Professional Characteristics
3.6. Limitations of the Study
4. Materials and Methods
4.1. Study Design, Questionnaire
4.2. Data Collection and Statistical Analysis
4.3. Ethical Approval
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gaynes, R. The Discovery of Penicillin—New Insights after More Than 75 Years of Clinical Use. Emerg. Infect. Dis. 2017, 23, 849. [Google Scholar] [CrossRef]
- Aminov, R.I. A Brief History of the Antibiotic Era: Lessons Learned and Challenges for the Future. Front. Microbiol. 2010, 1, 134. [Google Scholar] [CrossRef]
- Exner, M.; Bhattacharya, S.; Christiansen, B.; Gebel, J.; Goroncy-Bermes, P.; Hartemann, P.; Heeg, P.; Ilschner, C.; Kramer, A.; Larson, E.; et al. Antibiotic resistance: What is so special about multidrug-resistant Gram-negative bacteria? GMS Hyg. Infect. Control 2017, 12, Doc05. [Google Scholar] [PubMed]
- Gajdács, M. The Concept of an Ideal Antibiotic: Implications for Drug Design. Molecules 2019, 24, 892. [Google Scholar] [CrossRef] [PubMed]
- Gajdács, M.; Albericio, F. Antibiotic Resistance: From the Bench to Patients. Antibiotics 2019, 8, 129. [Google Scholar] [CrossRef] [PubMed]
- Laxminarayan, R.; Duse, A.; Wattal, C.; Zaidi, A.K.M.; Wertheim, H.F.L.; Sumpradit, N.; Vlieghe, E.; Hara, G.L.; Gould, I.M.; Goossens, H.; et al. Antibiotic resistance-the need for global solutions. Lancet Infect. Dis. 2013, 13, 1057–1098. [Google Scholar] [CrossRef]
- Chang, H.-H.; Cohen, T.; Grad, Y.H.; Hanage, W.P.; O’Brien, T.F.; Lipsitch, M. Origin and proliferation of multiple-drug resistance in bacterial pathogens. Microbiol. Mol. Biol. Rev. 2015, 79, 101–116. [Google Scholar] [CrossRef]
- Shallcross, L.J.; Howard, S.J.; Fowler, T.; Davies, S.C. Tackling the threat of antimicrobial resistance: From policy to sustainable action. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2015, 370, 20140082. [Google Scholar] [CrossRef]
- Boucher, H.W.; Talbot, G.H.; Bradley, J.S.; Edwards, J.E.; Gilbert, D.; Rice, L.B.; Scheld, M.; Spellberg, B.; Bartlett, J. Bad bugs, no drugs: No ESKAPE! An update from the Infectious Diseases Society of America. Clin. Infect. Dis. 2009, 48, 1–12. [Google Scholar] [CrossRef]
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef]
- WHO | Antimicrobial Resistance: No Action Today, No Cure Tomorrow. Available online: https://www.who.int/dg/speeches/2011/WHD_20110407/en/ (accessed on 14 December 2019).
- CDC. The Nation’s Plan to Combat Antibiotic Resistance. Available online: https://www.cdc.gov/drugresistance/us-activities/national-action-plan.html (accessed on 14 December 2019).
