In Vivo Effect of Halicin on Methicillin-Resistant Staphylococcus aureus-Infected Caenorhabditis elegans and Its Clinical Potential
Abstract
1. Introduction
2. Results
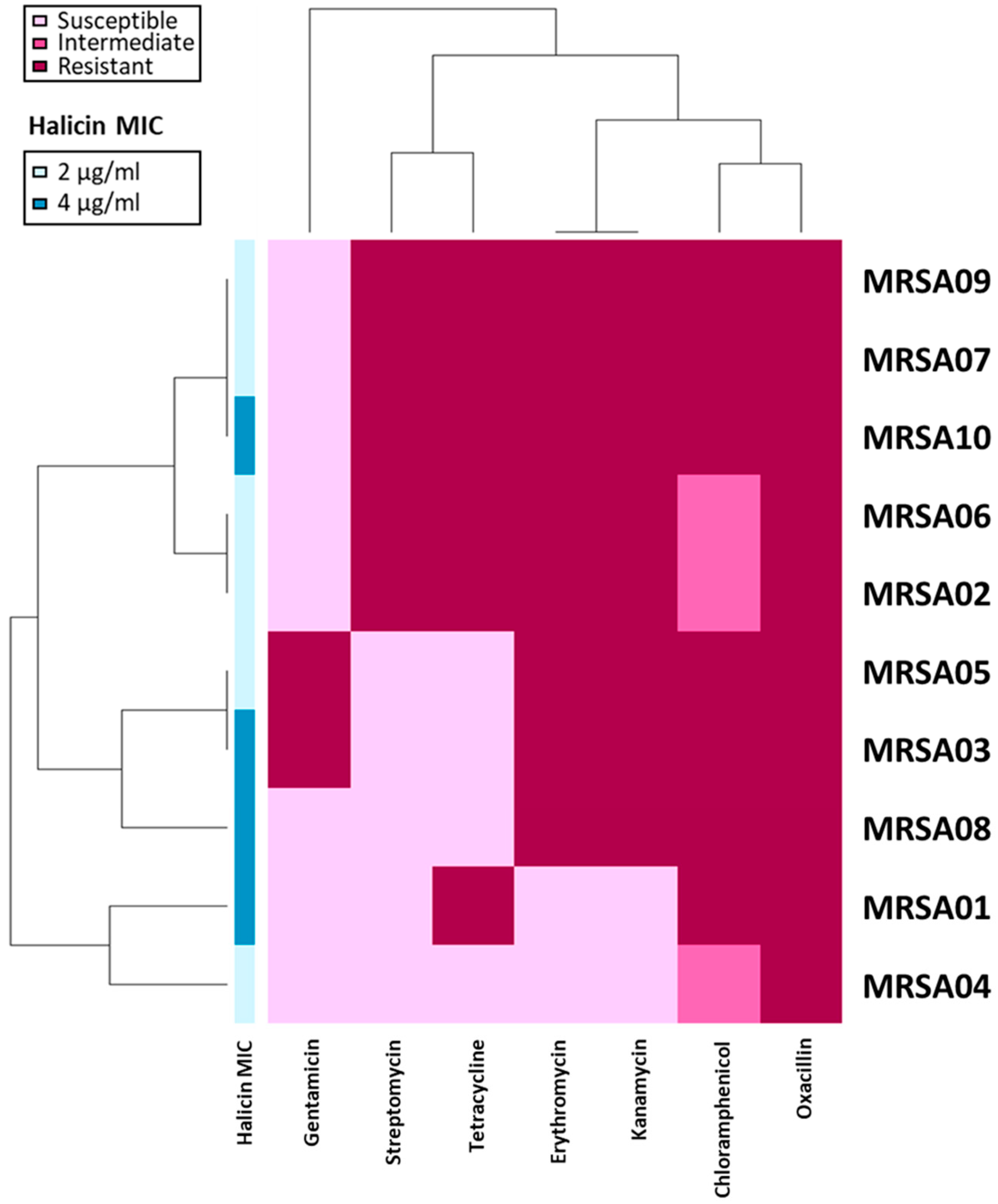
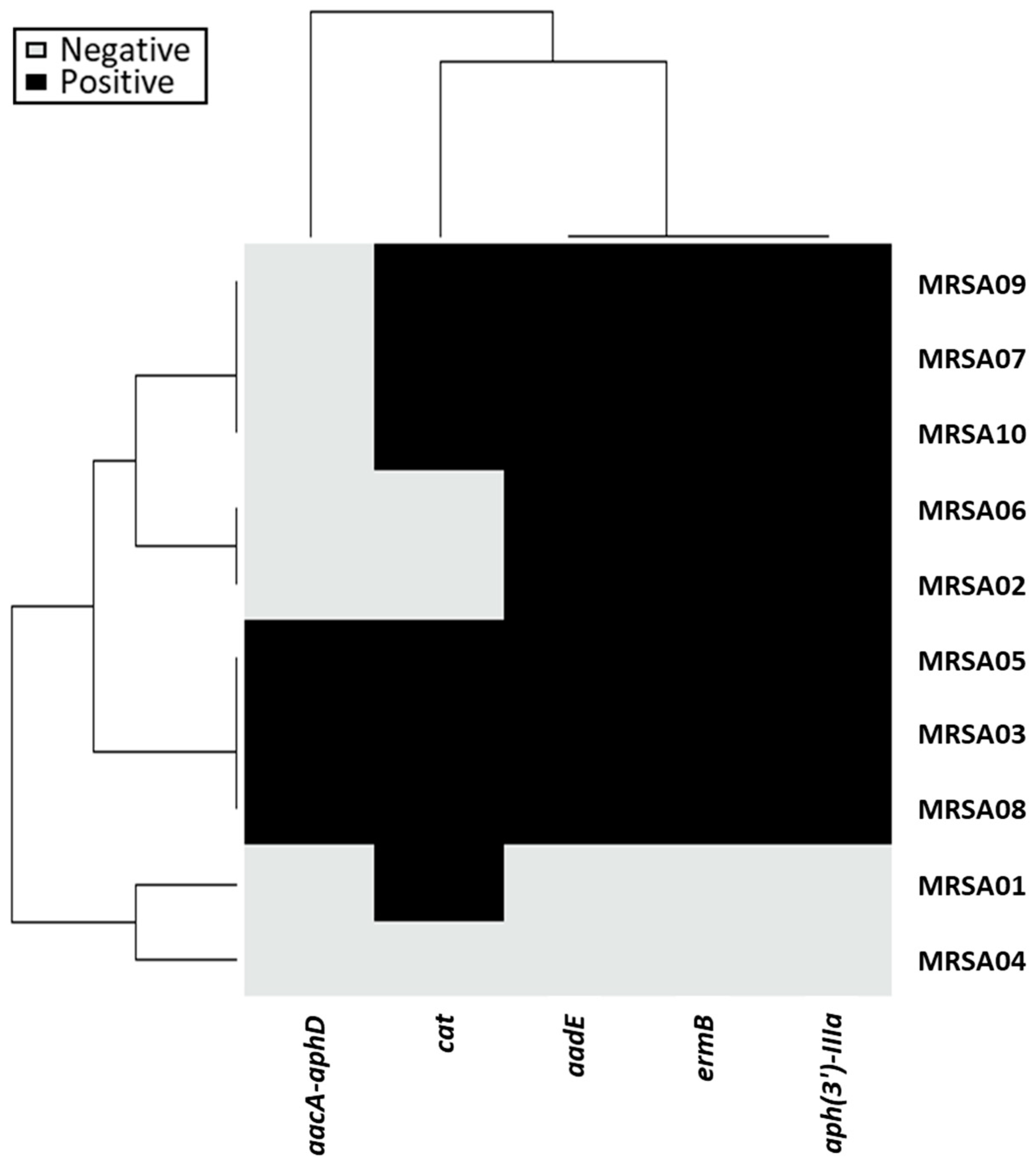
2.1. Characterization of MRSA Strains in This Study
2.2. Antibacterial Activity of Halicin
2.3. In Vivo Assessment of Halicin
3. Discussion
4. Materials and Methods
4.1. Bacterial Collection
4.2. Antimicrobial Susceptibility Testing
4.3. Gene Detection
4.4. Caenorhabditis Elegans In Vivo Study
4.5. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Foster, T.J. Staphylococcus aureus. Mol. Med. Microbiol. 2002, 2, 839–888. [Google Scholar]
- Howden, B.P.; Giulieri, S.G.; Wong Fok Lung, T.; Baines, S.L.; Sharkey, L.K.; Lee, J.Y.H.; Hachani, A.; Monk, I.R.; Stinear, T.P. Staphylococcus aureus host interactions and adaptation. Nat. Rev. Microbiol. 2023, 21, 380–395. [Google Scholar] [CrossRef] [PubMed]
- Taylor, T.A.; Unakal, C.G. Staphylococcus aureus Infection. In StatPearls; Ineligible Companies: Treasure Island, FL, USA, 2024. [Google Scholar]
- David, M.Z.; Daum, R.S. Treatment of Staphylococcus aureus infections. Curr. Top Microbiol. Immunol. 2017, 409, 325–383. [Google Scholar] [PubMed]
- Barber, M. Methicillin-resistant staphylococci. J. Clin. Pathol. 1961, 14, 385–393. [Google Scholar] [CrossRef]
- Stapleton, P.D.; Taylor, P.W. Methicillin resistance in Staphylococcus aureus: Mechanisms and modulation. Sci. Prog. 2002, 85, 57–72. [Google Scholar] [CrossRef]
- Peacock, S.J.; Paterson, G.K. Mechanisms of methicillin resistance in Staphylococcus aureus. Annu. Rev. Biochem. 2015, 84, 577–601. [Google Scholar] [CrossRef]
- Bæk, K.T.; Gründling, A.; Mogensen, R.G.; Thøgersen, L.; Petersen, A.; Paulander, W.; Frees, D. β-Lactam resistance in methicillin-resistant Staphylococcus aureus USA300 is increased by inactivation of the ClpXP protease. Antimicrob. Agents Chemother. 2014, 58, 4593–4603. [Google Scholar] [CrossRef]
