Identification of Additional Anti-Persister Activity against Borrelia burgdorferi from an FDA Drug Library
Abstract
:1. Introduction
2. Results and Discussion
2.1. Identification of Drug Candidates with High Anti-Persister Activity
| Drugs (50 μM) | Category | Residual Viable Cells (Microscopy) b | Residual Viable Cells (SYBR Green/PI) c | p-Value d |
|---|---|---|---|---|
| Control (no drug) | 93% | 94% | - | |
| Doxycycline | Lyme antibiotic | 75% | 67% | 0.23360 |
| Amoxicillin | Lyme antibiotic | 76% | 76% | 1.00000 |
| Cefuroxime | Lyme antibiotic | 49% | 43% | 0.00032 |
| Daptomycin | Antibiotic | 35% | 28% | 0.00001 |
| Verteporfin e | Ophthalmic | 47% | 27% | 0.00284 |
| 3-formyl Rifamycin | Antibacterial | 59% | 42% | 0.00103 |
| Tartar emetic | Anthelmintic | 45% | 42% | 0.00250 |
| Toltrazuril | Antiprotozoal | 60% | 43% | 0.00296 |
| Thiostrepton | Antibiotic | 66% | 43% | 0.00131 |
| Mepartricin | Antifungal | 60% | 43% | 0.03214 |
| Tilorone | Antiviral | 44% | 0.04955 | |
| Oxantel | Anthelmintic | 63% | 44% | 0.01599 |
| Pidolic acid e | Antiseptic | 45% | 45% | 0.00477 |
| Hycanthone | Anthelmintic | 45% | 0.00154 | |
| Pyrimethamine | Antiprotozoal | 55% | 45% | 0.00030 |
| Carbenicillin | Antibiotic | 64% | 46% | 0.06453 |
| Oltipraz | Antitumor | 55% | 46% | 0.00121 |
| Bitoscanate | Anthelmintic | 46% | 0.00730 | |
| Sarafloxacin | Antibiotic | 50% | 47% | 0.05063 |
| Bacitracin | Antibiotic | 60% | 47% | 0.06536 |
| Dextrorphan tartrate e | Analgesic | 43% | 47% | 0.00361 |
| Tetramisole | Anthelmintic | 48% | 0.07051 | |
| Bifonazole | Antifungal | 50% | 48% | 0.09243 |
| Ethacridine lactate | Antiseptic | 48% | 0.04619 | |
| Zanamivir | Antiviral | 60% | 49% | 0.01224 |
| Artemesinin | Antimalarial | 45% | 49% | 0.10432 |
