Antimicrobial Stewardship: A Correct Management to Reduce Sepsis in NICU Settings
Abstract
1. Introduction
1.1. Use of Antimicrobial Drugs in NICUs, Short-Term and Long-Term Effects
1.2. Antimicrobial Stewardship Programs: Perspectives
2. Materials and Methods
3. Antimicrobial Resistance (AMR) and Multidrug-Resistant Microorganisms (MDROs)
3.1. MDROs in NICUs
3.2. Clostridioides difficile Infections (CDIs)
4. Misuse of Antibiotics and Changes in Neonatal Microbiota
4.1. Comorbidities of Intestinal Dysbiosis and Antibiotic Resistance Genes
4.2. Changes in Newborns’ Microbiota Due to Antibiotic Therapy during Pregnancy
5. Antimicrobial Stewardship
- (1)
- To prevent infections;
- (2)
- To diagnose and treat infections correctly;
- (3)
- To use antimicrobials responsibly;
- (4)
- To prevent the transmission of MDROs [51].
- -
- The identification of newborns who really need antibiotic therapy;
- -
- The knowledge of the microbial epidemiology of the NICU, to initiate the empirical therapy;
- -
- The use of the most “tailored” antimicrobial drug(s) without overlapping antimicrobial activity;
- -
- The use of a correct posology (i.e., the selection of the optimal antimicrobial drug regimen, dose, duration of therapy, and route of administration);
- -
5.1. Main Strategies to Reduce AMR in NICUs
5.1.1. Prescriptive and Pre-Authorization Limitations
5.1.2. Audit and Feedback (A&F) for Prescribers
5.1.3. Guidelines’ Implementation
5.1.4. Training of Healthcare Personnel
5.1.5. Information Technology
5.1.6. Antimicrobial Cycling
5.2. Antimicrobial Stewardship Programs
5.3. Management Schemes for EOS and LOS
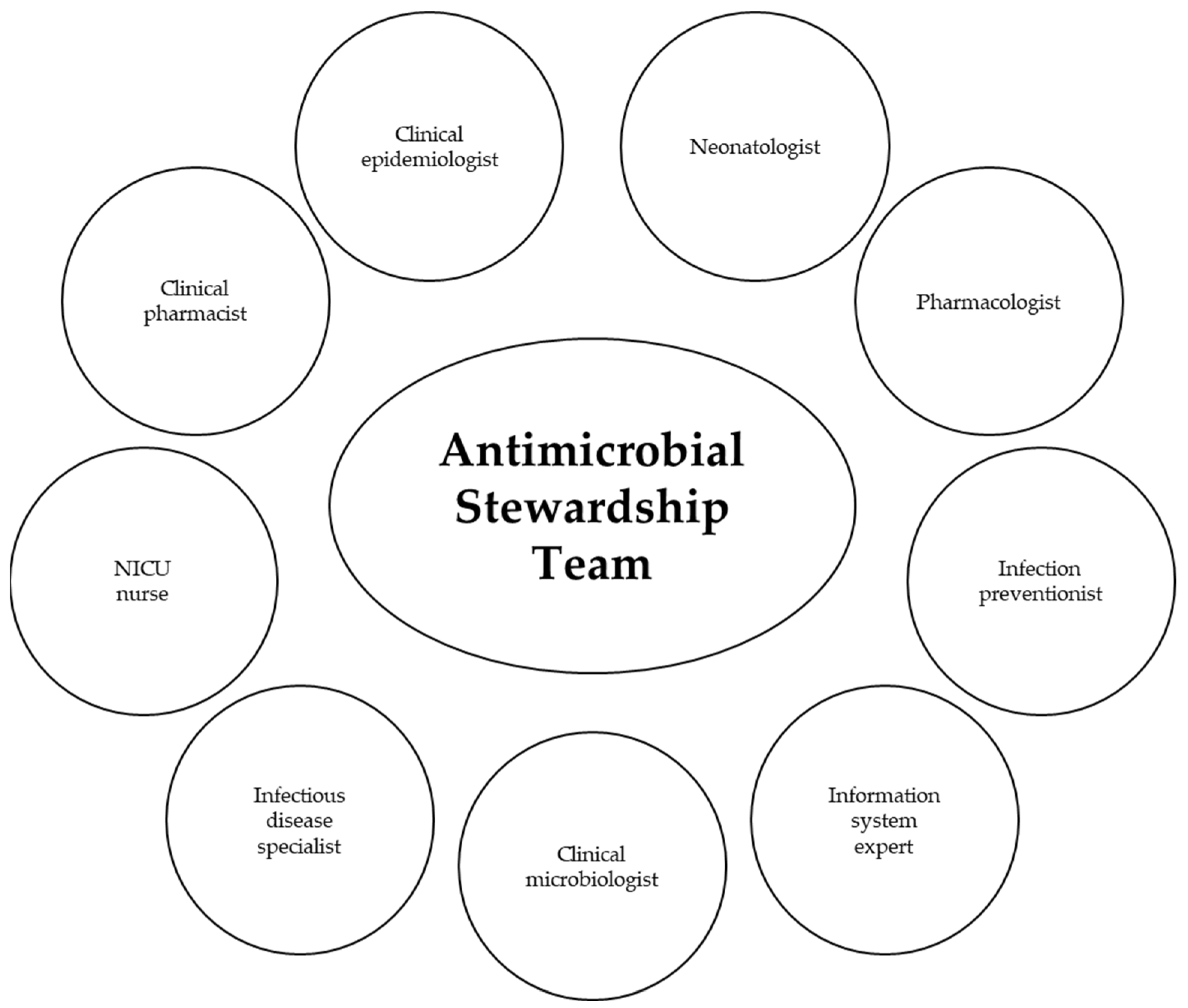
5.4. Antimicrobial Stewardship Team
6. Antimicrobial Stewardship Programs in NICUs around the World
7. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Wang, J.; Zhang, H.; Yan, J.; Zhang, T. Literature review on the distribution characteristics and antimicrobial resistance of bacterial pathogens in neonatal sepsis. J. Matern.-Fetal Neonatal Med. 2022, 35, 861–870. [Google Scholar] [CrossRef] [PubMed]
- Araujo da Silva, A.R.; Marques, A.; Di Biase, C.; Faitanin, M.; Murni, I.; Dramowski, A.; Hübner, J.; Zingg, W. Effectiveness of antimicrobial stewardship programmes in neonatology: A systematic review. Arch. Dis. Child. 2020, 105, 563–568. [Google Scholar] [CrossRef] [PubMed]
- Munita, J.M.; Arias, C.A. Mechanisms of Antibiotic Resistance. Microbiol. Spectr. 2016, 4, 481–511. [Google Scholar] [CrossRef]
- Gal-Mor, O.; Finlay, B.B. Pathogenicity islands: A molecular toolbox for bacterial virulence. Cell Microbiol. 2006, 8, 1707–1719. [Google Scholar] [CrossRef]
