Knowledge of Antimicrobial Resistance among Veterinary Students and Their Personal Antibiotic Use Practices: A National Cross-Sectional Survey
Abstract
1. Introduction
2. Materials and Methods
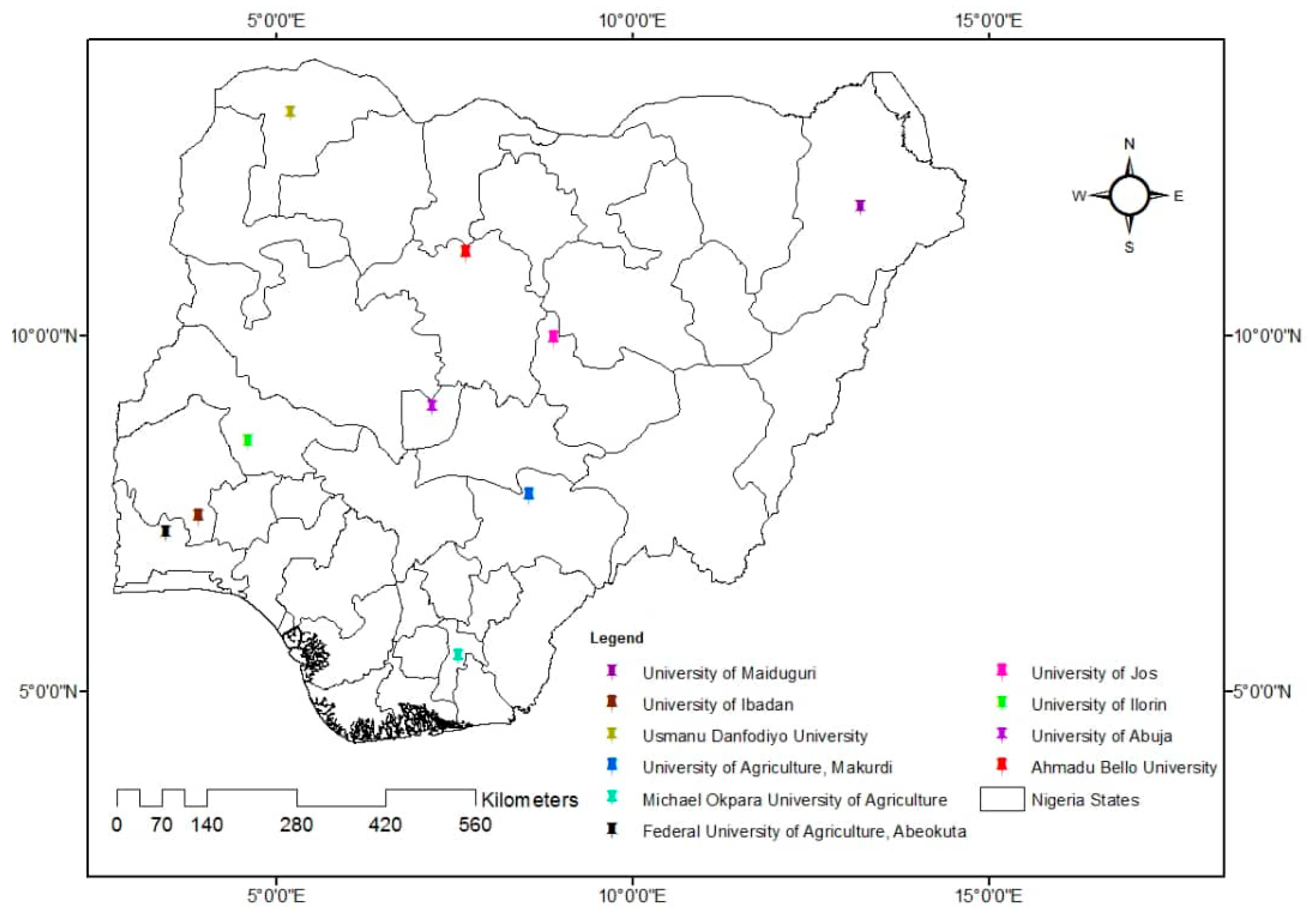
2.1. Structure of the Target Population
2.2. Study Design, Sample Size, and Sampling Protocol
2.3. Questionnaire Design, Pre-Test, and Administration
2.4. Data Management and Analysis
3. Results
3.1. Demographic Information
3.2. Personal Antibiotic Usage Pattern among Veterinary Students
