1. Introduction
Clostridioides difficile is a spore-forming and toxin-producing anaerobic bacillus causing diarrhea and life-threatening colitis in nearly half a million people in the United States with a cost burden estimated at USD 5.4 billion [
1,
2,
3].
Clostridioides difficile is a multi-drug-resistant organism (MDRO) that resists numerous antibiotics frequently used in clinical settings to treat bacterial infections, including aminoglycosides, lincomycin, erythromycin, clindamycin, penicillins, cephalosporins, and fluoroquinolones [
4,
5]. Currently, there are few therapeutic options for first-line treatment, with fidaxomicin being preferred; however, vancomycin remains the most commonly used due to its greater accessibility [
6,
7,
8,
9]. Up to 30% of patients with an initial CDI will develop a recurrence (rCDI), and up to 65% of patients who experience at least one recurrence will suffer a subsequent recurrence [
8,
10,
11,
12]. Given these challenges, there is a critical need for new antimicrobial agents to effectively combat
C. difficile and reduce the burden of this infection.
Filamentous fungi serve as a rich resource for producing organic acids, proteins, enzymes, antibiotics, statins, and steroids [
13]. Amongst these,
Aspergillus oryzae, an edible filamentous fungus recognized by the FDA as Generally Recognized as Safe (GRAS), is extensively used in fermenting foods such as sake, miso, soy sauce, and meju [
14]. In our previous work [
15,
16], we demonstrated the antimicrobial activity of
A. oryzae fermentate against various aerobic Gram-positive bacterial species, including
Staphylococcus aureus and
Listeria monocytogenes, as well as, to a lesser extent, Gram-negative bacteria such as
Escherichia coli and
Salmonella Typhimurium. Additionally, the fermentate exhibited strong activity against fungal pathogens, including
Aspergillus fumigatus,
Candida albicans, and
Penicillium roqueforti. We also assessed its potential toxicity using MCF-7 breast cancer cells and found that treatment with 500 µg/mL of lyophilized
A. oryzae fermentate had no adverse effect on cell viability [
15].
We studied the antimicrobial activity of ethyl acetate extract of A. oryzae fermentate (fungal extract) against several toxigenic C. difficile strains. We found that 80% of the tested strains showed greater susceptibility to the fungal extract than to 5 µg of vancomycin. The fungal extract exhibited a rapid bactericidal effect, causing severe membrane disruption and cell lysis. It induced significant depolarization and increased membrane permeability in C. difficile cells. These findings highlight the potential of the fungal extract as a promising candidate for developing new antimicrobials against CDI, warranting further in vitro and in vivo studies.
3. Discussion
Currently, oral vancomycin and fidaxomicin are the mainstays for the treatment of initial CDI, with vancomycin being more commonly used due to its greater accessibility [
6,
9]. However, their high cost and impact on the gut microbiome, especially for vancomycin, pose significant challenges [
17,
18]. Given these limitations, the urgent development of a new generation of therapeutics is critical to address the growing need for effective and accessible CDI treatment options.
The findings of this study demonstrate the potent antimicrobial activity of
A. oryzae fungal extract against
C. difficile, highlighting its potential as an effective bactericidal agent. The disc diffusion assay revealed that the fungal extract produced a significant zone of inhibition against all
C. difficile strains including non-toxigenic, clinical isolates, and hypervirulent strains such as Ribotype 027. There are significant differences in the diameter of the zone of inhibition between the fungal extract and vancomycin (5 µg) in 80% of tested strains (4 out of 5). Notably, the hypervirulent
C. difficile strain Ribotype 027 (ATCC BAA-1870) exhibited greater susceptibility to the fungal extract than to vancomycin, suggesting that the
A. oryzae fungal extract may target critical bacterial structures or processes distinct from those affected by vancomycin. Inhibition zones with inner colonies have been reported for all
C. difficile strains tested against vancomycin, but only present for one strain tested against the fungal extract. The presence of inner colonies within the zone of inhibition suggests potential heteroresistance, tolerance, or adaptive resistance among
C. difficile populations [
19]. These colonies may represent subpopulations with partial resistance, persisted cells, or bacteria capable of inactivating the antimicrobial agent [
20]. Alternatively, slow-growing variants or experimental factors could contribute to their emergence. Further analysis, including susceptibility retesting, genetic characterization, and enzyme activity assays, is necessary to determine the underlying mechanism. Understanding these factors is crucial for accurately assessing antimicrobial efficacy and resistance development for both vancomycin and
A. oryzae fermentate.
The time kill assay further validated the potency of
A. oryzae fungal extract, achieving complete eradication of
C. difficile within six hours. In contrast,
C. difficile continued to grow for 24 h when treated with vancomycin at 8 µg/mL. Despite its efficacy against vegetative cells, neither the fungal extract nor vancomycin inhibited
C. difficile spore germination, indicating that the extract does not interfere with the early stages of spore outgrowth. The spore core is encased by multiple protective layers, including the inner membrane, cell wall, cortex, outer membrane, spore coats, and exosporium. These layers form a permeability barrier that contributes to spore resistance by preventing the entry of DNA-damaging compounds [
3].
