Occurrence and Molecular Characterization of Extended-Spectrum Beta-Lactamase (ESBL)-Producing Escherichia coli in Broilers in Indonesia
Abstract
1. Introduction
2. Results
2.1. Third-Generation Cephalosporin-Resistant E. coli and ESBL-E. coli
2.2. Antimicrobial Resistance of ESBL-E. coli
2.3. Antimicrobial Resistance Level of ESBL-E. coli
2.4. ESBL Resistance Genes of ESBL-E. coli Isolates from Broilers
2.5. Phylogenetic Group
3. Discussion
4. Materials and Methods
4.1. E. coli Isolation
4.2. Antimicrobial Susceptibility Test
4.3. Phenotypic confirmation of ESBL-E. coli
4.4. Determination of ESBL Resistance Genes
4.5. Determination of E. coli Phylogenetic Group
4.6. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- FAO. Meat Market Review: Overview of Global Market Developments in 2023; FAO: Rome, Italy, 2024. [Google Scholar]
- Wahyono, N.; Utami, M. A Review of the Poultry Meat Production Industry for Food Safety in Indonesia. J. Phys. Conf. Ser. 2018, 953, 012125. [Google Scholar] [CrossRef]
- DGLAHS. Survey of Antimicrobial Usage in Poultry Farms in Indonesia; Emergency Centre for Transboundary Animal Diseases (ECTAD), FAO Indonesia: Jakarta, Indonesia, 2018. [Google Scholar]
- Ejaz, H.; Qamar, M.U.; Farhana, A.; Younas, S.; Batool, A.; Lone, D.; Atif, M.; Alruways, M.W.; Alruwaili, M.; Hamad, I.; et al. The Rising Tide of Antibiotic Resistance: A Study on Extended-Spectrum Beta-Lactamase and Carbapenem-Resistant Escherichia coli and Klebsiella pneumoniae. J. Clin. Lab. Anal. 2024, 38, e25081. [Google Scholar] [CrossRef]
- Husna, A.; Rahman, M.M.; Badruzzaman, A.T.M.; Sikder, M.H.; Islam, M.R.; Rahman, M.T.; Alam, J.; Ashour, H.M. Extended-Spectrum beta-Lactamases (ESBL): Challenges and Opportunities. Biomedicines 2023, 11, 2937. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.J.; Wang, H.W.; Tian, F.Y.; Yang, C.Z.; Zhao, M.; Ding, Y.X.; Wang, X.Y.; Cui, X.Y. Decolonization strategies for ESBL-producing or carbapenem-resistant Enterobacterales carriage: A systematic review and meta-analysis. Sci. Rep. 2024, 14, 24349. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, Y.; Walsh, T. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: A microbiological and molecular biological study. Lancet Infect. Dis. 2016, 16, 161–168. [Google Scholar] [CrossRef]
- Smith, H.Z.; Hollingshead, C.M.; Kendall, B. Carbapenem-Resistant Enterobacterales; StatPearls: Treasure Island, FL, USA, 2025. [Google Scholar]
- Tamma, P.D.; Heil, E.L.; Justo, J.A.; Mathers, A.J.; Satlin, M.J.; Bonomo, R.A. Infectious Diseases Society of America 2024 Guidance on the Treatment of Antimicrobial-Resistant Gram-Negative Infections. Clin. Infect. Dis. 2024, 79, ciae403. [Google Scholar] [CrossRef]
- Ribeiro, L.F.; Nespolo, N.M.; Rossi, G.A.M.; Fairbrother, J.M. Exploring Extended-Spectrum Beta-Lactamase (ESBL)-Producing Escherichia coli in Food-Producing Animals and Animal-Derived Foods. Pathogens 2024, 13, 346. [Google Scholar] [CrossRef]
- Or, P.; Boonyayatra, S.; Punyapornwithaya, V.; Awaiwanont, N. Prevalence of Extended-Spectrum Beta-Lactamase-Producing Escherichia Coli in Broiler Farms: A Systematic Review and Meta-Analysis. Vet. Integr. Sci. 2024, 23, e2025033. [Google Scholar] [CrossRef]