3.3. Knowledge and Factors Associated with AMR among Respondents
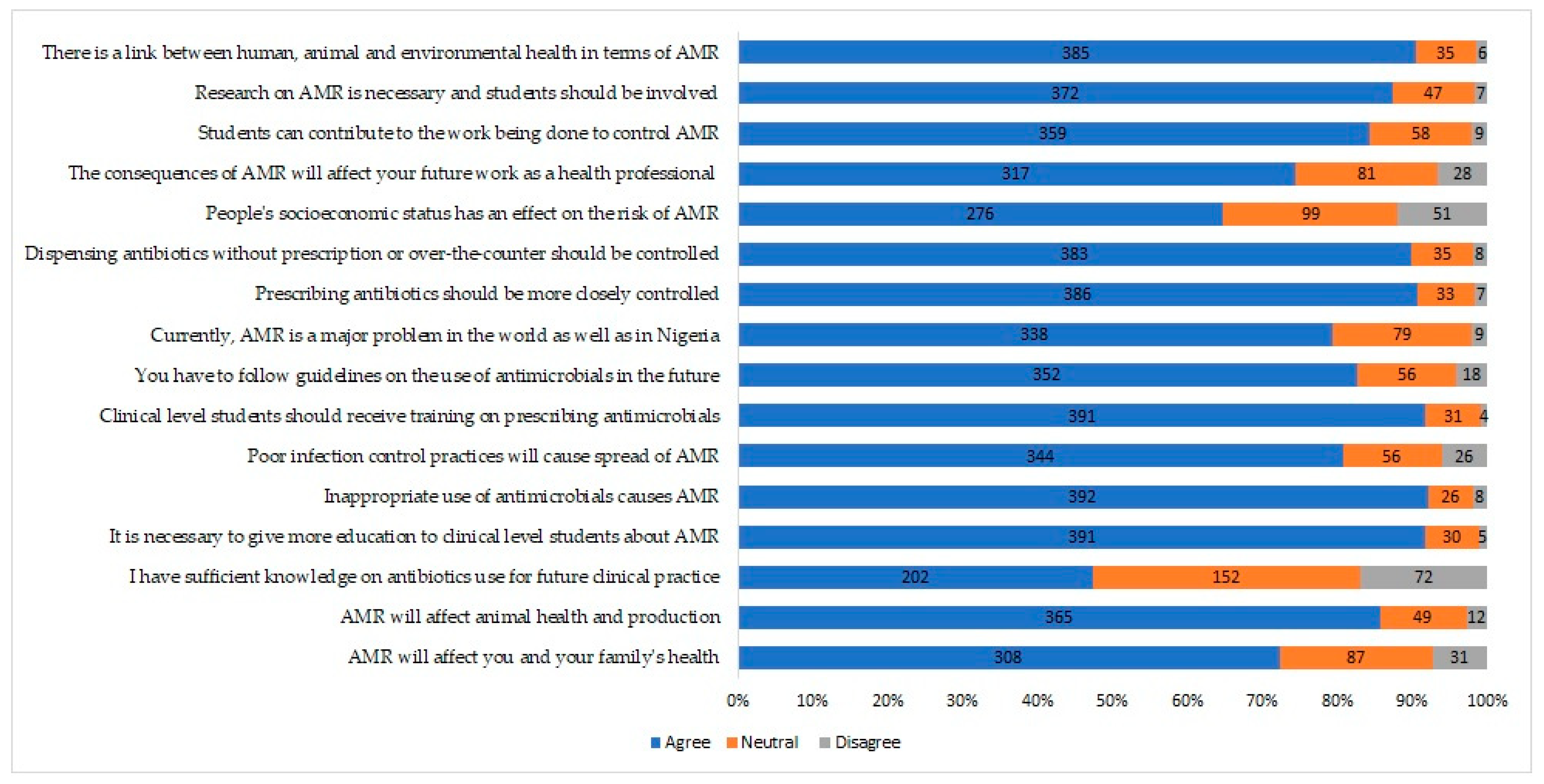
3.4. The Attitude of Respondents to AMR
3.5. AMR Awareness among Veterinary Students
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Prestinaci, F.; Pezzotti, P.; Pantosti, A. Antimicrobial resistance: A global multifaceted phenomenon. Pathog. Glob. Health 2015, 109, 309–318. [Google Scholar] [CrossRef] [PubMed]
- WHO. Antimicrobial Resistance. World Health Organization. Fact Sheet. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance (accessed on 31 October 2019).
