Physician Feedback Reduces Antibiotic Prescribing for Uncomplicated Upper Respiratory Tract Infection in the Emergency Department
Abstract
1. Introduction
2. Results
3. Discussion
4. Methods
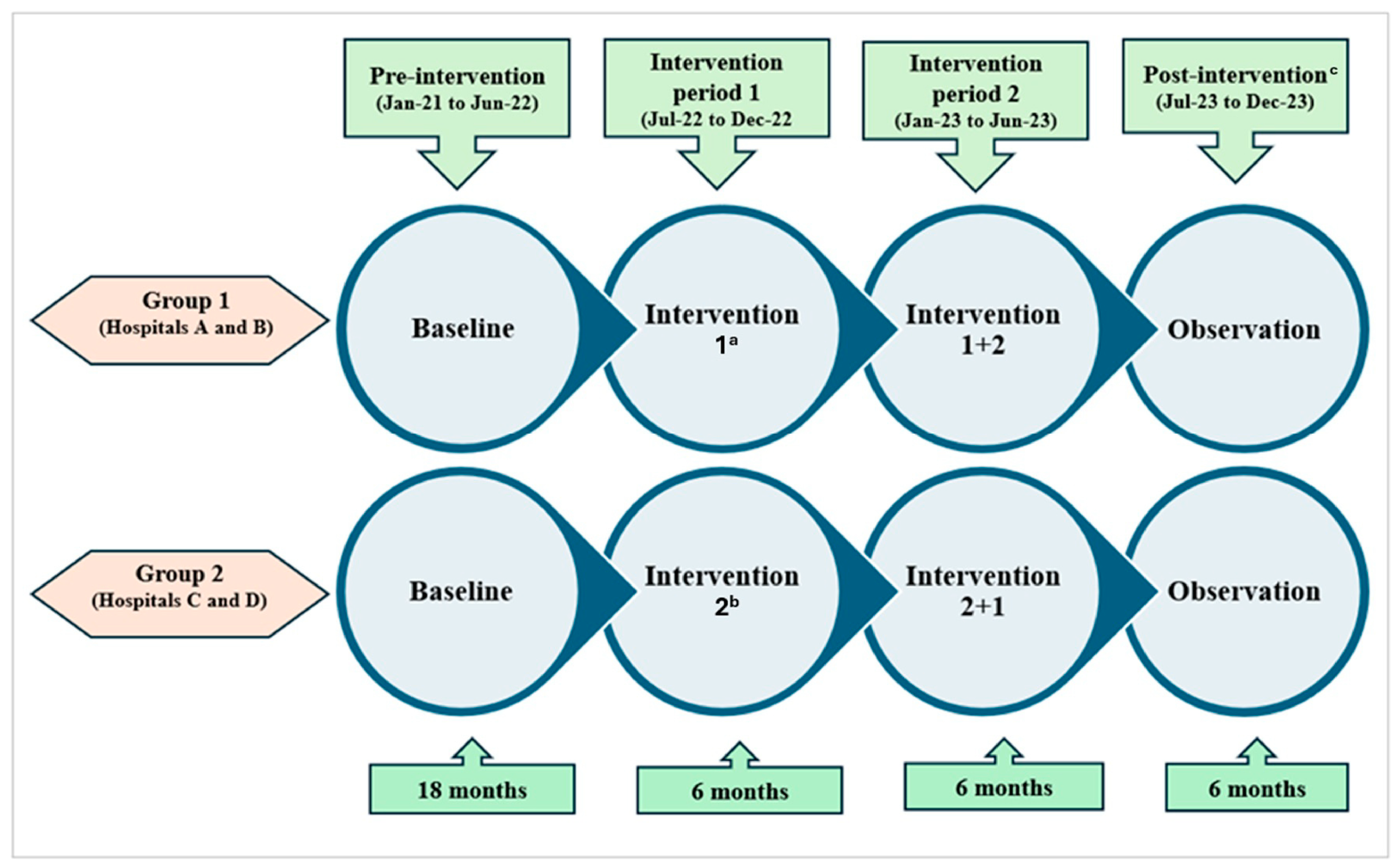
4.1. Study Design and Settings
4.2. Interventions
4.3. Data Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- May, L.; Cosgrove, S.; L’Archeveque, M.; Talan, D.A.; Payne, P.; Jordan, J.; Rothman, R.E. A call to action for antimicrobial stewardship in the emergency department: Approaches and strategies. Ann. Emerg. Med. 2013, 62, 69–77.e2. [Google Scholar] [CrossRef]
- Ladines-Lim, J.B.; Fischer, M.A.; Linder, J.A.; Chua, K.P. Appropriateness of Antibiotic Prescribing in US Emergency Department Visits, 2016–2021. Antimicrob. Steward. Healthc. Epidemiol. 2024, 4, e79. [Google Scholar] [CrossRef]
- Hersh, A.L.; King, L.M.; Shapiro, D.J.; Hicks, L.A.; Fleming-Dutra, K.E. Unnecessary Antibiotic Prescribing in US Ambulatory Care Settings, 2010–2015. Clin. Infect. Dis. 2021, 72, 133–137. [Google Scholar] [CrossRef]
- Denny, K.J.; Gartside, J.G.; Alcorn, K.; Cross, J.W.; Maloney, S.; Keijzers, G. Appropriateness of antibiotic prescribing in the Emergency Department. J. Antimicrob. Chemother. 2019, 74, 515–520. [Google Scholar] [CrossRef]
- Fleming-Dutra, K.E.; Hersh, A.L.; Shapiro, D.J.; Bartoces, M.; Enns, E.A.; File, T.M.; Finkelstein, J.A.; Gerber, J.S.; Hyun, D.Y.; Linder, J.A.; et al. Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010–2011. JAMA 2016, 315, 1864–1873. [Google Scholar] [CrossRef] [PubMed]
- Palms, D.L.; Hicks, L.A.; Bartoces, M.; Hersh, A.L.; Zetts, R.; Hyun, D.Y.; Fleming-Dutra, K.E. Comparison of antibiotic prescribing in retail clinics, urgent care centers, emergency departments, and traditional ambulatory care settings in the United States. JAMA Intern. Med. 2018, 178, 1267–1269. [Google Scholar] [CrossRef]
- Lee, W. Antibiotic prescribing for patients with upper respiratory tract infections by emergency physicians in a Singapore tertiary hospital. Hong Kong J. Emerg. Med. 2005, 12, 70–76. [Google Scholar] [CrossRef]
- Smieszek, T.; Pouwels, K.B.; Dolk, F.C.K.; Smith, D.R.M.; Hopkins, S.; Sharland, M.; Hay, A.D.; Moore, M.V.; Robotham, J.V. Potential for reducing inappropriate antibiotic prescribing in English primary care. J. Antimicrob. Chemother. 2018, 73 (Suppl. S2), ii36–ii43. [Google Scholar] [CrossRef] [PubMed]
- May, L.; Martín Quirós, A.; Ten Oever, J.; Hoogerwerf, J.; Schoffelen, T.; Schouten, J. Antimicrobial stewardship in the emergency department: Characteristics and evidence for effectiveness of interventions. Clin. Microbiol. Infect. 2021, 27, 204–209. [Google Scholar] [CrossRef]