- Humphrey, S.; San Millán, Á.; Toll-Riera, M.; Connolly, J.; Flor-Duro, A.; Chen, J.; Ubeda, C.; Craig MacLean, R.; Penadés, J.R. Staphylococcal phages and pathogenicity islands drive plasmid evolution. Nat. Commun. 2021, 12, 5845. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Available online: https://www.ecdc.europa.eu (accessed on 9 January 2024).
- Mukhopadhyay, S. Antibiotic stewardship in neonates and in neonatal intensive care units. Semin. Perinatol. 2020, 44, 151321. [Google Scholar] [CrossRef]
- Klingenberg, C.; Kornelisse, R.F.; Buonocore, G.; Maier, R.F.; Stocker, M. Culture-Negative Early-Onset Neonatal Sepsis—At the Crossroad Between Efficient Sepsis Care and Antimicrobial Stewardship. Front. Pediatr. 2018, 9, 285. [Google Scholar] [CrossRef]
- Gkentzi, D.; Dimitriou, G. Antimicrobial Stewardship in the Neonatal Intensive Care Unit: An Update. Curr. Pediatr. Rev. 2019, 15, 47–52. [Google Scholar] [CrossRef]
- McCarthy, K.N.; Hawke, A.; Dempsey, E.M. Antimicrobial stewardship in the neonatal unit reduces antibiotic exposure. Acta Paediatr. 2018, 107, 1716–1721. [Google Scholar] [CrossRef]
- Newby, B.; Mok, S.H.S.; Sun, Y. Antimicrobial stewardship intervention to reduce unnecessary antibiotic doses in neonates. Am. J. Infect. Control 2021, 49, 126–127. [Google Scholar] [CrossRef]
- Patel, S.J.; Vergnano, S. The impact of paediatric antimicrobial stewardship programmes on patient outcome. Curr. Opin. Infect. Dis. 2018, 31, 216–223. [Google Scholar] [CrossRef]
- Morowitz, M.J.; Katheria, A.C.; Polin, R.A.; Pace, E.; Huang, D.T.; Chang, C.C.H.; Yabes, J.G. The NICU Antibiotics and Outcomes (NANO) trial: A randomized multicenter clinical trial assessing empiric antibiotics and clinical outcomes in newborn preterm infants. Trials 2022, 23, 428. [Google Scholar] [CrossRef]
- Patangia, D.V.; Ryan, C.A.; Dempsey, E.; Ross, R.P.; Stanton, C. Impact of antibiotics on the human microbiome and consequences for host health. Microbiologyopen 2022, 11, e1260. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, R.G.; Chowdhury, D.; Hansen, N.I.; Smith, P.B.; Stoll, B.J.; Sánchez, P.J.; Das, A.; Puopolo, K.M.; Mukhopadhyay, S.; Higgins, R.D.; et al. Prolonged Duration of Early Antibiotic Therapy in Extremely Premature Infants. Pediatr. Res. 2019, 85, 994–1000. [Google Scholar] [CrossRef]
- Patel, S.J.; Saiman, L. Principles and Strategies of Antimicrobial Stewardship in the Neonatal Intensive Care Unit. Semin. Perinatol. 2012, 36, 431–436. [Google Scholar] [CrossRef]
