Microbiological Profile of Instrumented Spinal Infections: 10-Year Study at a French Spine Center
Abstract
1. Introduction
2. Results
2.1. Study Population
2.2. Microbiological Findings
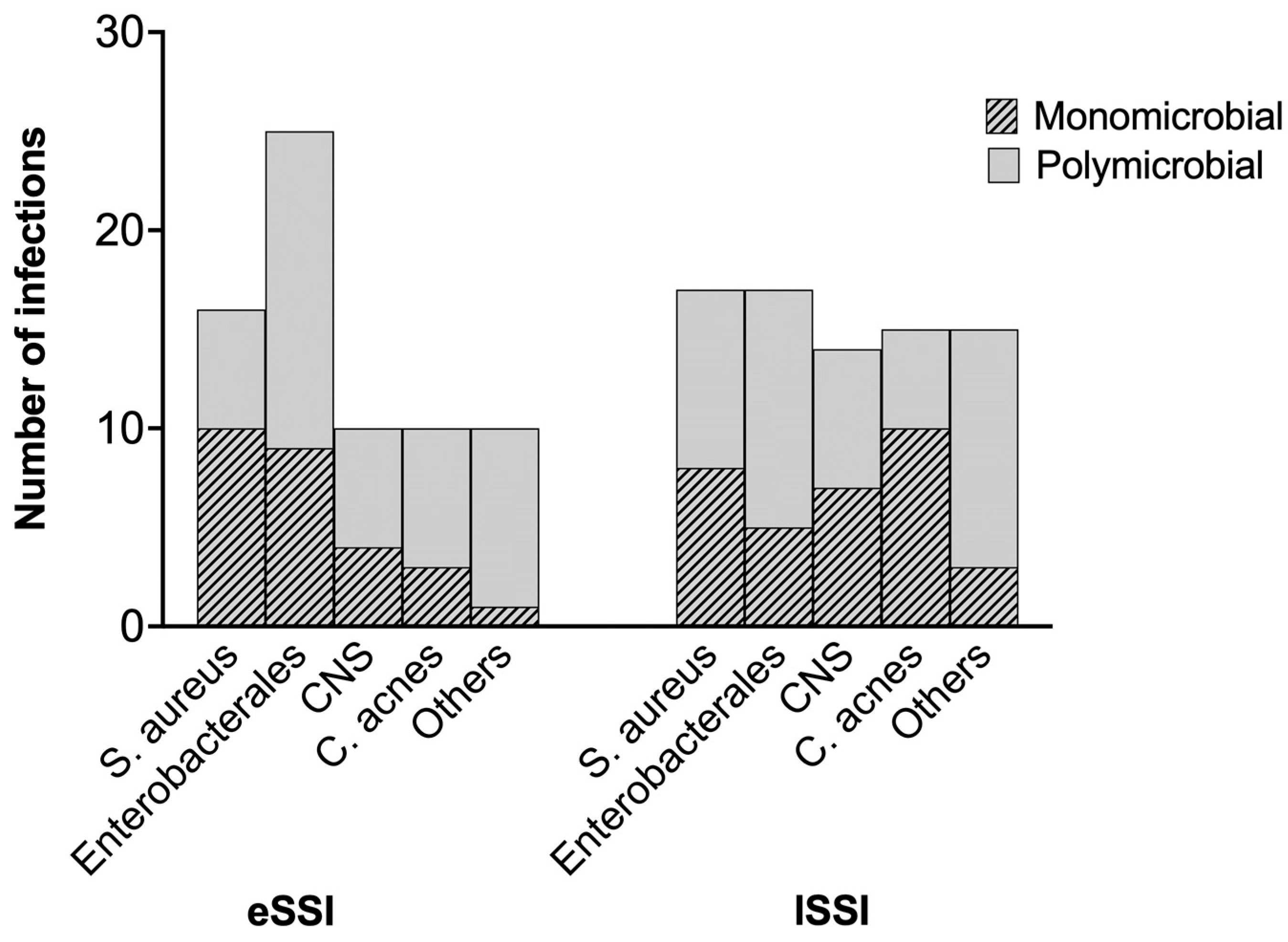
2.2.1. Early Infections (n = 46)
| Monomicrobial (n = 27) (%) | Polymicrobial (n = 19) (%) | Total (n = 46) (%) | |
|---|---|---|---|
| Staphylococcus aureus | 10 (37) | 6 (31.6) | 16 (31.6) |
| Escherichia coli | 5 (18.5) | 6 (31.6) | 11 (23.9) |
| Cutibacterium acnes | 3 (11.1) | 7 (36.8) | 10 (21.7) |
| Staphylococcus epidermidis | 3 (11.1) | 5 (26.3) | 8 (17.8) |
| Proteus mirabilis | 1 (3.7) | 4 (21.1) | 5 (10.9) |
| Klebsiella pneumoniae | - | 3 (15.8) | 3 (6.5) |
| Klebsiella oxytoca | 1 (3.7) | 1 (5.3) | 2 (4.3) |
| Enterobacter cloacae | 2 (7.4) | - | 2 (4.3) |
| Pseudomonas aeruginosa | - | 2 (10.5) | 2 (4.3) |
| Enterococcus faecalis | - | 3 (15.8) | 2 (4.3) |
| Staphylococcus capitis | 1 (3.7) | - | 1 (2.2) |
| Streptococcus anginosus | - | 2 (10.5) | 2 (4.3) |
| Bacteroides fragilis | - | 2 (10.5) | 2 (4.3) |
| Citrobacter koseri | - | 1 (5.3) | 1 (2.2) |
| Staphylococcus saccharolyticus | - | 1 (5.3) | 1 (2.2) |
| Corynebacterium striatum | 1 (3.7) | - | 1 (2.2) |
2.2.2. Late Infections (n = 50)
2.3. Surgical and Antibiotic Treatment
2.3.1. Early Infections (n = 46)
2.3.2. Late Infections
2.4. Follow-Up
3. Discussion
4. Materials and Methods
4.1. Patients and Samples
4.2. Treatment and Follow-Up
4.3. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Al Farii, H.; Slawaska-Eng, D.; Pankovitch, S.; Navarro-Ramirez, R.; Weber, M. Gram-Negative Surgical Site Infections after 989 Spinal Fusion Procedures: Associated Factors and the Role of Gram-Negative Prophylactic Antibiotic Coverage. Int. J. Spine Surg. 2021, 15, 341–347. [Google Scholar] [CrossRef]
- Pull ter Gunne, A.F.; van Laarhoven, C.J.H.M.; Cohen, D.B. Incidence of Surgical Site Infection Following Adult Spinal Deformity Surgery: An Analysis of Patient Risk. Eur. Spine J. 2010, 19, 982–988. [Google Scholar] [CrossRef]
- Peng, X.-Q.; Sun, C.-G.; Fei, Z.-G.; Zhou, Q.-J. Risk Factors for Surgical Site Infection after Spinal Surgery: A Systematic Review and Meta-Analysis Based on Twenty-Seven Studies. World Neurosurg. 2019, 123, e318–e329. [Google Scholar] [CrossRef]
