Statin Use and the Point Prevalence of Antibiotics in Ambulatory Patients with Diabetes in the National Health and Nutrition Examination Survey (NHANES) 2003–2012
Abstract
1. Introduction
2. Materials and Methods
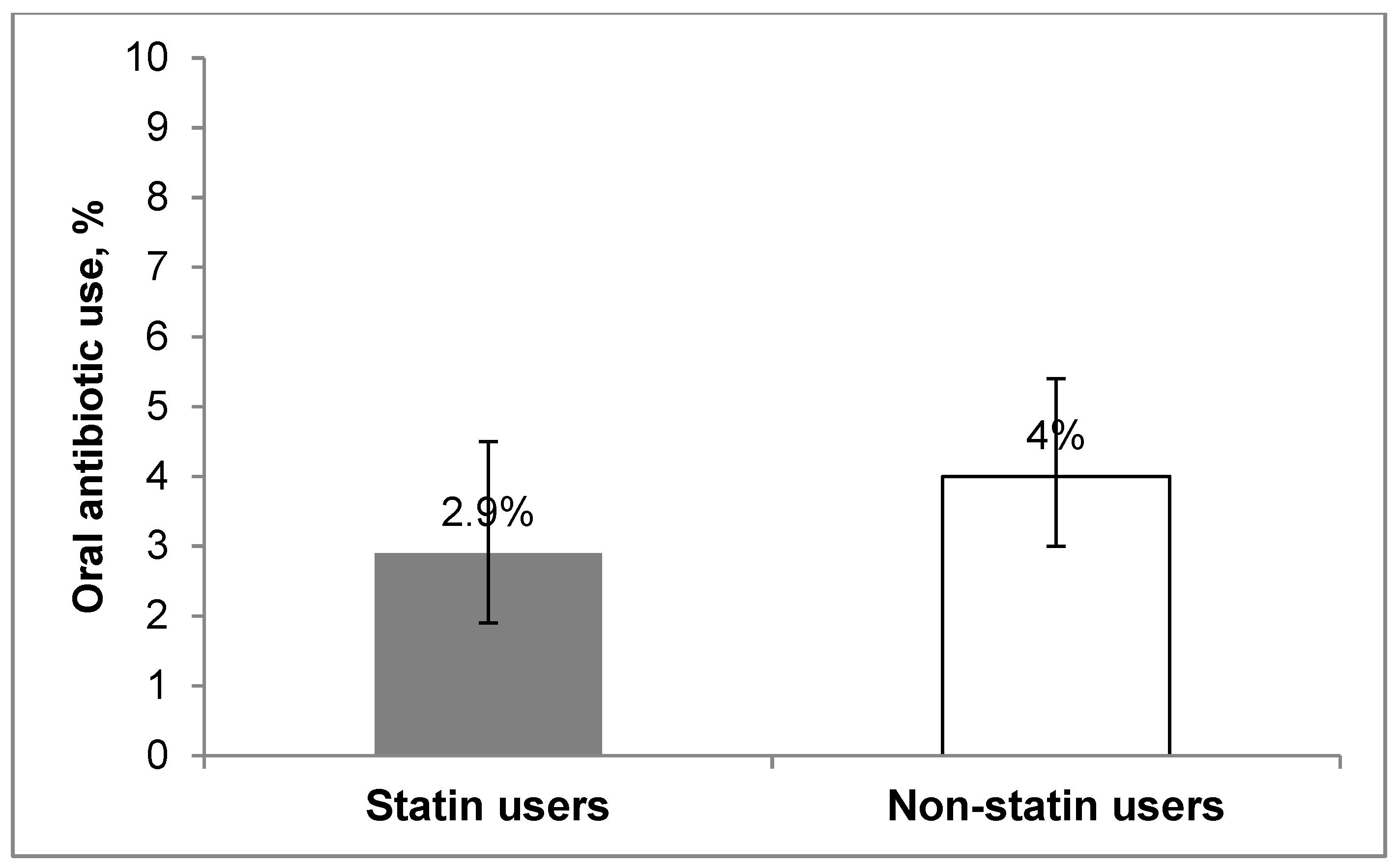
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Oral antibiotics listed in NHANES | |
|---|---|
| Penicillins Amoxicillin Amoxicillin-clavulanate Cloxacillin Dicloxacillin Penicillin V | Cephalosporins First Generation Cephalexin Cefadroxil Second Generation Cefuroxime Cefaclor Cefprozil Third Generation Cefdinir Cefditoren Cefixime Cefpodoxime Ceftibuten |
| Macrolide Antibiotics Azithromycin Erythromycin Clarithromycin Telithromycin | Quinolone Antibiotics Ciprofloxacin Norfloxacin Ofloxacin Levofloxacin Moxifloxacin Gemifloxacin |
| Lincosamides Clindamycin | Sulfonamides Trimethoprim-Sulfamethoxazole |
| Tetracycline Antibiotics Doxycycline Minocycline Tetracycline | Other Antibiotics Metronidazole Nitrofurantoin Vancomycin |
References
- Joshi, N.; Caputo, G.; Weitekamp, M. Infections in Patients with Diabetes Mellitus. N. Engl. J. 1999. [Google Scholar] [CrossRef]
- Muller, L.M.A.J.; Gorter, K.J.; Hak, E.; Goudzwaard, W.L.; Schellevis, F.G.; Hoepelman, A.I.M.; Rutten, G.E.H.M. Increased Risk of Common Infections in Patients with Type 1 and Type 2 Diabetes Mellitus. Clin. Infect. Dis. 2005. [Google Scholar] [CrossRef]
- Geerlings, S.E.; Hoepelman, A.I.M. Immune Dysfunction in Patients with Diabetes Mellitus (DM). FEMS Immunol. Med. Microbiol. 1999. [Google Scholar] [CrossRef]
- Shah, B.R.; Hux, J.E. Quantifying the Risk of Infectious Diseases for People with Diabetes. Diabetes Care 2003. [Google Scholar] [CrossRef]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. J. Am. Coll. Cardiol. 2018. [Google Scholar] [CrossRef]
- American Diabetes Association. Cardiovascular Disease and Risk Management. Diabetes Care 2017. [Google Scholar] [CrossRef]
- Bellosta, S.; Via, D.; Canavesi, M.; Pfister, P.; Fumagalli, R.; Paoletti, R.; Bernini, F. HMG-CoA Reductase Inhibitors Reduce MMP-9 Secretion by Macrophages. Arterioscler. Thromb. Vasc. Biol. 1998. [Google Scholar] [CrossRef]