| Oxibendazole | Anthelminthic | 51% | 0.00895 | |
| Indatraline e | Antidepressant | 43% | 51% | 0.02578 |
| Nevirapine | Antiviral | 51% | 0.01604 | |
| Ganciclovir | Antiviral | 53% | 0.04466 | |
| Phenothiazine | Anthelminthic | 53% | 54% | 0.00228 |
| Oxfendazole | Anthelminthic | 54% | 0.00095 | |
| Flubendazole | Anthelminthic | 54% | 0.01183 | |
| Tazobactam | Antibiotic | 56% | 54% | 0.10052 |
| Aztreonam | Antibiotic | 50% | 55% | 0.08105 |
| Benzoylpas | Antibiotic | 55% | 0.04017 | |
| Fluconazole | Antifungal | 45% | 55% | 0.10643 |
| Cefixime | Antibiotic | 56% | 56% | 0.03238 |
| Sulfamoxole | Antibiotic | 55% | 57% | 0.02541 |
| Tosufloxacin | Antibiotic | 57% | 0.00067 | |
| Lamivudine | Antiviral | 58% | 0.01121 | |
| Cefsulodin | Antibiotic | 60% | 0.01463 | |
| Didanosine | Antiviral | 61% | 0.02494 | |
| Floxuridine | Antiviral | 61% | 0.01935 | |
| Cyacetacide | Antibacterial | 61% | 0.03407 | |
| Oxiconazole nitrate | Antifungal | 62% | 0.04957 | |
| Roxithromycin | Antibiotic | 65% | 62% | 0.15382 |
| Ribavirin | Antiviral | 63% | 0.00801 | |
| Griseofulvin | Antifungal | 63% | 0.00957 | |
| Rifamycin sv | Antibiotic | 60% | 63% | 0.01872 |
| Penciclovir | Antiviral | 60% | 64% | 0.09707 |
| Nystatin | Antifungal | 64% | 0.03312 | |
| Penimepicycline | Antibiotic | 60% | 65% | 0.00972 |
| Puromycin | Antibiotic | 48% | 65% | 0.29297 |
| Quinaldine blue | Antimalarial | 35% | Over range f | - |
| Methylene blue hydrate | Antimethemoglobinemic | 40% | Over range f | - |
| Active Hits | MIC (μg/mL) | Cmax (μg/mL) |
|---|---|---|
| Verteporfin | 4.49–8.98 | 1.03–1.14 |
| Thonzonium Bromide | 0.92–1.85 | NA |
| Benzododecinium Chloride | 0.60–1.20 | NA |
| 3-formyl Rifamycin | 2.27–4.54 | 10 |
| Pidolic Acid | 0.81–1.61 | 0.024 |
