The Interplay between Antibiotics and the Host Immune Response in Sepsis: From Basic Mechanisms to Clinical Considerations: A Comprehensive Narrative Review
Abstract
1. Introduction
- -
- For the section on mechanisms of action, terms such as ‘immune dysfunction’ and ‘sepsis pathophysiology’ were paired with each class of antibiotics, with exclusion criteria for papers related to clinical research, inflammatory/rheumatic diseases, cystic fibrosis, and chronic respiratory diseases.
- -
- In the microbiome section, terms such as “antibiotics”, “immunomodulation/dysfunction”, “microbiota or microbiome”, and “sepsis” were utilized.
- -
- Regarding the clinical studies section, the search terms included “antibiotics”, “immunomodulation/dysfunction”, and “clinical research”, with exclusion criteria for studies involving animals and in-vitro and ex-vivo methodologies. However, for each search, temporal criteria were restricted to the last 25 years of publications, from 1999 onwards.
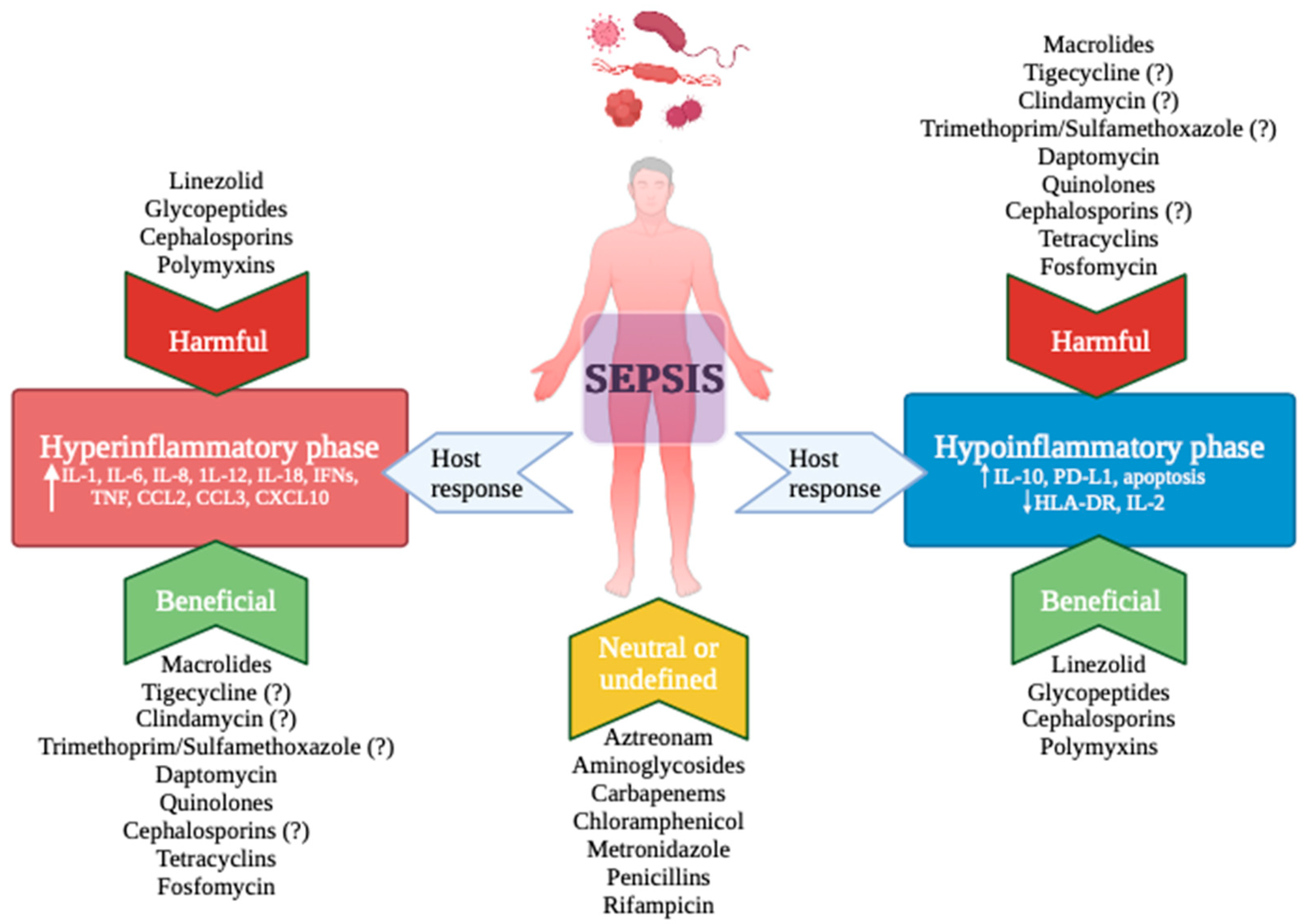
2. Antibiotics and Immune Response: Mechanisms of Action
2.1. Regulation of Pro-Inflammatory Cytokines Production
2.2. Modulation of Toll-like Receptors (TLRs) and Regulation of P38/Pmk-1 Pathway
2.3. Inhibition of Matrix Metalloproteinases (MMPs) and Blockade of Nitric Oxide (NO) Synthase
2.4. Regulation of Apoptosis Induced by Caspases
3. Antibiotics and Sepsis Impact on Microbiome Disruption
3.1. Animal Studies
3.2. Human Studies
4. Clinical Studies on Antibiotics and Immunity
4.1. Community-Acquired Pneumonia (CAP) and Ventilator-Associated Pneumonia (VAP)
4.2. Sepsis, Septic Shock, and ARDS
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Rudd, K.E.; Johnson, S.C.; Agesa, K.M.; Shackelford, K.A.; Tsoi, D.; Kievlan, D.R.; Colombara, D.V.; Ikuta, K.S.; Kissoon, N.; Finfer, S.; et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet 2020, 395, 200–211. [Google Scholar] [CrossRef]
- Vincent, J.-L.; Jones, G.; David, S.; Olariu, E.; Cadwell, K.K. Frequency and mortality of septic shock in Europe and North America: A systematic review and meta-analysis. Crit. Care 2019, 23, 196. [Google Scholar] [CrossRef]
- Santacroce, E.; D’angerio, M.; Ciobanu, A.L.; Masini, L.; Tartaro, D.L.; Coloretti, I.; Busani, S.; Rubio, I.; Meschiari, M.; Franceschini, E.; et al. Advances and Challenges in Sepsis Management: Modern Tools and Future Directions. Cells 2024, 13, 439. [Google Scholar] [CrossRef] [PubMed]
- Hotchkiss, R.S.; Monneret, G.; Payen, D. Immunosuppression in sepsis: A novel understanding of the disorder and a new therapeutic approach. Lancet Infect. Dis. 2013, 13, 260–268. [Google Scholar] [CrossRef]
