Efficacy of Daptomycin-Containing Regimen for Treatment of Staphylococcal or Enterococcal Vertebral Osteomyelitis: A Prospective Clinical Experience
Abstract
1. Introduction
2. Results
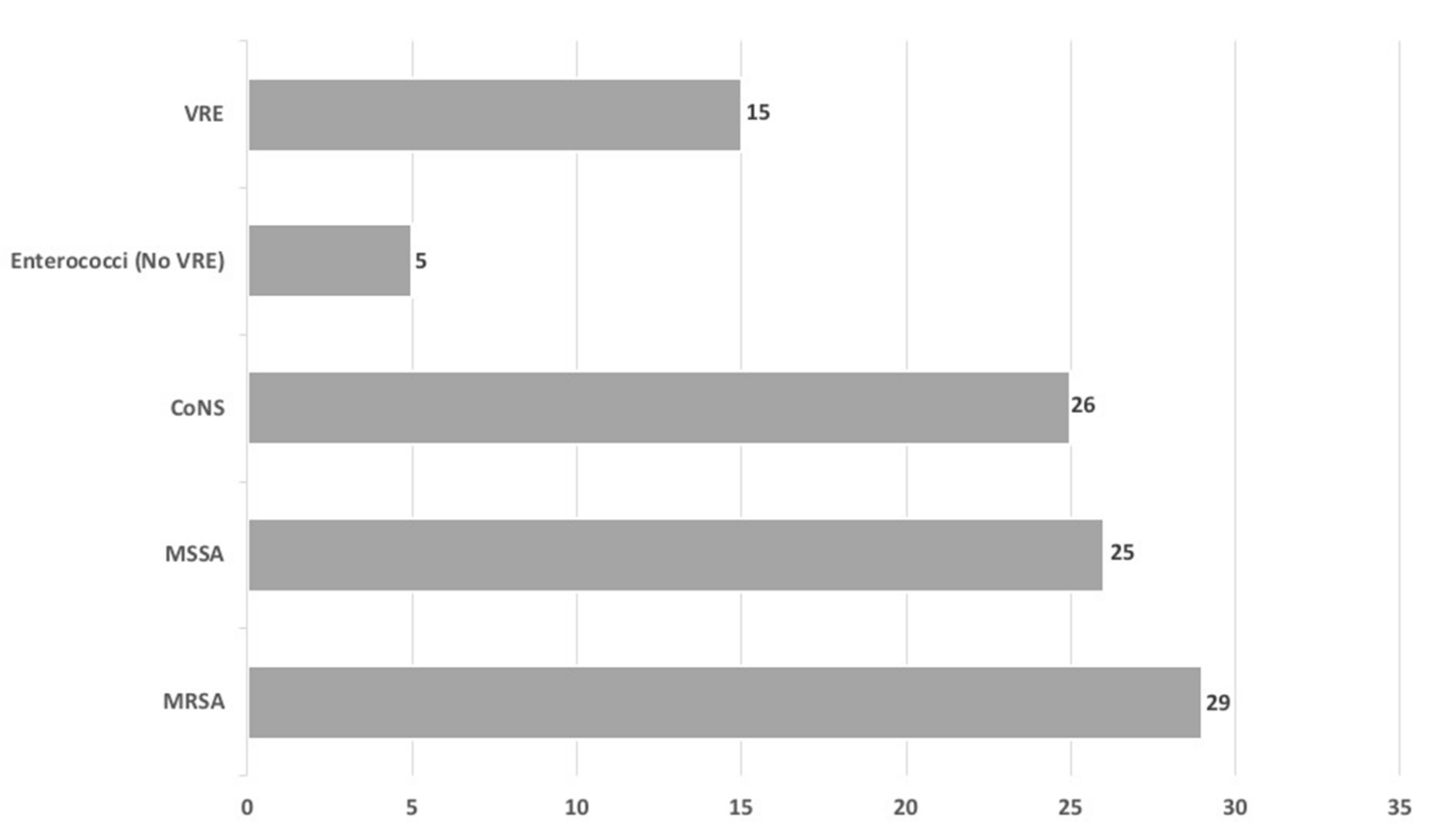
2.1. Baseline Characteristic and Etiology of VO
2.2. Comparison between Patients with Clinical Cure or Failure during Study Period
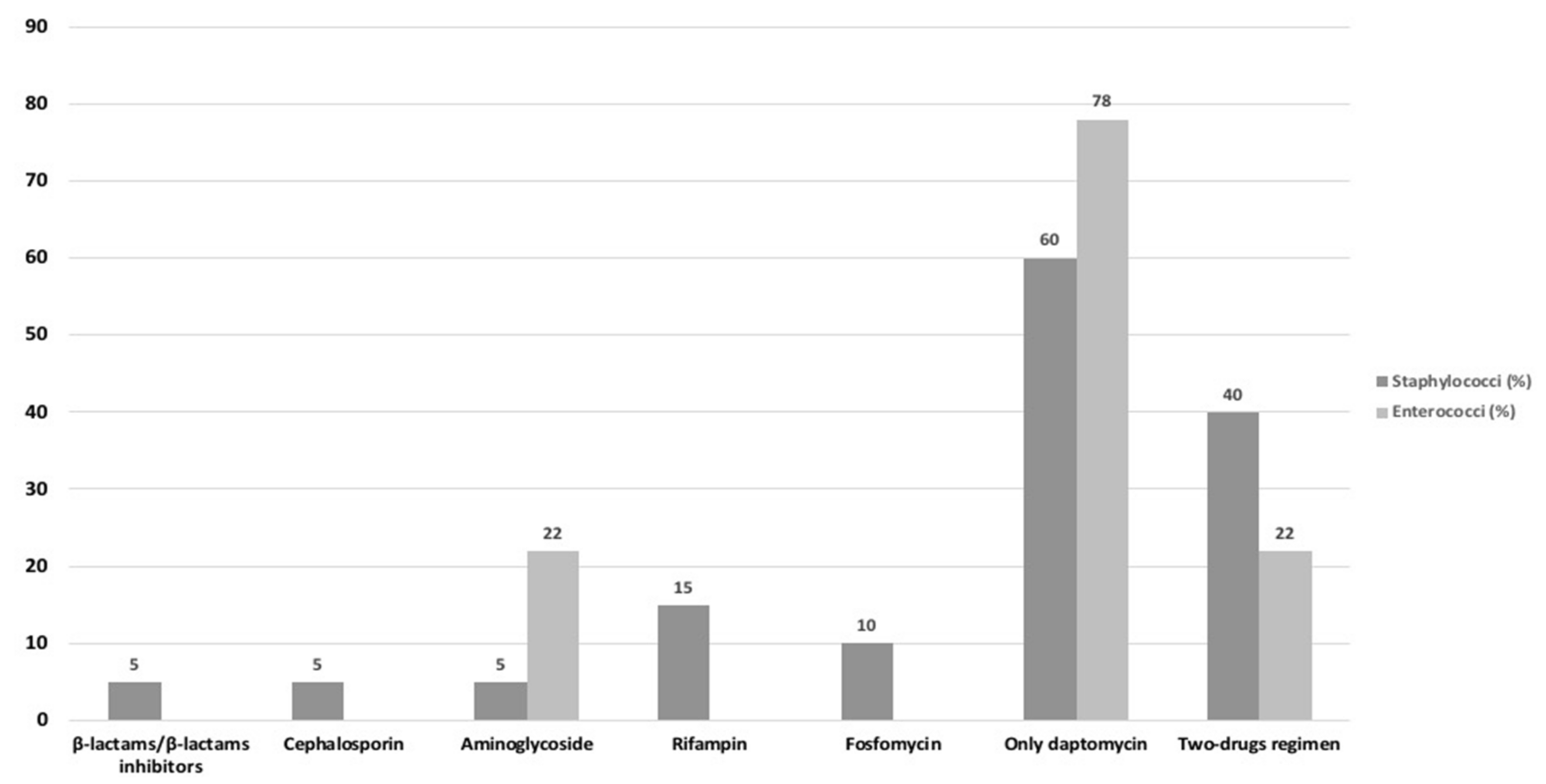
2.3. Comparison between Antibiotic Regimens Used in Definitive Therapy
2.4. Variables Independently Associated with Clinical Failure or Cure
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. Data Collection and Definitions
4.3. Microbiological Identification
4.4. Antimicrobial Treatment Evaluation
4.5. Primary Endpoints and Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chew, F.S.; Kline, M.J. Diagnostic yield of CT-guided percutaneous aspiration procedures in suspected spontaneous infectious diskitis. Radiology 2001, 218, 211–214. [Google Scholar] [CrossRef] [PubMed]
- Zimmerli, W. Clinical practice. Vertebral osteomyelitis. N. Engl. J. Med. 2010, 362, 1022–1029. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Kowalski, T.J.; Osmon, D.R.; Enzler, M.; Steckelberg, J.M.; Huddleston, P.M.; Nassr, A.; Mandrekar, J.M.; Berbari, E.F. Long-term outcome of pyogenic vertebral osteomyelitis: A cohort study of 260 patients. Open Forum Infect. Dis. 2014, 1, 8. [Google Scholar] [CrossRef] [PubMed]
- Berbari, E.F.; Kanj, S.S.; Kowalski, T.J.; Darouiche, R.O.; Widmer, A.F.; Schmitt, S.K.; Hendershot, E.F.; Holtom, P.D.; Huddleston, P.M.; Petermann, G.W.; et al. 2015 Infectious Diseases Society of America (IDSA) clinical practice guidelines for the diagnosis and treatment of native vertebral osteomyelitis in adults. Clin. Infect. Dis. 2015, 61, e26–e46. [Google Scholar] [CrossRef]