- Koh, K.K.; Ahn, J.Y.; Jin, D.K.; Han, S.H.; Kim, H.S.; Choi, I.S.; Ahn, T.H.; Shin, E.K.; Jeong, E.M. Comparative Effects of Statin and Fibrate on Nitric Oxide Bioactivity and Matrix Metalloproteinase in Hyperlipidemia. Int. J. Cardiol. 2004. [Google Scholar] [CrossRef]
- Laufs, U.; La Fata, V.; Plutzky, J.; Liao, J.K. Upregulation of Endothelial Nitric Oxide Synthase by HMG CoA Reductase Inhibitors. Circulation 1998. [Google Scholar] [CrossRef]
- Liao, J.K.; Laufs, U. Pleiotropic Effects of Statins. Annu. Rev. Pharmacol. Toxicol. 2005, 45, 89–118. [Google Scholar] [CrossRef]
- Endres, M.; Laufs, U.; Huang, Z.; Nakamura, T.; Huang, P.; Moskowitz, M.A.; Liao, J.K. Stroke Protection by 3-Hydroxy-3-Methylglutaryl (HMG)-CoA Reductase Inhibitors Mediated by Endothelial Nitric Oxide Synthase. Proc. Natl. Acad. Sci. USA 1998. [Google Scholar] [CrossRef]
- Pickup, J.C. Inflammation and Activated Innate Immunity in the Pathogenesis of Type 2 Diabletes. Diabetes Care 2004. [Google Scholar] [CrossRef]
- Hennessy, E.; Adams, C.; Reen, F.J.; O’Gara, F. Is There Potential for Repurposing Statins as Novel Antimicrobials? Antimicrob. Agents Chemother. 2016. [Google Scholar] [CrossRef]
- Deshpande, A.; Pasupuleti, V.; Rothberg, M.B. Statin Therapy and Mortality from Sepsis: A Meta-Analysis of Randomized Trials. Am. J. Med. 2015. [Google Scholar] [CrossRef]
- Tralhão, A.F.R.; De Souza-Dantas, V.C.; Figueira Salluh, J.I.; Rodrigues Póvoa, P.M.S. Impact of Statins in Outcomes of Septic Patients: A Systematic Review. Postgrad. Med. 2014. [Google Scholar] [CrossRef]
- Papazian, L.; Roch, A.; Charles, P.E.; Penot-Ragon, C.; Perrin, G.; Roulier, P.; Goutorbe, P.; Lefrant, J.Y.; Wiramus, S.; Jung, B.; et al. Effect of Statin Therapy on Mortality in Patients with Ventilator- Associated Pneumonia: A Randomized Clinical Trial. J. Am. Med. Assoc. 2013. [Google Scholar] [CrossRef]
- Kruger, P.; Bailey, M.; Bellomo, R.; Cooper, D.J.; Harward, M.; Higgins, A.; Howe, B.; Jones, D.; Joyce, C.; Kostner, K.; et al. A Multicenter Randomized Trial of Atorvastatin Therapy in Intensive Care Patients with Severe Sepsis. Am. J. Respir. Crit. Care Med. 2013. [Google Scholar] [CrossRef]