- Karanika, S.; Paudel, S.; Grigoras, C.; Kalbasi, A.; Mylonakis, E. Systematic Review and Meta-analysis of Clinical and Economic Outcomes from the Implementation of Hospital-Based Antimicrobial Stewardship Programs. Antimicrob. Agents Chemother. 2016, 60, 4840–4852. [Google Scholar]
- Ruiz-Ramos, J.; Escolà-Vergé, L.; Monje-López, Á.E.; Herrera-Mateo, S.; Rivera, A. The Interventions and Challenges of Antimicrobial Stewardship in the Emergency Department. Antibiotics 2023, 12, 1522. [Google Scholar] [CrossRef]
- Chan, Y.Y.; Bin Ibrahim, M.A.; Wong, C.M.; Ooi, C.K.; Chow, A. Determinants of antibiotic prescribing for upper respiratory tract infections in an emergency department with good primary care access: A qualitative analysis. Epidemiol. Infect. 2019, 147, e111. [Google Scholar] [CrossRef]
- Lim, D.W.; Htun, H.L.; Ong, L.S.; Guo, H.; Chow, A. Systematic review of determinants influencing antibiotic prescribing for uncomplicated acute respiratory tract infections in adult patients at the emergency department. Infect. Control Hosp. Epidemiol. 2022, 43, 366–375. [Google Scholar] [CrossRef]
- Huang, Z.; Weng, Y.; Ang, H.; Chow, A. Determinants of antibiotic over-prescribing for upper respiratory tract infections in an emergency department with good primary care access: A quantitative analysis. J. Hosp. Infect. 2021, 113, 71–76. [Google Scholar] [CrossRef]
- Tan, R.; Huang, Z.; Guo, H.; Weng, Y.; Chow, A. Antibiotic expectations of patients attending an emergency department with upper respiratory tract infections: Clinical and behavioural determinants of antibiotic use. Int. J. Antimicrob. Agents. 2022, 59, 106511. [Google Scholar] [CrossRef]
- Pulia, M.; Redwood, R.; May, L. Antimicrobial Stewardship in the Emergency Department. Emerg. Med. Clin. N. Am. 2018, 36, 853–872. [Google Scholar] [CrossRef] [PubMed]
- Losier, M.; Ramsey, T.D.; Wilby, K.J.; Black, E.K. A Systematic Review of Antimicrobial Stewardship Interventions in the Emergency Department. Ann. Pharmacother. 2017, 51, 774–790. [Google Scholar] [CrossRef] [PubMed]
- Metlay, J.P.; Camargo, C.A., Jr.; MacKenzie, T.; McCulloch, C.; Maselli, J.; Levin, S.K.; Kersey, A.; Gonzales, R.; IMPAACT Investigators. Cluster-randomized trial to improve antibiotic use for adults with acute respiratory infections treated in emergency departments. Ann. Emerg. Med. 2007, 50, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Yadav, K.; Meeker, D.; Mistry, R.D.; Doctor, J.N.; Fleming-Dutra, K.E.; Fleischman, R.J.; Gaona, S.D.; Stahmer, A.; May, L. A Multifaceted Intervention Improves Prescribing for Acute Respiratory Infection for Adults and Children in Emergency Department and Urgent Care Settings. Acad. Emerg. Med. 2019, 26, 719–731. [Google Scholar] [CrossRef]