- Ohtori, S.; Suzuki, M.; Koshi, T.; Yamashita, M.; Yamauchi, K.; Inoue, G.; Orita, S.; Eguchi, Y.; Kuniyoshi, K.; Ochiai, N.; et al. 18F-Fluorodeoxyglucose-PET for Patients with Suspected Spondylitis Showing Modic Change. Spine 2010, 35, E1599–E1603. [Google Scholar] [CrossRef]
- Hungenbach, S.; Delank, K.-S.; Dietlein, M.; Eysel, P.; Drzezga, A.; Schmidt, M.C. 18F-fluorodeoxyglucose uptake pattern in patients with suspected spondylodiscitis. Nucl. Med. Commun. 2013, 34, 1068–1074. [Google Scholar] [CrossRef]
- Russo, A.; Graziano, E.; Carnelutti, A.; Sponza, M.; Cadeo, B.; Sartor, A.; Righi, E.; Bassetti, M. Management of vertebral osteomyelitis over an eight-year period: The UDIPROVE (UDIne PROtocol on VErtebral osteomyelitis). Int. J. Infect. Dis. 2019, 89, 116–121. [Google Scholar] [CrossRef]
- Thabit, A.K.; Fatani, D.F.; Bamakhrama, M.S.; Barnawi, O.A.; Basudan, L.O.; Alhejaili, S.F. Antibiotic penetration into bone and joints: An updated review. Int. J. Infect. Dis. 2019, 81, 128–136. [Google Scholar] [CrossRef]
- Li, H.-K.; Rombach, I.; Zambellas, R.; Walker, A.S.; McNally, M.A.; Atkins, B.L.; Lipsky, B.A.; Hughes, H.C.; Bose, D.; Kümin, M.; et al. Oral versus Intravenous Antibiotics for Bone and Joint Infection. N. Engl. J. Med. 2019, 380, 425–436. [Google Scholar] [CrossRef]
- Bhavan, K.P.; Marschall, J.; Olsen, M.A.; Fraser, V.J.; Wright, N.M.; Warren, D.K. The epidemiology of hematogenous vertebral osteomyelitis: A cohort study in a tertiary care hospital. BMC Infect. Dis. 2010, 10, 158. [Google Scholar] [CrossRef]
- Saeed, K.; Esposito, S.; Ascione, T.; Bassetti, M.; Bonnet, E.; Carnelutti, A.; Chan, M.; Lye, D.C.B.; Cortes, N.; Dryden, M.; et al. Hot Topics on Vertebral Osteomyelitis from the International Society of Antimicrobial Chemotherapy. Int. J. Antimicrob. Agents 2019, 54, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Rissing, J.P. Antimicrobial Therapy for Chronic Osteomyelitis in Adults: Role of the Quinolones. Clin. Infect. Dis. 1997, 25, 1327–1333. [Google Scholar] [CrossRef] [PubMed]