- Septimus, E.J. Antimicrobial Resistance: An Antimicrobial/Diagnostic Stewardship and Infection Prevention Approach. Med. Clin. N. Am. 2018, 102, 819–829. [Google Scholar] [CrossRef]
- Rice, L.B. Antimicrobial Stewardship and Antimicrobial Resistance. Med. Clin. N. Am. 2018, 102, 805–818. [Google Scholar] [CrossRef]
- Cipolla, D.; Giuffrè, M.; Mammina, C.; Corsello, G. Prevention of nosocomial infections and surveillance of emerging resistances in NICU. J. Matern.-Fetal Neonatal Med. 2011, 24 (Suppl. S1), 23–26. [Google Scholar] [CrossRef]
- Nathwani, D.; Varghese, D.; Stephens, J.; Ansari, W.; Martin, S.; Charbonneau, C. Value of hospital antimicrobial stewardship programs [ASPs]: A systematic review. Antimicrob. Resist. Infect. Control 2019, 8, 35. [Google Scholar] [CrossRef]
- Bueno E Silva, A.C.; Márcia Anchieta, L.; Rosado, V.; Ferreira, J.; Trindade Clemente, W.; Sampaio Coelho, J.; Orlandi Mourăo, P.H.; Maia de Castro Romanelli, R. Antimicrobial use for treatment of healthcare-associated infections and bacterial resistance in a reference neonatal unit. J. Pediatr. 2021, 97, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, C.B.; Cantey, J.B. Antibiotic Resistance in the Neonatal Intensive Care Unit. Neoreviews 2019, 20, e135–e144. [Google Scholar] [CrossRef]
- Ting, J.Y.; Shah, P.S. Antibiotic stewardship in neonates: Challenges and opportunities. Transl. Pediatr. 2020, 9, 198–201. [Google Scholar] [CrossRef]
- Pinheiro, F.R.; Rozza-de-Menezes, R.E.; Blum, M.C.; Alves Pereira, R.F.; Rocha, J.A.; Guedes Pinto, M.C.F.; Penna, B.A.; Riley, L.W.; Aguiar-Alves, F. Evaluation of changes in antimicrobial susceptibility in bacteria infecting children and their mothers in pediatric, neonatal-intensive care unit, and gynecology/obstetrics wards of a quaternary referral hospital during the COVID-19 pandemic. Front. Microbiol. 2023, 14, 1096223. [Google Scholar] [CrossRef]
- Thoma, R.; Seneghini, M.; Seiffert, S.N.; Vuichard Gysin, D.; Scanferla, G.; Haller, S.; Flury, D.; Boggian, K.; Kleger, G.R.; Filipovic, M.; et al. The challenge of preventing and containing outbreaks of multidrug-resistant organisms and Candida auris during the coronavirus disease 2019 pandemic: Report of a carbapenem-resistant Acinetobacter baumannii outbreak and a systematic review of the literature. Antimicrob. Resist. Infect. Control 2022, 21, 12. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Antibiotic Resistance Threats in the United States. 2019. Available online: https://www.cdc.gov/DrugResistance/Biggest-Threats.html (accessed on 9 January 2024).