- Nahrgang, S.; Nolte, E.; Rechel, B. Antimicrobial Resistance; European Observatory on Health Systems and Policies: Copenhagen, Denmark, 2018. [Google Scholar]
- Pearson, M.; Chandler, C. Knowing antimicrobial resistance in practice: A multi-country qualitative study with human and animal healthcare professionals. Glob. Health Action 2019, 12, 1599560. [Google Scholar] [CrossRef] [PubMed]
- Norris, P.; Chamberlain, K.; Dew, K.; Gabe, J.; Hodgetts, D.; Madden, H. Public Beliefs about Antibiotics, Infection and Resistance: A Qualitative Study. Antibiotics 2013, 2, 465–476. [Google Scholar] [CrossRef] [PubMed]
- Dyar, O.J.; Hills, H.; Seitz, L.-T.; Perry, A.; Ashiru-Oredope, D. Assessing the Knowledge, Attitudes and Behaviors of Human and Animal Health Students towards Antibiotic Use and Resistance: A Pilot Cross-Sectional Study in the UK. Antibiotics 2018, 7, 10. [Google Scholar] [CrossRef] [PubMed]
- Napolitano, F.; Della Polla, G.; De Simone, C.; Lambiase, C.; Pelullo, C.P.; Angelillo, I.F. The Knowledge, Attitudes, and Practices of Community Pharmacists in their Approach to Antibiotic Use: A Nationwide Survey in Italy. Antibiotics 2019, 8, 177. [Google Scholar] [CrossRef] [PubMed]
- Rábano-Blanco, A.; Domínguez-Martís, E.M.; Mosteiro-Miguéns, D.G.; Freire-Garabal, M.; Novío, S. Nursing Students’ Knowledge and Awareness of Antibiotic Use, Resistance and Stewardship: A Descriptive Cross-Sectional Study. Antibiotics 2019, 8, 203. [Google Scholar] [CrossRef]
- Zawahir, S.; Lekamwasam, S.; Aslani, P. Antibiotic dispensing practice in community pharmacies: A simulated client study. Res. Soc. Adm. Pharm. 2019, 15, 584–590. [Google Scholar] [CrossRef]
- Inácio, J.; Barnes, L.-M.; Jeffs, S.; Castanheira, P.; Wiseman, M.; Inácio, S.; Bowler, L.; Lansley, A. Master of Pharmacy students’ knowledge and awareness of antibiotic use, resistance and stewardship. Curr. Pharm. Teach. Learn. 2017, 9, 551–559. [Google Scholar] [CrossRef]
- Jairoun, A.; Hassan, N.; Ali, A.; Jairoun, O.; Shahwan, M. Knowledge, attitude and practice of antibiotic use among university students: A cross sectional study in UAE. BMC Public Health 2019, 19, 518. [Google Scholar] [CrossRef]
- The Role of the Pharmacist in the Health Care System. Available online: https://apps.who.int/medicinedocs/en/d/Jh2995e/ (accessed on 14 December 2019).
- Scarpitta, F.; Restivo, V.; Bono, C.M.; Sannasardo, C.E.; Vella, C.; Ventura, G.; Bono, S.; Palmeri, S.; Caracci, F.; Casuccio, A.; et al. The role of the Community Pharmacist in promoting vaccinations among general population according to the National Vaccination Plan 2017–2019: Results from a survey in Sicily, Italy. Ann. Ig. 2019, 31, 25–35. [Google Scholar]
- The Role of Pharmacist in Encouraging Prudent Use of Antibiotics and Averting Antimicrobial Resistance: A Review of Policy and Experience in Europe. Available online: http://apps.who.int/medicinedocs/en/m/abstract/Js22244en/ (accessed on 14 December 2019).
- The Role of the Pharmacist in Public Health. Available online: https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2014/07/07/13/05/the-role-of-the-pharmacist-in-public-health (accessed on 14 December 2019).
- Horvat, N.; Kos, M. Contribution of Slovenian community pharmacist counseling to patients’ knowledge about their prescription medicines: A cross-sectional study. Croat. Med. J. 2015, 56, 41–49. [Google Scholar] [CrossRef][Green Version]
- Antimicrobial Consumption—Annual Epidemiological Report for 2018. Available online: https://www.ecdc.europa.eu/en/publications-data/surveillance-antimicrobial-consumption-europe-2018 (accessed on 14 December 2019).
- Special Eurobarometer 478: Antimicrobial Resistance (in the EU). Available online: https://data.europa.eu/euodp/en/data/dataset/S2190_90_1_478_ENG (accessed on 14 December 2019).
- Matuz, M.; Benkő, R.; Dóró, P.; Hajdú, E.; Soós, G. Non-prescription antibiotic use in Hungary. Pharm. World Sci. 2007, 29, 695–698. [Google Scholar] [CrossRef]
- Biro, A.; Elek, P. The effect of primary care availability on antibiotic consumption in Hungary: A population based panel study using unfilled general practices. BMJ Open 2019, 13, e028233. [Google Scholar]
- WHO | WHO Competency Framework for Health Workers’ Education and Training on Antimicrobial Resistance. Available online: http://www.who.int/hrh/resources/WHO-HIS-HWF-AMR-2018.1/en/ (accessed on 14 December 2019).
- Survey of Healthcare Workers’ Knowledge, Attitudes and Behaviours on Antibiotics, Antibiotic Use and Antibiotic Resistance in the EU/EEA. Available online: https://www.ecdc.europa.eu/en/publications-data/survey-healthcare-workers-knowledge-attitudes-and-behaviours-antibiotics (accessed on 14 December 2019).