- Valancius, K.; Hansen, E.S.; Høy, K.; Helmig, P.; Niedermann, B.; Bünger, C. Failure modes in conservative and surgical management of infectious spondylodiscitis. Eur. Spine J. 2012, 22, 1837–1844. [Google Scholar] [CrossRef] [PubMed]
- Livorsi, D.J.; Daver, N.G.; Atmar, R.L.; Shelburne, S.A.; White, A.C.; Musher, D.M. Outcomes of treatment for hematogenous Staphylococcus aureus vertebral osteomyelitis in the MRSA ERA. J. Infect. 2008, 57, 128–131. [Google Scholar] [CrossRef]
- Kowalski, T.J.; Layton, K.F.; Berbari, E.F.; Steckelberg, J.M.; Huddleston, P.M.; Wald, J.T.; Osmon, D.R. Follow-up MR imaging in patients with pyogenic spine infections: Lack of correlation with clinical features. Am. J. Neuroradiol. 2007, 28, 693–699. [Google Scholar]
- Zarrouk, V.; Feydy, A.; Salles, F.; Dufour, V.; Guigui, P.; Redondo, A.; Fantin, B. Imaging does not predict the clinical outcome of bacterial vertebral osteomyelitis. Rheumatology 2006, 46, 292–295. [Google Scholar] [CrossRef]
- Carragee, E.J. The Clinical Use of Magnetic Resonance Imaging in Pyogenic Vertebral Osteomyelitis. Spine 1997, 22, 780–785. [Google Scholar] [CrossRef]
- Nanni, C.; Boriani, L.; Salvadori, C.; Zamparini, E.; Rorato, G.; Ambrosini, V.; Gasbarrini, A.; Tumietto, F.; Cristini, F.; Scudeller, L.; et al. FDG PET/CT is useful for the interim evaluation of response to therapy in patients affected by haematogenous spondylodiscitis. Eur. J. Nucl. Med. Mol. Imaging 2012, 39, 1538–1544. [Google Scholar] [CrossRef]
- Kim, S.-J.; Kim, I.-J.; Suh, K.T.; Kim, Y.-K.; Lee, J.S. Prediction of Residual Disease of Spine Infection Using F-18 FDG PET/CT. Spine 2009, 34, 2424–2430. [Google Scholar] [CrossRef]
- Lalani, T.; Boucher, H.W.; Cosgrove, S.E.; Fowler, V.G.; Kanafani, Z.A.; Vigliani, G.A.; Campion, M.; Abrutyn, E.; Levine, D.P.; Price, C.S.; et al. Outcomes with daptomycin versus standard therapy for osteoarticular infections associated with Staphylococcus aureus bacteraemia. J. Antimicrob. Chemother. 2008, 61, 177–182. [Google Scholar] [CrossRef]