- FMAEH. Antimicrobial Use and Resistance in Nigeria: Situation Analysis and Recommendations. Federal Ministries of Agriculture, Environment and Health, Abuja, Nigeria. 2017. Available online: https://ncdc.gov.ng/themes/common/docs/protocols/56_1510840387.pdf (accessed on 31 October 2019).
- Manyi-Loh, C.; Mamphweli, S.; Meyer, E.; Okoh, A. Antibiotic use in agriculture and its consequential resistance in environmental sources: Potential public health implications. Molecules 2018, 23, 795. [Google Scholar] [CrossRef] [PubMed]
- WHO. Antimicrobial Resistance. In Global Report on Surveillance; WHO, Ed.; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- O’Neill, J. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. Review on Antimicrobial Resistance. London, UK. 2014. Available online: https://amr-review.org/sites/default/files/AMR%20Review%20Paper%20-%20Tackling%20a%20crisis%20for%20the%20health%20and%20wealth%20of%20nations_1.pdf (accessed on 18 June 2019).
- Tadesse, B.T.; Ashley, E.A.; Ongarello, S.; Havumaki, J.; Wijegoonewardena, M.; González, I.J.; Dittrich, S. Antimicrobial resistance in Africa: A systematic review. BMC Infect. Dis. 2017, 17, 616. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.W.; Agbaje, M.; LeRoux-Pullen, L.; Van Dyk, D.; Debusho, L.K.; Shittu, A.; Sirdar, M.M.; Fasanmi, O.G.; Adebowale, O.; Fasina, F.O. Implication of the knowledge and perceptions of veterinary students of antimicrobial resistance for future prescription of antimicrobials in animal health. J. S. Afr. Vet. Assoc. 2019, 90. [Google Scholar] [CrossRef]
- Oloso, N.O.; Fagbo, S.; Garbati, M.; Olonitola, S.O.; Awosanya, E.J.; Aworh, M.K.; Adamu, H.; Odetokun, I.A.; Fasina, F.O. Antimicrobial resistance in food animals and the environment in Nigeria: A review. Int. J. Environ. Res. Public Health 2018, 15, 1284. [Google Scholar] [CrossRef]
- Syed, M.A.; Bana, N.F. Developing countries need action plans to combat the challenge of antimicrobial resistance. Arch. Clin. Microbiol. 2016, 7, 12. [Google Scholar]
- Cuong, N.V.; Padungtod, P.; Thwaites, G.; Carrique-Mas, J.J. Antimicrobial usage in animal production: A review of the literature with a focus on Low- and Middle-Income countries. Antibiotics 2018, 7, 75. [Google Scholar] [CrossRef]
- Meseko, C.; Makanju, O.; Ehizibolo, D.; Muraina, I. Veterinary Pharmaceuticals and antimicrobial resistance in developing countries. IntechOpen. Vet. Pharm. 2019. [Google Scholar] [CrossRef]
- Alhaji, N.B.; Isola, T.O. Antimicrobial usage by pastoralists in food animals in North-central Nigeria: The associated socio-cultural drivers for antimicrobials misuse and public health implications. One Health 2018, 6, 41–47. [Google Scholar] [CrossRef]
- Adesokan, H.K.; Akanbi, I.O.; Akanbi, I.M.; Obaweda, R.A. Pattern of antimicrobial usage in livestock animals in south-western Nigeria: The need for alternative plans. Onderstepoort J. Vet. Res. 2015, 82, 01–06. [Google Scholar] [CrossRef]
- Ogaboh, A. National Health Insurance Scheme (NHIS) and employees’ access to health care services in Cross River State, Nigeria. Glob. J. Hum. Soc. Sci. 2010, 10, 9–16. [Google Scholar]