- Abdul-Jabbar, A.; Takemoto, S.; Weber, M.H.; Hu, S.S.; Mummaneni, P.V.; Deviren, V.; Ames, C.P.; Chou, D.; Weinstein, P.R.; Burch, S.; et al. Surgical Site Infection in Spinal Surgery: Description of Surgical and Patient-Based Risk Factors for Postoperative Infection Using Administrative Claims Data. Spine 2012, 37, 1340–1345. [Google Scholar] [CrossRef]
- Fang, A.; Hu, S.S.; Endres, N.; Bradford, D.S. Risk Factors for Infection after Spinal Surgery. Spine 2005, 30, 1460–1465. [Google Scholar] [CrossRef]
- Dubée, V.; Leflon-Guibout, V.; Lenoir, T.; Fantin, B. Les Infections Du Site Opératoire Après Chirurgie Rachidienne Instrumentée. J. Anti-Infect. 2012, 14, 68–77. [Google Scholar] [CrossRef]
- Schierholz, J.M.; Beuth, J. Implant Infections: A Haven for Opportunistic Bacteria. J. Hosp. Infect. 2001, 49, 87–93. [Google Scholar] [CrossRef]
- Radcliff, K.E.; Neusner, A.D.; Millhouse, P.W.; Harrop, J.D.; Kepler, C.K.; Rasouli, M.R.; Albert, T.J.; Vaccaro, A.R. What Is New in the Diagnosis and Prevention of Spine Surgical Site Infections. Spine J. 2015, 15, 336–347. [Google Scholar] [CrossRef]
- Kohler, P.; Eshaghi, A.; Kim, H.C.; Plevneshi, A.; Green, K.; Willey, B.M.; McGeer, A.; Patel, S.N. Toronto Invasive Bacterial Diseases Network (TIBDN) Prevalence of Vancomycin-Variable Enterococcus Faecium (VVE) among vanA-Positive Sterile Site Isolates and Patient Factors Associated with VVE Bacteremia. PLoS ONE 2018, 13, e0193926. [Google Scholar] [CrossRef]
- Kowalski, T.J.; Berbari, E.F.; Huddleston, P.M.; Steckelberg, J.M.; Mandrekar, J.N.; Osmon, D.R. The Management and Outcome of Spinal Implant Infections: Contemporary Retrospective Cohort Study. Clin. Infect. Dis. 2007, 44, 913–920. [Google Scholar] [CrossRef] [PubMed]
- Shillingford, J.N.; Laratta, J.L.; Reddy, H.; Ha, A.; Lehman, R.A.; Lenke, L.G.; Fischer, C.R. Postoperative Surgical Site Infection after Spine Surgery: An Update from the Scoliosis Research Society (SRS) Morbidity and Mortality Database. Spine Deform. 2018, 6, 634–643. [Google Scholar] [CrossRef] [PubMed]
- Rico Nieto, A.; Loeches Yagüe, B.; Quiles Melero, I.; Talavera Buedo, G.; Pizones, J.; Fernández-Baillo Sacristana, N. Descriptive Study of Spinal Instrumentation-Related Infections in a Tertiary Hospital. Rev. Esp. Cir. Ortop. Traumatol. 2024, 68, 201–208. [Google Scholar] [CrossRef]
- Gerometta, A.; Olaverri, J.C.R.; Bitan, F. Infections in Spinal Instrumentation. Int. Orthop. 2012, 36, 457–464. [Google Scholar] [CrossRef]