- Moenster, R.P.; Linneman, T.W.; Finnegan, P.M.; McDonald, J.R. Daptomycin Compared to Vancomycin for the Treatment of Osteomyelitis: A Single-Center, Retrospective Cohort Study. Clin. Ther. 2012, 34, 1521–1527. [Google Scholar] [CrossRef] [PubMed]
- Rangaraj, G.; Cleveland, K.O.; Gelfand, M.S. Comparative Analysis of Daptomycin and Vancomycin in the Treatment of Vertebral Osteomyelitis. Infect. Dis. Clin. Pract. 2013, 22, 219–222. [Google Scholar] [CrossRef]
- Falcone, M.; Russo, A.; Pompeo, M.E.; Vena, A.; Marruncheddu, L.; Ciccaglioni, A.; Grossi, P.; Mancini, C.; Novelli, A.; Stefani, S.; et al. Retrospective case–control analysis of patients with staphylococcal infections receiving daptomycin or glycopeptide therapy. Int. J. Antimicrob. Agents 2012, 39, 64–68. [Google Scholar] [CrossRef] [PubMed]
- Kullar, R.; Davis, S.L.; Levine, D.P.; Rybak, M.J. Impact of Vancomycin Exposure on Outcomes in Patients With Methicillin-Resistant Staphylococcus aureus Bacteremia: Support for Consensus Guidelines Suggested Targets. Clin. Infect. Dis. 2011, 52, 975–981. [Google Scholar] [CrossRef] [PubMed]
- Leite, B.; Gomes, F.; Teixeira, P. In vitro activity of daptomycin, linezolid and rifampin on Staphylococcus epidermidis biofilms. Curr. Microbiol. 2011, 63, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Russo, A.; Peghin, M.; Givone, F.; Ingani, M.; Graziano, E.; Bassetti, M. Daptomycin-containing regimens for treatment of Gram-positive endocarditis. Int. J. Antimicrob. Agents 2019, 54, 423–434. [Google Scholar] [CrossRef] [PubMed]
- Peghin, M.; Russo, A.; Givone, F.; Ingani, M.; Graziano, E.; Bassetti, M. Should High-dose Daptomycin be an Alternative Treatment Regimen for Enterococcal Endocarditis? Infect. Dis. Ther. 2019, 8, 695–702. [Google Scholar] [CrossRef] [PubMed]