- Jones, G.F.; Fabre, V.; Hinson, J.; Levin, S.; Toerper, M.; Townsend, J.; Cosgrove, S.E.; Saheed, M.; Klein, E.Y. Improving antimicrobial prescribing for upper respiratory infections in the emergency department: Implementation of peer comparison with behavioral feedback. Antimicrob. Steward. Healthc. Epidemiol. 2021, 1, e70. [Google Scholar] [CrossRef]
- Buehrle, D.J.; Phulpoto, R.H.; Wagener, M.M.; Clancy, C.J.; Decker, B.K. Decreased Overall and Inappropriate Antibiotic Prescribing in a Veterans Affairs Hospital Emergency Department following a Peer Comparison-Based Stewardship Intervention. Antimicrob. Agents Chemother. 2020, 65, e01660-20. [Google Scholar] [CrossRef]
- Zeng, Y.; Shi, L.; Liu, C.; Li, W.; Li, J.; Yang, S.; Yang, X.; Huang, Q.; Yang, L. Effects of social norm feedback on antibiotic prescribing and its characteristics in behaviour change techniques: A mixed-methods systematic review. Lancet Infect. Dis. 2023, 23, e175–e184. [Google Scholar] [CrossRef]
- Xu, A.X.T.; Brown, K.; Schwartz, K.L.; Aghlmandi, S.; Alderson, S.; Brehaut, J.C.; Brown, B.C.; Bucher, H.C.; Clarkson, J.; De Sutter, A.; et al. Audit and Feedback Interventions for Antibiotic Prescribing in Primary Care: A Systematic Review and Meta-analysis. Clin. Infect. Dis. 2025, 80, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Tan, V.; Ang, G.; Tan, K.B.; Chen, C. Impact of COVID-19 national response on primary care utilisation in Singapore: An interrupted time-series analysis. Sci. Rep. 2024, 14, 6408. [Google Scholar] [CrossRef] [PubMed]
- Yau, J.W.K.; Lee, M.Y.K.; Lim, E.Q.Y.; Tan, J.Y.J.; Tan, K.B.J.C.; Chua, R.S.B. Genesis, evolution and effectiveness of Singapore’s national sorting logic and home recovery policies in handling the COVID-19 Delta and Omicron waves. Lancet Reg. Health West. Pac. 2023, 35, 100719. [Google Scholar] [CrossRef]
- Tan, H.Y.T.; Yau, J.W.K.; Toh, M.P.H.S.; Vasoo, S.; Leo, Y.S. Coronavirus disease and home recovery: A Singapore perspective. West. Pac. Surveill. Response J. 2023, 14, 1–7. [Google Scholar] [CrossRef]
- Ministry of Health Singapore. Preparing for Rise in COVID-19 Cases Driven by the BA.4 and BA.5 Subvariants. Available online: https://www.moh.gov.sg/newsroom/rise-in-ba4-and-ba5-subvariant-cases-drives-recent-increase-in-covid-19-cases/ (accessed on 9 November 2025).
- Du, W.; Feng, Z.; Zhao, Y. The impact of lifting COVID-19 restrictions on influenza transmission across countries. Adv. Contin. Discret. Models 2025, 2025, 23. [Google Scholar] [CrossRef]