- Ibiwoye, A.; Adeleke, I.A. Does national health insurance promote access to quality health care? Evidence from Nigeria. Geneva Pap. Risk Insur. Ssues Pract. 2008, 33, 219–233. [Google Scholar] [CrossRef]
- Ekwochi, U.; Chinawa, J.M.; Obi, I.; Obu, H.A.; Agwu, S. Use and/or misuse of antimicrobials in management of diarrhoea among children in Enugu, South-East Nigeria. J. Trop. Paediatr. 2013, 59, 314–316. [Google Scholar] [CrossRef] [PubMed]
- Ekwochi, U.; Chinawa, J.M.; Osuorah, C.D.; Odetunde, O.I.; Obu, H.A.; Agwu, S. The use of unprescribed antimicrobials in management of upper respiratory tract infection in children in Enugu, South East Nigeria. J. Trop Paediatr. 2014, 60, 249–252. [Google Scholar] [CrossRef]
- Castro-Sánchez, E.; Drumright, L.N.; Gharbi, M.; Farrell, S.; Holmes, A.H. Mapping antimicrobial stewardship in undergraduate medical, dental, pharmacy, nursing and veterinary education in the United Kingdom. PLoS ONE 2016, 11, e0150056. [Google Scholar] [CrossRef]
- Moran, D. Antimicrobial resistance in animal agriculture: Understanding user attitude and behaviours. Vet. Rec. 2017, 181, 508–509. [Google Scholar] [CrossRef]
- Dyar, O.J.; Hills, H.; Seitz, L.T.; Perry, A.; Ashiru-Oredope, D. Assessing the knowledge, attitudes and behavior of human and animal health students towards antibiotic use and resistance: A pilot cross-sectional study in the UK. Antibiotics 2018, 7, 10. [Google Scholar] [CrossRef]
- MacDougall, C.; Schwartz, B.S.; Kim, L.; Nanamori, M.; Shekarchian, S.; Chin-Hong, P.V. An interprofessional curriculum on antimicrobial stewardship improves knowledge and attitudes toward appropriate antimicrobial use and collaboration. Open Forum Infect. Dis. 2017, 4, ofw225. [Google Scholar] [CrossRef]
- Wasserman, S.; Potgieter, S.; Shoul, E.; Constant, D.; Stewart, A.; Mendelson, M.; Boyles, T.H. South African medical students’ perceptions and knowledge about antibiotic resistance and appropriate prescribing: Are we providing adequate training to future prescribers? S. Afr. Med. J. 2017, 107, 405–410. [Google Scholar] [CrossRef]
- Weier, N.; Thursky, K.; Zaidi, S.T.R. Antimicrobial knowledge and confidence amongst final year medical students in Australia. PLoS ONE 2017, 12, e0182460. [Google Scholar] [CrossRef]
- Hardefeldt, L.; Nielsen, T.; Crabb, H.; Gilkerson, J.; Squires, R.; Heller, J.; Sharp, C.; Cobbold, R.; Norris, J.; Browning, G. Veterinary students’ knowledge and perceptions about antimicrobial stewardship and biosecurity—A national survey. Antibiotics. 2018, 7, 34. [Google Scholar] [CrossRef] [PubMed]
- Anyanwu, M.U.; Okorie-Kanu, O.J.; Anyaoha, C.O.; Kolade, A.O. Veterinary medical students’ perceptions, attitude and knowledge about antibiotic resistance and stewardship: How prepared are our future prescribers? Notulae Scientia Biologicae 2018, 10, 156–174. [Google Scholar] [CrossRef]
- Thrusfield, M. Veterinary Epidemiology, 3rd ed.; Blackwell Publishing: Oxford, UK, 2009; pp. 626–630. [Google Scholar]
- Dean, A.G.; Sullivan, K.M.; Soe, M.M. OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version. 2013. Available online: https://www.OpenEpi.com (accessed on 6 April 2013).