- Falcone, M.; Russo, A.; Venditti, M.; Novelli, A.; Pai, M.P. Considerations for Higher Doses of Daptomycin in Critically Ill Patients with Methicillin-Resistant Staphylococcus aureus Bacteremia. Clin. Infect. Dis. 2013, 57, 1568–1576. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Flamm, R.K.; Castanheira, M.; Sader, H.S.; Mendes, R.E. Dalbavancin in-vitro activity obtained against Gram-positive clinical isolates causing bone and joint infections in US and European hospitals (2011–2016). Int. J. Antimicrob. Agents 2018, 51, 608–611. [Google Scholar] [CrossRef]
- Pai, M.P.; Russo, A.; Novelli, A.; Venditti, M.; Falcone, M. Simplified Equations Using Two Concentrations to Calculate Area under the Curve for Antimicrobials with Concentration-Dependent Pharmacodynamics: Daptomycin as a Motivating Example. Antimicrob. Agents Chemother. 2014, 58, 3162–3167. [Google Scholar] [CrossRef]
- Falcone, M.; Russo, A.; Cassetta, M.I.; Lappa, A.; Tritapepe, L.; D’Ettorre, G.; Fallani, S.; Novelli, A.; Venditti, M. Variability of pharmacokinetic parameters in patients receiving different dosages of daptomycin: Is therapeutic drug monitoring necessary? J. Infect. Chemother. 2013, 19, 732–739. [Google Scholar] [CrossRef] [PubMed]
- Falcone, M.; Russo, A.; Cassetta, M.I.; Lappa, A.; Tritapepe, L.; Fallani, S.; Vullo, V.; Venditti, M.; Novelli, A. Daptomycin serum levels in critical patients undergoing continuous renal replacement. J. Chemother. 2012, 24, 253–256. [Google Scholar] [CrossRef] [PubMed]
- Montange, D.; Berthier, F.; Leclerc, G.; Serre, A.; Jeunet, L.; Berard, M.; Muret, P.; Vettoretti, L.; Leroy, J.; Hoen, B.; et al. Penetration of Daptomycin into Bone and Synovial Fluid in Joint Replacement. Antimicrob. Agents Chemother. 2014, 58, 3991–3996. [Google Scholar] [CrossRef] [PubMed]
- European Committee on Antimicrobial Susceptibility Testing (EUCAST). 2020. Available online: http://www.eucast.org/clinical_breakpoints (accessed on 6 July 2020).