- Cunha, C.B. Antimicrobial Stewardship Programs: Principles and Practice. Med. Clin. N. Am. 2018, 102, 797–803. [Google Scholar] [CrossRef]
- Saeed, N.K.; Al-Beltagi, M.; Bediwy, A.S.; El-Sawaf, Y.; Toema, O. Gut microbiota in various childhood disorders: Implication and indications. World J. Gastroenterol. 2022, 28, 1875–1901. [Google Scholar] [CrossRef]
- Groer, M.W.; Morgan, K.H.; Louis-Jacques, A.; Miller, E.M. A scoping review of research on the human milk microbiome. J. Hum. Lact. 2020, 36, 628–643. [Google Scholar] [CrossRef]
- Notarbartolo, V.; Giuffrè, M.; Montante, C.; Corsello, G.; Carta, M. Composition of Human Breast Milk Microbiota and Its Role in Children’s Health. Pediatr. Gastroenterol. Hepatol. Nutr. 2022, 25, 194–210. [Google Scholar] [CrossRef]
- Renz, H.; Skevaki, C. Early life microbial exposures and allergy risks: Opportunities for prevention. Nat. Rev. Immunol. 2021, 21, 177–191. [Google Scholar] [CrossRef]
- Notarbartolo, V.; Carta, M.; Accomando, S.; Giuffrè, M. The First 1000 Days of Life: How Changes in the Microbiota Can Influence Food Allergy Onset in Children. Nutrients 2023, 15, 4014. [Google Scholar] [CrossRef]
- McPherson, C.; Liviskie, C.; Zeller, B.; Nelson, M.P.; Newland, J.G. Antimicrobial Stewardship in Neonates: Challenges and Opportunities. Neonatal Netw. 2018, 37, 116–123. [Google Scholar] [CrossRef]
- Reyman, M.; van Houten, M.A.; Watson, R.L.; Chu, M.L.J.N.; Arp, K.; de Waal, W.J.; Schiering, I.; Plötz, F.B.; Willems, R.J.L.; van Schaik, W.; et al. Effects of early-life antibiotics on the developing infant gut microbiome and resistome: A randomized trial. Nat. Commun. 2022, 13, 893. [Google Scholar] [CrossRef]
- Ramasethu, J.; Kawakita, T. Antibiotic stewardship in perinatal and neonatal care. Semin. Fetal Neonatal Med. 2017, 22, 278–283. [Google Scholar] [CrossRef]
- Dyar, O.J.; Huttner, B.; Schouten, J.; Pulcini, C.; ESGAP (ESCMID Study Group for Antimicrobial Stewardship). What is antimicrobial stewardship? Clin. Microbiol. Infect. 2017, 23, 793–798. [Google Scholar] [CrossRef]
- Puopolo, K.M.; Lynfield, R.; Cummings, J.J.; Committee on Fetus and Newborn; Committee on Infectious Diseases. Management of Infants at Risk for Group B Streptococcal Disease. Pediatrics 2019, 144, e20191881. [Google Scholar] [CrossRef]
- Pan, X.; Zhou, Z.; Liu, B.; Wu, Z. A novel therapeutic concern: Antibiotic resistance genes in common chronic diseases. Front. Microbiol. 2022, 13, 1037389. [Google Scholar] [CrossRef]
- Carvalho, M.J.; Sands, K.; Thomson, K.; Portal, E.; Mathias, J.; Milton, R.; Gillespie, D.; Dyer, C.; Akpulu, C.; Boostrom, I.; et al. Antibiotic resistance genes in the gut microbiota of mothers and linked neonates with or without sepsis from low- and middle-income countries. Nat. Microbiol. 2022, 7, 1337–1347. [Google Scholar] [CrossRef]
- Zou, Z.H.; Liu, D.; Li, H.D.; Zhu, D.P.; He, Y.; Hou, T.; Yu, J.L. Prenatal and postnatal antibiotic exposure influences the gut microbiota of preterm infants in neonatal intensive care units. Ann. Clin. Microbiol. Antimicrob. 2018, 17, 9. [Google Scholar] [CrossRef]
- Nogacka, A.; Salazar, N.; Suárez, M.; Milani, C.; Arboleya, S.; Solís, G.; Fernández, N.; Alaez, L.; Hernández-Barranco, A.M.; de Los Reyes-Gavilán, C.G.; et al. Impact of intrapartum antimicrobial prophylaxis upon the intestinal microbiota and the prevalence of antibiotic resistance genes in vaginally delivered full-term neonates. Microbiome 2017, 5, 93. [Google Scholar] [CrossRef]
- Kenyon, S.; Boulvain, M.; Neilson, J.P. Antibiotic for preterm rupture of membranes. Cochrane Database Syst. Rev. 2013, 2, CD001058. [Google Scholar] [CrossRef]
- Vuillermin, P.J.; O’Hely, M.; Collier, F.; Allen, K.J.; Tang, M.L.K.; Harrison, L.C.; Carlin, J.B.; Saffery, R.; Ranganathan, S.; Sly, P.D.; et al. Maternal carriage of Prevotella during pregnancy associates with protection against food allergy in the offspring. Nat. Commun. 2020, 11, 1452. [Google Scholar] [CrossRef]