- Cizik, A.M.; Lee, M.J.; Martin, B.I.; Bransford, R.J.; Bellabarba, C.; Chapman, J.R.; Mirza, S.K. Using the Spine Surgical Invasiveness Index to Identify Risk of Surgical Site Infection: A Multivariate Analysis. J. Bone Jt. Surg. Am. 2012, 94, 335–342. [Google Scholar] [CrossRef]
- Olsen, M.A.; Nepple, J.J.; Riew, K.D.; Lenke, L.G.; Bridwell, K.H.; Mayfield, J.; Fraser, V.J. Risk Factors for Surgical Site Infection Following Orthopaedic Spinal Operations. J. Bone Jt. Surg. Am. 2008, 90, 62–69. [Google Scholar] [CrossRef]
- Epstein, N.E. Do Silver-Impregnated Dressings Limit Infections after Lumbar Laminectomy with Instrumented Fusion? Surg. Neurol. 2007, 68, 483–485, discussion 485. [Google Scholar] [CrossRef]
- Friedman, N.D.; Sexton, D.J.; Connelly, S.M.; Kaye, K.S. Risk Factors for Surgical Site Infection Complicating Laminectomy. Infect. Control Hosp. Epidemiol. 2007, 28, 1060–1065. [Google Scholar] [CrossRef] [PubMed]
- Köder, K.; Hardt, S.; Gellert, M.S.; Haupenthal, J.; Renz, N.; Putzier, M.; Perka, C.; Trampuz, A. Outcome of Spinal Implant-Associated Infections Treated with or without Biofilm-Active Antibiotics: Results from a 10-Year Cohort Study. Infection 2020, 48, 559–568. [Google Scholar] [CrossRef]
- Núñez-Pereira, S.; Rodríguez-Pardo, D.; Pellisé, F.; Pigrau, C.; Bagó, J.; Villanueva, C.; Cáceres, E. Postoperative Urinary Tract Infection and Surgical Site Infection in Instrumented Spinal Surgery: Is There a Link? Clin. Microbiol. Infect. 2014, 20, 768–773. [Google Scholar] [CrossRef] [PubMed]
- Mok, J.M.; Cloyd, J.M.; Bradford, D.S.; Hu, S.S.; Deviren, V.; Smith, J.A.; Tay, B.; Berven, S.H. Reoperation after Primary Fusion for Adult Spinal Deformity: Rate, Reason, and Timing. Spine 2009, 34, 832–839. [Google Scholar] [CrossRef] [PubMed]
- Cahill, P.J.; Warnick, D.E.; Lee, M.J.; Gaughan, J.; Vogel, L.E.; Hammerberg, K.W.; Sturm, P.F. Infection after Spinal Fusion for Pediatric Spinal Deformity: Thirty Years of Experience at a Single Institution. Spine 2010, 35, 1211–1217. [Google Scholar] [CrossRef]
- Hedge, A.; Mohan, S.; Lim, W.E.H. Infections of the Deep Neck Spaces. Singap. Med. J. 2012, 53, 305–311, quiz 312. [Google Scholar]
- Wille, H.; Dauchy, F.-A.; Desclaux, A.; Dutronc, H.; Vareil, M.-O.; Dubois, V.; Vital, J.-M.; Dupon, M. Efficacy of Debridement, Antibiotic Therapy and Implant Retention within Three Months during Postoperative Instrumented Spine Infections. Infect. Dis. 2017, 49, 261–267. [Google Scholar] [CrossRef]
