Development of an Effective and Cost-Saving Synergistic-Antibacterial Therapy for Prevention of Endophthalmitis
Abstract
1. Introduction
2. Results
2.1. Individual Antibiotic Eradication Ability
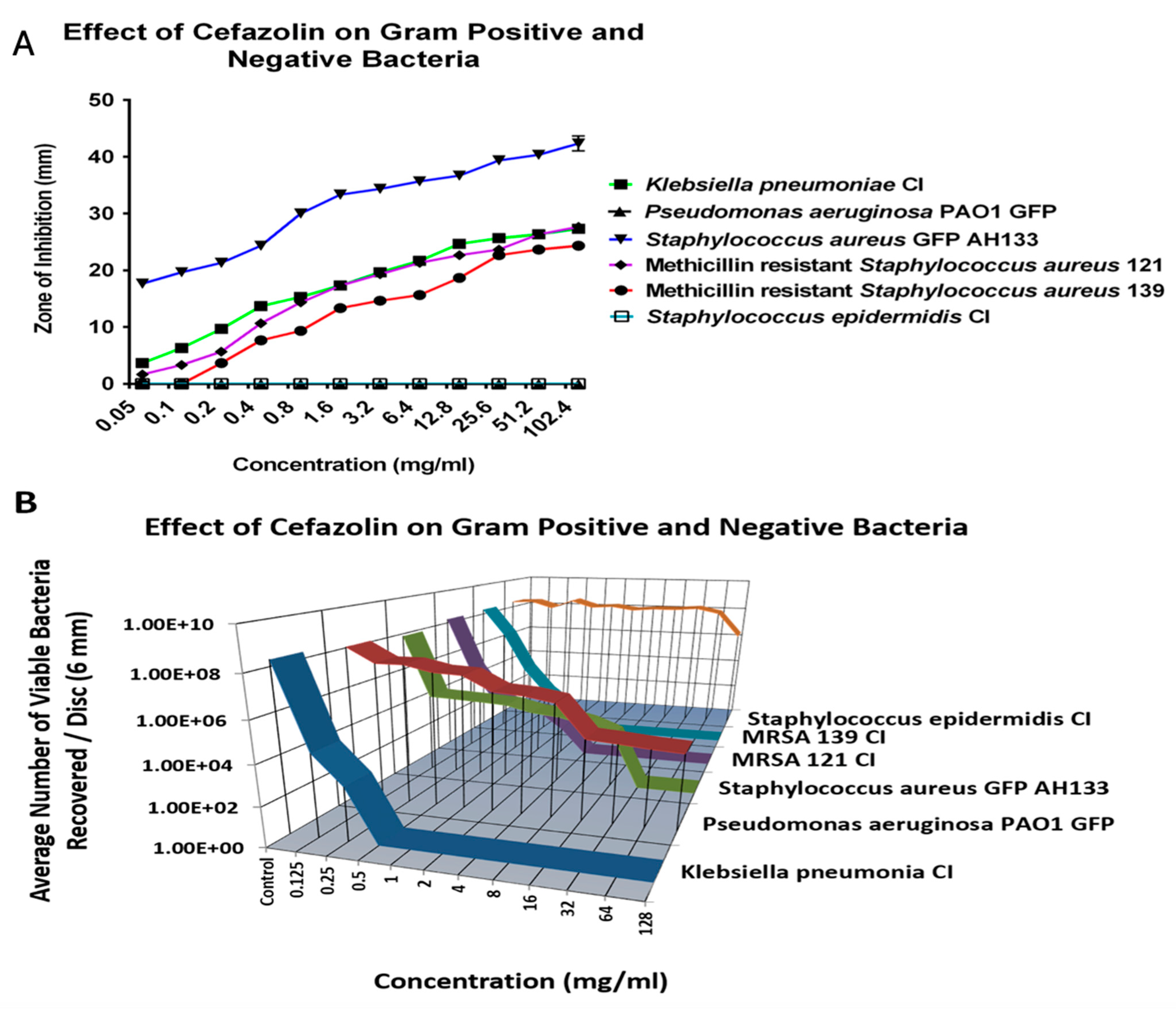
2.1.1. Cefazolin
2.1.2. Cefuroxime
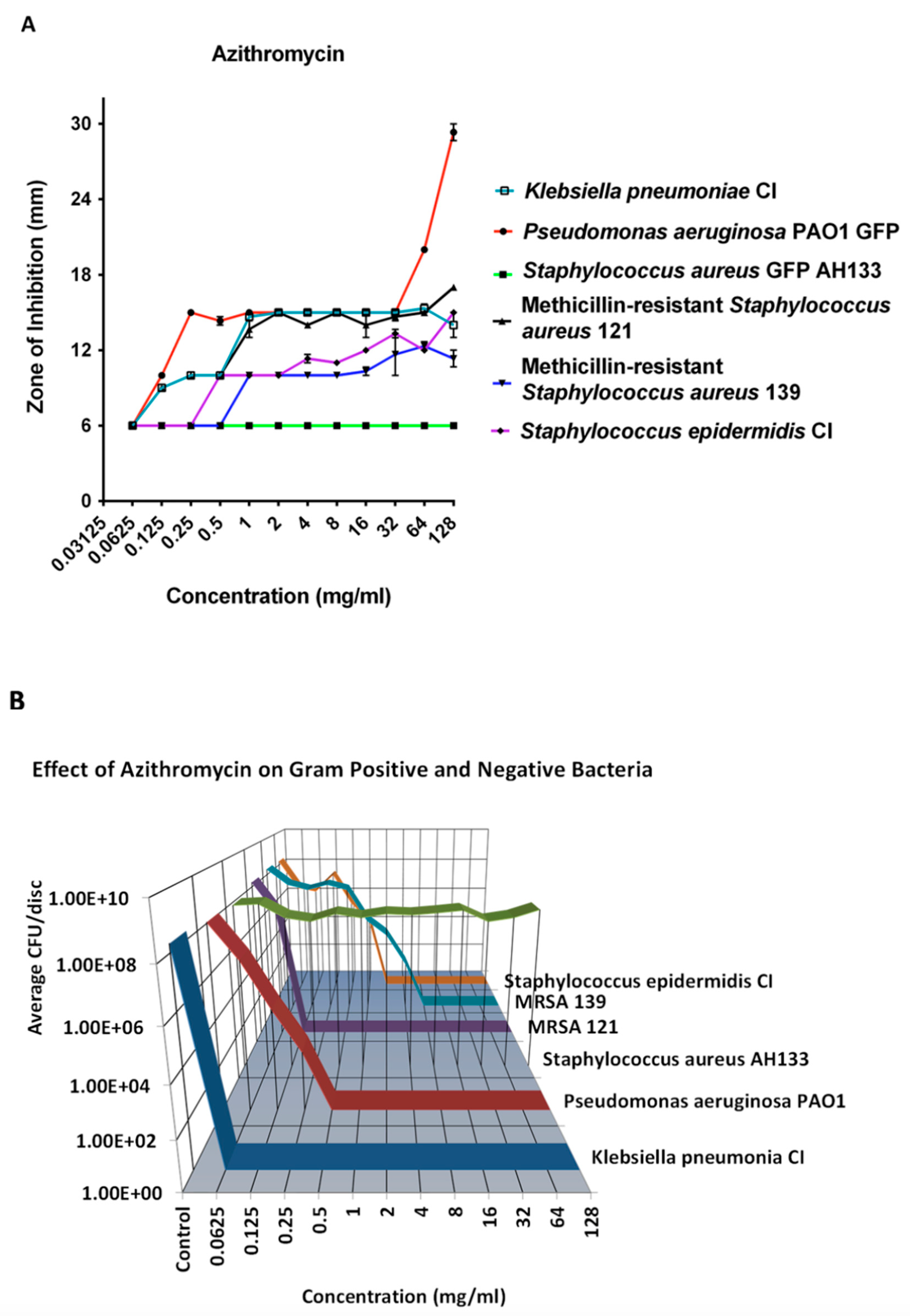
2.1.3. Azithromycin
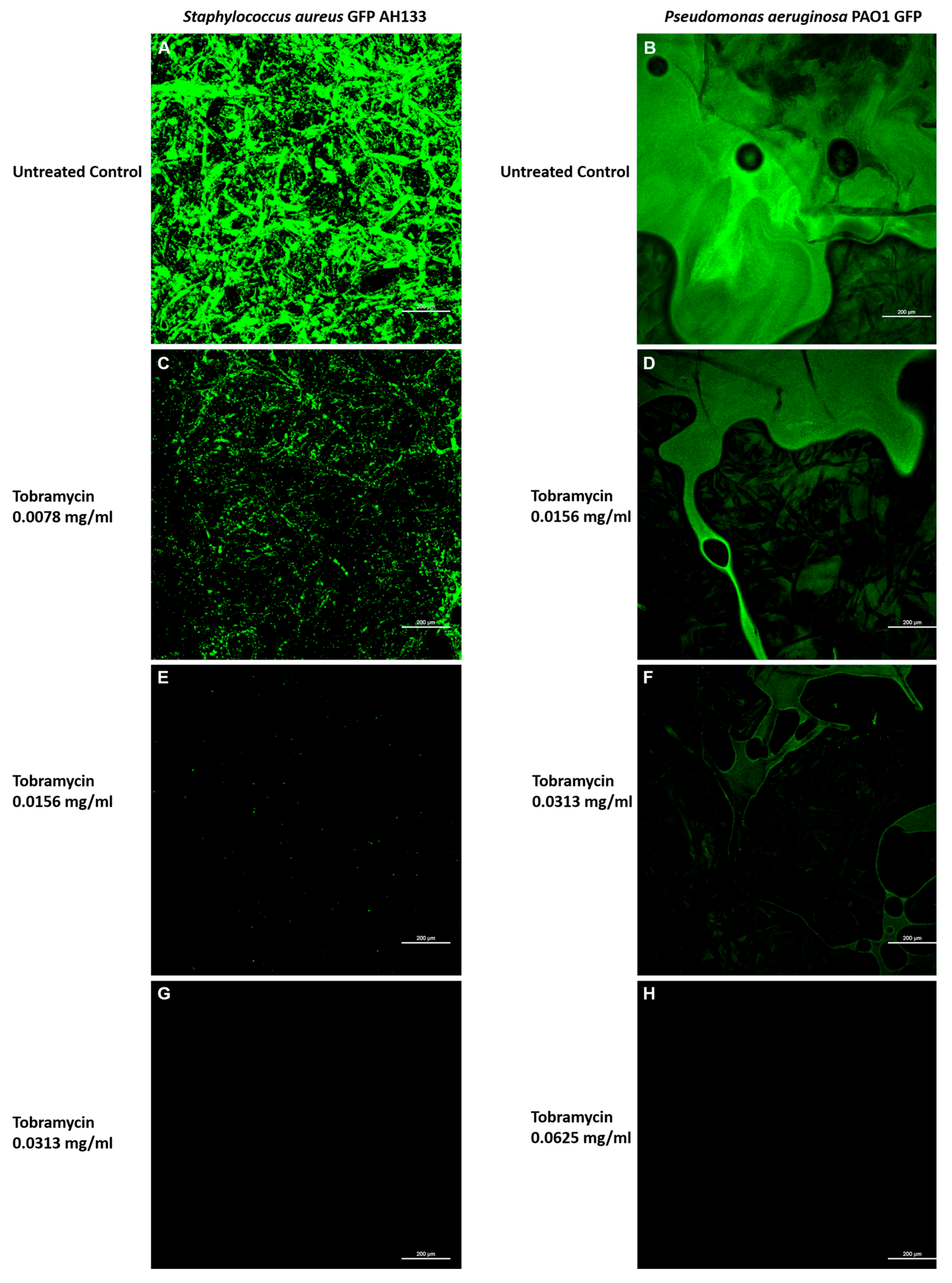
2.1.4. Tobramycin
2.1.5. Moxifloxacin and Gatifloxacin
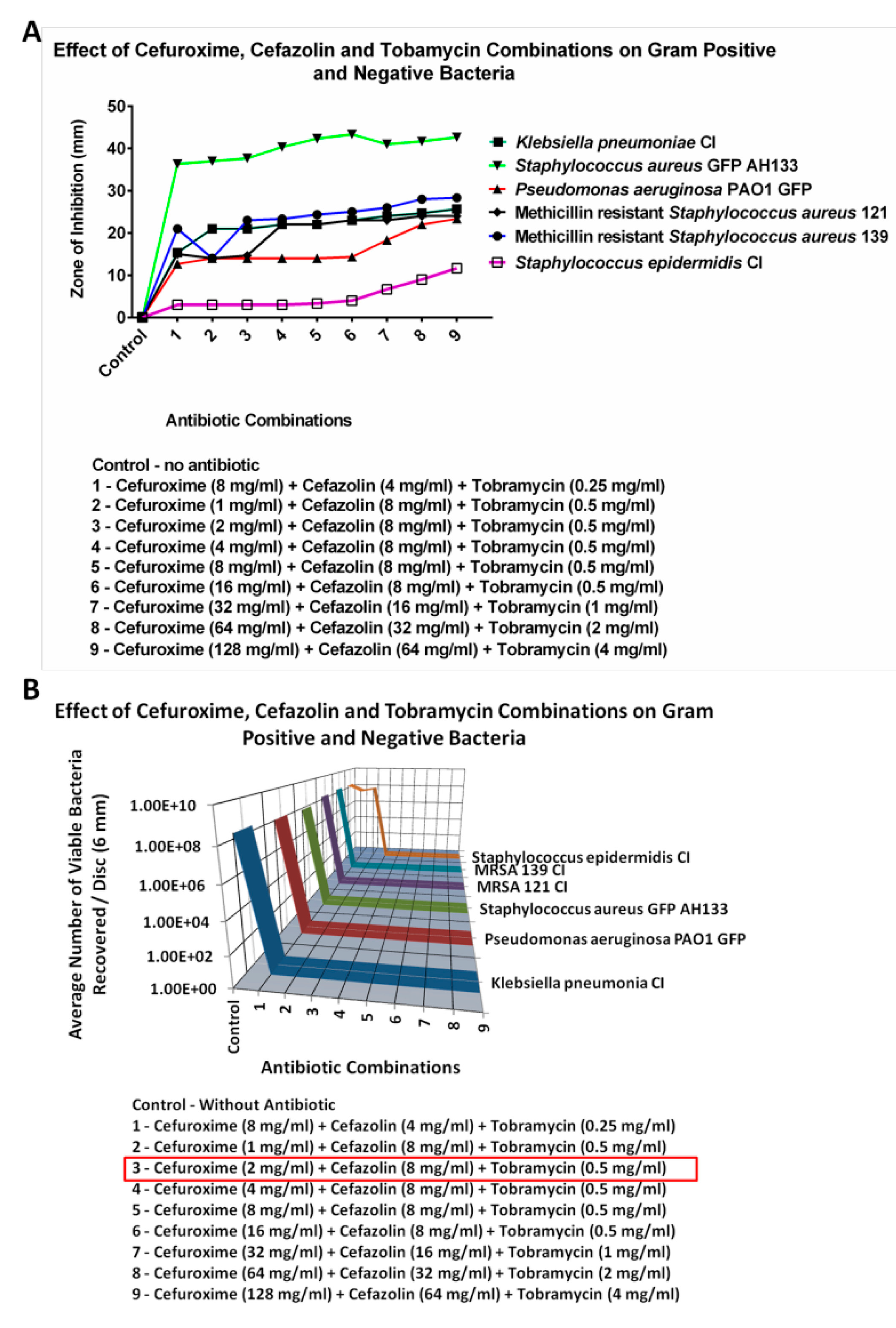
2.2. Combinations of Antimicrobials
2.2.1. Cefuroxime and Azithromycin
2.2.2. Cefuroxime/Tobramycin or Azithromycin/Tobramycin
2.2.3. Cefazolin
2.2.4. Zone of Inhibition Results
3. Discussion
4. Materials and Methods
4.1. Bacterial Strains, Media, and Growth Conditions
4.2. Antibiotic Solution Preparation
4.3. Disc Diffusion Assay
4.4. Confocal Laser Scanning Microscopy (CLSM) of the GFP Containing Bacteria
4.5. Determination of Colony Forming Units
4.6. Statistical Analyses
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Lundstrom, M.; Friling, E.; Montan, P. Risk factors for endophthalmitis after cataract surgery: Predictors for causative organisms and visual outcomes. J. Cataract. Refract. Surg. 2015, 41, 2410–2416. [Google Scholar] [CrossRef] [PubMed]