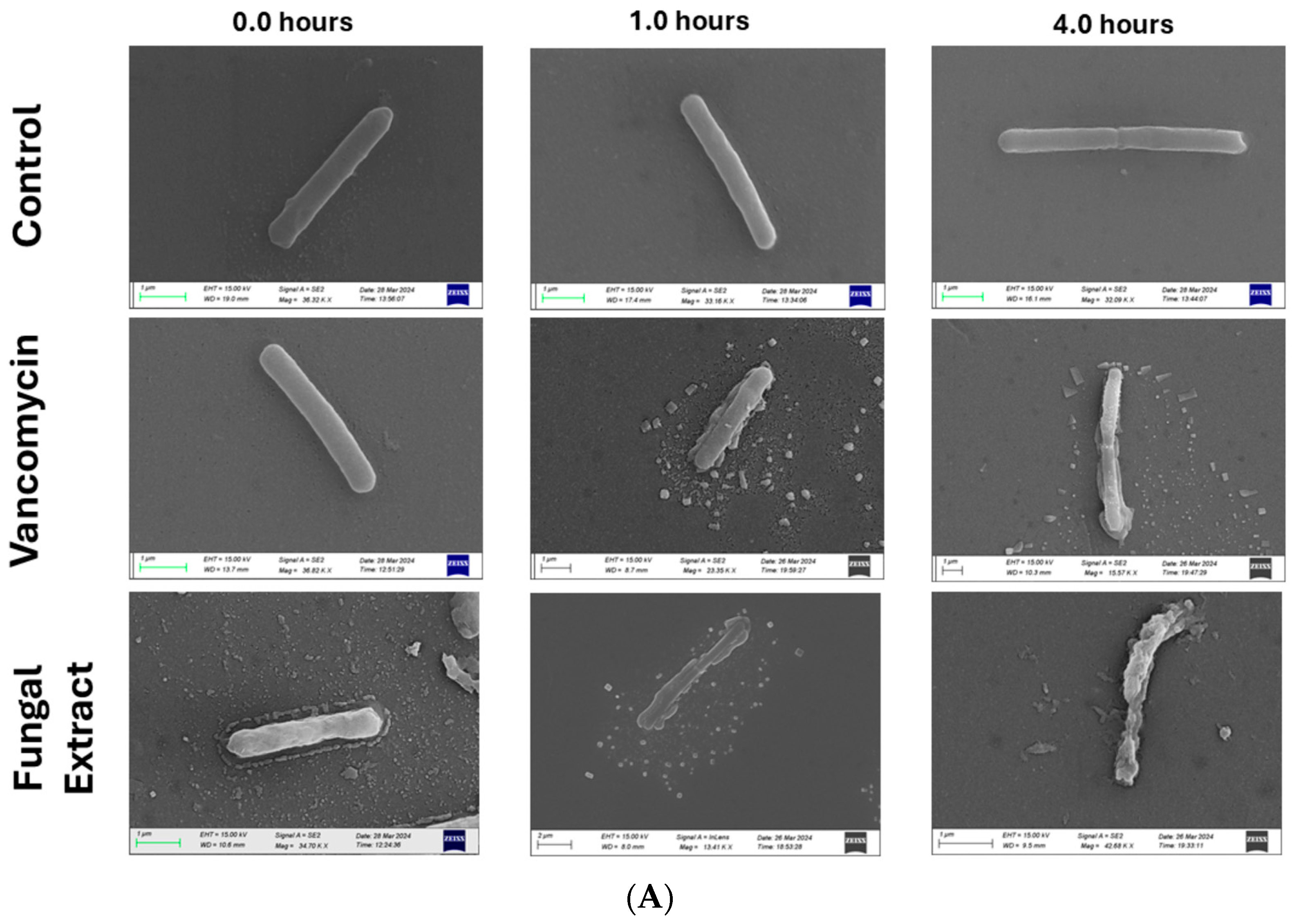
To elucidate the mechanism of action, scanning electron microscopy (SEM) and flow cytometry were employed to assess cellular morphology and membrane integrity. SEM imaging revealed extensive cellular damage in C. difficile cells treated with the fungal extract, characterized by intracellular leakage and complete cell lysis after four hours. This morphological disruption closely paralleled the effects observed with vancomycin, reinforcing the bactericidal nature of the extract. Flow cytometry analysis provided additional mechanistic insights, demonstrating that fungal extract induces both membrane depolarization and loss of membrane integrity, as evidenced by dual staining with propidium iodide (PI) and DiBAC4. The significant shift in fluorescence intensity, particularly in quadrant Q2, indicates late-stage bacterial damage characterized by extensive membrane disruption. In contrast, vancomycin-treated cells did not show the same staining pattern, suggesting that at the tested concentrations, vancomycin did not induce sufficient membrane permeability loss to enhance dye uptake. Given that vancomycin primarily targets peptidoglycan synthesis rather than directly disrupting membrane integrity, it is possible that higher concentrations (>32 µg/mL) may be required to produce similar effects.