- Gao, Y.; Nanan, R.; Macia, L.; Tan, J.; Sominsky, L.; Quinn, T.P.; O’Hely, M.; Ponsonby, A.; Tang, M.L.K.; Collier, F.; et al. The maternal gut microbiome during pregnancy and offspring allergy and asthma. J. Allergy Clin. Immunol. 2021, 148, 669–678. [Google Scholar] [CrossRef]
- Wang, S.; Zhang, R.; Li, X.; Gao, Y.; Dai, N.; We, Y.; Liu, L.; Xing, Y.; Li, Z. Relationship between maternal-infant gut microbiota and infant food allergy. Front. Microbiol. 2022, 13, 933152. [Google Scholar] [CrossRef]
- Hirsch, A.G.; Pollak, J.; Glass, T.A.; Poulsen, M.N.; Bailey-Davis, L.; Mowery, J.; Schwartz, B.S. Early Life Antibiotic Use and Subsequent Diagnosis of Food Allergy and Allergic Diseases. Clin. Exp. Allergy 2017, 47, 236–244. [Google Scholar] [CrossRef]
- Miller, K.A.; Vicentini, F.A.; Hirota, S.A.; Sharkey, K.A.; Wieser, M.E. Antibiotic treatment affects the expression levels of copper transporters and the isotopic composition of copper in the colon of mice. Proc. Natl. Acad. Sci. USA 2019, 116, 5955–5960. [Google Scholar] [CrossRef]
- Ríos-Covián, D.; Ruas-Madiedo, P.; Margolles, A.; Gueimonde, M.; de Los Reyes-Gavilán, C.G.; Salazar, N. Intestinal Short Chain Fatty Acids and their Link with Diet and Human health. Front. Microbiol. 2016, 7, 185. [Google Scholar] [CrossRef]
- Barlam, T.F.; Cosgrove, S.E.; Abbo, L.M.; MacDougall, C.; Schuetz, A.N.; Septimus, E.J.; Srinivasan, A.; Dellit, T.H.; Falck-Ytter, Y.T.; Fishman, N.O.; et al. Implementing an Antibiotic Stewardship Program: Guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin. Infect. Dis. 2016, 62, e51–e77. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). The Core Elements of Hospital Antibiotic Stewardship Programs. 2019. Available online: https://www.cdc.gov/antibiotic-use/core-elements/hospital.html (accessed on 9 January 2024).
- Hyun, D.Y.; Hersh, A.L.; Namtu, K.; Palazzi, D.L.; Maples, H.D.; Newland, J.G.; Saiman, L. Antimicrobial stewardship in pediatrics: How every pediatrician can be a steward. JAMA Pediatr. 2013, 167, 859–866. [Google Scholar] [CrossRef]
- Nzegwu, N.; Rychalsky, M.R.; Nallu, L.A.; Song, X.; Deng, Y.; Natusch, A.M.; Baltimore, R.S.; Paci, G.R.; Bizzarro, M.J. Implementation of an Antimicrobial Stewardship Program in a Neonatal Intensive Care Unit. Infect. Control Hosp. Epidemiol. 2017, 38, 1137–1143. [Google Scholar] [CrossRef]
- Qureshi, N.; Kroger, J.; Zangwill, K.M.; Joshi, N.S.; Payton, K.; Mendel, P. Changes in perceptions of antibiotic stewardship among neonatal intensive care unit providers over the course of a learning collaborative: A prospective, multisite, mixed-methods evaluation. J. Perinatol. 2024, 44, 62–70. [Google Scholar] [CrossRef]
- Laplante, K.; Cunha, C.; Morrill, H.; Rice, L.; Mylonakis, E. Antimicrobial Stewardship: Principles and Practice; CAB® International: Wallingford, UK, 2017; pp. 8–12. [Google Scholar]
- Berardi, A.; Ficara, M.; Pietrella, E.; Boncompagni, A.; Toffoli, C.; Bianchini, A.; Della Casa, E.; Spada, C.; Spaggiari, E.; Ciccia, M.; et al. Stewardship antimicrobica nel neonato e nel piccolo lattante. Med. Bambino 2017, 8, 493–501. [Google Scholar]
- Brindle, M.E.; McDiarmid, C.; Short, K.; Miller, K.; MacRobie, A.; Lam, J.Y.K.; Brockel, M.; Raval, M.V.; Howlett, A.; Lee, K.S.; et al. Consensus Guidelines for Perioperative Care in Neonatal Intestinal Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J. Surg. 2020, 44, 2482–2492. [Google Scholar] [CrossRef]
- Bratzler, D.W.; Dellinger, E.P.; Olsen, K.M.; Perl, T.M.; Auwaerter, P.G.; Bolon, M.K.; Fish, D.N.; Napolitano, L.M.; Sawyer, R.G.; Slain, D.; et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg. Infect. 2013, 14, 73–156. [Google Scholar] [CrossRef]
- Viel-Thériault, I.; Agarwal, A.; Bariciak, E.; Le Saux, N.; Thampi, N. Antimicrobial Prophylaxis Use in the Neonatal Intensive Care Unit: An Antimicrobial Stewardship Target That Deserves Attention! Am. J. Perinatol. 2022, 39, 1288–1291. [Google Scholar] [CrossRef]
- Antimicrobial Stewardship: Systems and Processes for Effective Antimicrobial Medicine Use. 2019. Available online: https://www.nice.org.uk/guidance/ng15 (accessed on 9 January 2024).