- Hryniewicz, W. Epidemiology of MRSA. Infection 1999, 27 (Suppl. S2), S13–S16. [Google Scholar] [CrossRef]
- Herwaldt, L.A. Control of methicillin-resistant Staphylococcus aureus in the hospital setting. Am. J. Med. 1999, 106, 11S–18S; discussion 48S–52S. [Google Scholar] [CrossRef]
- Pittet, D.; Hugonnet, S.; Harbarth, S.; Mourouga, P.; Sauvan, V.; Touveneau, S.; Perneger, T.V. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet 2000, 356, 1307–1312. [Google Scholar] [CrossRef]
- Okuma, K.; Iwakawa, K.; Turnidge, J.D.; Grubb, W.B.; Bell, J.M.; O’Brien, F.G.; Coombs, G.W.; Pearman, J.W.; Tenover, F.C.; Kapi, M.; et al. Dissemination of new methicillin-resistant Staphylococcus aureus clones in the community. J. Clin. Microbiol. 2002, 40, 4289–4294. [Google Scholar] [CrossRef] [PubMed]
- Abramson, M.A.; Sexton, D.J. Nosocomial methicillin-resistant and methicillin-susceptible Staphylococcus aureus primary bacteremia: At what costs? Infect. Control Hosp. Epidemiol. 1999, 20, 408–411. [Google Scholar] [CrossRef] [PubMed]
- Köck, R.; Becker, K.; Cookson, B.; van Gemert-Pijnen, J.; Harbarth, S.; Kluytmans, J.; Mielke, M.; Peters, G.; Skov, R.; Struelens, M. Methicillin-resistant Staphylococcus aureus (MRSA): Burden of disease and control challenges in Europe. Euro. Surveill. 2010, 15, 19688. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, P.; Rajbhandari, P.; Nagaraja, S.; Shrestha, P.; Grigoryan, R.; Satyanarayana, S.; Davtyan, H. Prevalence of methicillin-resistant Staphylococcus aureus in a tertiary hospital in Nepal. Public Health Action 2021, 11, 46–51. [Google Scholar] [CrossRef]
- Hsueh, P.R.; Liu, C.Y.; Luh, K.T. Current status of antimicrobial resistance in Taiwan. Emerg. Infect. Dis. 2002, 8, 132–137. [Google Scholar] [CrossRef]
- Changchien, C.-H.; Chen, S.-W.; Chen, Y.-Y.; Chu, C. Antibiotic susceptibility and genomic variations in Staphylococcus aureus associated with skin and soft tissue infection (SSTI) disease groups. BMC Infect. Dis. 2016, 16, 276. [Google Scholar] [CrossRef]