- Fernandez-Gerlinger, M.-P.; Arvieu, R.; Lebeaux, D.; Rouis, K.; Guigui, P.; Mainardi, J.-L.; Bouyer, B. Successful 6-Week Antibiotic Treatment for Early Surgical-Site Infections in Spinal Surgery. Clin. Infect. Dis. 2019, 68, 1856–1861. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.E.; Shufflebarger, H.L. Late-Developing Infection in Instrumented Idiopathic Scoliosis. Spine 1999, 24, 1909–1912. [Google Scholar] [CrossRef] [PubMed]
- Schofferman, L.; Zucherman, J.; Schofferman, J.; Hsu, K.; Gunthorpe, H.; Picetti, G.; Goldthwaite, N.; White, A. Diptheroids and Associated Infections as a Cause of Failed Instrument Stabilization Procedures in the Lumbar Spine. Spine 1991, 16, 356–358. [Google Scholar] [CrossRef] [PubMed]
- Bémer, P.; Corvec, S.; Tariel, S.; Asseray, N.; Boutoille, D.; Langlois, C.; Tequi, B.; Drugeon, H.; Passuti, N.; Touchais, S. Significance of Propionibacterium Acnes-Positive Samples in Spinal Instrumentation. Spine 2008, 33, E971–E976. [Google Scholar] [CrossRef]
- Shifflett, G.D.; Bjerke-Kroll, B.T.; Nwachukwu, B.U.; Kueper, J.; Burket, J.; Sama, A.A.; Girardi, F.P.; Cammisa, F.P.; Hughes, A.P. Microbiologic Profile of Infections in Presumed Aseptic Revision Spine Surgery. Eur. Spine J. 2016, 25, 3902–3907. [Google Scholar] [CrossRef]
- Bosch-Nicolau, P.; Rodríguez-Pardo, D.; Pigrau, C.; Pellisé, F.; Haddad, S.; Lung, M.; Almirante, B. Acute Spinal Implant Infection Treated with Debridement: Does Extended Antibiotic Treatment Improve the Prognosis? Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 951–958. [Google Scholar] [CrossRef]
- Viola, R.W.; King, H.A.; Adler, S.M.; Wilson, C.B. Delayed Infection after Elective Spinal Instrumentation and Fusion. A Retrospective Analysis of Eight Cases. Spine 1997, 22, 2444–2450, discussion 2450–2451. [Google Scholar] [CrossRef] [PubMed]
- Richards, B.R.; Emara, K.M. Delayed Infections after Posterior TSRH Spinal Instrumentation for Idiopathic Scoliosis: Revisited. Spine 2001, 26, 1990–1996. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.H.-K.; Duong, H.A.; Williams, S.; Lee, J.; Oh, M.; Rosen, C.; Lee, Y.-P.; Bhatia, N. The Efficacy of Bactrim in Reducing Surgical Site Infections after Spine Surgery. N. Am. Spine Soc. J. 2021, 9, 100095. [Google Scholar] [CrossRef] [PubMed]