- Roque, F.; Soares, S.; Breitenfeld, L.; Figueiras, A.; Herdeiro, M.T. Influence of Community Pharmacists’ Attitudes on Antibiotic Dispensing Behavior: A Cross-sectional Study in Portugal. Clin. Ther. 2015, 37, 168–177. [Google Scholar] [CrossRef]
- Broom, A.; Broom, J.; Kirby, E.; Plage, S.; Adams, J. What role do pharmacists play in mediating antibiotic use in hospitals? A qualitative study. BMJ Open 2015, 5, e008326. [Google Scholar] [CrossRef]
- Hoxha, I.; Malaj, A.; Kraja, B.; Bino, S.; Oluka, M.; Marković-Peković, V.; Godman, B. Are pharmacists’ good knowledge and awareness on antibiotics taken for granted? The situation in Albania and future implications across countries. J. Glob. Antimicrob. Resist. 2018, 13, 240–245. [Google Scholar] [CrossRef]
- Koji, E.M.; Gebretekle, G.B.; Tekle, T.A. Practice of over-the-counter dispensary of antibiotics for childhood illnesses in Addis Ababa, Ethiopia: A simulated patient encounter study. Antimicrob. Resist. Infect. Control 2019, 8, 119. [Google Scholar] [CrossRef]
- Nafade, V.; Huddart, S.; Sulis, G.; Daftary, A.; Miraj, S.S.; Saravu, K.; Pai, M. Over-the-counter antibiotic dispensing by pharmacies: A standardised patient study in Udupi district, India. BMJ Glob. Health 2019, 4, e001869. [Google Scholar] [CrossRef]
- Alhomoud, F.; Almahasnah, R.; Alhomoud, F.K. “You could lose when you misuse”—Factors affecting over-the-counter sale of antibiotics in community pharmacies in Saudi Arabia: A qualitative study. BMC Health Serv. Res. 2018, 18, 915. [Google Scholar] [CrossRef]
- Vazquez-Lago, J.; Gonzalez-Gonzalez, C.; Zapata-Cachafeiro, M.; Lopez-Vazquez, P.; Taracido, M.; López, A.; Figueiras, A. Knowledge, attitudes, perceptions and habits towards antibiotics dispensed without medical prescription: A qualitative study of Spanish pharmacists. BMJ Open 2017, 7, e015674. [Google Scholar] [CrossRef]
- Llor, C.; Cots, J.M. The sale of antibiotics without prescription in pharmacies in Catalonia, Spain. Clin. Infect. Dis. 2009, 48, 1345–1349. [Google Scholar] [CrossRef]
- Plachouras, D.; Kavatha, D.; Antoniadou, A.; Giannitsioti, E.; Poulakou, G.; Kanellakopoulou, K.; Giamarellou, H. Dispensing of antibiotics without prescription in Greece, 2008: Another link in the antibiotic resistance chain. Eurosurveillance 2010, 15, 19488. [Google Scholar]
- Zapata-Cachafeiro, M.; González-González, C.; Váquez-Lago, J.M.; López-Vázquez, P.; López-Durán, A.; Smyth, E.; Figueiras, A. Determinants of antibiotic dispensing without a medical prescription: A cross-sectional study in the north of Spain. J. Antimicrob. Chemother. 2014, 69, 3156–3160. [Google Scholar] [CrossRef] [PubMed]
- Roque, F.; Soares, S.; Breitenfeld, L.; López-Durán, A.; Figueiras, A.; Herdeiro, M.T. Attitudes of community pharmacists to antibiotic dispensing and microbial resistance: A qualitative study in Portugal. Int. J. Clin. Pharm. 2013, 35, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Ghiga, I.; Stålsby Lundborg, C. ‘Struggling to be a defender of health’—A qualitative study on the pharmacists’ perceptions of their role in antibiotic consumption and antibiotic resistance in Romania. J. Pharm. Policy Pract. 2016, 9, 10. [Google Scholar] [CrossRef]