These findings suggest that A. oryzae fungal extract represents a promising natural antimicrobial with potent activity against C. difficile. Its ability to induce membrane damage and bacterial lysis sets it apart from conventional antibiotics, which may act more slowly or through different mechanisms. However, additional studies are needed to fully characterize the mechanism of action and its active components, to explore its potential synergy with existing therapies, and to assess its effectiveness in vivo models of C. difficile infection. Furthermore, understanding the impact of A. oryzae fungal extract on the gut microbiota will be essential to evaluate its therapeutic potential and safety in clinical applications.
4. Materials and Methods
4.1. Fungal Strain and Fermentate Production
A. oryzae NRRL 3483 was used in this study to produce the fermentate. A. oryzae was cultured on potato dextrose agar (PDA) for 4 days at 30 °C. Asexual spores were harvested from individual cultures on PDA using sterile 0.1% Tween-80 solution and counted using a hemocytometer. Spore numbers were adjusted to 5 × 107 conidia/mL with sterile deionized water (DI) water. The fungal spore suspension was stored at 4 °C and used within two weeks of preparation. To produce the fermentate, A. oryzae NRRL 3483 was inoculated at a final concentration of 5 × 105 conidia/mL into 250 mL Erlenmeyer flasks containing 150 mL of liquid culture medium and incubated for 6 days at 25 ± 2 °C with shaking at 220 rpm. The liquid culture medium contains 17.0 g pancreatic digest of casein, 3.0 g papain digest of soybean, 2.5 g dextrose, 5.0 g sodium chloride, and 2.5 g dipotassium phosphate in 1000 mL distilled water. At the end of the incubation period, A. oryzae mycelia were separated from the culture broth by filtration through four layers of Miracloth (MilliporeSigma, Burlington, MA, USA), and the sterile cell-free culture fermentate, A. oryzae fermentate (AOF), was obtained by filtering through a 0.22 mm PES membrane filter unit (Thermo Scientific, Waltham, MA, USA). As a control group, a liquid culture medium with no fungus was treated similarly. A. oryzae fermentate was stored in the fridge at 5 °C throughout the experiments. “A. oryzae fermentate” refers to the entire cell-free culture supernatant obtained directly from the fermentation of Aspergillus oryzae, without any solvent-based extraction.
Preparation of the fungal extract: 20 mL of A. oryzae fermentate (AOF) was mixed with an equal volume of ethyl acetate (EA) (v/v) in a 50 mL conical tube and incubated overnight at 25 °C with shaking at 150 rpm. Then, the mixture was centrifuged at 5000 rpm and the top organic ethyl acetate layer was transferred to a new tube and dried under gentle airflow, reconstituted in 1.0 mL of methanol (Thermo Fisher Scientific, Waltham, MA, USA), and filtered using a sterile 0.45 μm PES membrane filter unit (Thermo Fisher Scientific, USA). The resulting methanol solution, referred to as the “fungal extract”, was stored at 5 °C and utilized throughout the study. “The fungal extract” refers to the ethyl acetate extract derived from the fermentate, which is a more purified or concentrated form of the bioactive compounds present in the fermentate.