- Du, D.T.; Wagoner, A.; Barone, S.B.; Zinderman, C.E.; Kelman, J.A.; MaCurdy, T.E.; Forshee, R.A.; Worrall, C.M.; Izurieta, H.S. Incidence of endophthalmitis after corneal transplant or cataract surgery in a Medicare population. Ophthalmology 2014, 121, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Yan, W.; Fotis, K.; Prasad, N.M.; Lansingh, V.-C.; Taylor, R.; Finger, R.P.; Facciolo, D.; He, M. Cataract Surgical Rate and Socioeconomics: A Global Study. Invest. Ophth Vis. Sci. 2017, 57, 5872–5881. [Google Scholar] [CrossRef] [PubMed]
- Vaziri, K.; Schwartz, S.G.; Kishor, K.; Flynn, H.W., Jr. Endophthalmitis: State of the art. Clin. Ophthalmol. 2015, 9, 95–108. [Google Scholar]
- Friling, E.; Lundstrom, M.; Stenevi, U.; Montan, P. Six-year incidence of endophthalmitis after cataract surgery: Swedish national study. J. Cataract. Refract. Surg. 2013, 39, 15–21. [Google Scholar] [CrossRef]
- Keay; Gower, E.W.; Cassard, S.D.; Tielsch, J.M.; Schein, O.D. Post cataract surgery endophthalmitis in the United States: Analysis of the complete 2003 to 2004 Medicare database of cataract surgeries. Ophthalmology 2012, 119, 914–922. [Google Scholar] [CrossRef]
- Kaatz, G.W.; Seo, S.; Ruble, C.A. Effulx-Mediated Fluoroquinolone resistance in S. aureus. Antimicrob. Agents Chemother. 1993, 37, 1086–1094. [Google Scholar] [CrossRef]
- Schimel, A.M.; Miller, D.; Flynn, H.W. Evolving fluoroquinolone resistance among coagulase-negative Staphylococcus isolates causing endophthalmitis. Arch. Ophthalmol. 2012, 130, 1617–1618. [Google Scholar] [CrossRef]