- Caffrey, A.R.; Timbrook, T.T.; Noh, E.; Sakoulas, G.; Opal, S.M.; Nizet, V.; Laplante, K.L. Evidence to Support Continuation of Statin Therapy in Patients with Staphylococcus Aureus Bacteremia. Antimicrob. Agents Chemother. 2017. [Google Scholar] [CrossRef]
- Leung, S.; Pokharel, R.; Gong, M.N. Statins and Outcomes in Patients with Bloodstream Infection: A Propensity-Matched Analysis. Crit. Care Med. 2012. [Google Scholar] [CrossRef]
- Havers, F.; Bramley, A.M.; Finelli, L.; Reed, C.; Self, W.H.; Trabue, C.; Fakhran, S.; Balk, R.; Courtney, D.M.; Girard, T.D.; et al. Statin Use and Hospital Length of Stay among Adults Hospitalized with Community-Acquired Pneumonia. Clin. Infect. Dis. 2016. [Google Scholar] [CrossRef]
- Khan, A.R.; Riaz, M.; Abdulhak, A.A.B.; Al-Tannir, M.A.; Garbati, M.A.; Erwin, P.J.; Baddour, L.M.; Tleyjeh, I.M. The Role of Statins in Prevention and Treatment of Community Acquired Pneumonia: A Systematic Review and Meta-Analysis. PLoS ONE 2013. [Google Scholar] [CrossRef]
- Atamna, A.; Yahav, D.; Eliakim-Raz, N.; Goldberg, E.; Ben-Zvi, H.; Barsheshet, A.; Elis, A.; Bishara, J. The Effect of Statins on the Outcome of Clostridium Difficile Infection in Hospitalized Patients. Eur. J. Clin. Microbiol. Infect. Dis. 2016. [Google Scholar] [CrossRef] [PubMed]
- Motzkus-Feagans, C.; Pakyz, A.; Polk, R.; Gambassi, G.; Lapane, K.L. Statin Use and the Risk of Clostridium Difficile in Academic Medical Centres. Gut 2012. [Google Scholar] [CrossRef]
- Bruyere, R.; Vigneron, C.; Prin, S.; Pechinot, A.; Quenot, J.P.; Aho, S.; Papazian, L.; Charles, P.E. Impact of Prior Statin Therapy on the Outcome of Patients with Suspected Ventilator-Associated Pneumonia: An Observational Study. Crit. Care 2014. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Outpatient Antibiotic Prescriptions—United States, 2015; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2015; pp. 1–3.
- Center for Disease Control and Prevention. National Health and Nutrition Examination Survey. Available online: https://www.cdc.gov/nchs/nhanes/about_nhanes.htm (accessed on 16 January 2019).
