Burden of Clostridioides difficile Infection and Risk Factors for Recurrences in an Italian Tertiary Care University Hospital: A Prospective Observational Study
Abstract
1. Introduction
2. Objectives
- Characterizing CDI cases in terms of incidence, demographics, hospital ward distribution, clinical characteristics, severity, mortality, and treatment strategies.
- Assessing factors associated with severe CDI presentations.
- Examining predictors of death during CDI.
- Evaluating factors associated with bloodstream infections (bacteremia or candidemia) within 60 days of CDI onset.
3. Materials and Methods
- Epidemiological data (age, sex, nationality);
- Date and hospital ward where CDI onset occurred, and length of hospital stay (LOS);
- Presence of known CDI risk factors at the time of diagnosis, including chronic use of antacids or PPIs, infections and/or antibiotic therapy within the previous 3 months, immunosuppression, prior hospitalization or transfer from another healthcare facility within the preceding 3 months, abdominal surgery within 3 months before CDI onset, inflammatory bowel disease, chronic kidney disease, and liver cirrhosis;
- Comorbidities;
- Concurrent infections and associated antimicrobial therapies;
- CDI-related characteristics, including primary or secondary episode, healthcare-associated or community-acquired form, clinical presentation, laboratory findings (leukocyte count, C-reactive protein (CRP), procalcitonin (PCT), serum creatinine, serum albumin), diagnostic test results, severity classification according to ZAR score (according to Zar et al., 2007 [26] a validated clinical tool derived from hospitalized patient cohorts that incorporates age, temperature, leukocyte count, serum albumin, and comorbidities to stratify patients according to the risk of severe disease and CDI-related mortality) or ESCMID criteria, and treatment administered;
- All-cause mortality during the CDI episode, occurrence of bacteremia or candidemia within 60 days of CDI onset, and CDI recurrence.
4. Results
4.1. Distribution, Incidence, and Patient Features
4.2. Concomitant Infection
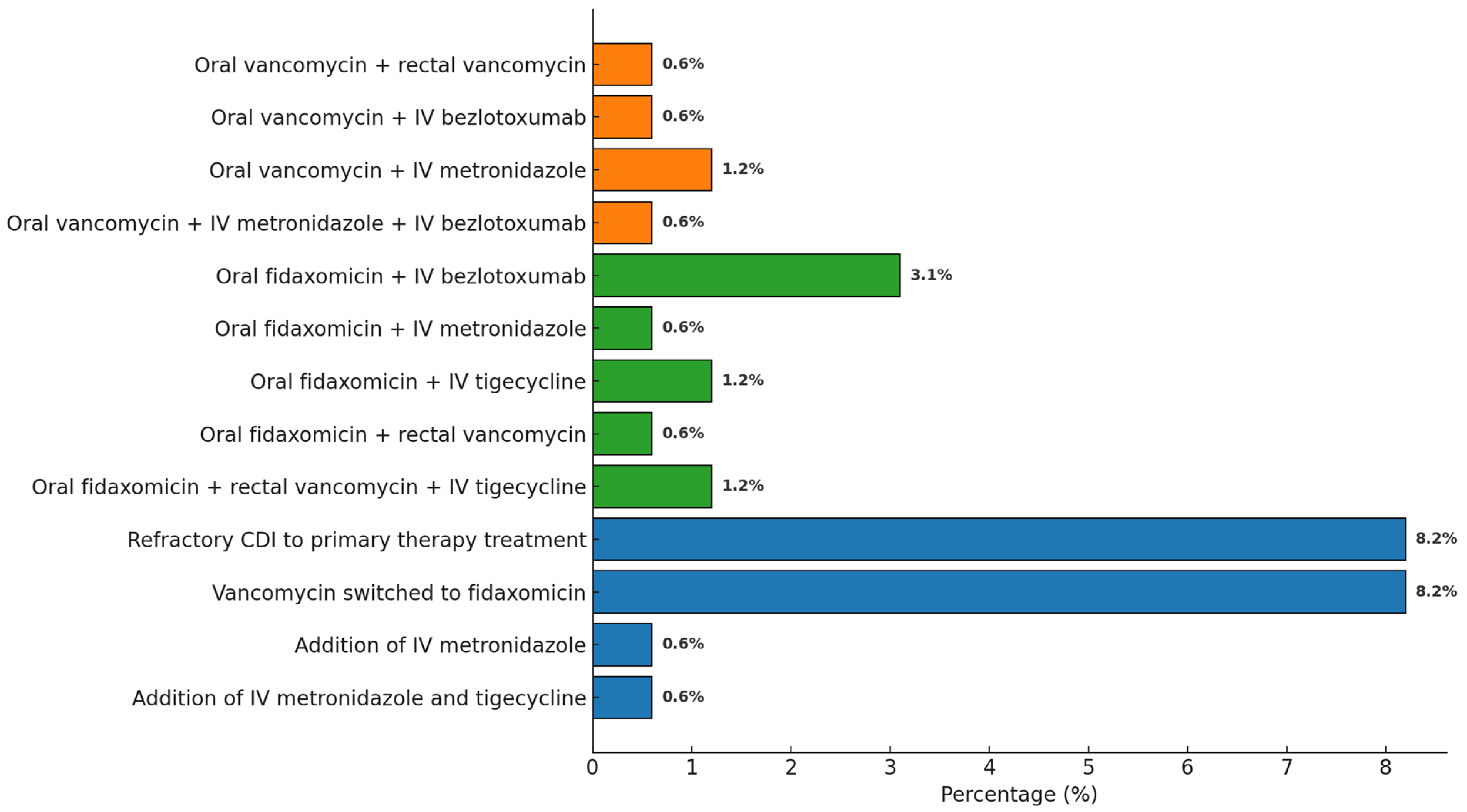
4.3. Presentation of CDI and Management
4.4. CDI and Outcomes
4.4.1. Recurrent CDI
4.4.2. Death During CDI
4.4.3. BSI
5. Discussion
Study Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ABSSSI | Acute bacterial skin and skin structure infections |
| BSI | Bloodstream infection |
| CA-CDI | Community-acquired Clostridioides difficile infection |
| CCI | Charlson comorbidity index |
| CD | Clostridioides difficile |
| CDI | Clostridioides difficile infection |
| CI | Confidence interval |