- Abelson, M.; Forbes, M. The enigma of endophthalmitis. Rev. Ophthalmol. 2004, 11. [Google Scholar]
- Blomquist, P.H. Methicillin-Resistant Staphylococcus aureus infections of the eye and orbit (An American Ophthalmological Society Thesis). Trans. Am. Ophthalmol. Soc. 2006, 104, 322–345. [Google Scholar]
- Major, J.C., Jr.; Engelbert, M.; Flynn, H.W., Jr.; Miller, D.; Smiddy, W.E.; Davis, J.L. Staphylococcus aureus endophthalmitis: Antibiotic susceptibilities, methicillin resistance, and clinical outcomes. Am. J. Ophthalmol. 2010, 149, 278–283.e271. [Google Scholar] [CrossRef]
- Sharifi, E.; Porco, T.C.; Naseri, A. Cost-effectiveness analysis of intracameral cefuroxime use for prophylaxis of endophthalmitis after cataract surgery. Ophthalmology 2009, 116, 1887–1896.e1881. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.singlecare.com/ (accessed on 1 April 2025).
- Barry, P.; Seal, D.V.; Gettinby, G.; Lees, F.; Peterson, M.; Revie, C.W. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: Preliminary report of principal results from a European multicenter study. J. Cataract. Refract. Surg. 2006, 32, 407–410. [Google Scholar] [CrossRef] [PubMed]
- Fintelmann, R.E.; Naseri, A. Prophylaxis of postoperative endophthalmitis following cataract surgery: Current status and future directions. Drugs 2010, 70, 1395–1409. [Google Scholar] [CrossRef]