- Koh, S.W.C.; Low, S.H.; Goh, J.C.; Hsu, L.Y. Increase in Antibiotic Utilisation in Primary Care Post COVID-19 Pandemic. Antibiotics 2025, 14, 309. [Google Scholar] [CrossRef] [PubMed]
- Academy of Medicine, Singapore. Resource Page on COVID-19. Available online: https://www.ams.edu.sg/policy-advocacy/covid-19-resource-page (accessed on 9 November 2025).
- Gerber, J.S.; Prasad, P.A.; Fiks, A.G.; Localio, A.R.; Bell, L.M.; Keren, R.; Zaoutis, T.E. Durability of benefits of an outpatient antimicrobial stewardship intervention after discontinuation of audit and feedback. JAMA 2014, 312, 2569–2570. [Google Scholar] [CrossRef] [PubMed]
- Meeker, D.; Linder, J.A.; Fox, C.R.; Friedberg, M.W.; Persell, S.D.; Goldstein, N.J.; Knight, T.K.; Hay, J.W.; Doctor, J.N. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: A randomized clinical trial. JAMA 2016, 315, 562. [Google Scholar]
- Huang, Z.; Kuan, W.S.; Tan, H.Y.; Seow, E.; Tiah, L.; Peng, L.L.; Weng, Y.; Chow, A. Antibiotic expectation, behaviour, and receipt among patients presenting to emergency departments with uncomplicated upper respiratory tract infection during the COVID-19 pandemic. J. Glob. Antimicrob. Resist. 2023, 33, 89–96. [Google Scholar] [CrossRef]
- Satterfield, J.; Miesner, A.R.; Percival, K.M. The role of education in antimicrobial stewardship. J. Hosp. Infect. 2020, 105, 130–141. [Google Scholar] [CrossRef] [PubMed]
- McNicholas, M.; Hooper, G. Effects of patient education to reduce antibiotic prescribing rates for upper respiratory infections in primary care. Fam. Pract. 2022, 39, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Biezen, R.; Ciavarella, S.; Manski-Nankervis, J.A.; Monaghan, T.; Buising, K. Addressing Antimicrobial Stewardship in Primary Care-Developing Patient Information Sheets Using Co-Design Methodology. Antibiotics 2023, 12, 458. [Google Scholar] [CrossRef]
- Duan, L.; Liu, C.; Wang, D.; Lin, R.; Qian, P.; Zhang, X.; Liu, C. The vicious cycle of the public’s irrational use of antibiotics for upper respiratory tract infections: A mixed methods systematic review. Front. Public Health 2022, 10, 985188. [Google Scholar] [CrossRef]
- Medina-Perucha, L.; Gálvez-Hernández, P.; García-Sangenís, A.; Moragas, A.; Cots, J.M.; Lanau-Roig, A.; Borrás, A.; Amo, I.; Barragán, N.; Monfá, R.; et al. A Co-Design Process to Elaborate Educational Materials to Promote Appropriate Use of Antibiotics for Acute Lower Respiratory Tract Infections in Primary Healthcare in Catalonia (Spain). Patient Prefer. Adher. 2021, 15, 543–548. [Google Scholar] [CrossRef] [PubMed]
- McDonald, I.R.; Blocker, E.S.; Weyman, E.A.; Smith, N.; Dwyer, A.A. What Are the Best Practices for Co-Creating Patient-Facing Educational Materials? A Scoping Review of the Literature. Healthcare 2023, 11, 2615. [Google Scholar] [CrossRef]