- Lu, P.-L.; Chin, L.-C.; Peng, C.-F.; Chiang, Y.-H.; Chen, T.-P.; Ma, L.; Siu, L. Risk factors and molecular analysis of community methicillin-resistant Staphylococcus aureus carriage. J. Clin. Microbiol. 2005, 43, 132–139. [Google Scholar] [CrossRef]
- Rajpurkar, P.; Chen, E.; Banerjee, O.; Topol, E.J. AI in health and medicine. Nat. Med. 2022, 28, 31–38. [Google Scholar] [CrossRef]
- Branda, F.; Scarpa, F. Implications of artificial intelligence in addressing antimicrobial resistance: Innovations, global Challenges, and healthcare’s future. Antibiotics 2024, 13, 502. [Google Scholar] [CrossRef]
- Masoudi-Sobhanzadeh, Y.; Omidi, Y.; Amanlou, M.; Masoudi-Nejad, A. Drug databases and their contributions to drug repurposing. Genomics 2020, 112, 1087–1095. [Google Scholar] [CrossRef]
- Stokes, J.M.; Yang, K.; Swanson, K.; Jin, W.; Cubillos-Ruiz, A.; Donghia, N.M.; MacNair, C.R.; French, S.; Carfrae, L.A.; Bloom-Ackermann, Z.; et al. A deep learning approach to antibiotic discovery. Cell 2020, 180, 688–702.e13. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Lin, S.; Han, L.; Zhang, J.; Liu, S.; Yang, X.; Wang, R.; Yang, X.; Yi, Y. Safety and efficacy evaluation of halicin as an effective drug for inhibiting intestinal infections. Front. Pharmacol. 2024, 15, 1389293. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zhao, K.; Chen, Z.; Liu, D.; Tang, S.; Sun, C.; Chen, H.; Wang, Y.; Wu, C. Halicin: A new horizon in antibacterial therapy against veterinary pathogens. Antibiotics 2024, 13, 492. [Google Scholar] [CrossRef] [PubMed]
- Higashihira, S.; Simpson, S.J.; Morita, A.; Suryavanshi, J.R.; Arnold, C.J.; Natoli, R.M.; Greenfield, E.M. Halicin remains active against Staphylococcus aureus in biofilms grown on orthopaedically relevant substrates. Bone Jt. Res. 2024, 13, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Higashihira, S.; Simpson, S.J.; Collier, C.D.; Natoli, R.M.; Kittaka, M.; Greenfield, E.M. Halicin is effective against Staphylococcus aureus biofilms in vitro. Clin. Orthop. Relat. Res. 2022, 480, 1476–1487. [Google Scholar] [CrossRef]