- Prophylaxis of postoperative endophthalmitis following cataract surgery: Results of the ESCRS multicenter study and identification of risk factors. J. Cataract. Refract. Surg. 2007, 33, 978–988. [CrossRef] [PubMed]
- Seal, D.V.; Barry, P.; Gettinby, G.; Lees, F.; Peterson, M.; Revie, C.W.; ESCRS Endophthalmitis Study Group. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: Case for a European multicenter study. J. Cataract. Refract. Surg. 2006, 32, 396–406. [Google Scholar] [CrossRef]
- Wejde, G.; Montan, P.; Lundstrom, M.; Stenevi, U.; Thorburn, W. Endophthalmitis following cataract surgery in Sweden: National prospective survey 1999–2001. Acta Ophthalmol. Scand. 2005, 83, 7–10. [Google Scholar] [CrossRef]
- Garat, M.; Moser, C.L.; Martin-Baranera, M.; Alonso-Tarres, C.; Alvarez-Rubio, L. Prophylactic intracameral cefazolin after cataract surgery: Endophthalmitis risk reduction and safety results in a 6-year study. J. Cataract. Refract. Surg. 2009, 5, 637–642. [Google Scholar] [CrossRef]
- Rhee, S.S.; Mah, F.S. Comparison of tobramycin 0.3%/dexamethasone 0.1% and tobramycin 0.3%, loteprednol 0.5% in the management of blepharo-keratoconjunctivitis. Adv. Ther. 2007, 24, 60–67. [Google Scholar] [CrossRef]
- Wilhelmus, K.R.; Gilbert, M.L.; Osato, M.S. Tobramycin in ophthalmology. Surv. Ophthalmol. 1987, 32, 111–122. [Google Scholar] [CrossRef]