| Oltipraz | 0.71–1.41 | 4.97 |
| Fluconazole | 0.48–0.96 | 1.48–11.9 |
| Dextrorphan Tartrate | 1.27–2.55 | 0.025–0.030 |
| Quinaldine Blue | 2.43–4.86 | NA |
2.2. Antimicrobial Agents with High Activity against Stationary Phase B. burgdorferi
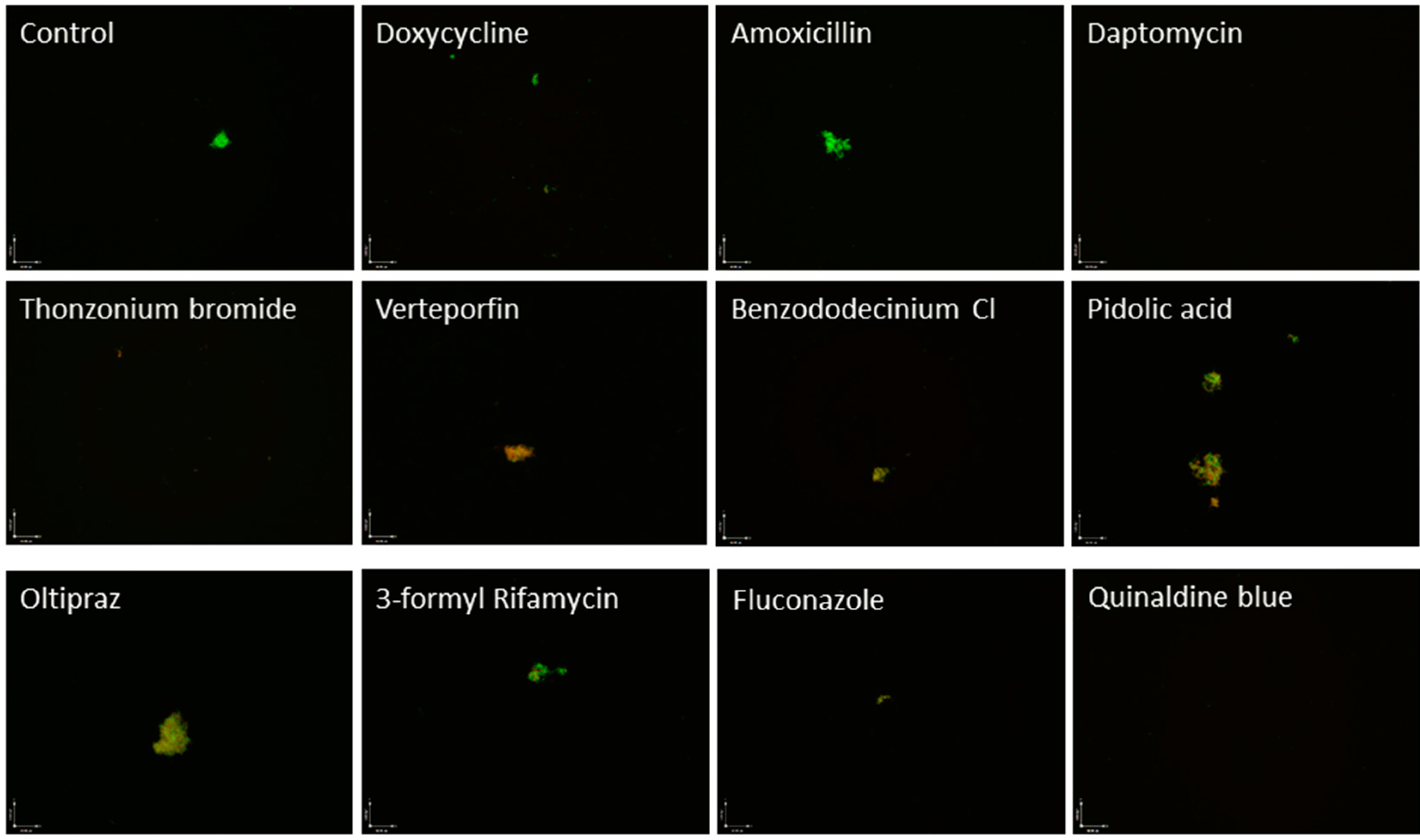
2.3. Agents Used for Treating Other Disease Conditions
2.4. Active Hits that Are Topical Agents or Toxic for Internal Use
3. Experimental Section
3.1. Strain and Culture Techniques
3.2. Microscopy
3.3. Drug Library Screens for Activity against B. burgdorferi Persisters in Vitro
4. Conclusions
Supplementary Files
Supplementary File 1Acknowledgments
Author Contributions
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Lyme Disease. Available online: http://www.cdc.gov/lyme/ (accessed on 5 June 2015).
- Hinckley, A.F.; Connally, N.P.; Meek, J.I.; Johnson, B.J.; Kemperman, M.M.; Feldman, K.A.; White, J.L.; Mead, P.S. Lyme disease testing by large commercial laboratories in the United States. Clin. Infect. Dis. 2014, 59, 676–681. [Google Scholar] [CrossRef] [PubMed]
- Radolf, J.D.; Caimano, M.J.; Stevenson, B.; Hu, L.T. Of ticks, mice and men: Understanding the dual-host lifestyle of lyme disease spirochaetes. Nat. Rev. Microbiol. 2012, 10, 87–99. [Google Scholar] [CrossRef] [PubMed]
- Wormser, G.P.; Dattwyler, R.J.; Shapiro, E.D.; Halperin, J.J.; Steere, A.C.; Klempner, M.S.; Krause, P.J.; Bakken, J.S.; Strle, F.; Stanek, G.; et al. The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: Clinical practice guidelines by the infectious diseases society of america. Clin. Infect. Dis. 2006, 43, 1089–1134. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Post Treatment Lyme Disease. Available online: http://www.cdc.gov/lyme/postLDS (accessed on 5 June 2015).