- Black, E.; Cartwright, A.; Bakharaiba, S.; Al-Mekaty, E.; Alsahan, D. A qualitative study of pharmacists’ perceptions of, and recommendations for improvement of antibiotic use in Qatar. Int. J. Clin. Pharm. 2014, 36, 787–794. [Google Scholar] [CrossRef]
- Chandy, S.J.; Mathai, E.; Thomas, K.; Faruqui, A.R.; Holloway, K.; Lundborg, C.S. Antibiotic use and resistance: Perceptions and ethical challenges among doctors, pharmacists and the public in Vellore, South India. Indian J. Med. Ethics 2013, 10, 20–27. [Google Scholar] [CrossRef]
- Wood, F.; Simpson, S.; Butler, C.C. Socially responsible antibiotic choices in primary care: A qualitative study of GPs’ decisions to prescribe broad-spectrum and fluroquinolone antibiotics. Fam. Pract. 2007, 24, 427–434. [Google Scholar] [CrossRef]
- Gajdács, M.; Szabó, A. Physicians’ opinions towards antibiotic use and resistance in the southeastern region of Hungary (article in Hungarian). Orv. Hetil. 2019. accepted. [Google Scholar]
- Gilchrist, M.; Wade, P.; Ashiru-Oredope, D.; Howard, P.; Sneddon, J.; Whitney, L.; Wickens, H. Antimicrobial Stewardship from Policy to Practice: Experiences from UK Antimicrobial Pharmacists. Infect. Dis. 2015, 4, 51–64. [Google Scholar] [CrossRef]
- Nagy, V.; Sohajda, A.; Hankó, Z. How is the current staffing situation in community pharmacies? (article in Hungarian). Gyógyszerészet 2019, 63, 459–466. [Google Scholar]
- Altiner, A.; Brockmann, S.; Sielk, M.; Wilm, S.; Wegscheider, K.; Abholz, H.-H. Reducing antibiotic prescriptions for acute cough by motivating GPs to change their attitudes to communication and empowering patients: A cluster-randomized intervention study. J. Antimicrob. Chemother. 2007, 60, 638–644. [Google Scholar] [CrossRef]
- Mason, T.; Trochez, C.; Thomas, R.; Babar, M.; Hesso, I.; Kayyali, R. Knowledge and awareness of the general public and perception of pharmacists about antibiotic resistance. BMC Public Health 2018, 18, 711. [Google Scholar] [CrossRef] [PubMed]
- Saramunee, K.; Krska, J.; Mackridge, A.; Richards, J.; Suttajit, S.; Phillips-Howard, P. How to enhance public health service utilization in community pharmacy?: General public and health providers’ perspectives. Res. Soc. Adm. Pharm. 2014, 10, 272–284. [Google Scholar] [CrossRef] [PubMed]
- Eades, C.E.; Ferguson, J.S.; O’Carroll, R.E. Public health in community pharmacy: A systematic review of pharmacist and consumer views. BMC Public Health 2011, 11, 582. [Google Scholar] [CrossRef] [PubMed]
- Lima, S.I.V.C.; Diniz, R.S.; Egito, E.S.T.; Azevedo, P.R.M.; Oliveira, A.G.; Araujo, I.B. Rationality of Antimicrobial Prescriptions in Community Pharmacy Users. PLoS ONE 2015, 10, e0141615. [Google Scholar] [CrossRef]
- Vervloet, M.; Meulepas, M.A.; Cals, J.W.L.; Eimers, M.; van der Hoek, L.S.; van Dijk, L. Reducing antibiotic prescriptions for respiratory tract infections in family practice: Results of a cluster randomized controlled trial evaluating a multifaceted peer-group-based intervention. NPJ Prim. Care Respir. Med. 2016, 26, 15083. [Google Scholar] [CrossRef]
- Fighting Antimicrobial Resistance. The Contribution of Pharmacists. 2015. Available online: http://apps.who.int/medicinedocs/en/m/abstract/Js23317en/ (accessed on 14 December 2019).