- Tran, P.; Desai, A.; Luth, K.; Huynh, E.; Dong, H.; Dev, A.; Hamood, A.; Mitchell, K.; Reid, T.W. An in vitro Study of 2.5, 5.0, and 10% Providone-iodine (Betadine) Solutions in Inhibiting the Growth of Different Gram Negative and Gram Positive Pathogens Showed a Lack of Efficacy with Several Bacterial Species. J. Ophthalmol. Ophthalmic Surg. 2017, 2, 100–111. [Google Scholar]
- Malone, C.L.; Boles, B.R.; Lauderdale, K.J.; Thoendel, M.; Kavanaugh, J.S.; Horswill, A.R. Fluorescent reporters for Staphylococcus aureus. J. Microbiol. Methods 2009, 77, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Holloway, B.W.; Krishnapillai, V.; Morgan, A.F. Chromosomal genetics of Pseudomonas. Microbiol. Rev. 1979, 43, 73–102. [Google Scholar] [CrossRef] [PubMed]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Disc Susceptibility Tests, 35th ed.; Approved standard; CLSI publication M02-A10; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2025. [Google Scholar]
- Tran, P.; Hamood, A.; Mosley, T.; Gray, T.; Jarvis, C.; Reid, T.W. Organo-selenium containing dental sealant inhibits bacterial biofilm. J. Dent. Res. 2013, 92, 461–466. [Google Scholar] [CrossRef]
- Tweldemedhim, M.; Grebreyesus, H.; Atsbaha, A.H.; Asgendom, S.W.; Saravanan, M. Bacterial profile of ocular infections: A systematic review. BMC Ophthalmol. 2017, 17, 212–220. [Google Scholar] [CrossRef]





| Cefuroxime | Cefazolin | Tobramycin | Azithromycin |