- Attal, H.; Huang, Z.; Kuan, W.S.; Weng, Y.; Tan, H.Y.; Seow, E.; Peng, L.L.; Lim, H.C.; Chow, A. N-of-1 Trials of Antimicrobial Stewardship Interventions to Optimize Antibiotic Prescribing for Upper Respiratory Tract Infection in Emergency Departments: Protocol for a Quasi-Experimental Study. JMIR Res. Protoc. 2024, 13, e50417. [Google Scholar] [CrossRef]
- Low, I.J.; Ong, E.C.I.; Pek, P.P.M.; Quah, L.J.J.; Chong, S.L.; Lim, J.H.; Boggs, K.M.; Camargo, C.A.J.; Anantharaman, V.; Ho, A.F.W.; et al. 2021 NEDI-Singapore study: An updated inventory of emergency department characteristics. Singap. Med. J. 2024. [Google Scholar] [CrossRef]
- Klein, E.; Saheed, M.; Irvin, N.; Balhara, K.S.; Badaki-Makun, O.; Poleon, S.; Kelen, G.; Cosgrove, S.E.; Hinson, J. Racial and Socioeconomic Disparities Evident in Inappropriate Antibiotic Prescribing in the Emergency Department. Ann. Emerg. Med. 2024, 84, 101–110. [Google Scholar] [CrossRef]
- Laka, M.; Milazzo, A.; Merlin, T. Inappropriate antibiotic prescribing: Understanding clinicians’ perceptions to enable changes in prescribing practices. Aust. Health Rev. 2022, 46, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Schröder, W.; Sommer, H.; Gladstone, B.P.; Foschi, F.; Hellman, J.; Evengard, B.; Tacconelli, E. Gender differences in antibiotic prescribing in the community: A systematic review and meta-analysis. J. Antimicrob. Chemother. 2016, 71, 1800–1806. [Google Scholar] [CrossRef] [PubMed]

| Group 1 (Hospital A and Hospital B) | Group 2 (Hospital C and Hospital D) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Intervention Period 1 (Jan 2021–Dec 2021 | Pre-Intervention Period 2 (Jan 2022–Jun 2022) | Intervention Period 1 Intervention 1 a (Jul 2022–Dec 2022) | Intervention Period 2 Intervention 1 + 2 (Jan 2023–Jun 2023) | Post-Intervention (Jul 2023–Dec 2023) | Pre-Intervention Period 1 (Jan 2021–Dec 2021) | Pre-Intervention Period 2 (Jan 2022–Jun 2021) | Intervention Period 1 Intervention 2 b (Jul 2022–Dec 2022) | Intervention Period 2 Intervention 2 + 1 (Jan 2023–Jun 2023) | Post-Intervention (Jul 2023–Dec 2023) | |
| URTI attendance characteristics | ||||||||||
| Number of URTI attendances | 8673 | 2857 | 3064 | 3411 | 2994 | 4121 | 1376 | 2381 | 2522 | 2328 |
| Age in years, mean (SD) | 33.6 (13.6) | 36.7 (16.4) | 36.8 (16.4) | 39.1 (16.5) | 39.1 (17.3) | 37.1 (14.5) | 38.6 (15.6) | 38.2 (15.6) | 40.0 (15.8) | 40.4 (16.1) |
| Age group, % | ||||||||||
| 21–34 years | 66.3% | 58.9% | 58.2% | 50.3% | 52.1% | 55.5% | 52.4% | 53.2% | 47.7% | 46.5% |
| 35–49 years | 19.9% | 19.4% | 20.8% | 24.9% | 22.5% | 25.8% | 25.4% | 25.5% | 27.2% | 27.5% |