- Mandujano-Hernandez, A.; Martinez-Vazquez, A.V.; Paz-Gonzalez, A.D.; Herrera-Mayorga, V.; Sanchez-Sanchez, M.; Lara-Ramirez, E.E.; Vazquez, K.; de Jesus de Luna-Santillana, E.; Bocanegra-Garcia, V.; Rivera, G. The Global Rise of ESBL-Producing Escherichia coli in the Livestock Sector: A Five-Year Overview. Animals 2024, 14, 2490. [Google Scholar] [CrossRef] [PubMed]
- Aliyu, A.B.; Jalila, A.; Saleha, A.A.; Zunita, Z. ESBL Producing E. coli in Chickens and Poultry Farms Environment in Selangor, Malaysia: A Cross-Sectional Study on Their Occurrence and Associated Risk Factors with Environment and Public Health Importance. Zoonoses Public Health 2024, 71, 962–971. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Wu, S.; Wang, Y.; Chen, F.; Shen, Z.; Lan, Z. Antimicrobial Resistance Genes in Clinical Escherichia coli Strains from Livestock and Poultry in Shandong Province, China During 2015–2020. Antibiotics 2025, 14, 95. [Google Scholar] [CrossRef]
- Acharya, J.; Jha, R.; Gompo, T.R.; Chapagain, S.; Shrestha, L.; Rijal, N.; Shrestha, A.; Koirala, P.; Subedi, S.; Tamang, B.; et al. Prevalence of Extended-Spectrum Beta-Lactamase (ESBL)-Producing Escherichia coli in Humans, Food, and Environment in Kathmandu, Nepal: Findings From ESBL E. coli Tricycle Project. Int. J. Microbiol. 2024, 2024, 1094816. [Google Scholar] [CrossRef] [PubMed]
- Widodo, A.; Khairullah, A.R.; Effendi, M.H.; Moses, I.B.; Agustin, A.L.D. Extended-spectrum beta-lactamase-producing Escherichia coli from poultry: A review. Vet. World 2024, 17, 2017–2027. [Google Scholar] [CrossRef] [PubMed]
- Smet, A.; Martel, A.; Persoons, D.; Dewulf, J.; Heyndrickx, M.; Herman, L.; Haesebrouck, F.; Butaye, P. Broad-spectrum β-lactamases among Enterobacteriaceae of animal origin: Molecular aspects, mobility and impact on public health. FEMS Microbiol. Rev. 2009, 34, 295–316. [Google Scholar] [CrossRef] [PubMed]
- Effendi, M.; Witaningrum, A. Cases of Multidrug Resistance (MDR) and Extended Spectrum Beta-Lactamase (ESBL) Producing Escherichia Coli from Broiler Chicken in Blitar, Indonesia. Biochem. Cell. Arch. 2021, 21, 1923–1929. [Google Scholar]
- Masruroh, C.A.; Sudarwanto, M.B.; Latif, H. The Occurrence of extended spectrum B-Lactamase-producing Escherichia coli from broiler feces in Bogor. J. Sain Vet. 2016, 34, 42–49. [Google Scholar]
- Effendi, M.; Wibisono, F.; Witaningrum, A.; Permatasari, D. Identification of Bla TEM and Bla SHV Genes of Extended Spectrum Beta Lactamase (ESBL) Producing Escherichia coli from Broilers Chicken in Blitar, Indonesia. Syst. Rev. Pharm. 2021, 12, 976–981. [Google Scholar]
- Reich, F.; Atanassova, V.; Klein, G. Extended-spectrum β-lactamase- and AmpC-producing enterobacteria in healthy broiler chickens, Germany. Emerg. Infect. Dis. 2013, 19, 1253–1259. [Google Scholar] [CrossRef]
- Ferreira, M.; Leao, C.; Clemente, L.; Albuquerque, T.; Amaro, A. Antibiotic Susceptibility Profiles and Resistance Mechanisms to beta-Lactams and Polymyxins of Escherichia coli from Broilers Raised under Intensive and Extensive Production Systems. Microorganisms 2022, 10, 2044. [Google Scholar] [CrossRef]
- WHO. WHO Integrated Global Surveillance on ESBL-Producing E. coli Using a “One Health” Approach: Implementation and Opportunities; WHO: Geneva, Switzerland, 2021; Available online: https://apps.who.int/iris/bitstream/handle/10665/340079/9789240021402-eng.pdf (accessed on 30 September 2025).