- Grasso, G.; Gregori, F.; Iaiani, G.; Marotta, N.; Torregrossa, F.; Landi, A. Treatment algorithm for spontaneous spinal infections: A review of the literature. J. Craniovertebral Junction Spine 2019, 10, 3–9. [Google Scholar] [CrossRef] [PubMed]
| Variables | All Population n = 60 (%) | Clinical Cure n = 49 (%) | Clinical Failure n = 11 (%) | p |
|---|---|---|---|---|
| Age, mean ± SD (years) | 65.2 ± 19.9 | 66.4 ± 20.7 | 64.9 ± 19.4 | 0.654 |
| Male sex | 39 (65) | 31 (63.2) | 8 (72.7) | 0.713 |
| Charlson Comorbidity Index, mean ± SD | 2.2 ± 1.9 | 2.2 ± 1.8 | 2 ± 1.9 | 1.0 |
| Previous spinal surgery | 35 (58.3) | 31 (63.2) | 4 (36.3) | 0.1 |
| Previous antimicrobial therapy (30 days) | 41 (68.3) | 30 (61.2) | 11 (100) | 0.011 |
| 14-day antimicrobial treatment discontinuation before vertebral biopsy | 35 (58.3) | 25 (51) | 10 (90.9) | 0.018 |
| >2 vertebrae involved | 42 (70) | 31 (63.2) | 11 (100) | 0.024 |
| Endocarditis | 5 (8.3) | 4 (8.1) | 1 (9.1) | 1.0 |
| Other localization of infection | 11 (18.3) | 7 (14.2) | 4 (36.3) | 0.1 |
| Biopsy/drainage performed | 42 (70) | 37 (75.5) | 5 (45.4) | 0.07 |
| Blood culture positivity | 35 (58.3) | 28 (57.1) | 7 (63.6) | 0.748 |
| CRP concentration (mg/L), mean ± SD | 76.2 ± 41.5 | 77.3 ± 40.2 | 74.9 ± 44.9 | 0.098 |
| WBC concentration (109/L), mean ± SD | 9.7 ± 5.9 | 9.9 ± 6.2 | 9.2 ± 5.2 | 0.787 |
| Inadequate source control of infection | 5 (8.3) | 0 | 5 (45.4) | <0.001 |
| Time to biopsy, mean ± SD (days) | 4.6 ± 2.8 | 3.8 ± 3.3 | 5.9 ± 2.6 | 0.019 |
| Length of hospitalization, mean ± SD (days) | 36.5 ± 13.8 | 35.8 ± 14.5 | 39.7 ± 11.8 | 0.032 |
| Use of FDG-PET/CT | 4 (6.6) | 3 (6.1) | 1 (9.1) | 0.565 |
| Antibiotic Therapy * | Clinical Cure n = 49 (%) | Clinical Failure n = 11 (%) | p |
|---|---|---|---|
| Use of only 1 antibiotic | 25 (51) | 7 (63.6) | 0.518 |
| Use of 2 antibiotics in combination | 22 (44.9) | 4 (36.3) | 0.741 |
| Use of 3 antibiotics in combination | 2 (4.1) | 0 | 1.0 |
| Daptomycin-containing regimen | 23 (46.9) | 0 | 0.004 |
| Vancomycin-containing regimen | 12 (24.4) | 7 (63.6) | 0.07 |
| Teicoplanin-containing regimen | 4 (8.1) | 1 (9.1) | 1.0 |
| β-lactams-containing regimen | 5 (10.2) | 2 (18.2) | 0.601 |
| Fosfomycin-containing regimen | 4 (8.1) | 0 | 1.0 |
| Quinolones-containing regimen | 5 (10.2) | 4 (36.3) | 0.049 |
| Dalbavancin-containing regimen | 3 (6.1) | 0 | 1.0 |
| Linezolid-containing regimen | 2 (4.1) | 1 (9.1) | 0.461 |
| Rifampin-containing regimen | 6 (12.2) | 3 (27.2) | 0.344 |
| Length of definitive antibiotic therapy, mean ± SD (days) | 38.3 ±12.9 | 44.9 ± 23.1 | <0.001 |
| Time to initial definitive therapy, mean ± SD (days) | 8.9 ± 5.2 | 10.9 ± 4.9 | 0.091 |
| Time to oral therapy, mean ± SD (days) | 21.9 ± 8.3 | 41.9 ± 19.3 | <0.001 |
| Variables | Other Antibiotic Regimens n = 37 (%) | Daptomycin-Containing Regimen n = 23 (%) | p |
|---|---|---|---|
| Age, mean ± SD (years) | 65 ± 17.5 | 63.9 ± 18.4 | 0.324 |
| Male sex | 22 (59.4) | 17 (73.9) | 0.281 |
| Charlson Comorbidity Index, mean ± SD | 2.3 ± 1.8 | 2.2 ± 1.9 | 1.0 |
| Previous spinal surgery | 19 (51.3) | 16 (69.5) | 0.188 |