| CKD | Chronic kidney disease |
| CNSI | Central nervous system infection |
| CRP | C-reactive protein |
| ECDC | European centre for disease prevention and control |
| ESCMID | European society of clinical microbiology and infectious diseases |
| GDH | Glutamate dehydrogenase |
| HA-CDI | Healthcare-associated Clostridioides difficile infection |
| HAI | Healthcare-associated infection |
| IAI | Intra-abdominal infection |
| IBD | Inflammatory bowel disease |
| iCDI | Initial CDI |
| ID | Infectious disease |
| IDSA | Infectious Diseases Society of America |
| IL | Interleukin |
| IM | Intramuscolar |
| IQR | Interquartile range |
| IV | Intravenous |
| LOS | Length of hospital stay |
| LTCF | Long-term care facility |
| NAAT | Nucleic acid amplification test |
| OR | Odds ratio |
| pCDI | Primary CDI |
| PCR | Polymerase chain reaction |
| PCT | Procalcitonin |
| PNA | Pneumonia |
| PPI | Proton pump inhibitor |
| rCDI | Recurrent CDI |
| sCDI | Secondary CDI |
| SD | Standard deviation |
| TOX | Toxin |
| UTI | Urinary tract infection |
| WBC | White blood cell |
References
- Smits, W.K.; Lyras, D.; Lacy, D.B.; Wilcox, M.H.; Kuijper, J. Clostridium Difficile Infection. Nat. Rev. Dis. Primers 2016, 2, 16020. [Google Scholar] [CrossRef]
- Sandhu, B.K.; McBride, S.M. Clostridioides difficile. Trends Microbiol. 2018, 26, 1049–1050. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Clostridioides difficile infections. In Annual Epidemiological Report for 2018−2020; ECDC: Stockholm, Sweden, 2024. [Google Scholar]
- ECDC. Surveillance Report Annual Epidemiological Report for 2016 Clostridium Difficile Infections; ECDC: Stockholm, Sweden, 2018. [Google Scholar]
- Medaglia, A.A.; Buffa, S.; Gioè, C.; Bonura, S.; Rubino, R.; Iaria, C.; Colomba, C.; Cascio, A. An emergent infectious disease: Clostridioides difficile infection hospitalizations, 10-year trend in Sicily. Infection 2021, 49, 1221–1229, Correction in Infection 2021, 49, 1231. https://doi.org/10.1007/s15010-021-01700-y. [Google Scholar] [CrossRef]
- Nour, C.; Chakra, A.; Pepin, J.; Sirard, S.; Valiquette, L. Risk Factors for Recurrence, Complications and Mortality in Clostridium difficile Infection: A Systematic Review; National Institutes of Health: Bethesda, MD, USA, 2014. [Google Scholar] [CrossRef]
- Wingen-Heimann, S.M.; Davies, K.; Viprey, V.F.; Davis, G.; Wilcox, M.H.; Vehreschild, M.J.; Lurienne, L.; Bandinelli, P.-A.; Cornely, O.A.; Vilken, T.; et al. Clostridioides difficile infection (CDI): A pan-European multi-center cost and resource utilization study, results from the Combatting Bacterial Resistance in Europe CDI (COMBACTE-CDI). Clin. Microbiol. Infect. 2023, 29, 651.e1–651.e8. [Google Scholar] [CrossRef]