- DGLAHS. Survey Result: Antibiotic Use to Prevent Disease on Chicken Farms Is Still High; Ministry of Agriculture, Republic of Indonesia: Jakarta, Indonesia, 2018. [Google Scholar]
- BPS. Provinsi Kalimantan Barat Dalam Angka 2022; Badan Pusat Statistik Provinsi Kalimantan Barat: Pontianak, Indonesia, 2022. [Google Scholar]
- Siahaan, S.; Herman, M.J.; Fitri, N. Antimicrobial Resistance Situation in Indonesia: A Challenge of Multisector and Global Coordination. J. Trop. Med. 2022, 2022, 2783300. [Google Scholar] [CrossRef]
- Hendriksen, R.S.; Cavaco, L.M.; Guerra, B.; Bortolaia, V.; Agersø, Y.; Svendsen, C.A.; Nielsen, H.N.; Kjeldgaard, J.S.; Pedersen, S.K.; Fertner, M.; et al. Evaluation and validation of laboratory procedures for the surveillance of ESBL-, AmpC-, and carbapenemase-producing Escherichia coli from fresh meat and caecal samples. Front. Microbiol. 2023, 14, 1229542. [Google Scholar] [CrossRef]
- Ministry of Agriculture. Outlook Ayam Ras Pedaging 2022; Kementerian Pertanian, Satu Data Pertanian: Jakarta, Indonesia, 2022. [Google Scholar]
- Alonso, C.A.; Zarazaga, M.; Sallem, R.; Jouini, A.; Karim, B.S.; Torres, C. Antibiotic resistance in Escherichia coli in husbandry animals: The African perspective. Lett. Appl. Microbiol. 2017, 64, 318–334. [Google Scholar] [CrossRef]
- van den Bogaard, A.E.; London, N.; Driessen, C.; Stobberingh, E.E. Antibiotic resistance of faecal Escherichia coli in poultry, poultry farmers and poultry slaughterers. J. Antimicrob. Chemother. 2001, 47, 763–771. [Google Scholar] [CrossRef]
- Sáenz, Y.; Zarazaga, M.; Briñas, L.; Lantero, M.; Ruiz-Larrea, F.; Torres, C. Antibiotic resistance in Escherichia coli isolates obtained from animals, foods and humans in Spain. Int. J. Antimicrob. Agents 2001, 18, 353–358. [Google Scholar] [CrossRef]
- Cantón, R.; Coque, T.M. The CTX-M beta-lactamase pandemic. Curr. Opin. Microbiol. 2006, 9, 466–475. [Google Scholar] [CrossRef]
- Moniri, R.D.K. Fluoroquinolone-resistant Escherichia coli isolated from healthy broilers with previous exposure to fluoroquinolones. J. Infect. Dis. Antimicrob. Agents 2005, 22, 39–44. [Google Scholar]
- Miranda, J.M.; Vázquez, B.I.; Fente, C.A.; Barros-Velázquez, J.; Cepeda, A.; Franco, C.M. Evolution of resistance in poultry intestinal Escherichia coli during three commonly used antimicrobial therapeutic treatments in poultry. Poult. Sci. 2008, 87, 1643–1648. [Google Scholar] [CrossRef]
- Horton, R.A.; Randall, L.; Snary, E.; Cockrem, H.; Lotz, S.; Wearing, H.; Duncan, D.; Rabie, A.; McLaren, I.; Watson, E.; et al. Fecal Carriage and Shedding Density of CTX-M Extended-Spectrum β-Lactamase-Producing Escherichia coli in Cattle, Chickens, and Pigs: Implications for Environmental Contamination and Food Production. Appl. Environ. Microbiol. 2011, 77, 3715–3719. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Agriculture, Republic of Indonesia. Annual Report; Ministry of Agriculture: Jakarta, Indonesia, 2018. [Google Scholar]
- Wasnaeni, Y.; Iqbal, A.; Ismoyowati, I. Broiler Farmers’ Behavior in Administering Antibiotic and Types of Antibiotic Content in Commercial Feed (A Case Study). Anim. Prod. 2015, 17, 62. [Google Scholar] [CrossRef]
- Morosini, M.I.; García-Castillo, M.; Coque, T.M.; Valverde, A.; Novais, A.; Loza, E.; Baquero, F.; Cantón, R. Antibiotic coresistance in extended-spectrum-beta-lactamase-producing Enterobacteriaceae and in vitro activity of tigecycline. Antimicrob. Agents Chemother. 2006, 50, 2695–2699. [Google Scholar] [CrossRef] [PubMed]
- Yaghoubi, S.; Zekiy, A.O.; Krutova, M.; Gholami, M.; Kouhsari, E.; Sholeh, M.; Ghafouri, Z.; Maleki, F. Tigecycline antibacterial activity, clinical effectiveness, and mechanisms and epidemiology of resistance: Narrative review. Eur. J. Clin. Microbiol. Infect. Dis. 2022, 41, 1003–1022. [Google Scholar] [CrossRef]