- Seid, M.A.; Hussen, M.S. Knowledge and attitude towards antimicrobial resistance among final year undergraduate paramedical students at University of Gondar, Ethiopia. BMC Infect Dis. 2018, 18, 312. [Google Scholar] [CrossRef]
- Sakeena, M.H.F.; Bennett, A.A.; Jamshed, S.; Mohamed, F.; Herath, D.R.; Gawarammana, I.; McLachlan, A.J. Investigating knowledge regarding antibiotics and antimicrobial resistance among pharmacy students in Sri Lankan universities. BMC Infect. Dis. 2018, 18, 209. [Google Scholar] [CrossRef] [PubMed]
- WMA. World Medical Association Declaration of Helsinki ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Odetokun, I.A.; Jagun-Jubril, A.T.; Onoja, B.A.; Wungak, Y.S.; Raufu, I.A.; Chen, J.C. Status of laboratory biosafety and biosecurity in veterinary research facilities in Nigeria. Saf. Health Work. 2017, 8, 49–58. [Google Scholar] [CrossRef]
- Sanya, T.; Titilayo, O.; Adisa, R.; Segun, J. Use of antibiotics among non-medical students in a Nigerian university. Afr. Health Sci. 2013, 13, 1149–1155. [Google Scholar] [CrossRef]
- Asogwa, I.E.; Offor, S.J.; Mbagwu, H.O.C. Knowledge, attitude and practice towards antibiotics use among non-medical university students in Uyo, Nigeria. J. Adv. Med. Pharm. Sci. 2017, 15, 1–11. [Google Scholar] [CrossRef]
- Minen, M.T.; Duquaine, D.; Marx, M.A.; Weiss, D. A survey of knowledge, attitudes, and beliefs of medical students concerning antimicrobial use and resistance. Microb. Drug Resist. 2010, 16, 285–289. [Google Scholar] [CrossRef]
- Abbo, L.M.; Cosgrove, S.E.; Pottinger, P.S.; Pereyra, M.; Sinkowitz-Cochran, R.; Srinivasan, A.; Webb, D.J.; Hooton, T.M. Medical students’ perceptions and knowledge about antimicrobial stewardship: How are we educating our future prescribers? Clin. Infect. Dis. 2013, 57, 631–638. [Google Scholar] [CrossRef]
- Dyar, O.J.; Howard, P.; Nathwani, D.; Pulcini, C.; ESGAP. Knowledge, attitudes, and beliefs of French medical students about antibiotic prescribing and resistance. Médecine et maladies infectieuses 2013, 43, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Dyar, O.J.; Pulcini, C.; Howard, P.; Nathwani, D.; ESGAP. European medical students: A first multicenter study of knowledge, attitudes and perceptions of antibiotic prescribing and antibiotic resistance. J. Antimicrob. Chemother. 2014, 69, 842–846. [Google Scholar] [CrossRef] [PubMed]
- Anyanwu, M.U.; Kolade, O.A. Veterinarians’ perception, knowledge and practices of antibiotic stewardship in Enugu State Southeast, Nigeria. Notulae Scientia Biologicae. 2017, 9, 321–331. [Google Scholar] [CrossRef]