- Granata, G.; Petrosillo, N.; Adamoli, L.; Bartoletti, M.; Bartoloni, A.; Basile, G.; Bassetti, M.; Bonfanti, P.; Borromeo, R.; Ceccarelli, G.; et al. Prospective Study on Incidence, Risk Factors and Outcome of Recurrent Clostridioides difficile Infections. J. Clin. Med. 2021, 10, 1127. [Google Scholar] [CrossRef]
- Johnson, S.; Lavergne, V.; Skinner, A.M.; Gonzales-Luna, A.J.; Garey, K.W.; Kelly, C.P.; Wilcox, M.H. Clinical Practice Guideline by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA): 2021 Focused Update Guidelines on Management of Clostridioides difficile Infection in Adults. Clin. Infect. Dis. 2021, 73, e1029–e1044. [Google Scholar] [CrossRef]
- van Prehn, J.; Reigadas, E.; Vogelzang, E.H.; Bouza, E.; Hristea, A.; Guery, B.; Krutova, M.; Norén, T.; Allerberger, F.; Coia, J.E.; et al. European Society of Clinical Microbiology and Infectious Diseases: 2021 update on the treatment guidance document for Clostridioides difficile infection in adults. Clin. Microbiol. Infect. 2021, 27, S1–S21. [Google Scholar] [CrossRef]
- van Rossen, T.M.; Ooijevaar, R.E.; Vandenbroucke-Grauls, C.M.; Dekkers, O.M.; Kuijper, E.J.; Keller, J.J.; van Prehn, J. Prognostic factors for severe and recurrent Clostridioides difficile infection: A systematic review. Clin. Microbiol. Infect. 2022, 28, 321–331. [Google Scholar] [CrossRef]
- Finn, E.; Andersson, F.L.; Madin-Warburton, M. Burden of Clostridioides difficile infection (CDI)-a systematic review of the epidemiology of primary and recurrent CDI. BMC Infect. Dis. 2021, 21, 456. [Google Scholar] [CrossRef] [PubMed]
- Pépin, J.; Alary, M.-E.; Valiquette, L.; Raiche, E.; Ruel, J.; Fulop, K.; Godin, D.; Bourassa, C. Increasing risk of relapse after treatment of Clostridium difficile colitis in Quebec, Canada. Clin. Infect. Dis. 2005, 40, 1591–1597. [Google Scholar] [CrossRef] [PubMed]
- Sheitoyan-Pesant, C.; Abou Chakra, C.N.; Pépin, J.; Marcil-Héguy, A.; Nault, V.; Valiquette, L. Clinical and Healthcare Burden of Multiple Recurrences of Clostridium difficile Infection. Clin. Infect. Dis. 2016, 62, 574–580. [Google Scholar] [CrossRef]
- Medaglia, A.A.; Mancuso, A.; Albano, C.; Zinna, G.; Pipitò, L.; Calà, C.; Immordino, R.; Rubino, R.; Bonura, S.; Canino, B.; et al. Clostridioides difficile Infection in an Italian Tertiary Care University Hospital: A Retrospective Analysis. Antibiotics 2023, 12, 837. [Google Scholar] [CrossRef]
- Meschiari, M.; Cozzi-Lepri, A.; Cervo, A.; Granata, G.; Rogati, C.; Franceschini, E.; Casolari, S.; Tatarelli, P.; Giacobbe, D.R.; Bassetti, M.; et al. Efficacy of bezlotoxumab in preventing the recurrence of Clostridioides difficile infection: An Italian multicenter cohort study. Int. J. Infect. Dis. 2023, 131, 147–154. [Google Scholar] [CrossRef]