- Van De Garde, E.M.W.; Hak, E.; Souverain, P.C.; Hoes, A.W.; Van Den Bosch, J.M.M.; Leufkens, H.G.M. Statin Treatment and Reduced Risk of Pneumonia in Patients with Diabetes. Thorax 2006. [Google Scholar] [CrossRef]
- Yang, T.L.; Lin, L.Y.; Huang, C.C.; Huang, P.H.; Lin, S.J.; Chen, J.W.; Chan, W.L.; Leu, H.B. Association of Statin Use and Reduced Risk of Lower-Extremity Amputation among Patients with Diabetes: A Nationwide Population-Based Cohort Observation. Diabetes Care 2016. [Google Scholar] [CrossRef]
- Magulick, J.P.; Frei, C.R.; Ali, S.K.; Mortensen, E.M.; Pugh, M.J.; Oramasionwu, C.U.; Daniels, K.R.; Mansi, I.A. The Effect of Statin Therapy on the Incidence of Infections: A Retrospective Cohort Analysis. Am. J. Med. Sci. 2014. [Google Scholar] [CrossRef] [PubMed]
- Van Den Hoek, H.L.; Bos, W.J.W.; De Boer, A.; Van De Garde, E.M.W. Statins and Prevention of Infections: Systematic Review and Meta-Analysis of Data from Large Randomised Placebo Controlled Trials. BMJ 2011. [Google Scholar] [CrossRef]
- Cooke, D.M.; Salter, A.J.; Phillips, I. The Impact of Antibiotic Policy on Prescribing in a London Teaching Hospital a One-Day Prevalence Survey as an Indicator of Antibiotic Use. J. Antimicrob. Chemother. 1983. [Google Scholar] [CrossRef]
- Dean, B.; Lawson, W.; Jacklin, A.; Rogers, T.; Azadian, B.; Holmes, A. The Use of Serial Point-Prevalence Studies to Investigate Hospital Anti-Infective Prescribing. Int. J. Pharm. Pract. 2002. [Google Scholar] [CrossRef]
- Graziano, T.S.; Cuzzullin, M.C.; Franco, G.C.; Schwartz-Filho, H.O.; De Andrade, E.D.; Groppo, F.C.; Cogo-Müller, K. Statins and Antimicrobial Effects: Simvastatin as a Potential Drug against Staphylococcus Aureus Biofilm. PLoS ONE 2015. [Google Scholar] [CrossRef] [PubMed]
- Jerwood, S.; Cohen, J. Unexpected Antimicrobial Effect of Statins. J. Antimicrob. Chemother. 2008. [Google Scholar] [CrossRef] [PubMed]
- Masadeh, M.; Mhaidat, N.; Alzoubi, K.; Al-azzam, S.; Alnasser, Z. Antibacterial Activity of Statins: A Comparative Study of Atorvastatin, Simvastatin, and Rosuvastatin. Ann. Clin. Microbiol. Antimicrob. 2012. [Google Scholar] [CrossRef]
- Thangamani, S.; Mohammad, H.; Abushahba, M.F.N.; Hamed, M.I.; Sobreira, T.J.P.; Hedrick, V.E.; Paul, L.N.; Seleem, M.N. Exploring Simvastatin, an Antihyperlipidemic Drug, as a Potential Topical Antibacterial Agent. Sci. Rep. 2015. [Google Scholar] [CrossRef] [PubMed]
- Majumdar, S.R.; McAlister, F.A.; Eurich, D.T.; Padwal, R.S.; Marrie, T.J. Statins and Outcomes in Patients Admitted to Hospital with Community Acquired Pneumonia: Population Based Prospective Cohort Study. Br. Med. J. 2006. [Google Scholar] [CrossRef] [PubMed]
- Egede, L.E. Association between Number of Physician Visits and Influenza Vaccination Coverage among Diabetic Adults with Access to Care. Diabetes Care 2003. [Google Scholar] [CrossRef][Green Version]
| Parameters | Overall (n = 3240) | Statin Users (n = 1575) | Non-Statin Users (n = 1665) | ||||