| Outcomes | Maximum Obtainable Score | Scores Obtained by Respondents | Mean ± SD | Satisfactory n (%) | Unsatisfactory n (%) | |
|---|---|---|---|---|---|---|
| Lowest | Highest | |||||
| Antibiotics and antimicrobial resistance in humans | 15 | 5.00 | 15.00 | 11.33 ± 2.25 1 | 146 (35.4) | 267 (64.6) |
| Antibiotics and antimicrobial resistance in Animals | 13 | 4.00 | 13.00 | 9.97 ± 1.69 1 | 72 (17.4) | 341 (82.6) |
| Contributory factors to antimicrobial resistance | 10 | 0.00 | 10.00 | 5.24 ± 2.69 1 | 137 (33.2) | 276 (66.8) |
| Overall knowledge of antimicrobial resistance | 38 | 11.00 | 37.00 | 26.55 ± 4.93 1 | 166 (40.0) | 248 (60.0) |
| Demographic Factors | n (%) |
|---|---|
| Gender | |
| Male | 264 (62.0) |
| Female | 162 (38.0) |
| Age (year) | |
| 17–21 | 141 (33.1) |
| 22–26 | 237 (55.6) |
| 27–31 | 48 (11.3) |
| Level of study | |
| Year 2 | 56 (13.1) |
| Year 3 | 84 (19.7) |
| Year 4 | 84 (19.7) |
| Year 5 | 86 (20.2) |
| Year 6 | 116 (27.2) |
| University | |
| UNILORIN | 79 (18.5) |
| FUNAAB | 16 (3.8) |
| UNIMAID | 64 (15.0) |
| UDUS | 40 (9.4) |
| UNIABUJA | 31 (7.3) |
| ABU | 28 (6.6) |
| UI | 26 (6.1) |
| UAM 1 | 5 (1.2) |
| UNIJOS 1 | 8 (1.9) |
| MOUAU | 129 (30.3) |
| Parameters | n (%) |
|---|---|
| Last antibiotic use | |
| In the last month | 167 (39.2) |
| In the last 6 months | 108 (25.4) |
| In the last year | 47 (11.0) |
| More than a year ago | 29 (6.8) |
| Never | 15 (3.5) |
| Can’t remember | 60 (14.1) |
| Getting antibiotics from a doctor’s prescription | |
| Yes | 250 (60.7) |
| No | 143 (34.7) |
| Can’t remember | 18 (4.4) |
| On that occasion, did you get advice from a doctor, nurse or pharmacist on how to take them? | |
| Yes | 290 (70.4) |
| No | 104 (25.2) |
| Can’t remember | 18 (4.4) |
| On that occasion, where did you get the antibiotics? | |
| Medical store/Pharmacy | 363 (88.1) |
| Stall/hawker | 7 (1.7) |
| Friends/Family member | 18 (4.4) |
| I have them saved up from previous time | 10 (2.4) |
| Somewhere/someone else | 14 (3.4) |
| When do you think you should stop taking antibiotics once you have begun treatment? | |
| When you feel better | 44 (10.7) |
| When you have taken all antibiotics as directed | 359 (87.1) |
| Don’t know | 9 (2.2) |
| It is okay to use antibiotics that were given to a friend or family member, as long as they were used to treat the same illnesses | |
| False | 297 (72.1) |
| True | 89 (21.6) |
| Don’t know | 26 (6.3) |
| It is okay to buy the same antibiotics, or request these from a doctor if you are sick and they helped you get better when you had the same symptoms before? | |
| False | 220 (53.4) |