|---|---|---|---|
| 1.0 | 1.25 | ||
| 0.25 | 0.312 | 0.25 | |
| 2.0 | 1.0 | ||
| 0.312 | 1.0 | ||
| 2.0 | 8.0 | 0.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dong, H.; Tran, P.; Luth, K.; Thalman, D.; Ray, C.; Lin, P.; Moss, S.; Hamood, A.; McCartney, D.; Reid, T.W. Development of an Effective and Cost-Saving Synergistic-Antibacterial Therapy for Prevention of Endophthalmitis. Antibiotics 2025, 14, 588. https://doi.org/10.3390/antibiotics14060588
Dong H, Tran P, Luth K, Thalman D, Ray C, Lin P, Moss S, Hamood A, McCartney D, Reid TW. Development of an Effective and Cost-Saving Synergistic-Antibacterial Therapy for Prevention of Endophthalmitis. Antibiotics. 2025; 14(6):588. https://doi.org/10.3390/antibiotics14060588
Chicago/Turabian StyleDong, Huy, Phat Tran, Keaton Luth, Dana Thalman, Coby Ray, Pamela Lin, Staci Moss, Abdul Hamood, David McCartney, and Ted W. Reid. 2025. "Development of an Effective and Cost-Saving Synergistic-Antibacterial Therapy for Prevention of Endophthalmitis" Antibiotics 14, no. 6: 588. https://doi.org/10.3390/antibiotics14060588
APA StyleDong, H., Tran, P., Luth, K., Thalman, D., Ray, C., Lin, P., Moss, S., Hamood, A., McCartney, D., & Reid, T. W. (2025). Development of an Effective and Cost-Saving Synergistic-Antibacterial Therapy for Prevention of Endophthalmitis. Antibiotics, 14(6), 588. https://doi.org/10.3390/antibiotics14060588