- Basu, S.; Mukherjee, M. Incidence and risk of co-transmission of plasmid-mediated quinolone resistance and extended-spectrum beta-lactamase genes in fluoroquinolone-resistant uropathogenic Escherichia coli: A first study from Kolkata, India. J. Glob. Antimicrob. Resist. 2018, 14, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Uddin, T.M.; Chakraborty, A.J.; Khusro, A.; Zidan, B.R.M.; Mitra, S.; Emran, T.B.; Dhama, K.; Ripon, M.K.H.; Gajdacs, M.; Sahibzada, M.U.K.; et al. Antibiotic resistance in microbes: History, mechanisms, therapeutic strategies and future prospects. J. Infect. Public Health 2021, 14, 1750–1766. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Wang, P.; Dai, Y.; Liu, Y.; Song, Y.; Yu, L.; Feng, C.; Liu, M.; Xie, Z.; Shang, Y.; et al. Longitudinal monitoring of multidrug resistance in Escherichia coli on broiler chicken fattening farms in Shandong, China. Poult. Sci. 2021, 100, 100887. [Google Scholar] [CrossRef] [PubMed]
- Lukman, D.W.; Sudarwanto, M.B.; Purnawarman, T.; Latif, H.; Pisestyani, H.; Sukmawinata, E.; Akineden, Ö. CTX-M-1 and CTX-M-55 producing Escherichia coli isolated from broiler feces in poultry slaughterhouse, Bogor, West Java Province. Glob. Adv. Res. J. Med. Med. Sci. 2016, 5, 287–291. [Google Scholar]
- Ejaz, H.; Younas, S.; Abosalif, K.O.A.; Junaid, K.; Alzahrani, B.; Alsrhani, A.; Abdalla, A.E.; Ullah, M.I.; Qamar, M.U.; Hamam, S.S.M. Molecular analysis of blaSHV, blaTEM, and blaCTX-M in extended-spectrum β-lactamase producing Enterobacteriaceae recovered from fecal specimens of animals. PLoS ONE 2021, 16, e0245126. [Google Scholar] [CrossRef]
- Harijani, N.; Tyasningsih, W.; Effendi, M. Biological Hazard on Multidrug Resistance (MDR) of Escherichia Coli Collected from Cloacal Swab of Broiler Chicken on Wet Markets Surabaya. Indian J. Forensic Med. Toxicol. 2020, 14, 3239–3244. [Google Scholar]
- Wang, J.; Stephan, R.; Karczmarczyk, M.; Yan, Q.; Hächler, H.; Fanning, S. Molecular characterization of bla ESBL-harboring conjugative plasmids identified in multi-drug resistant Escherichia coli isolated from food-producing animals and healthy humans. Front. Microbiol. 2013, 4, 188. [Google Scholar] [CrossRef]
- Che, Y.; Yang, Y.; Xu, X.; Břinda, K.; Polz, M.F.; Hanage, W.P.; Zhang, T. Conjugative plasmids interact with insertion sequences to shape the horizontal transfer of antimicrobial resistance genes. Proc. Natl. Acad. Sci. USA 2021, 118, e2008731118. [Google Scholar] [CrossRef]
- Brolund, A.; Rajer, F.; Giske, C.G.; Melefors, Ö.; Titelman, E.; Sandegren, L. Dynamics of Resistance Plasmids in Extended-Spectrum-β-Lactamase-Producing Enterobacteriaceae during Postinfection Colonization. Antimicrob. Agents Chemother. 2019, 63, e02201-18. [Google Scholar] [CrossRef]
- Coura, F.; Diniz, S.; Silva, M.; Mussi, J.M.; Minharro, S.; Lage, A.; Heinemann, M. Phylogenetic Group Determination of Escherichia coli Isolated from Animals Samples. Sci. World J. 2015, 2015, 258424. [Google Scholar] [CrossRef] [PubMed]
- Teh, H.B.H. Phylogeny and Virulence Factor Genes of Canine Urinary Escherichia coli in Relation to Clinical Disease and Antimicrobial Resistance. Master’s Thesis, University of Melbourne, Melbourne, Australia, 2018. [Google Scholar]
- Zhuge, X.; Zhou, Z.; Jiang, M.; Wang, Z.; Sun, Y.; Tang, F.; Xue, F.; Ren, J.; Dai, J. Chicken-source Escherichia coli within phylogroup F shares virulence genotypes and is closely related to extraintestinal pathogenic E. coli causing human infections. Transbound Emerg. Dis. 2021, 68, 880–895. [Google Scholar] [CrossRef] [PubMed]
- Özavci, V.; Yüksel, T.; Kirkan, Ş. Phylogenetic characterization and determination of antibiotic susceptibility of avian pathogenic Escherichia coli strains isolated from broiler visceral organs. Rev. Científica Fac. Cienc. Vet. 2022, XXXII, 1–8. [Google Scholar]
- Wang, M.; Jiang, M.; Wang, Z.; Chen, R.; Zhuge, X.; Dai, J. Characterization of Antimicrobial Resistance in Chicken-source Phylogroup F Escherichia coli: Similar Populations and Resistance Spectrums Between E. coli Recovered from Chicken Colibacillosis Tissues and Retail Raw Meats in Eastern China. Poult. Sci. 2021, 100, 101370. [Google Scholar] [CrossRef]
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing. Approved Standard. Informational Supplement, 31st ed.; Clinical & Laboratory Standards Institute: Wayne, PA, USA, 2021. [Google Scholar]
- EUCAST. Breakpoint Tables for Interpretation of MICs and Zone Diameters. Available online: http://www.eucast.org/clinical_breakpoints/ (accessed on 20 June 2025).