| True | 158 (38.3) |
| Don’t know | 34 (8.3) |
| Age (Years) | Antibiotics and Antimicrobial Resistance in Humans | |||||
|---|---|---|---|---|---|---|
| Unsatisfactory (%) | Satisfactory (%) | p Value (χ2) | OR | 95%CI | p Value | |
| 17–21 | 107 (85.0) | 30 (15.0) | 0.000 | 1.00 | - | - |
| 22–26 | 135 (58.7) | 95 (41.3) | 2.51 | 1.55, 4.07 | <0.001 * | |
| 27–31 | 25 (54.3) | 21 (45.7) | 2.99 | 1.48, 6.08 | 0.004 * | |
| Antibiotics and antimicrobial resistance in animals | ||||||
| Unsatisfactory (%) | Satisfactory (%) | |||||
| 17–21 | 122 (89.1) | 15 (10.9) | 0.049 | 1.00 | - | - |
| 22–26 | 183 (79.6) | 47 (20.4) | 2.09 | 1.12, 3.90 | 0.025 * | |
| 27–31 | 36 (78.3) | 10 (21.7) | 2.26 | 0.94, 5.46 | 0.118 | |
| Contributory factors to antimicrobial resistance | ||||||
| Unsatisfactory (%) | Satisfactory (%) | |||||
| 17–21 | 105 (76.6) | 32 (23.4) | 0.004 | 1.00 | - | - |
| 22–26 | 138 (60.0) | 92 (40.0) | 2.19 | 1.36, 3.52 | 0.001 * | |
| 27–31 | 33 (71.7) | 13 (28.3) | 1.29 | 0.61, 2.73 | 0.629 | |
| Overall knowledge of antimicrobial resistance | ||||||
| Unsatisfactory (%) | Satisfactory (%) | |||||
| 17–21 | 107 (78.1) | 30 (21.9) | 0.000 | 1.00 | - | - |
| 22–26 | 115 (50.0) | 115 (50.0) | 3.57 | 2.21, 5.77 | <0.001 * | |
| 27–31 | 26 (56.5) | 20 (43.5) | 2.74 | 1.35, 5.58 | 0.009 * | |
| Year of Study | Antibiotics and Antimicrobial Resistance in Humans | |||||
|---|---|---|---|---|---|---|
| Unsatisfactory (%) | Satisfactory (%) | p Value (χ2) | OR | 95% CI | p Value | |
| Two | 45 (90.0) | 5 (10.0) | 0.000 | 1.00 | - | - |
| Three | 64 (81.0) | 15 (18.9) | 2.11 | 0.71, 6.22 | 0.259 | |
| Four | 57 (67.9) | 27 (32.1) | 4.26 | 1.52, 11.95 | 0.005 * | |
| Five | 44 (52.4) | 40 (47.6) | 8.12 | 2.96, 22.65 | <0.001 * | |
| Six | 57 (49.1) | 59 (50.9) | 9.32 | 3.45, 25.15 | <0.001 * | |
| Antibiotics and antimicrobial resistance in animals | ||||||
| Unsatisfactory (%) | Satisfactory (%) | |||||
| Two | 49 (98.0) | 1 (2.0) | 0.000 | 1.00 | - | - |
| Three | 75 (94.9) | 4 (5.1) | 2.61 | 0.28, 24.08 | 0.709 | |
| Four | 71 (84.5) | 13 (15.5) | 8.97 | 1.14, 388.90 | 0.020 * | |
| Five | 55 (65.5) | 29 (34.5) | 25.89 | 3.39, 196.80 | <0.001 * | |
| Six | 90 (77.6) | 26 (22.4) | 14.16 | 1.86, 107.50 | <0.001 * | |
| Contributory factors to antimicrobial resistance | ||||||
| Unsatisfactory (%) | Satisfactory (%) | |||||
| Two | 40 (80.0) | 10 (20.0) | 0.000 | 1.00 | - | - |
| Three | 64 (81.0) | 15 (19.0) | 1.00 | 0.41, 2.42 | >0.999 | |
| Four | 60 (71.4) | 24 (28.6) | 1.60 | 0.69, 4.16 | 0.371 | |
| Five | 48 (57.1) | 36 (42.9) | 3.00 | 1.33, 6.79 | 0.011 * | |