- Bouhrour, N.; van der Reijden, T.J.K.; Voet, M.M.; Schonkeren-Ravensbergen, B.; Cordfunke, R.A.; Drijfhout, J.W.; Bendali, F.; Nibbering, P.H. Novel antibacterial agents SAAP-148 and halicin combat Gram-negative bacteria colonizing catheters. Antibiotics 2023, 12, 1743. [Google Scholar] [CrossRef]
- van Gent, M.E.; van der Reijden, T.J.K.; Lennard, P.R.; de Visser, A.W.; Schonkeren-Ravensbergen, B.; Dolezal, N.; Cordfunke, R.A.; Drijfhout, J.W.; Nibbering, P.H. Synergism between the synthetic antibacterial and antibiofilm peptide (SAAP)-148 and halicin. Antibiotics 2022, 11, 673. [Google Scholar] [CrossRef]
- Li, H.; Xu, L.; Liu, Y.; She, P.; Wu, Y. Antibacterial effects of small molecule antidiabetic agent halicin against Staphylococcus aureus. Chin. J. Lab. Med. 2021, 12, 1029–1034. [Google Scholar]
- Booq, R.Y.; Tawfik, E.A.; Alfassam, H.A.; Alfahad, A.J.; Alyamani, E.J. Assessment of the Antibacterial Efficacy of Halicin against Pathogenic Bacteria. Antibiotics 2021, 10, 1480. [Google Scholar] [CrossRef]
- Jang, S.; Javadov, S. Inhibition of JNK aggravates the recovery of rat hearts after global ischemia: The role of mitochondrial JNK. PLoS ONE 2014, 9, e113526. [Google Scholar] [CrossRef]
- Gehringer, M.; Muth, F.; Koch, P.; Laufer, S.A. c-Jun N-terminal kinase inhibitors: A patent review (2010–2014). Expert Opin. Ther. Pat 2015, 25, 849–872. [Google Scholar] [CrossRef] [PubMed]
- Hung, W.C.; Wan, T.W.; Kuo, Y.C.; Yamamoto, T.; Tsai, J.C.; Lin, Y.T.; Hsueh, P.R.; Teng, L.J. Molecular evolutionary pathways toward two successful community-associated but multidrug-resistant ST59 methicillin-resistant Staphylococcus aureus Lineages in Taiwan: Dynamic modes of mobile genetic element salvages. PLoS ONE 2016, 11, e0162526. [Google Scholar] [CrossRef] [PubMed]