- Schwarz, S.; Silley, P.; Simjee, S.; Woodford, N.; van Duijkeren, E.; Johnson, A.P.; Gaastra, W. Assessing the antimicrobial susceptibility of bacteria obtained from animals. Vet. Microbiol. 2010, 141, 601–604. [Google Scholar] [CrossRef]
- Hudzicki, J. Kirby-Bauer disk diffusion susceptibility test protocol. Am. Soc. Microbiol. 2009, 15, 55–63. [Google Scholar]
- Perez, F.; Hujer, A.M.; Hujer, K.M.; Decker, B.K.; Rather, P.N.; Bonomo, R.A. Global challenge of multidrug-resistant Acinetobacter baumannii. Antimicrob. Agents Chemother. 2007, 51, 3471–3484. [Google Scholar] [CrossRef]
- Ogutu, J.; Zhang, Q.; Huang, Y.; Yan, H.; Su, L.; Gao, B.; Zhang, W.; Zhao, J.; Cai, W.; Li, W.; et al. Development of a multiplex PCR system and its application in detection of blaSHV, blaTEM, blaCTX-M-1, blaCTX-M-9 and blaOXA-1 group genes in clinical Klebsiella pneumoniae and Escherichia coli strains. J. Antibiot. 2015, 68, 725–733. [Google Scholar] [CrossRef]
- Peterson, E.; Kaur, P. Antibiotic Resistance Mechanisms in Bacteria: Relationships Between Resistance Determinants of Antibiotic Producers, Environmental Bacteria, and Clinical Pathogens. Front. Microbiol. 2018, 9, 2928. [Google Scholar] [CrossRef]
- Batchelor, M.; Hopkins, K.; Threlfall, E.J.; Clifton-Hadley, F.A.; Stallwood, A.D.; Davies, R.H.; Liebana, E. blaCTX-M Genes in Clinical Salmonella Isolates Recovered from Humans in England and Wales from 1992 to 2003. Antimicrob. Agents Chemother. 2005, 49, 1319–1322. [Google Scholar] [CrossRef]
- Clermont, O.; Christenson, J.; Denamur, E.; Gordon, D. The Clermont Escherichia coli phylo-typing method revisited: Improvement of specificity and detection of new phylo-groups. Environ. Microbiol. Rep. 2013, 5, 58–65. [Google Scholar] [CrossRef]
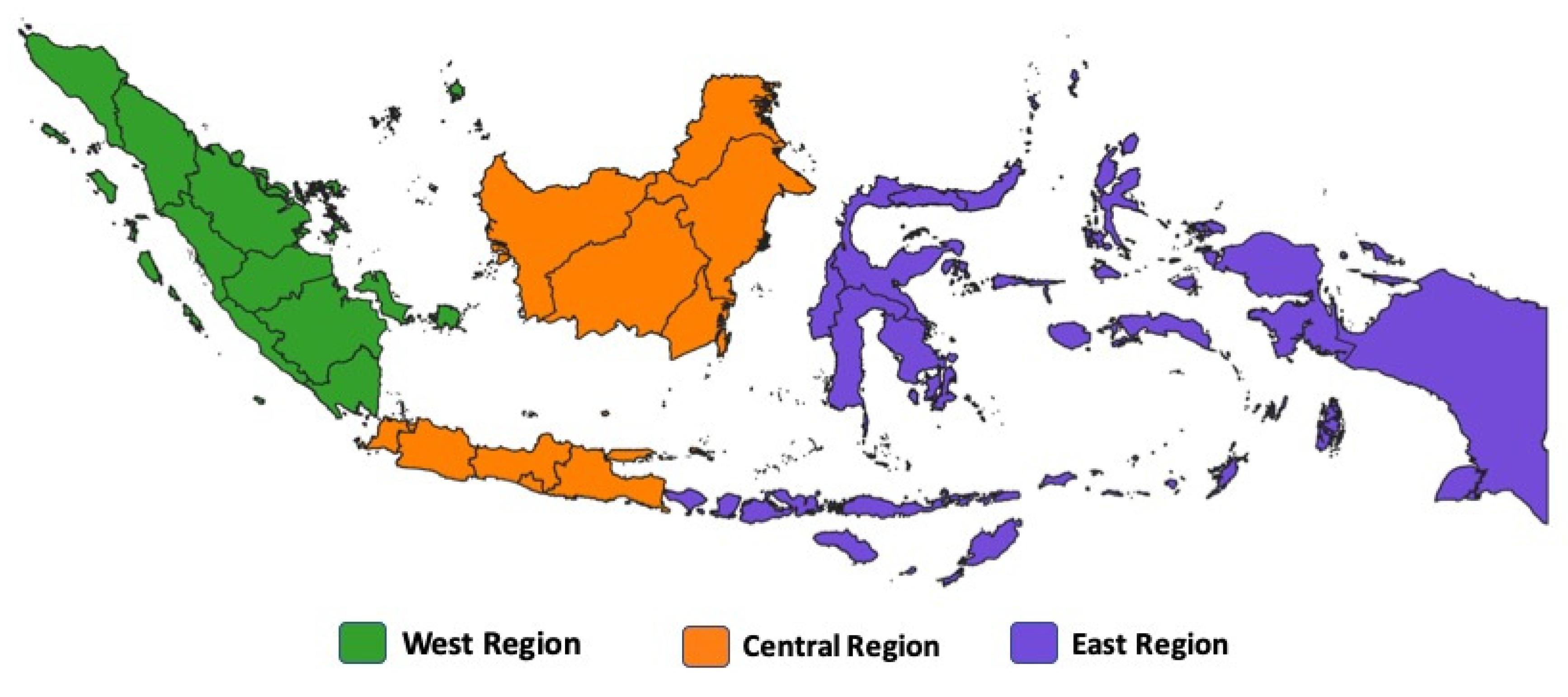
| Region | Cefotaxime and/or Ceftazidime-Resistant E. coli | ESBL-E. coli | ||||||
|---|---|---|---|---|---|---|---|---|
| N | Positive (%) | 95% CI | p-Value for
Regions Differences | N | Positive (%) | 95% CI | p-Value for
Regions Differences | |
| East | 808 | 167 (20.7) a | 18.1–23.6 | <0.001 | 767 | 55 (7.2) a | 5.5–9.2 | <0.001 |
| Central | 742 | 209 (28.2) b | 25.1–31.5 | 646 | 52 (8.0) a | 6.2–10.4 | ||
| West | 632 | 208 (32.9) b | 29.4–36.7 | 610 | 93 (15.2) b | 12.6–18.3 | ||