| Six | 64 (55.2) | 52 (44.8) | 3.25 | 1.48, 7.12 | 0.003 * | |
| Overall knowledge of antimicrobial resistance | ||||||
| Unsatisfactory (%) | Satisfactory (%) | |||||
| Two | 45 (90.0) | 5 (10.0) | 0.000 | 1.00 | - | - |
| Three | 65 (82.3) | 14 (17.7) | 1.94 | 0.65, 5.76 | 0.343 | |
| Four | 56 (66.67) | 28 (33.33) | 4.50 | 1.61, 12.60 | 0.003 * | |
| Five | 35 (45.2) | 49 (54.8) | 12.60 | 4.50, 34.96 | <0.001 * | |
| Six | 47 (40.52) | 69 (59.48) | 13.21 | 4.88, 35.75 | <0.001 * | |
| Terms | No (%) | Yes (%) |
|---|---|---|
| AMR | 246 (57.7) | 180 (42.3) |
| Superbugs | 353 (82.9) | 73 (17.1) |
| Antimicrobial stewardship | 370 (86.9) | 56 (13.1) |
| World Antibiotic Awareness Week | 272 (63.8) | 154 (36.2) |
| Global Antimicrobial Resistance Surveillance System (GLASS) | 324 (76.1) | 102 (23.9) |
| Global Antibiotic Research and Development Partnership (GARDP) | 343 (80.5) | 83 (19.5) |
| Global Action Plan on Antimicrobial Resistance | 349 (81.9) | 77 (18.1) |
| National Action Plan for Antimicrobial Resistance, Nigeria | 309 (72.5) | 117 (27.5) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Odetokun, I.A.; Akpabio, U.; Alhaji, N.B.; Biobaku, K.T.; Oloso, N.O.; Ghali-Mohammed, I.; Biobaku, A.J.; Adetunji, V.O.; Fasina, F.O. Knowledge of Antimicrobial Resistance among Veterinary Students and Their Personal Antibiotic Use Practices: A National Cross-Sectional Survey. Antibiotics 2019, 8, 243. https://doi.org/10.3390/antibiotics8040243
Odetokun IA, Akpabio U, Alhaji NB, Biobaku KT, Oloso NO, Ghali-Mohammed I, Biobaku AJ, Adetunji VO, Fasina FO. Knowledge of Antimicrobial Resistance among Veterinary Students and Their Personal Antibiotic Use Practices: A National Cross-Sectional Survey. Antibiotics. 2019; 8(4):243. https://doi.org/10.3390/antibiotics8040243
Chicago/Turabian StyleOdetokun, Ismail A., Uduak Akpabio, Nma B. Alhaji, Khalid T. Biobaku, Nurudeen O. Oloso, Ibraheem Ghali-Mohammed, Asmau J. Biobaku, Victoria O. Adetunji, and Folorunso O. Fasina. 2019. "Knowledge of Antimicrobial Resistance among Veterinary Students and Their Personal Antibiotic Use Practices: A National Cross-Sectional Survey" Antibiotics 8, no. 4: 243. https://doi.org/10.3390/antibiotics8040243
APA StyleOdetokun, I. A., Akpabio, U., Alhaji, N. B., Biobaku, K. T., Oloso, N. O., Ghali-Mohammed, I., Biobaku, A. J., Adetunji, V. O., & Fasina, F. O. (2019). Knowledge of Antimicrobial Resistance among Veterinary Students and Their Personal Antibiotic Use Practices: A National Cross-Sectional Survey. Antibiotics, 8(4), 243. https://doi.org/10.3390/antibiotics8040243