- Long, D.R.; Bryson-Cahn, C.; Pergamit, R.; Tavolaro, C.; Saigal, R.; Chan, J.D.; Lynch, J.B. 2021 Young Investigator Award Winner: Anatomic Gradients in the Microbiology of Spinal Fusion Surgical Site Infection and Resistance to Surgical Antimicrobial Prophylaxis. Spine 2021, 46, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Triffault-Fillit, C.; Ferry, T.; Laurent, F.; Pradat, P.; Dupieux, C.; Conrad, A.; Becker, A.; Lustig, S.; Fessy, M.H.; Chidiac, C.; et al. Microbiologic Epidemiology Depending on Time to Occurrence of Prosthetic Joint Infection: A Prospective Cohort Study. Clin. Microbiol. Infect. 2019, 25, 353–358. [Google Scholar] [CrossRef]
- Lacasse, M.; Derolez, S.; Bonnet, E.; Amelot, A.; Bouyer, B.; Carlier, R.; Coiffier, G.; Cottier, J.P.; Dinh, A.; Maldonado, I.; et al. 2022 SPILF–Clinical Practice Guidelines for the Diagnosis and Treatment of Disco-Vertebral Infection in Adults. Infect. Dis. Now 2023, 53, 104647. [Google Scholar] [CrossRef]
- CASFM Recommandations 2013–2021. Available online: https://www.sfm-microbiologie.org (accessed on 1 January 2013).
- Eucast: Breakpoint Tables for 2013–2021. Available online: https://www.eucast.org (accessed on 1 January 2013).
| eSSI (n = 46) (%) | lSSI (n = 50) (%) | p Value | |
|---|---|---|---|
| Gender | |||
| Men | 26 (56.5) | 34 (68) | 0.29 |
| Women | 20 (43.5) | 16 (32) | 0.29 |
| Age (median/years) | 50.5 | 51.7 | 0.73 |
| Delay surgery/infection (median/days) | 17.3 | 245.5 | |
| Comorbidities | 27 (58.7) | 21 (42) | 0.66 |
| Spine surgery | 15 (55.6) | 14 (66.7) | 0.55 |
| Immunodeficiency | 4 (14.8) | 4 (19) | 0.72 |
| Diabetes | 7 (25.9) | 2 (9.5) | 0.26 |
| Scoliosis | 6 (22.2) | 7 (33.3) | 0.52 |
| Cerebral palsy | 8 (29.6) | 6 (28.6) | 1 |
| Infection | |||
| Monomicrobial | 27 (58.7) | 33 (66) | 0.46 |
| Polymicrobial | 19 (41.3) | 17 (33) | 0.46 |
| Surgical approach | |||
| ND | 12 (26.1) | 18 (36) | |
| Posterior | 32 (94.1) | 31 (96.9) | 1 |
| Median | 2 (5.9) | 1 (3.1) | 1 |
| Surgical treatment | 41 (97.6) | 45 (95.7) | |
| ND | 4 (8.7) | 3 (6) | |
| DAIR | 32 (78) | 23 (51.1) | <0.001 |
| Hardware removal | 2 (4.9) | 15 (33.3) | <0.001 |
| Hardware replacement | 7 (17.1) | 7 (15.6) | 1 |
| Antibiotic therapy | 42 (91.3) | 48 (96) | 1 |
| Duration (mean/weeks) | 6 | 9 |
| Monomicrobial (n = 33) (%) | Polymicrobial (n = 17) (%) | Total (n = 50) (%) | |
|---|---|---|---|