| Total | 2182 | 584 (26.8) | 2023 | 200 (9.9) | ||||
| Antibiotic | Resistance Status (%) | ||
|---|---|---|---|
| R | I | S | |
| Cefotaxime | 98.5 | 0.0 | 1.5 |
| Ampicillin | 97.5 | 0.5 | 2.0 |
| Sulfamethoxazole | 86.0 | 0.0 | 14.0 |
| Trimethoprim | 84.0 | 0.0 | 16.0 |
| Gentamicin | 84.0 | 0.5 | 15.5 |
| Ciprofloxacin | 72.0 | 16.0 | 12.0 |
| Nalidixic acid | 71.5 | 0.0 | 28.5 |
| Azithromycin | 62.5 | 0.0 | 37.5 |
| Tetracycline | 55.0 | 1.5 | 43.5 |
| Ceftazidime | 51.1 | 34.0 | 15.0 |
| Chloramphenicol | 17.5 | 4.5 | 78.0 |
| Colistin | 14.5 | 85.5 | 0.0 |
| Meropenem | 3.0 | 0.5 | 96.5 |
| Tigecycline | 2.5 | 0.0 | 97.5 |
| No. of Antimicrobial Classes | No. of ESBL-E. coli Isolates | Percentage |
|---|---|---|
| 2 | 3 | 1.5% |
| 3 | 4 | 2.0% |
| 4 | 16 | 8.0% |
| 5 | 39 | 19.5% |
| 6 | 62 | 31.0% |
| 7 | 56 | 28.0% |
| 8 | 14 | 7.0% |
| 9 | 6 | 3.0% |
| Total | 200 | 100% |
| Antibiotic | Class | MIC50 (µg/mL) | MIC90 (µg/mL) | GM (µg/mL) | MIC Range | MIC Breakpoint (µg/mL) |
|---|---|---|---|---|---|---|
| Sulfamethoxazole | Sulfonamides | >1024 | >1024 | 576.0 | ≤8–>1024 | ≥512 |
| Trimethoprim | Sulfonamides | 32 | >32 | 15.6 | ≤0.25–>32 | ≥16 |
| Ciprofloxacin | Quinolones | 8 | >8 | 2.5 | 0.03–>8 | ≥1 |
| Nalidixic Acid | Quinolones | 128 | >128 | 56.7 | ≤4–>128 | ≥32 |
| Colistin | Polymyxins | 1 | 8 | 1.4 | ≤1–>16 | ≥4 |
| Meropenem | Carbapenems | 0.03 | 0.06 | 0.041 | ≤0.03–>16 | ≥4 |
| Azithromycin | Macrolides | 32 | 64 | 22.6 | ≤2–>64 | ≥32 |
| Tetracycline | Tetracyclines | 32 | >64 | 13.4 | ≤2–>64 | ≥16 |
| Chloramphenicol | Phenicols | 8 | 128 | 12.5 | ≤8–>128 | ≥32 |
| Tigecycline | Tetracyclines | 0.25 | 0.5 | 0.282 | ≤0.25–4 | >0.5 |
| Ceftazidime | Cephalosporins | >8 | >8 | 6.9 | ≤0.5–>8 | ≥16 |
| Cefotaxime | Cephalosporins | 4 | >4 | 3.8 | ≤0.25–>4 | ≥4 |
| Ampicillin | Penicillins | 64 | >64 | 59.3 | 1–>64 | ≥32 |
| Gentamicin | Aminoglycosides | 32 | >32 | 18.3 | ≤0.5–>32 | ≥16 |
| Antibiotic | Region | N | MIC50 (µg/mL) | MIC90 (µg/mL) | GM (µg/mL) | p-Value |
|---|---|---|---|---|---|---|
| Sulfamethoxazole | East | 55 | 1024 | 1024 | 667.1 | 0.721 |
| Central | 52 | 1024 | 1024 | 600.8 | ||
| West | 93 | 1024 | 1024 | 515.8 | ||
| Trimethoprim | East | 55 | 32 | 32 | 17.9 | 0.712 |
| Central | 52 | 32 | 32 | 15.6 | ||
| West | 93 | 32 | 32 | 14.3 | ||