- Cantey, J.B. Optimizing the Use of Antibacterial Agents in the Neonatal Period. Paediatr. Drugs 2016, 18, 109–122. [Google Scholar] [CrossRef]
- National Centre for Antimicrobial Stewardship. Available online: https://www.ncas-australia.org (accessed on 12 February 2024).
- Balkhy, H.H.; El-Saed, A.; Alshehri, A.; Alshaalan, M.; Hijazi, O.; El-Metwally, A.; Aljohany, S.M.; Al Saif, S. Antimicrobial consumption in three pediatric and neonatal intensive care units in Saudi Arabia: 33-month surveillance study. Ann. Clin. Microbiol. Antimicrob. 2019, 18, 20. [Google Scholar] [CrossRef]
- Rub, D.M.; Dhudasia, M.B.; Healy, T.; Mukhopadhyay, S. Role of microbiological tests and biomarkers in antibiotic stewardship. Semin. Perinatol. 2020, 44, 151328. [Google Scholar] [CrossRef]
- Dukhovny, D.; Buus-Frank, M.E.; Edwards, E.M.; Ho, T.; Morrow, K.A.; Srinivasan, A.; Pollock, D.A.; Zupancic, J.A.F.; Pursley, D.M.; Goldmann, D.; et al. A Collaborative Multicenter QI Initiative to Improve Antibiotic Stewardship in Newborns. Pediatrics 2019, 144, e20190589. [Google Scholar] [CrossRef]
- Beltrami Doltrario, A.; Gambero Gaspar, G.; Queiroz Ungari, A.; Martinez, R.; Pazin Filho, A.; Maciel, B.C.; Bellissimo-Rodrigues, F.; de Carvalho Santana, R. Assesment of preauthorization and 24-hour expert consultation as a restrictive antimicrobial stewardship bundle in a Brazilian tertiary-care hospital: An interrupted time series analysis. Infect. Prev. Pract. 2022, 4, 100201. [Google Scholar] [CrossRef] [PubMed]
- Good Practice Recommendations for Hospital Antimicrobial Stewardship in NHS Scotland. Available online: https://www.sapg.scot/guidance-qi-tools/ (accessed on 9 January 2024).
- Schwartz, K.L.; Xu, A.X.T.; Alderson, S.; Bjerrum, L.; Behaut, J.; Brown, B.C.; Bucher, H.C.; De Sutter, A.; Francis, N.; Grimshaw, J.; et al. Best practice guidance for antibiotic audit and feedback interventions in primary care: A modified Delphi study from the Joint Programming Initiative on Antimicrobial resistance: Primary Care Antibiotic Audit and Feedback Network (JPIAMR-PAAN). Antimicrob. Resist. Infect. Control 2023, 12, 72. [Google Scholar] [CrossRef]
- Lu, C.; Liu, Q.; Yuan, H.; Wang, L. Implementation of the smart use of antibiotics program to reduce unnecessary antibiotic use in a neonatal ICU: A prospective interrupted timeseries study in a developing country. Crit. Care Med. 2019, 47, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Trotter, N.E.; Slight, S.P.; Karimi, R.; Bates, D.W.; Sheikh, A.; Weir, C.; Tolley, C.L. The effect of digital antimicrobial stewardship programmes on antimicrobial usage, length of stay, mortality and cost. Inform. Med. Unlocked 2023, 37, 101183. [Google Scholar] [CrossRef]
- Kim, J.Y.; Sohn, J.W.; Park, D.W.; Yoon, Y.K.; Kim, Y.M.; Kim, M.J. Control of extended-spectrum {beta}-lactamase-producing Klebsiella pneumoniae using a computer-assisted management program to restrict third-generation cephalosporin use. J. Antimicrob. Chemother. 2008, 62, 416–421. [Google Scholar] [CrossRef] [PubMed]
- Bond, S.E.; Chubaty, A.J.; Adhikari, S.; Miyakis, S.; Boutlis, C.S.; Yeo, W.W.; Konecny, P. Outcomes of multisite antimicrobial stewardship programme implementation with a shared clinical decision support system. J. Antimicrob. Chemother. 2017, 72, 2110–2118. [Google Scholar] [CrossRef] [PubMed]