- Kay, M.K.; Koelemay, K.G.; Kwan-Gett, T.S.; Cadwell, B.L.; Duchin, J.S. 2009 Pandemic Influenza A Vaccination of Pregnant Women: King County, Washington State, 2009–2010. Am. J. Prev. Med. 2012, 42, S172–S179. [Google Scholar] [CrossRef]
- Alhameed, A.F.; Khansa, S.A.; Hasan, H.; Ismail, S.; Aseeri, M. Bridging the Gap between Theory and Practice; the Active Role of Inpatient Pharmacists in Therapeutic Drug Monitoring. Pharmacy 2019, 7, 20. [Google Scholar] [CrossRef]
- McCullough, A.R.; Rathbone, J.; Parekh, S.; Hoffmann, T.C.; Del Mar, C.B. Not in my backyard: A systematic review of clinicians’ knowledge and beliefs about antibiotic resistance. J. Antimicrob. Chemother. 2015, 70, 2465–2473. [Google Scholar] [CrossRef]
- Liu, C.; Liu, C.; Wang, D.; Zhang, X. Knowledge, Attitudes and Intentions to Prescribe Antibiotics: A Structural Equation Modeling Study of Primary Care Institutions in Hubei, China. Int. J. Environ. Res. Public Health 2019, 16, 2385. [Google Scholar] [CrossRef]
| Characteristics | % (n=) |
|---|---|
| Gender | |
| Female | 69.8% (n = 134) |
| Male | 30.2% (n = 58) |
| Age | |
| 24–35 years | 58.9% (n = 113) |
| 36–50 years | 27.1% (n = 52) |
| over 50 years | 14.0% (n = 27) |
| Board-Certified specializations | |
| No specializations (Pharm.D. only) | 65.6% (n = 126) |
| BCPS (Pharm.D. and specialization) Specializations represented: | 34.4% (n = 66) |
| Pharmacy operation and management | 31.4% (n = 60) |
| Pharmacology, pharmacotherapy | 1.0% (n = 2) |
| Pharmaceutical care | 1.0% (n = 2) |
| Phytotherapy | 1.0% (n = 2) |
| True % (n=) | False % (n=) | Don’t Know/Uncertain % (n=) | |
|---|---|---|---|
| QK1My knowledge regarding the pharmacological aspects of antibiotic therapy are appropriate. | 90.1% (n = 173) | 2.1% (n = 4) | 7.8% (n = 15) |
| QK2My knowledge regarding the pathomechanism and prevention of infectious diseases are appropriate. | 70.8% (n = 136) | 12.5% (n = 24) | 16.7% (n = 32) |
| QK3My knowledge regarding bacterial resistance are appropriate. | 67.2% (n = 129) | 12.0% (n = 23) | 20.8% (n = 40) |
| 0%–5.0% | 9.9% |
| 5.1%–10.0% | 24.5% |
| 10.1%–15.0% | 21.5% |
| 15.1%–20.0% | 19.3% |
| 20.1%–25.0% | 12.5% |
| more than 25.0% | 12.5% |
| Questions Regarding Attitudes and Professional Responsibility (QA) | SD | D | U/DK | A | SA |
|---|---|---|---|---|---|
| Disagree | Agree | ||||
| Theoretical attitude | |||||
| QTA3I agree with the current funding policy of the National Institute of Health Insurance Fund Management regarding antibiotics (detailed in Decree No.32/2004 (IV.26.) Regulation by Ministry of Health, Social and Family Affairs about health insurance supported pharmaceuticals and the amount of subsidy). | 2.1% (n = 4) | 21.9% (n = 42) | 28.6% (n = 55) | 44.3% (n = 85) | 3.1% (n = 6) |
| QTA4Antibiotics are medicines of special importance. | 2.1% (n = 4) | 3.6% (n = 7) | 0.5% (n = 1) | 45.3% (n = 87) | 48.4% (n = 93) |
| QTA5I may be held responsible for the non-prescription dispensing of antibiotics, as this is a public health risk. | 0.5% (n = 1) | 12.5% (n = 24) | 2.1% (n = 4) | 43.8% (n = 84) | 41.1% (n = 79) |
| QTA6Inappropriate antibiotic therapy does not cause significant surplus health costs on an annual basis. | 41.1% (n = 79) | 35.9% (n = 69) | 4.2% (n = 8) | 12.5% (n = 24) | 6.3% (n = 12) |
| QTA7Education regarding antibiotics and antibiotic resistance should be more prominent during university training. | 1.0% (n = 2) | 5.2% (n = 10) | 1.0% (n = 2) | 35.9% (n = 69) | 56.8% (n = 109) |
| QTA8The use of antibiotics in animal husbandry as growth promoters is just as important (or more important) in the development of bacterial resistance as their inappropriate prescription/consumption in health care. | 0% (n = 0) | 8.3% (n = 16) | 12.5% (n = 24) | 40.6% (n = 78) | 38.5% (n = 74) |
| QTA9I consider it important to become acquainted with the antibiotics of the current drug pool and those newly licensed on the market. | 0% (n = 0) | 5.2% (n = 10) | 1.0% (n = 2) | 31.3% (n = 60) | 62.5% (n = 120) |