- Adrion, E.R.; Aucott, J.; Lemke, K.W.; Weiner, J.P. Health care costs, utilization and patterns of care following lyme disease. PLoS ONE 2015, 10, e0116767. [Google Scholar] [CrossRef] [PubMed]
- Aucott, J.N.; Rebman, A.W.; Crowder, L.A.; Kortte, K.B. Post-treatment lyme disease syndrome symptomatology and the impact on life functioning: Is there something there? Qual. Life Res. 2013, 22, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Phillips, S.E.; Mattman, L.H.; Hulinska, D.; Moayad, H. A proposal for the reliable culture of Borrelia burgdorferi from patients with chronic lyme disease, even from those previously aggressively treated. Infection 1998, 26, 364–367. [Google Scholar] [CrossRef] [PubMed]
- Barthold, S.W.; Hodzic, E.; Imai, D.M.; Feng, S.; Yang, X.; Luft, B.J. Ineffectiveness of tigecycline against persistent Borrelia burgdorferi. Antimicrob. Agents Chemother. 2010, 54, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Embers, M.E.; Barthold, S.W.; Borda, J.T.; Bowers, L.; Doyle, L.; Hodzic, E.; Jacobs, M.B.; Hasenkampf, N.R.; Martin, D.S.; Narasimhan, S.; et al. Persistence of Borrelia burgdorferi in Rhesus macaques following antibiotic treatment of disseminated infection. PLoS ONE 2012, 7, e29914. [Google Scholar] [CrossRef] [PubMed]
- Hodzic, E.; Imai, D.; Feng, S.; Barthold, S.W. Resurgence of persisting non-cultivable Borrelia burgdorferi following antibiotic treatment in mice. PLoS ONE 2014, 9, e86907. [Google Scholar] [CrossRef] [PubMed]
- Straubinger, R.K.; Summers, B.A.; Chang, Y.F.; Appel, M.J. Persistence of Borrelia burgdorferi in experimentally infected dogs after antibiotic treatment. J. Clin. Microbiol. 1997, 35, 111–116. [Google Scholar]
- Marques, A.; Telford, S.R., 3rd; Turk, S.P.; Chung, E.; Williams, C.; Dardick, K.; Krause, P.J.; Brandeburg, C.; Crowder, C.D.; Carolan, H.E.; et al. Xenodiagnosis to detect Borrelia burgdorferi infection: A first-in-human study. Clin. Infect. Dis. 2014, 58, 937–945. [Google Scholar] [CrossRef] [PubMed]
- Hodzic, E.; Feng, S.; Holden, K.; Freet, K.J.; Barthold, S.W. Persistence of Borrelia burgdorferi following antibiotic treatment in mice. Antimicrob. Agents Chemother. 2008, 52, 1728–1736. [Google Scholar] [CrossRef] [PubMed]
- Bayer, M.E.; Zhang, L.; Bayer, M.H. Borrelia burgdorferi DNA in the urine of treated patients with chronic lyme disease symptoms. A PCR study of 97 cases. Infection 1996, 24, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Lewis, K. Persister cells. Annu. Rev. Microbiol. 2010, 64, 357–372. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y. Persisters, persistent infections and the yin-yang model. Emerg. Microbes Infect. 2014, 3. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Wang, T.; Shi, W.; Zhang, S.; Sullivan, D.; Auwaerter, P.G.; Zhang, Y. Identification of novel activity against Borrelia burgdorferi persisters using an FDA approved drug library. Emerg. Microbes Infect. 2014, 3. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Auwaerter, P.G.; Zhang, Y. Drug combinations against Borrelia burgdorferi persisters in vitro: Eradication achieved by using daptomycin, cefoperazone and doxycycline. PLoS ONE 2015, 10, e0117207. [Google Scholar] [CrossRef] [PubMed]
- Sapi, E.; Kaur, N.; Anyanwu, S.; Luecke, D.F.; Datar, A.; Patel, S.; Rossi, M.; Stricker, R.B. Evaluation of in vitro antibiotic susceptibility of different morphological forms of Borrelia burgdorferi. Infect. Drug Resist. 2011, 4, 97–113. [Google Scholar] [PubMed]
- Feng, J.; Shi, W.; Zhang, S.; Zhang, Y. Identification of new compounds with high activity against Borrelia burgdorferi persisters from the nci compound collection. Emerg. Microbes Infect. 2015, 4. [Google Scholar] [CrossRef]
- US National Library of Medicine. Zanamivir Oral Inhalation. Available online: http://www.nlm.nih.gov/medlineplus/druginfo/meds/a699021.html (accessed on 24 June 2015).