- Kesselheim, A.S.; Cresswell, K.; Phansalkar, S.; Bates, D.W.; Sheikh, A. Clinical decision support systems could be modified to reduce ‘alert fatigue’while still minimizing the risk of litigation. Health Aff. 2011, 30, 2310–2317. [Google Scholar] [CrossRef]
- Bremmer, D.N.; Trienski, T.L.; Walsh, T.L.; Moffa, M.A. Role of Technology in Antimicrobial Stewardship. Med. Clin. N. Am. 2018, 102, 955–963. [Google Scholar] [CrossRef] [PubMed]
- Mustafa, Z.U.; Hayat Khan, A.; Salman, M.; Syed Sulaiman, S.A.; Godman, B. Antimicrobial Utilization among Neonates and Children: A Multicenter Point Prevalence Study from Leading Children’s Hospitals in Punjab, Pakistan. Antibiotics 2022, 11, 1056. [Google Scholar] [CrossRef] [PubMed]
- Tzialla, C.; Pedicino, R.; Stolfi, I. Manuale di Infettivologia Neonatale, 3rd ed.; Antonio Delfino Editore: Rome, Italy, 2022; pp. 23–34. [Google Scholar]
- Molloy, J.; Allen, K.; Collier, F.; Tang, M.L.K.; Ward, A.C.; Vuillermin, P. The potential link between gut microbiota and IgE mediated food allergy in early life. Int. J. Environ. Res. Public Health 2013, 10, 7235–7256. [Google Scholar] [CrossRef] [PubMed]
- Chatzopoulou, M.; Reynolds, L. Systematic review of the effects of antimicrobial cycling on bacterial resistance rates within hospital settings. Br. J. Clin. Pharmacol. 2022, 88, 897–910. [Google Scholar] [CrossRef]
- Bueno Silva, A.C.; Anchieta, L.M.; Fischer de Paula Lopes, M.; Maia de Castro Romanelli, R. Inadequate use of antibiotics and increase in neonatal sepsis caused by resistant bacteria related to health care assistance: A systematic review. Braz. J. Infect. Dis. 2018, 22, 328–337. [Google Scholar] [CrossRef]
- Cantey, J.B.; Wozniak, P.S.; Pruszynski, J.E.; Sánchez, P.J. Reducing unnecessary antibiotic use in the neonatal intensive care unit (SCOUT): A prospective interrupted time-series study. Lancet Infect. Dis. 2016, 16, 1178–1184. [Google Scholar] [CrossRef]
- Rajar, P.; Saugstad, O.D.; Berild, D.; Dutta, A.; Greisen, G.; Lausten-Thomsen, U.; Mande, S.S.; Nangia, S.; Petersen, F.C.; Dahle, U.R.; et al. Antibiotic Stewardship in Premature Infants: A Systematic Review. Neonatology 2020, 117, 673–686. [Google Scholar] [CrossRef]
- Zingg, W.; Pfister, R.; Posfay-Barbe, K.M.; Huttner, B.; Touveneau, S.; Pittet, D. Secular trends in antibiotic use among neonates: 2001–2008. Pediatr. Infect. Dis. J. 2011, 30, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, J.A.; Pontefract, S.K.; Cresswell, K.; Williams, R.; Sheikh, A.; Coleman, J.J. Antimicrobial stewardship using electronic prescribing systems in hospital settings: A scoping review of interventions and outcome measures. JAC Antimicrob. Resist. 2022, 4, diac063. [Google Scholar] [CrossRef]
- Cantey, J.B.; Baird, S.D. Ending the Culture of Culture-Negative Sepsis in the Neonatal ICU. Pediatrics 2017, 140, e20170044. [Google Scholar] [CrossRef]
- Howard, A.K.; Parbuoni, K.A.; Claeys, K.; Biggs, J.M.; Seung, H.; Johnson, K.; Campbell, J.; Morgan, J.A. Validation of neonatal and paediatric antimicrobial stewardship treatment algorithms in rapid diagnostic-detected bacteraemia. Int. J. Pharm. Pract. 2021, 29, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Kaiser Permanente Research. Available online: https://neonatalsepsiscalculator.kaiserpermanente.org (accessed on 9 January 2024).