|---|---|---|---|---|---|---|---|
| Estimate | SE | Estimate | SE | Estimate | SE | p-Value | |
| Age, % | |||||||
| 20–40 years | 9.2 | 0.6 | 4.1 | 0.7 | 14.1 | 1.1 | 0.000 |
| 41–60 years | 40.7 | 1.2 | 36.5 | 1.8 | 44.8 | 1.6 | |
| 61 years and above | 50.1 | 1.3 | 59.4 | 1.8 | 41.1 | 1.7 | |
| Gender, % | |||||||
| Female | 52 | 1.2 | 49 | 1.7 | 54.9 | 1.4 | 0.003 |
| Race/Ethnicity, % | |||||||
| Hispanics | 13.3 | 1.5 | 10.5 | 1.3 | 16 | 1.9 | 0.000 |
| Whites | 61.7 | 2.2 | 66.6 | 2 | 57.1 | 2.8 | |
| Blacks | 17.6 | 1.5 | 15.9 | 1.5 | 19.2 | 1.7 | |
| Others | 7.4 | 0.8 | 7.1 | 1 | 7.7 | 1 | |
| Education Level, % | |||||||
| High school and below | 54.1 | 1.6 | 55.2 | 2.2 | 53.1 | 2 | 0.686 |
| Some college | 28.1 | 1.2 | 27.8 | 2 | 28.4 | 1.7 | |
| College and above | 17.8 | 1.2 | 17 | 1.5 | 18.5 | 1.6 | |
| Smoking, % | 34.2 | 1.3 | 27.30 | 2.20 | 41.4 | 2.5 | 0.000 |
| BMI, % | |||||||
| Normal | 14 | 0.9 | 12.5 | 1.2 | 15.4 | 1.2 | 0.034 |
| Overweight | 25.5 | 1.1 | 23.8 | 1.5 | 27.3 | 1.7 | |
| Obese | 60.5 | 1.4 | 63.8 | 1.9 | 57.3 | 1.9 | |
| Age at Diabetes Diagnosis | 0.229 | ||||||
| <20 years, % | 6.3% | 0.6% | 5.5% | 0.9% | 7.1% | 0.9% | |
| ≥20 years, % | 93.7% | 0.6% | 94.5% | 0.9% | 92.9% | 0.9% | |
| A1c < 7% (53 mmol/mol), % | 54 | 1.5 | 54 | 2 | 53.9 | 1.8 | 0.975 |
| DM Years, % | |||||||
| <5 | 33.2 | 1.1 | 29.4 | 1.4 | 36.9 | 1.8 | 0.003 |
| 5–10 | 28.4 | 0.8 | 28.5 | 1.5 | 28.4 | 1.3 | |
| >10 | 38.3 | 1.2 | 42.1 | 1.8 | 34.6 | 1.7 | |
| Health Insurance, % | 89.7 | 1.6 | 94.1 | 2.1 | 87.1 | 2 | 0.028 |
| Receive regular DM care, % | 97.3 | 0.4 | 99.1 | 0.4 | 95.6 | 0.6 | 0.000 |
| Prescription drug coverage 1, % | 91.7 | 1 | 92.9 | 1.1 | 90.3 | 1.2 | 0.038 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alarfaj, S.J.; Perez, A.; Unger, N.R. Statin Use and the Point Prevalence of Antibiotics in Ambulatory Patients with Diabetes in the National Health and Nutrition Examination Survey (NHANES) 2003–2012. Antibiotics 2019, 8, 64. https://doi.org/10.3390/antibiotics8020064
Alarfaj SJ, Perez A, Unger NR. Statin Use and the Point Prevalence of Antibiotics in Ambulatory Patients with Diabetes in the National Health and Nutrition Examination Survey (NHANES) 2003–2012. Antibiotics. 2019; 8(2):64. https://doi.org/10.3390/antibiotics8020064
Chicago/Turabian StyleAlarfaj, Sumaiah J., Alexandra Perez, and Nathan R. Unger. 2019. "Statin Use and the Point Prevalence of Antibiotics in Ambulatory Patients with Diabetes in the National Health and Nutrition Examination Survey (NHANES) 2003–2012" Antibiotics 8, no. 2: 64. https://doi.org/10.3390/antibiotics8020064
APA StyleAlarfaj, S. J., Perez, A., & Unger, N. R. (2019). Statin Use and the Point Prevalence of Antibiotics in Ambulatory Patients with Diabetes in the National Health and Nutrition Examination Survey (NHANES) 2003–2012. Antibiotics, 8(2), 64. https://doi.org/10.3390/antibiotics8020064