4.2. Bacterial Strains and Culture Conditions
Five C. difficile strains were used in this study: a non-toxigenic strain (ATCC 700057), a toxigenic hypervirulent ribotype 027 strain (ATCC BAA-1870), and three clinical toxigenic isolates: a tcdA+ tcdB+ cdtB− isolate (ORLVS 020), a tcda+ tcdB+ cdtB+ isolate (ORLVS 052), and a tcdA− tcdb+ cdtB− isolate (ORLVS 131). All strains and isolates were cultured from frozen glycerol stocks −80 °C either on pre-reduced Tryptone Soya Agar (TSA) with 5% sheep blood (Thermo Scientific, USA) or in pre-reduced brain heart infusion broth (DOT Scientific, Burton, MI, USA) supplemented with 5 g/L yeast extract (Thermo Fisher, Waltham, MA, USA), 1% L-cysteine (Sigma-Aldrich, St. Louis, MO, USA), and 0.1% sodium taurocholate (Sigma-Aldrich, USA) (BHIS). The cultures were incubated at 37 °C for 24–48 h under anaerobic conditions prior to use.
4.3. Antimicrobial Activity: Agar Disc Diffusion Assay
Agar disc diffusion assay was used to assess the antimicrobial activity of the fungal extract against all five
C. difficile strains and compared with 5 µg vancomycin (BD Diagnostic, Franklin Lakes, NJ, USA) according to the Antimicrobial Susceptibility Testing Standards outlined by the Clinical and Laboratory Standards Institute [
21] and method for antimicrobial susceptibility testing of anaerobic bacteria [
22], with some modifications. Briefly, 100 mL of the fungal extract was loaded onto sterile blank 6 mm discs (BD, Franklin Lakes, NJ, USA) and air dried under a Biological Safety Cabinet (BSC). A sterile blank 6 mm disc was loaded with methanol (Sigma, St. Louis, MO, USA) and dried and served as a control. To standardize the inoculum density, single colonies of
C. difficile were picked, and the turbidity was adjusted by pre-reduced Phosphate-buffered saline (PBS) to match a 0.5 McFarland standard. This results in a bacterial suspension containing approximately ∼10
7 colony-forming units (cfu)/mL. The bacterial suspension density was confirmed to be 0.08–0.1 using a spectrophotometer at a 600 nm absorbance.
A cotton applicator was submerged into the PBS bacterial suspension and then streaked onto Brucella Blood Agar (BBA, Fisher Scientific, Waltham, MA, USA). BBA plates are supplemented with Hemin and Vitamin K (BBA, Fisher Scientific) and were reduced for 24 h in the anaerobic chamber to ensure the removal of residual oxygen [
23]. Then, all discs were placed on the surface of BBA plates and incubated anaerobically at 37 °C for 48 h. This process was completed in triplicate. After the incubation period, the colony-free zone of inhibitions was measured in millimeters (mm) using a ruler and recorded.
4.4. Time Kill Assay
A time kill assay was conducted against the hypervirulent
C. difficile ATCC BAA-1870 to assess whether the fungal extract exhibits bactericidal or bacteriostatic activity [
24,
25]. Log-phase cultures of
C. difficile (10
8 cfu/mL) were incubated at 37 °C in a falcon tube with the fungal extract, vancomycin at a final concentration of 8 µg/mL and negative control in pre-reduced brain heart infusion broth (BHIS) supplemented with 5 g/L yeast extract + 1% L-cysteine + 0.1% taurocholate. One mL of the fungal extract was evaporated in a 5 mL falcon tube and used in this experiment. Sterile BHIS with no fungal extract or vancomycin was used as a negative control. Aliquots (20 µL) were taken from each treatment at specific time points of incubation (0 h, 6 h, 24 h, and 48 h), diluted, and plated onto pre-reduced BBA agar plates to determine the viable bacterial count. The experiment was performed in triplicate. Each plate was counted three times by two separate people using a tally counter. The numbers were then averaged and CFUs were determined for each plate. With this method, the threshold of detection was 100 CFU/mL. Bactericidal activity was defined by a ≥3-log10 reduction in colonies compared to the starting inoculum.