- Soon, G.; Muir, A.; Gomez, M.I.; Waks, J.; Reddy, B.; Planet, P.; Singh, P.K.; Kanetko, Y.; Wolfgang, M.C.; Hsiao, Y.; et al. Bacterial neuraminidase facilitates mucosal infection by participating in biofilm production. J. Clin. Investig. 2006, 116, 2297–2305. [Google Scholar] [CrossRef] [PubMed]
- Chiou, J.F.; Wang, Y.H.; Jou, M.J.; Liu, T.Z.; Shiau, C.Y. Verteporfin-photoinduced apoptosis in HepG2 cells mediated by reactive oxygen and nitrogen species intermediates. Free Radic. Res. 2010, 44, 155–170. [Google Scholar] [CrossRef] [PubMed]
- Tate, S.S.; Ross, L.L.; Meister, A. The gamma-glutamyl cycle in the choroid plexus: Its possible function in amino acid transport. Proc. Natl. Acad. Sci. USA 1973, 70, 1447–1449. [Google Scholar] [CrossRef] [PubMed]
- Anderson, M.E. Glutathione: An overview of biosynthesis and modulation. Chem. Biol. Interact. 1998, 111–112, 1–14. [Google Scholar] [CrossRef]
- U.S. National Library of Medicine. Verteporfin Injection. Available online: http://www.nlm.nih.gov/medlineplus/druginfo/meds/a607060.html (accessed on 21 June 2015).
- Novartis Company. Visudyne: Verteporfin. Available online: http://www.novartis.com.au/PI_PDF/vid.pdf (accessed on 5 June 2015).
- Pancewicz, S.A.; Skrzdlewska, E.; Hermanowska-Szpakowicz, T.; Zajkowska, J.M.; Kondrusik, M. Role of reactive oxygen species (ros) in patients with erythema migrans, an early manifestation of lyme borreliosis. Med. Sci. Monit. 2001, 7, 1230–1235. [Google Scholar] [PubMed]
- Townsend, D.M.; Tew, K.D. The role of glutathione-s-transferase in anti-cancer drug resistance. Oncogene 2003, 22, 7369–7375. [Google Scholar] [CrossRef]
- Kensler, T.W.; Qian, G.S.; Chen, J.G.; Groopman, J.D. Translational strategies for cancer prevention in liver. Nat. Rev. Cancer 2003, 3, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Siles, S.A.; Srinivasan, A.; Pierce, C.G.; Lopez-Ribot, J.L.; Ramasubramanian, A.K. High-throughput screening of a collection of known pharmacologically active small compounds for identification of Candida albicans biofilm inhibitors. Antimicrob. Agents Chemother. 2013, 57, 3681–3687. [Google Scholar] [CrossRef] [PubMed]
- Hayek, S.R.; Lee, S.A.; Parra, K.J. Advances in targeting the vacuolar proton-translocating ATPase (V-ATPase) for anti-fungal therapy. Front. Pharmacol. 2014, 5. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.Y.; Prudom, C.; Raines, S.M.; Charkhzarrin, S.; Melman, S.D.; de Haro, L.P.; Allen, C.; Lee, S.A.; Sklar, L.A.; Parra, K.J. Inhibitors of V-ATPase proton transport reveal uncoupling functions of tether linking cytosolic and membrane domain of v0 subunit a (vph1p). J. Biol. Chem. 2012, 287, 10236–10250. [Google Scholar] [CrossRef] [PubMed]
- Fraser, C.M.; Casjens, S.; Hang, W.M.; Sutton, G.G.; Clayton, R.; Lathigra, R.; White, O.; Ketchum, K.A.; Dodson, R.; Hickey, E.K.; et al. Genomic sequence of a lyme disease spirochaete, Borrelia burgdorferi. Nature 1997, 390, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Daull, P.; Lallemand, F.; Garrique, J.S. Benefits of cetalkonium chloride cationic oil-in-water nanoemulsions for topical opthalmic drug delivery. J. Pharm. Pharmacol. 2014, 66, 531–541. [Google Scholar] [CrossRef] [PubMed]