| Staphylococcus aureus | 8 (24.2) | 9 (52.9) | 17 (34) |
| Cutibacterium acnes | 10 (30.3) | 5 (29.4) | 15 (30) |
| Staphylococcus epidermidis | 5 (15.2) | 5 (29.4) | 10 (20) |
| Escherichia coli | 3 (9.1) | 4 (23.4) | 7 (14) |
| Staphylococcus lugdunensis | 1 (3) | 2 (11.8) | 3 (6) |
| Corynebacterium spp. | - | 3 (17.6) | 3 (6) |
| Proteus mirabilis | 1 (3) | 2 (11.8) | 3 (6) |
| Enterococcus faecalis | 2 (6.1) | 1 (5.9) | 3 (6) |
| Serratia marcescens | 1 (3) | 1 (5.9) | 2 (4) |
| Morganella morganii | - | 2 (11.8) | 2 (4) |
| Streptococcus agalactiae | - | 2 (11.8) | 2 (4) |
| Bacteroides fragilis | - | 2 (11.8) | 2 (4) |
| Enterobacter cloacae | - | 1 (5.9) | 1 (2) |
| Staphylococcus capitis | 1 (3) | - | 1 (2) |
| Cutibacterium avidum | 1 (3) | - | 1 (2) |
| Citrobacter koseri | - | 1 (5.9) | 1 (2) |
| Klebsiella aerogenes | - | 1 (5.9) | 1 (2) |
| Pseudomonas aeruginosa | - | 1 (5.9) | 1 (2) |
| Streptococcus pyogenes | - | 1 (5.9) | 1 (2) |
| Peptoniphilus indolicus | - | 1 (5.9) | 1 (2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reissier, S.; Couzigou, C.; Courseau, R.; Aubert, E.; Le Monnier, A.; Bonnet, E.; Upex, P.; Moreau, P.-E.; Riouallon, G.; Lourtet-Hascoët, J. Microbiological Profile of Instrumented Spinal Infections: 10-Year Study at a French Spine Center. Antibiotics 2024, 13, 791. https://doi.org/10.3390/antibiotics13090791
Reissier S, Couzigou C, Courseau R, Aubert E, Le Monnier A, Bonnet E, Upex P, Moreau P-E, Riouallon G, Lourtet-Hascoët J. Microbiological Profile of Instrumented Spinal Infections: 10-Year Study at a French Spine Center. Antibiotics. 2024; 13(9):791. https://doi.org/10.3390/antibiotics13090791
Chicago/Turabian StyleReissier, Sophie, Carine Couzigou, Romain Courseau, Elise Aubert, Alban Le Monnier, Eric Bonnet, Peter Upex, Pierre-Emmanuel Moreau, Guillaume Riouallon, and Julie Lourtet-Hascoët. 2024. "Microbiological Profile of Instrumented Spinal Infections: 10-Year Study at a French Spine Center" Antibiotics 13, no. 9: 791. https://doi.org/10.3390/antibiotics13090791
APA StyleReissier, S., Couzigou, C., Courseau, R., Aubert, E., Le Monnier, A., Bonnet, E., Upex, P., Moreau, P.-E., Riouallon, G., & Lourtet-Hascoët, J. (2024). Microbiological Profile of Instrumented Spinal Infections: 10-Year Study at a French Spine Center. Antibiotics, 13(9), 791. https://doi.org/10.3390/antibiotics13090791