| Practical attitude | |||||
| QPA2Patients are mostly receptive of my advice during dispensing, they welcome it. | 3.1% (n = 6) | 12.5% (n = 24) | 5.2% (n = 10) | 64.1% (n = 123) | 15.1% (n = 29) |
| QPA3For patients requesting antibiotics without a prescription and are probably not in need of antibiotic therapy, I feel obligated to inform and educate them. | 0% (n = 0) | 12.0% (n = 23) | 2.6% (n = 5) | 53.1% (n = 102) | 32.3% (n = 62) |
| QPA4There are several occasions when more time is needed to educate patients because doctors have not done this properly. | 0% (n = 0) | 6.3% (n = 12) | 7.8% (n = 15) | 52.6% (n = 101) | 33.3% (n = 64) |
| QPA5The personality and behavior of patients significantly influences my dispensing practices. | 17.2% (n = 33) | 34.4% (n = 66) | 4.7% (n = 9) | 29.2% (n = 56) | 14.6% (n = 28) |
| QPA6I offer probiotics for the patients purchasing a prescribed antibiotic. | 0% (n = 0) | 7.3% (n = 14) | 0.5% (n = 1) | 46.4% (n = 89) | 45.8% (n = 88) |
| QPA7I detail the proper use of antibiotics when counselling the patient. | 0% (n = 0) | 2.0% (n = 4) | 0% (n = 0) | 36.5% (n = 70) | 61.5% (n = 118) |
| Preventive attitude | |||||
| QPrA1The media devotes enough energy to disseminate information on infectious diseases. | 37.0% (n = 71) | 51.6% (n = 99) | 2.6% (n = 5) | 8.9% (n = 17) | 0% (n = 0) |
| QPrA2Appropriate patient education would effectively reduce the incidence of infectious diseases. | 0% (n = 0) | 6.3% (n = 12) | 1.6% (n = 3) | 56.8% (n = 109) | 35.4% (n = 68) |
| QPrA3As I am in direct contact with patients on a daily basis, I have the opportunity to influence their approach to infectious diseases. | 0.5% (n = 1) | 6.3% (n = 12) | 1.6% (n = 3) | 65.6% (n = 126) | 26.0% (n = 50) |
| QPrA4During my work as a pharmacist, I not only have to make therapeutic decisions about acute infection, but I also have to provide lifestyle advice to the patient. | 0% (n = 0) | 2.6% (n = 5) | 4.7% (n = 9) | 53.1% (n = 102) | 39.6% (n = 76) |
| QPrA5Proper use of antibiotics would be greater if pharmacists had time to perform their pharmacological care duties. | 0.5% (n = 1) | 15.6% (n = 30) | 4.7% (n = 9) | 53.1% (n = 102) | 26.0% (n = 50) |
| Professional attitude | |||||
| QPh1Pharmacists should be authorized to perform the task of selecting the therapy in case of proven uncomplicated infections. | 8.3% (n = 16) | 33.9% (n = 65) | 4.2% (n = 8) | 39.1% (n = 75) | 14.6% (n = 28) |
| QPh2After appropriate training, pharmacists could also perform the task of administering vaccines. | 21.4% (n = 41) | 32.8% (n = 63) | 6.3% (n = 12) | 30.2% (n = 58) | 9.4% (n = 18) |
| QPh3Medicine-related counseling of community pharmacists is just as important as the physician’s recommendations. | 2.6% (n = 5) | 4.2% (n = 8) | 0% (n = 0) | 33.9% (n = 65) | 59.4% (n = 114) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gajdács, M.; Paulik, E.; Szabó, A. Knowledge, Attitude and Practice of Community Pharmacists Regarding Antibiotic Use and Infectious Diseases: A Cross-Sectional Survey in Hungary (KAPPhA-HU). Antibiotics 2020, 9, 41. https://doi.org/10.3390/antibiotics9020041
Gajdács M, Paulik E, Szabó A. Knowledge, Attitude and Practice of Community Pharmacists Regarding Antibiotic Use and Infectious Diseases: A Cross-Sectional Survey in Hungary (KAPPhA-HU). Antibiotics. 2020; 9(2):41. https://doi.org/10.3390/antibiotics9020041
Chicago/Turabian StyleGajdács, Márió, Edit Paulik, and Andrea Szabó. 2020. "Knowledge, Attitude and Practice of Community Pharmacists Regarding Antibiotic Use and Infectious Diseases: A Cross-Sectional Survey in Hungary (KAPPhA-HU)" Antibiotics 9, no. 2: 41. https://doi.org/10.3390/antibiotics9020041
APA StyleGajdács, M., Paulik, E., & Szabó, A. (2020). Knowledge, Attitude and Practice of Community Pharmacists Regarding Antibiotic Use and Infectious Diseases: A Cross-Sectional Survey in Hungary (KAPPhA-HU). Antibiotics, 9(2), 41. https://doi.org/10.3390/antibiotics9020041