4.5. Scanning Electron Microscope (SEM)
Scanning electron microscopy (SEM) was used to visualize the effects of the fungal extract on the cell wall of
C. difficile ATCC BAA-1870 [
26]. To prepare the cells for imaging, 200 μL of the fungal extract was added to a microplate and left to evaporate in sterile conditions. An equal volume of BHIS was added to the wells to rehydrate the fungal extract. Also, 10 μL of sterile DI water and 500 ug/mL vancomycin solution were added to wells containing 200 μL of BHIS to prepare the negative and positive controls, respectively. To each well, 5 μL of
C. difficile broth culture was added, pipet mixed, and incubated at 37 °C under anaerobic conditions. Samples were collected from each time point (0 h, 1 h, and 4 h) in microcentrifuge tubes, centrifuged at 10,000×
g for 10 min, and washed with 1 mL of PBS. Samples were centrifuged again at 10,000×
g for 10 min, resuspended in 1 mL of 4% paraformaldehyde, and incubated for 1 h at room temperature. Samples were centrifuged one more time at 10,000×
g for 10 min and washed twice with DI water before being resuspended in 100 μL of sterile DI water. Approximately 40 μL of the suspension was pipetted onto glass microscope slides and allowed to dry in sterile conditions. Samples were transferred to the Nanoscale Imaging and Analysis Center for coating and scanning electron microscopy. The slides were coated with gold for 30 s at 80 mA in the Leica ACE600 sputtering machine (Leica Camera, Wetzlar, Germany). The slides containing the samples were affixed to the stage of the Zeiss GeminiSEM 450 (ZEISS, Jena, Germany) with copper tape before being inserted into the chamber for imaging. Samples were imaged and analyzed with the Zeiss SmartSEM software. Samples were imaged using the SE2 electron source at working distances between 5.5 and 10.5 mm and with beam voltages ranging from 5 kV to 15 kV.
4.6. Flow Cytometry
Flow cytometry was used to investigate the effects of the fungal extract on the permeability and membrane potential of the hypervirulent
C. difficile strain ATCC BAA-1870 (ribotype 27). Membrane permeability and potential were assessed using propidium iodide (PI) and bis-(1,3-dibutylbarbituric acid) trimethine oxonol (DiBAC4) (Invitrogen, Carlsbad, CA, USA) [
27]. A pre-culture of
C. difficile ATCC BAA-1870 was inoculated into BHI broth and incubated for 18–24 h at 37 °C under anaerobic conditions. After incubation, the bacterial cells were harvested by centrifuging at 4500 rpm for 5 min. The resulting pellets were resuspended in BHI broth to an optical density (OD
600) of 0.18–0.22.
The fungal extract was added to 1.5 mL microcentrifuge tubes and then dried. An equal volume of adjusted broth was added to rehydrate the samples. Vancomycin was tested at concentrations of 32 µg/μL and 2 µg/μL, and a positive control was created by heating a sample at 100 °C for 30 min. All samples were centrifuged at 4500 rpm for 5 min, and the pellets were washed with 1× phosphate-buffered saline (PBS). The pellets were then resuspended in PBS containing 10 μg/mL DiBAC4 and incubated at room temperature for 10 min. Following this incubation, the mixtures were centrifuged again at 4500 rpm for 10 min. The pellets were washed with PBS and resuspended in 500 μL of PBS containing 5 μg/mL PI. Flow cytometric analyses were performed using a ThermoFisher Attune NxT with 100,000 events collected for each sample (ThermoFisher, USA). The data were analyzed and plotted as histograms of fluorescence events against fluorescence intensity using FlowJo version 10.10.0 (BD, USA).
4.7. Spore Germination Assay
We conducted this assay to evaluate whether the fungal extract can inhibit
Clostridioides difficile spore germination [
28]. The hypervirulent
C. difficile strain ATCC BAA-1870 was used for this assay. Spores were prepared and purified as described previously (31), and spore stocks were stored at −20 °C until use. About 10
7 C. difficile spores were suspended in 1 mL brain heart infusion (BHI) broth with or without germinants (5 g/L yeast extract, 1% L-cysteine, and 0.1% taurocholate). Using a sterile 24-well flat bottom plate (Costar, Washington, DC, USA), 0.5 mL of the fungal extract was evaporated and then reconstituted with 1 mL of BHI with and without the supplements. In total, 8 µg/mL of vancomycin was included as a positive control, with and without supplements. As a negative control, we used BHI only with and without supplements. The spore suspension was heated at 65 °C for 20 min prior to the assay run to kill vegetative cells within the suspension. After setting all treatment groups, 1 mL of BHI with/without supplements was added and then
C. difficile spore was swiftly added. Then, the absorbance was measured on Synergy H1 Microplate Reader at 600 nm for a time point of T0. Then, the OD
600 was measured every 5 min for 80 min. The absorbance data were then transferred and plotted into an Excel sheet.
4.8. Statistical Analysis
Antimicrobial activity results are expressed as the mean ± standard deviation (SD). T-tests were used to compare the diameter of the zone of inhibition between the vancomycin-treated group and the fungal extract-treated group for each C. difficile strain. A p-value ≤ 0.05 was considered statistically significant.