- Bassetti, M.; Cascio, A.; De Rosa, F.G.; Meschiari, M.; Parrella, R.; Petrosillo, N.; Armuzzi, A.; Caprioli, F.; Dentali, F.; Pani, M.; et al. Management of Clostridioides difficile infection: An Italian Delphi consensus. J. Antimicrob. Chemother. 2024, 79, 2103–2118. [Google Scholar] [CrossRef]
- Pipitone, G.; Granata, G.; Sartelli, M.; Gizzi, A.; Imburgia, C.; Cascio, A.; Iaria, C. Intravenous metronidazole for fulminant Clostridioides difficile infection. Clin. Microbiol. Infect. 2023, 29, 656–657. [Google Scholar] [CrossRef]
- Pipitone, G.; Granata, G.; Sartelli, M.; Gizzi, A.; Imburgia, C.; Marsala, L.; Cascio, A.; Iaria, C. On the use of intravenous metronidazole for severe and complicated Clostridioides difficile infection: A review and meta-analysis. Infez. Med. 2024, 32, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Pipitone, G.; Iaria, C.; Granata, G.; Cascio, A.; Maraolo, A.E. Which trials do we need? Fidaxomicin plus either intravenous metronidazole or tigecycline versus vancomycin plus either intravenous metronidazole or tigecycline for fulminant Clostridioides difficile infection. Clin. Microbiol. Infect. 2025, 31, 315–318. [Google Scholar] [CrossRef]
- Russo, A.; Falcone, M.; Fantoni, M.; Murri, R.; Masucci, L.; Carfagna, P.; Ghezzi, M.; Posteraro, B.; Sanguinetti, M.; Venditti, M. Risk factors and clinical outcomes of candidaemia in patients treated for Clostridium difficile infection. Clin. Microbiol. Infect. 2015, 21, 493.e1–493.e4. [Google Scholar] [CrossRef]
- Tsay, S.; Williams, S.R.; Benedict, K.; Beldavs, Z.; Farley, M.; Harrison, L.; Schaffner, W.; Dumyati, G.; Blackstock, A.; Guh, A.; et al. A Tale of Two Healthcare-Associated Infections: Clostridium difficile Coinfection Among Patients with Candidemia. Clin. Infect. Dis. 2019, 68, 676. [Google Scholar] [CrossRef] [PubMed]
- Giuliano, S.; Guastalegname, M.; Jenco, M.; Morelli, A.; Falcone, M.M.; Venditti, M. Severe community onset healthcare-associated Clostridium difficile infection complicated by carbapenemase producing Klebsiella pneumoniae bloodstream infection. BMC Infect. Dis. 2014, 14, 475. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, R.J.; Santhosh, K.; Mogle, J.A.; Young, V.B.; Rao, K. Is Clostridium difficile infection a Risk Factor for Subsequent Bloodstream Infection? Anaerobe 2017, 48, 27. [Google Scholar] [CrossRef]
- Brenchley, J.M.; Douek, D.C. Microbial Translocation Across the GI Tract. Annu. Rev. Immunol. 2012, 30, 149. [Google Scholar] [CrossRef]