| Ciprofloxacin | East | 55 | 8 | 8 | 3.0 | 0.051 |
| Central | 52 | 2 | 8 | 1.8 | ||
| West | 93 | 8 | 8 | 2.8 | ||
| Nalidixic Acid | East | 55 | 128 | 128 | 51.7 | 0.270 |
| Central | 52 | 128 | 128 | 48.4 | ||
| West | 93 | 128 | 128 | 65.4 | ||
| Colistin | East | 55 | 1 | 1.6 | 1.3 | 0.614 |
| Central | 52 | 1 | 3.8 | 1.3 | ||
| West | 93 | 1 | 8 | 1.6 | ||
| Meropenem | East | 55 | 0.03 | 0.162 | 0.051 | 0.095 |
| Central | 52 | 0.03 | 0.06 | 0.037 | ||
| West | 93 | 0.03 | 0.03 | 0.037 | ||
| Azithromycin | East | 55 | 32 | 64 | 28.6 | 0.085 |
| Central | 52 | 32 | 64 | 19.0 | ||
| West | 93 | 32 | 64 | 21.7 | ||
| Tetracycline | East | 55 | 64 | 64 | 17.9 a | 0.044 |
| Central | 52 | 64 | 64 | 15.8 ab | ||
| West | 93 | 8 | 64 | 10.3 b | ||
| Chloramphenicol | East | 55 | 8 | 32 | 10.4 a | 0.036 |
| Central | 52 | 8 | 15.2 | 10.4 a | ||
| West | 93 | 8 | 128 | 15.4 b | ||
| Tigecycline | East | 55 | 0.25 | 0.5 | 0.302 | 0.629 |
| Central | 52 | 0.25 | 0.475 | 0.271 | ||
| West | 93 | 0.25 | 0.25 | 0.277 | ||
| Ceftazidime | East | 55 | 8 | 8 | 7.1 | 0.607 |
| Central | 52 | 8 | 8 | 6.7 | ||
| West | 93 | 8 | 8 | 6.8 | ||
| Cefotaxime | East | 55 | 4 | 4 | 3.4 | 0.064 |
| Central | 52 | 4 | 4 | 4.0 | ||
| West | 93 | 4 | 4 | 3.9 | ||
| Ampicillin | East | 55 | 64 | 64 | 56.4 | 0.528 |
| Central | 52 | 64 | 64 | 59.1 | ||
| West | 93 | 64 | 64 | 61.2 | ||
| Gentamicin | East | 55 | 32 | 32 | 16.4 | 0.570 |
| Central | 52 | 32 | 32 | 19.8 | ||
| West | 93 | 32 | 32 | 18.7 |
| Region | N | ESBL Resistance Genes | |||||
|---|---|---|---|---|---|---|---|
| blaCTX-M | blaCTX-M-1 | blaCTX-M-9 | blaTEM | blaSHV | blaOXA-1 | ||
| East | 55 | 55 (100%) | 55 (100%) | 1 (1.8%) | 19 (34.5%) | 0 | 0 |
| Central | 52 | 49 (94.2%) | 49 (94.2%) | 3 (5.8%) | 20 (38.5%) | 0 | 0 |
| West | 93 | 91 (97.8%) | 91 (97.8%) | 1 (1.1%) | 27 (29.0%) | 0 | 0 |
| Total | 200 | 195 (97.5%) | 195 (97.5%) | 5 (2.5%) | 66 (33.0%) | 0 | 0 |
| Region | Phylogenetic Group | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| A | B1 | B2 | C | D | E | F | ||
| East | 24 (43.6%) a | 7 (12.7%) a | 0 (0.0%) a | 2 (3.6%) a | 0 (0.0%) a | 21 (38.2%) a | 1 (1.8%) a | 55 |
| Central | 17 (32.7%) a | 12 (23.1%) a | 0 (0.0%) a | 1 (1.9%) a | 0 (0.0%) a | 14 (26.9%) a,b | 8 (15.4%) a | 52 |