- Puopolo, K.M.; Draper, D.; Wi, S.; Newman, T.B.; Zupancic, J.; Lieberman, E.; Smith, M.; Escobar, G.J. Estimating the Probability of Neonatal Early-Onset Infection on the Basis of Maternal Risk Factors. Pediatrics 2011, 128, e1155–e1163. [Google Scholar] [CrossRef]
- Rosa-Fraile, M.; Spellerberg, B. Reliable Detection of Group B Streptococcus in the Clinical Laboratory. J. Clin. Microbiol. 2017, 55, 2590–2598. [Google Scholar] [CrossRef]
- Redefining the Antibiotic Stewardship Team: Recommendations from the American Nurses Association/Centers for Disease Control and Prevention Workgroup on the Role of Registered Nurses in Hospital Antibiotic Stewardship Practices. JAC Antimicrob. Resist. 2019, 1, dlz037. [CrossRef]
- Villanueva, P.; Freyne, B.; Hockey, L.; Carr, J.; Bryant, P.A. Impact of an antimicrobial stewardship intervention in neonatal intensive care: Recommendations and implementation. J. Paediatr. Child Health 2021, 57, 1208–1214. [Google Scholar] [CrossRef]
- Ho, T.; Buus-Frank, M.E.; Edwards, E.M.; Morrow, K.A.; Ferrelli, K.; Srinivasan, A.; Pollock, D.A.; Dukhovny, D.; Zupancic, J.A.F.; Pursley, D.M.; et al. Adherence of Newborn-Specific Antibiotic Stewardship Programs to CDC Recommendations. Pediatrics 2018, 142, e20174322. [Google Scholar] [CrossRef] [PubMed]
- Kitano, T.; Takagi, K.; Arai, I.; Yasuhara, H.; Ebisu, R.; Ohgitani, A.; Kitagawa, D.; Oka, M.; Masuo, K.; Minowa, H. A simple and feasible antimicrobial stewardship program in a neonatal intensive care unit of a Japanese community hospital. J. Infect. Chemother. 2019, 25, 860–865. [Google Scholar] [CrossRef] [PubMed]
- Ting, J.Y.; Roberts, A.; Tilley, P.; Robinson, J.L.; Dunn, M.S.; Paquette, V.; Lee, K.S.; Shah, V.; Yoon, E.; Richter, L.L.; et al. Development of a national neonatal intensive care unit-specific antimicrobial stewardship programme in Canada: Protocol for a cohort study. BMJ Open 2020, 10, e043403. [Google Scholar] [CrossRef] [PubMed]
- Maalouf, F.; Saad, T.; Zakhour, R.; Yunis, K. Successful establishment and five-year sustainability of a neonatal-specific antimicrobial stewardship program in a low middle-income country. Front. Pharmacol. 2022, 13, 1076392. [Google Scholar] [CrossRef] [PubMed]
| Diagnosis of Neonatal Sepsis | |
| Choice of Empirical Antimicrobial Treatment |
|
| Re-evaluation of treatment already underway |
|
| Measurement of blood levels of antimicrobial drugs | |
| Perioperative prophylaxis | |
| Continuous monitoring of the use of antimicrobial drugs with performance indicators |
|
| Clear documentation of baseline data and dedicated guidelines within a specific AMS group |
|
| Application of appropriate A&F mechanisms |
|
| Avoidance of prolonged empirical antibiotic therapy with automatic discontinuation when clinical and biochemical conditions allow it |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Notarbartolo, V.; Badiane, B.A.; Insinga, V.; Giuffrè, M. Antimicrobial Stewardship: A Correct Management to Reduce Sepsis in NICU Settings. Antibiotics 2024, 13, 520. https://doi.org/10.3390/antibiotics13060520
Notarbartolo V, Badiane BA, Insinga V, Giuffrè M. Antimicrobial Stewardship: A Correct Management to Reduce Sepsis in NICU Settings. Antibiotics. 2024; 13(6):520. https://doi.org/10.3390/antibiotics13060520
Chicago/Turabian StyleNotarbartolo, Veronica, Bintu Ayla Badiane, Vincenzo Insinga, and Mario Giuffrè. 2024. "Antimicrobial Stewardship: A Correct Management to Reduce Sepsis in NICU Settings" Antibiotics 13, no. 6: 520. https://doi.org/10.3390/antibiotics13060520
APA StyleNotarbartolo, V., Badiane, B. A., Insinga, V., & Giuffrè, M. (2024). Antimicrobial Stewardship: A Correct Management to Reduce Sepsis in NICU Settings. Antibiotics, 13(6), 520. https://doi.org/10.3390/antibiotics13060520