| Previous antimicrobial therapy (30 days) | 21 (56.7) | 20 (86.9) | 0.021 |
| 14-day antimicrobial treatment discontinuation before vertebral biopsy | 20 (54) | 15 (65.2) | 0.431 |
| >2 vertebrae involved | 20 (54) | 22 (95.6) | <0.001 |
| Endocarditis | 3 (8.1) | 2 (8.7) | 1.0 |
| Other localization of infection | 4 (10.8) | 7 (30.4) | 0.086 |
| Biopsy/drainage performed | 23 (62.1) | 19 (82.6) | 0.147 |
| Blood culture positivity | 19 (51.3) | 16 (69.5) | 0.188 |
| CRP concentration (mg/L), mean ± SD | 77.4 ± 39.5 | 76. 8 ± 37.8 | 1.0 |
| WBC concentration (109/L), mean ± SD | 9.3 ± 5.8 | 9.8 ± 4.9 | 0.876 |
| Inadequate source control of infection | 1 (2.7) | 4 (17.4) | 0.066 |
| Time to biopsy, mean ± SD (days) | 5.1 ± 3.1 | 4.2 ± 3.8 | 0.234 |
| Length of hospitalization, mean ± SD (days) | 42.4 ± 23.8 | 28.4 ± 13.9 | <0.001 |
| Use of FDG-PET/CT | 3 (8.1) | 1 (4.3) | 1.0 |
| Clinical failure | 11 (29.7) | 0 | 0.004 |
| 30-day mortality | 2 (5.4) | 0 | 0.519 |
| Variables | OR | CI 95% | p | OR | CI 95% | p |
|---|---|---|---|---|---|---|
| Without Propensity Score Adjustment | With Propensity Score Adjustment | |||||
| Daptomycin-containing-regimen | 0.15 | 0.04–0.46 | <0.001 | 0.3 | 0.15–0.87 | 0.001 |
| >2 vertebrae involved | 2.4 | 1.12–5.24 | 0.002 | 3.22 | 2.09–5.47 | <0.001 |
| Inadequate drainage of infection | 4.8 | 2.45–8.51 | <0.001 | 5.4 | 3.22–9.12 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Russo, A.; Ceccarelli, G.; Bellelli, V.; Bianchi, L.; Marincola Cattaneo, F.; Gregori, F.; Palmarini, V.; Marotta, N.; Landi, A.; Cuzzolino, A.; et al. Efficacy of Daptomycin-Containing Regimen for Treatment of Staphylococcal or Enterococcal Vertebral Osteomyelitis: A Prospective Clinical Experience. Antibiotics 2020, 9, 889. https://doi.org/10.3390/antibiotics9120889
Russo A, Ceccarelli G, Bellelli V, Bianchi L, Marincola Cattaneo F, Gregori F, Palmarini V, Marotta N, Landi A, Cuzzolino A, et al. Efficacy of Daptomycin-Containing Regimen for Treatment of Staphylococcal or Enterococcal Vertebral Osteomyelitis: A Prospective Clinical Experience. Antibiotics. 2020; 9(12):889. https://doi.org/10.3390/antibiotics9120889
Chicago/Turabian StyleRusso, Alessandro, Giancarlo Ceccarelli, Valeria Bellelli, Luigi Bianchi, Federica Marincola Cattaneo, Fabrizio Gregori, Valeria Palmarini, Nicola Marotta, Alessandro Landi, Alessandro Cuzzolino, and et al. 2020. "Efficacy of Daptomycin-Containing Regimen for Treatment of Staphylococcal or Enterococcal Vertebral Osteomyelitis: A Prospective Clinical Experience" Antibiotics 9, no. 12: 889. https://doi.org/10.3390/antibiotics9120889
APA StyleRusso, A., Ceccarelli, G., Bellelli, V., Bianchi, L., Marincola Cattaneo, F., Gregori, F., Palmarini, V., Marotta, N., Landi, A., Cuzzolino, A., Stefanini, M., Aureli, A., Mastroianni, C. M., Venditti, M., d’Ettorre, G., & Sabetta, F. (2020). Efficacy of Daptomycin-Containing Regimen for Treatment of Staphylococcal or Enterococcal Vertebral Osteomyelitis: A Prospective Clinical Experience. Antibiotics, 9(12), 889. https://doi.org/10.3390/antibiotics9120889