- Noecker, R. Effects of common ophthalmic preservatives on ocular health. Adv. Ther. 2001, 18, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Cabo, M.L.; Herrera, J.J.; Crespo, M.D.; Pastoriza, L. Comparison among the effectiveness of ozone, nisin and benzalkonium chloride for the elimination of planktonic cells and biofilms of Staphylococcus aureus cect4459 on polypropylene. Food Control 2009, 20, 521–525. [Google Scholar] [CrossRef]
- Zhang, Y.; Wade, M.M.; Scorpio, A.; Zhang, H.; Sun, Z. Mode of action of pyrazinamide: Disruption of Mycobacterium tuberculosis membrane transport and energetics by pyrazinoic acid. J. Antimicrob. Chemother. 2003, 52, 790–795. [Google Scholar] [CrossRef] [PubMed]
- Niu, H.; Cui, P.; Shi, W.; Zhang, S.; Feng, J.; Wang, Y.; Sullivan, D.; Zhu, B.; Zhang, Y. Identification of anti-persister activity against uropathogenic Escherichia coli from a clinical drug library. Antibiotics 2015, 4, 179–187. [Google Scholar] [CrossRef]
- Hurdle, J.G.; O’Neill, A.J.; Chopra, I.; Lee, R.E. Targeting bacterial membrane function: An underexploited mechanism for treating persistent infections. Nat. Rev. Microbiol. 2011, 9, 62–75. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Shi, W.; Zhang, S.; Zhang, Y. Persister mechanisms in Borrelia burgdorferi: Implications for improved intervention. Emerg. Microbes Infect. 2015, 4. [Google Scholar] [CrossRef]
- Sharma, B.; Brown, A.V.; Matluck, N.E.; Hu, L.T.; Lewis, K. Borrelia burgdorferi, the causative agent of lyme disease, forms drug-tolerant persister cells. Antimicrob. Agents Chemother. 2015, 59, 4616–4624. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Wang, T.; Zhang, S.; Shi, W.; Zhang, Y. An optimized SYBR Green I/PI assay for rapid viability assessment and antibiotic susceptibility testing for Borrelia burgdorferi. PLoS ONE 2014, 9, e111809. [Google Scholar] [CrossRef] [PubMed]
- Baell, J.; Walters, M.A. Chemistry: Chemical con artists foil drug discovery. Nature 2014, 513, 481–483. [Google Scholar] [CrossRef] [PubMed]
- PUBCHEM PROMISCUITY. Available online: http://chemutils.florida.scripps.edu:8080/pcpromiscuity/pcpromiscuity.html (accessed on 5 June 2015).
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feng, J.; Weitner, M.; Shi, W.; Zhang, S.; Sullivan, D.; Zhang, Y. Identification of Additional Anti-Persister Activity against Borrelia burgdorferi from an FDA Drug Library. Antibiotics 2015, 4, 397-410. https://doi.org/10.3390/antibiotics4030397
Feng J, Weitner M, Shi W, Zhang S, Sullivan D, Zhang Y. Identification of Additional Anti-Persister Activity against Borrelia burgdorferi from an FDA Drug Library. Antibiotics. 2015; 4(3):397-410. https://doi.org/10.3390/antibiotics4030397
Chicago/Turabian StyleFeng, Jie, Megan Weitner, Wanliang Shi, Shuo Zhang, David Sullivan, and Ying Zhang. 2015. "Identification of Additional Anti-Persister Activity against Borrelia burgdorferi from an FDA Drug Library" Antibiotics 4, no. 3: 397-410. https://doi.org/10.3390/antibiotics4030397
APA StyleFeng, J., Weitner, M., Shi, W., Zhang, S., Sullivan, D., & Zhang, Y. (2015). Identification of Additional Anti-Persister Activity against Borrelia burgdorferi from an FDA Drug Library. Antibiotics, 4(3), 397-410. https://doi.org/10.3390/antibiotics4030397