| West | 43 (46.2%) a | 22 (23.7%) a | 0 (0.0%) a | 2 (2.2%) a | 4 (4.3%) a | 10 (10.8%) b | 12 (12.9%) a | 93 |
| Total | 84 (42.0%) | 41 (20.5%) | 0 (0.0%) | 5 (2.5%) | 4 (2.0%) | 45 (22.5%) | 21 (10.5%) | 200 |
| Gene Targeted | Sequence (5′-3′) | Amplicon Size (bp) | Purpose | Reference |
|---|---|---|---|---|
| blaTEM | CATTTCCGTGTCGCCCTTATTC CGTTCATCCATAGTTGCCTGAC | 800 | Multiplex PCR | [60] |
| blaSHV | AGCCGCTTGAGCAAATTAAAC ATCCCGCAGATAAATCACCAC | 713 | Multiplex PCR | [60] |
| blaOXA-1 | GGCACCAGATTCAACTTTCAAG GACCCCAAGTTTCCTGTAAGTG | 564 | Multiplex PCR | [60] |
| blaCTX-M-1 | TTAGGAAGTGTGCCGCTGTA CGGTTTTATCCCCCACAAC | 655 | Multiplex PCR | [59] |
| blaCTX-M-9 | GGTGATGAACGCTTTCCAAT TTATCACCTGCAGTCCACGA | 518 | Multiplex PCR | [59] |
| blaCTX-M | CGATGTGCAGTACCAGTAA TTAGTGACCAGAATCAGCGG | 585 | Singleplex PCR | [61] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hidayatullah, N.; Suandy, I.; Intanon, M.; Alter, T.; Susanti, O.; Herpianti, A.; Susanty, S.; Desitania, R.; Awaiwanont, N. Occurrence and Molecular Characterization of Extended-Spectrum Beta-Lactamase (ESBL)-Producing Escherichia coli in Broilers in Indonesia. Antibiotics 2025, 14, 1030. https://doi.org/10.3390/antibiotics14101030
Hidayatullah N, Suandy I, Intanon M, Alter T, Susanti O, Herpianti A, Susanty S, Desitania R, Awaiwanont N. Occurrence and Molecular Characterization of Extended-Spectrum Beta-Lactamase (ESBL)-Producing Escherichia coli in Broilers in Indonesia. Antibiotics. 2025; 14(10):1030. https://doi.org/10.3390/antibiotics14101030
Chicago/Turabian StyleHidayatullah, Nur, Imron Suandy, Montira Intanon, Thomas Alter, Oli Susanti, Ajeng Herpianti, Sani Susanty, Riska Desitania, and Nattakarn Awaiwanont. 2025. "Occurrence and Molecular Characterization of Extended-Spectrum Beta-Lactamase (ESBL)-Producing Escherichia coli in Broilers in Indonesia" Antibiotics 14, no. 10: 1030. https://doi.org/10.3390/antibiotics14101030
APA StyleHidayatullah, N., Suandy, I., Intanon, M., Alter, T., Susanti, O., Herpianti, A., Susanty, S., Desitania, R., & Awaiwanont, N. (2025). Occurrence and Molecular Characterization of Extended-Spectrum Beta-Lactamase (ESBL)-Producing Escherichia coli in Broilers in Indonesia. Antibiotics, 14(10), 1030. https://doi.org/10.3390/antibiotics14101030