| 50 years and above | 13.8% | 21.7% | 21.0% | 24.8% | 25.3% | 18.7% | 22.2% | 21.3% | 25.1% | 26.0% |
| Gender, % | ||||||||||
| Male | 60.7% | 62.9% | 63.3% | 57.9% | 61.7% | 51.8% | 52.3% | 54.4% | 50.0% | 47.0% |
| Female | 39.3% | 37.1% | 36.7% | 42.1% | 38.3% | 48.2% | 47.7% | 45.6% | 50.0% | 53.0% |
| Ethnicity, % | ||||||||||
| Chinese | 43.7% | 41.9% | 37.4% | 38.0% | 39.3% | 44.6% | 39.5% | 42.6% | 43.3% | 48.0% |
| Malay | 25.0% | 23.6% | 28.9% | 27.6% | 25.5% | 17.3% | 18.2% | 19.7% | 20.1% | 16.5% |
| Indian | 15.6% | 16.9% | 16.8% | 17.1% | 17.2% | 17.3% | 19.2% | 19.3% | 19.2% | 16.4% |
| Others | 15.7% | 17.6% | 16.8% | 17.3% | 18.0% | 20.8% | 23.1% | 18.4% | 17.3% | 19.1% |
| Physician characteristics | ||||||||||
| Number of attending physicians | 216 | 171 | 201 | 234 | 225 | 305 | 205 | 243 | 233 | 238 |
| Years of clinical experience, mean (SD) | 4.7 (4.2) | 6.2 (5.6) | 5.8 (5.4) | 5.9 (5.4) | 5.9 (5.5) | 6.3 (6.2) | 7.6 (6.6) | 7.5 (6.5) | 7.5 (6.7) | 7.3 (6.6) |
| Years of clinical experience, min–max | 0.5–30.4 | 1.0–31.6 | 0.4–32.2 | 0.8–32.7 | 0.1–33.1 | 1.0–34.7 | 1.0–35.2 | 1.1–35.7 | 1.0–36.2 | 0.2–36.7 |
| Antibiotic prescribing rates per week | ||||||||||
| Number of URTI attendances, mean (SD) | 167 (43) | 110 (61) | 118 (21) | 131 (24) | 115 (18) | 79 (28) | 53 (25) | 92 (18) | 97 (23) | 90 (16) |
| Number of URTI attendances, min–max | 95–302 | 36–260 | 89–170 | 87–191 | 73–162 | 26–168 | 20–125 | 58–132 | 62–137 | 62–123 |
| Antibiotic prescribing for URTI attendances (%), mean (SD) | 5.0% (2.3%) | 6.3% (3.2%) | 9.6% (4.1%) | 10.0% (3.8%) | 8.8% (2.7%) | 9.2% (4.8%) | 8.2% (5.0%) | 16.4% (5.8%) | 11.2% (7.9%) | 11.3% (4.7%) |
| All 1249 Physicians with > 1 URTI Patient Attendance During the Study Period Number of Observations: 33,727 | |||||||
|---|---|---|---|---|---|---|---|
| Estimate | SE | AOR a | Lower Bound 95% CI | Upper Bound 95% CI | p Value * | ||
| Group 1 (Hospital A and Hospital B) | Started with physician feedback | ||||||
| Level at baseline (week 1) | −3.467 | 0.178 | 0.031 | 0.022 | 0.044 | <0.001 | |
| Pre-intervention period 1 trend | −0.002 | 0.001 | 0.998 | 0.995 | 1.001 | 0.220 | |
| Trend (slope) change in pre-intervention period 2 (relative to pre-intervention period 1) | 0.022 | 0.007 | 1.023 | 1.009 | 1.036 | 0.001 | |
| Level change at the start of intervention period 1 | 0.897 | 0.151 | 2.452 | 1.825 | 3.294 | <0.001 | |
| Trend (slope) change in intervention period 1 (relative to pre-intervention period 2) | −0.019 | 0.009 | 0.981 | 0.964 | 0.998 | 0.032 | |
| Level change at the start of intervention period 2 | 0.829 | 0.166 | 2.291 | 1.656 | 3.169 | <0.001 | |