- Clinical & Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing: Twenty-Seventh Informational Supplement. Document M100-S34 CLSI; Clinical & Laboratory Standards Institute (CLSI): Wayne, PA, USA, 2024. [Google Scholar]
- van Wamel, W.J.; Rooijakkers, S.H.; Ruyken, M.; van Kessel, K.P.; van Strijp, J.A. The innate immune modulators staphylococcal complement inhibitor and chemotaxis inhibitory protein of Staphylococcus aureus are located on beta-hemolysin-converting bacteriophages. J. Bacteriol. 2006, 188, 1310–1315. [Google Scholar] [CrossRef] [PubMed]
- Takano, T.; Higuchi, W.; Zaraket, H.; Otsuka, T.; Baranovich, T.; Enany, S.; Saito, K.; Isobe, H.; Dohmae, S.; Ozaki, K.; et al. Novel characteristics of community-acquired methicillin-resistant Staphylococcus aureus strains belonging to multilocus sequence type 59 in Taiwan. Antimicrob. Agents Chemother. 2008, 52, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.C.; Huang, Y.T.; Chen, C.S.; Chen, Y.W.; Huang, Y.T.; Su, J.C.; Teng, L.J.; Shiau, C.W.; Chiu, H.C. In vitro and in vivo activity of a novel sorafenib derivative SC5005 against MRSA. J. Antimicrob. Chemother. 2016, 71, 449–459. [Google Scholar] [CrossRef]
- Ermolaeva, M.A.; Schumacher, B. Insights from the worm: The C. elegans model for innate immunity. Semin. Immunol. 2014, 26, 303–309. [Google Scholar] [CrossRef]

| Clinical Isolate | PVL | seb | hlb | chp | sak | scn | sea | sep |
|---|---|---|---|---|---|---|---|---|
| MRSA01 | + | + | + | + | − | + | − | − |
| MRSA02 | + | + | + | + | − | + | − | − |
| MRSA03 | + | + | + | − | + | + | − | + |
| MRSA04 | + | + | + | + | − | + | − | − |
| MRSA05 | − | + | + | − | + | + | − | + |
| MRSA06 | + | + | + | + | − | + | − | − |
| MRSA07 | + | + | + | + | − | + | − | − |
| MRSA08 | − | + | + | − | + | + | − | + |
| MRSA09 | + | + | + | + | − | + | − | − |
| MRSA10 | + | + | + | + | − | + | − | − |
| Total proportion | 80% | 100% | 100% | 70% | 30% | 100% | 0% | 30% |
| Lab Strain 1 | Halicin MIC (µg/mL) |
|---|---|
| MSSA ATCC 29213 | 2 |