- Zar, F.A.; Bakkanagari, S.R.; Moorthi, K.M.; Davis, M.B. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin. Infect. Dis. 2007, 45, 302–307. [Google Scholar] [CrossRef]
- Louie, T.J.; Miller, M.A.; Mullane, K.M.; Weiss, K.; Lentnek, A.; Golan, Y.; Gorbach, S.; Sears, P.; Shue, Y.K. OPT-80-003 Clinical Study Group. Fidaxomicin versus vancomycin for Clostridium difficile infection. N. Engl. J. Med. 2011, 364, 422–431. [Google Scholar] [CrossRef] [PubMed]
- Cornely, A.O.; Crook, D.W.; Esposito, R.; Poirier, A.; Somero, M.S.; Weiss, K.; Sears, P.; Gorbach, S. Fidaxomicin versus vancomycin for infection with Clostridium difficile in Europe, Canada, and the USA: A double-blind, non-inferiority, randomised controlled trial. Lancet Infect. Dis. 2012, 12, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Wu, Y.; Geng, X.; Yuan, C.; Fu, Y.; Yang, G. Efficacy of fidaxomicin versus vancomycin in the treatment of Clostridium difficile infection: A systematic meta-analysis. Medicine 2024, 103, e39213. [Google Scholar] [CrossRef]
- Negrut, N.; Bungau, S.; Behl, T.; Khan, S.A.; Vesa, C.M.; Bustea, C.; Nistor-Cseppento, D.C.; Rus, M.; Pavel, F.-M.; Tit, D.M. Risk Factors Associated with Recurrent Clostridioides difficile Infection. Healthcare 2020, 8, 352. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Simmonds, A.; Kubin, C.J.; Furuya, E.Y. Comparison of 3 severity criteria for Clostridium difficile infection. Infect Control Hosp. Epidemiol. 2014, 35, 196–199. [Google Scholar] [CrossRef] [PubMed]
- Czepiel, J.; Krutova, M.; Mizrahi, A.; Khanafer, N.; Enoch, D.A.; Patyi, M.; Deptuła, A.; Agodi, A.; Nuvials, X.; Pituch, H.; et al. Mortality Following Clostridioides difficile Infection in Europe: A Retrospective Multicenter Case-Control Study. Antibiotics 2021, 10, 299. [Google Scholar] [CrossRef]
- Katzer, K.C.; Hagel, S.; Reuken, P.A.; Bruns, T.; Stallmach, A. Development and validation of a simple and robust model to predict 30-day mortality in patients with Clostridioides difficile-associated enterocolitis. BMJ Open Gastroenterol. 2020, 7, e000468. [Google Scholar] [CrossRef]
- Khanafer, N.; Barbut, F.; Eckert, C.; Perraud, M.; Demont, C.; Luxemburger, C.; Vanhems, P. Factors predictive of severe Clostridium difficile infection depend on the definition used. Anaerobe 2016, 37, 43–48. [Google Scholar] [CrossRef] [PubMed]


| Laboratory Parameters | Median (Interquartile Range) Mean ± SD |
|---|---|
| WBC (N°/mmc) | 9990 (6820–14,040) 12,719 ± 10,333 |
| Basal creatininemia (mg/dL) | 1.05 (0.81–2.00) 1.77 ± 1.66 |
| Creatininemia during CDI | 0.96 (0.68–1.68) 1.56 ± 1.54 |
| CRP (mg/L) | 48.8 (18.8–117) 81.6 ± 84.7 |