| Trend (slope) change in intervention period 2 (relative to intervention period 1) | −0.013 | 0.009 | 0.987 | 0.970 | 1.004 | 0.137 | |
| Trend (slope) change in post-intervention period (relative to intervention period 2) | 0.033 | 0.010 | 1.034 | 1.014 | 1.054 | 0.001 | |
| Group 2 (Hospital C and Hospital D) | Started with patient education | ||||||
| Level at baseline (week 1) | −3.200 | 0.183 | 0.041 | 0.028 | 0.058 | <0.001 | |
| Pre-intervention period 1 | −0.004 | 0.002 | 0.996 | 0.993 | 0.999 | 0.004 | |
| Trend (slope) change in pre-intervention period 2 (relative to pre-intervention period 1) | 0.022 | 0.008 | 1.023 | 1.007 | 1.039 | 0.005 | |
| Level change at the start of intervention period 1 | 0.688 | 0.162 | 1.989 | 1.449 | 2.731 | <0.001 | |
| Trend (slope) change in intervention period 1 (relative to pre-intervention period 2) | 0.035 | 0.008 | 1.036 | 1.019 | 1.053 | <0.001 | |
| Level change at the start of intervention period 2 | 1.666 | 0.168 | 5.289 | 3.806 | 7.348 | <0.001 | |
| Trend (slope) change in intervention period 2 (relative to intervention period 1) | −0.082 | 0.010 | 0.921 | 0.903 | 0.940 | <0.001 | |
| Trend (slope) change in post-intervention period (relative to intervention period 2) | 0.050 | 0.010 | 1.051 | 1.030 | 1.072 | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guo, H.; Aithal, S.; Phua, H.P.; Kuan, W.S.; Seow, E.; Weng, Y.; Lim, H.C.; Peng, L.L.; Tan, H.Y.; Chow, A. Physician Feedback Reduces Antibiotic Prescribing for Uncomplicated Upper Respiratory Tract Infection in the Emergency Department. Antibiotics 2025, 14, 1196. https://doi.org/10.3390/antibiotics14121196
Guo H, Aithal S, Phua HP, Kuan WS, Seow E, Weng Y, Lim HC, Peng LL, Tan HY, Chow A. Physician Feedback Reduces Antibiotic Prescribing for Uncomplicated Upper Respiratory Tract Infection in the Emergency Department. Antibiotics. 2025; 14(12):1196. https://doi.org/10.3390/antibiotics14121196
Chicago/Turabian StyleGuo, Huiling, Seema Aithal, Hwee Pin Phua, Win Sen Kuan, Eillyne Seow, Yanyi Weng, Hoon Chin Lim, Li Lee Peng, Hann Yee Tan, and Angela Chow. 2025. "Physician Feedback Reduces Antibiotic Prescribing for Uncomplicated Upper Respiratory Tract Infection in the Emergency Department" Antibiotics 14, no. 12: 1196. https://doi.org/10.3390/antibiotics14121196
APA StyleGuo, H., Aithal, S., Phua, H. P., Kuan, W. S., Seow, E., Weng, Y., Lim, H. C., Peng, L. L., Tan, H. Y., & Chow, A. (2025). Physician Feedback Reduces Antibiotic Prescribing for Uncomplicated Upper Respiratory Tract Infection in the Emergency Department. Antibiotics, 14(12), 1196. https://doi.org/10.3390/antibiotics14121196