| MRSA ATCC 33592 | 2 |
| MRSA USA300 | 4 |
| hVISA Mu3 | 2 |
| VISA Mu50 | 1 |
| Methicillin-Resistant S. aureus Clinical Strains | Halicin | |||
| MIC Range (µg/mL) | MIC50 (µg/mL) | MIC90 (µg/mL) | Mode of MIC (µg/mL) | |
| 2–4 | 2 | 4 | 2 | |
| Treatment | Median Time (Days) | p Value | Hazard Ratio | 95% Confidence Interval (CI) | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| control | 4 | - | Reference | ||
| 4 µg/mL halicin | 5.5 | <0.0001 | 0.493 | 0.309 | 0.785 |
| 8 µg/mL halicin | 6 | <0.0001 | 0.432 | 0.267 | 0.698 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kao, L.-T.; Yang, T.-Y.; Hung, W.-C.; Yang, W.-T.; He, P.; Chen, B.-X.; Wang, Y.-C.; Chen, S.-S.; Lai, Y.-W.; Wang, H.-Y.; et al. In Vivo Effect of Halicin on Methicillin-Resistant Staphylococcus aureus-Infected Caenorhabditis elegans and Its Clinical Potential. Antibiotics 2024, 13, 906. https://doi.org/10.3390/antibiotics13090906
Kao L-T, Yang T-Y, Hung W-C, Yang W-T, He P, Chen B-X, Wang Y-C, Chen S-S, Lai Y-W, Wang H-Y, et al. In Vivo Effect of Halicin on Methicillin-Resistant Staphylococcus aureus-Infected Caenorhabditis elegans and Its Clinical Potential. Antibiotics. 2024; 13(9):906. https://doi.org/10.3390/antibiotics13090906
Chicago/Turabian StyleKao, Li-Ting, Tsung-Ying Yang, Wei-Chun Hung, Wei-Te Yang, Pu He, Bo-Xuan Chen, Yu-Chi Wang, Shiou-Sheng Chen, Yu-Wei Lai, Hsian-Yu Wang, and et al. 2024. "In Vivo Effect of Halicin on Methicillin-Resistant Staphylococcus aureus-Infected Caenorhabditis elegans and Its Clinical Potential" Antibiotics 13, no. 9: 906. https://doi.org/10.3390/antibiotics13090906
APA StyleKao, L.-T., Yang, T.-Y., Hung, W.-C., Yang, W.-T., He, P., Chen, B.-X., Wang, Y.-C., Chen, S.-S., Lai, Y.-W., Wang, H.-Y., & Tseng, S.-P. (2024). In Vivo Effect of Halicin on Methicillin-Resistant Staphylococcus aureus-Infected Caenorhabditis elegans and Its Clinical Potential. Antibiotics, 13(9), 906. https://doi.org/10.3390/antibiotics13090906