| PCT (mcg/L) | 0.511 (0.201–1.487) 5.268 ± 14.672 |
| Variables | rCDI (n = 17) | Non rCDI (n = 110) | OR | CI | p-Value |
|---|---|---|---|---|---|
| Univariate analysis | |||||
| Oral vancomycin | 15 (11.8%) | 79 (62.1%) | 6.17 | 1.36–27.97 | 0.008 |
| Rectal vancomycin | 2 (1.6%) | 2 (1.6%) | 9.47 | 1.24–72.15 | 0.056 |
| Fidaxomicin | 2 (1.6%) | 63 (49.6%) | 0.17 | 0.04–0.78 | 0.016 |
| rCDI (presenting CDI) | 2 (1.6%) | 2 (1.6%) | 9.47 | 1.24–72.15 | 0.056 |
| Dysphagia | 4 (3.1%) | 9 (7.1%) | 4.61 | 1.25–17.07 | 0.034 |
| Increased creatininemia | 9 (7.1%) | 43 (33.8%) | 2.64 | 0.96–7.31 | 0.054 |
| Peripheral vascular disease | 9 (7.1%) | 23 (18.1%) | 5.92 | 2.07–16.94 | <0.001 |
| Multivariable analysis | |||||
| Oral vancomycin | 15 (11.8%) | 79 (62.1%) | 15.03 | 2.03–111.25 | 0.008 |
| Dysphagia | 4 (3.1%) | 9 (7.1%) | 2.18 | 0.35–13.60 | 0.403 |
| Peripheral vascular disease | 9 (7.1%) | 23 (18.1%) | 7.27 | 2.05–25.78 | 0.002 |
| Age ≥ 65 years | 11 (8.7%) | 106 (83.5%) | 0.60 | 0.17–2.10 | 0.423 |
| rCDI (presenting CDI) | 2 (1.6%) | 2 (1.6%) | 6.50 | 0.69–61.12 | 0.102 |
| ZAR score ≥ 2 | 8 (6.3%) | 45 (35.4%) | 1.56 | 0.45–5.43 | 0.481 |
| Recent hospitalization * | 9 (7.1%) | 77 (60.6%) | 1.30 | 0.29–5.76 | 0.729 |
| Transfer from nursing home/LTCF | 4 (3.1%) | 18 (14.2%) | 1.84 | 0.35–9.97 | 0.475 |
| Recent antibiotic use * | 8 (6.3%) | 73 (57.5%) | 0.65 | 0.14–2.95 | 0.580 |
| Variables | Death During CDI (n = 15) | Survivors (n = 146) | OR | 95% CI | p-Value |
|---|---|---|---|---|---|
| Univariate analysis | |||||
| Age > 77 years * | 12 (7.5%) | 68 (42.2%) | 1.58 | 0.54–4.68 | 0.014 |
| Transfer from nursing home/LTCF * | 6 (3.7%) | 16 (9.9%) | 5.42 | 1.70–17.21 | 0.002 |
| Lymphoma | 2 (1.2%) | 1 (0.6%) | 22.31 | 1.89–262.84 | 0.023 |
| Hematological malignancy | 3 (1.9%) | 6 (3.7%) | 5.83 | 1.29–26.30 | 0.039 |
| Peripheral vascular disease | 6 (3.7%) | 26 (16.1%) | 3.08 | 1.01–9.40 | 0.040 |
| Connective tissue disease | 2 (1.2%) | 1 (0.6%) | 22.31 | 1.89–262.84 | 0.023 |
| Immobilization syndrome | 11 (6.8%) | 49 (30.4%) | 5.44 | 1.65–17.98 | 0.002 |
| Dysphagia | 4 (2.5%) | 9 (5.6%) | 5.53 | 1.47–20.89 | 0.021 |
| Increased lactates (>1 mmol/L) | 6 (3.7%) | 20 (12.4%) | 3.70 | 1.08–12.72 | 0.029 |
| CRP > 48.8 mg/L * during CDI | 10 (6.2%) | 67 (41.6%) | 3.53 | 0.93–13.39 | 0.050 |
| Septic shock | 7 (4.3%) | 2 (1.2%) | 63.00 | 11.22–353.66 | <0.001 |
| Severe or severe-complicated CDI (ESCMID criteria) | 10 (6.2%) | 55 (34.2%) | 3.31 | 1.07–10.12 | 0.029 |
| Severe-complicated CDI (ESCMID criteria) | 7 (4.3%) | 13 (8.1%) | 8.95 | 2.80–28.65 | <0.001 |
| WBC > 15,000/mm3 during CDI | 7 (4.3%) | 29 (18.0%) | 3.53 | 1.18–10.53 | 0.018 |
| ZAR score ≥ 2 | 10 (6.2%) | 43 (26.7%) | 4.79 | 1.55–14.84 | 0.003 |
| Contextual BSI | 5 (3.1%) | 18 (11.2%) | 3.56 | 1.09–11.59 | 0.027 |
| Contextual PNA | 10 (6.2%) | 45 (28.0%) | 4.49 | 1.45–13.89 | 0.005 |
| Multivariable analysis | |||||
| Age > 77 years * | 12 (7.5%) | 68 (42.2%) | 0.58 | 0.13–2.60 | 0.475 |
| Transfer from nursing home/LTCF * | 6 (3.7%) | 16 (9.9%) | 4.13 | 0.75–22.86 | 0.104 |
| Lymphoma | 2 (1.2%) | 1 (0.6%) | 22.87 | 1.05–497.15 | 0.046 |
| Hematological malignancy | 3 (1.9%) | 6 (3.7%) | 6.54 | 0.58–73.87 | 0.129 |
| Severe or severe-complicated CDI (ESCMID criteria) | 10 (6.2%) | 55 (34.2%) | 0.53 | 0.03–8.11 | 0.651 |
| Severe-complicated CDI (ESCMID criteria) | 7 (4.3%) | 13 (8.1%) | 4.14 | 0.53–32.48 | 0.176 |
| ZAR score ≥ 2 | 10 (6.2%) | 43 (26.7%) | 2.38 | 0.17–33.51 | 0.520 |
| Septic shock | 7 (4.3%) | 2 (1.2%) | 34.94 | 4.19–291.53 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Gagliano, M.C.; D’Agati, G.; Medaglia, A.A.; Pipitò, L.; Catania, B.; Conti, C.; Tuttolomondo, A.; Cefalù, A.B.; Cammà, C.; Scichilone, N.; et al. Burden of Clostridioides difficile Infection and Risk Factors for Recurrences in an Italian Tertiary Care University Hospital: A Prospective Observational Study. Antibiotics 2026, 15, 23. https://doi.org/10.3390/antibiotics15010023
Gagliano MC, D’Agati G, Medaglia AA, Pipitò L, Catania B, Conti C, Tuttolomondo A, Cefalù AB, Cammà C, Scichilone N, et al. Burden of Clostridioides difficile Infection and Risk Factors for Recurrences in an Italian Tertiary Care University Hospital: A Prospective Observational Study. Antibiotics. 2026; 15(1):23. https://doi.org/10.3390/antibiotics15010023
Chicago/Turabian StyleGagliano, Maria Chiara, Giulio D’Agati, Alice Annalisa Medaglia, Luca Pipitò, Bianca Catania, Claudia Conti, Antonino Tuttolomondo, Angelo Baldassare Cefalù, Calogero Cammà, Nicola Scichilone, and et al. 2026. "Burden of Clostridioides difficile Infection and Risk Factors for Recurrences in an Italian Tertiary Care University Hospital: A Prospective Observational Study" Antibiotics 15, no. 1: 23. https://doi.org/10.3390/antibiotics15010023
APA StyleGagliano, M. C., D’Agati, G., Medaglia, A. A., Pipitò, L., Catania, B., Conti, C., Tuttolomondo, A., Cefalù, A. B., Cammà, C., Scichilone, N., Licata, A., Barbagallo, M., Immordino, R., Virruso, R., Giammanco, G. M., & Cascio, A. (2026). Burden of Clostridioides difficile Infection and Risk Factors for Recurrences in an Italian Tertiary Care University Hospital: A Prospective Observational Study. Antibiotics, 15(1), 23. https://doi.org/10.3390/antibiotics15010023