- Busani, S.; Roat, E.; Tosi, M.; Biagioni, E.; Coloretti, I.; Meschiari, M.; Gelmini, R.; Brugioni, L.; De Biasi, S.; Girardis, M. Adjunctive Immunotherapy with Polyclonal Ig-M Enriched Immunoglobulins for Septic Shock: From Bench to Bedside. The Rationale for a Personalized Treatment Protocol. Front. Med. 2021, 8, 616511. [Google Scholar] [CrossRef]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; Mcintyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Crit. Care Med. 2021, 49, e1063. [Google Scholar] [CrossRef]
- Culić, O.; Eraković, V.; Parnham, M.J. Anti-inflammatory effects of macrolide antibiotics. Eur. J. Pharmacol. 2001, 429, 209–229. [Google Scholar] [CrossRef] [PubMed]
- Giamarellos-Bourboulis, E.J.; Baziaka, F.; Antonopoulou, A.; Koutoukas, P.; Kousoulas, V.; Sabracos, L.; Panagou, C.; Perrea, D.; Giamarellou, H. Clarithromycin co-administered with amikacin attenuates systemic inflammation in experimental sepsis with Escherichia coli. Int. J. Antimicrob. Agents 2005, 25, 168–172. [Google Scholar] [CrossRef]
- Giamarellos-Bourboulis, E.J.; Tziortzioti, V.; Koutoukas, P.; Baziaka, F.; Raftogiannis, M.; Antonopoulou, A.; Adamis, T.; Sabracos, L.; Giamarellou, H. Clarithromycin is an effective immunomodulator in experimental pyelonephritis caused by pan-resistant Klebsiella pneumoniae. J. Antimicrob. Chemother. 2006, 57, 937–944. [Google Scholar] [CrossRef]
- Kikuchi, T.; Hagiwara, K.; Honda, Y.; Gomi, K.; Kobayashi, T.; Takahashi, H.; Tokue, Y.; Watanabe, A.; Nukiwa, T. Clarithromycin suppresses lipopolysaccharide-induced interleukin-8 production by human monocytes through AP-1 and NF-kappa B transcription factors. J. Antimicrob. Chemother. 2002, 49, 745–755. [Google Scholar] [CrossRef]
- Tkalčević, V.I.; Bošnjak, B.; Hrvačić, B.; Bosnar, M.; Marjanović, N.; Ferenčić, Ž.; Šitum, K.; Čulić, O.; Parnham, M.J.; Eraković, V. Anti-inflammatory activity of azithromycin attenuates the effects of lipopolysaccharide administration in mice. Eur. J. Pharmacol. 2006, 539, 131–138. [Google Scholar] [CrossRef]
- Lin, S.-J.; Kuo, M.-L.; Hsiao, H.-S.; Lee, P.-T. Azithromycin modulates immune response of human monocyte-derived dendritic cells and CD4+ T cells. Int. Immunopharmacol. 2016, 40, 318–326. [Google Scholar] [CrossRef]
- Dey, S.; Majhi, A.; Mahanti, S.; Dey, I.; Bishayi, B. In Vitro Anti-inflammatory and Immunomodulatory Effects of Ciprofloxacin or Azithromycin in Staphylococcus aureus-Stimulated Murine Macrophages are Beneficial in the Presence of Cytochalasin D. Inflammation 2015, 38, 1050–1069. [Google Scholar] [CrossRef]
- Kushiya, K.; Nakagawa, S.; Taneike, I.; Iwakura, N.; Yamamoto, T.; Tsukada, H.; Gejyo, F.; Imanishi, K.; Uchiyama, T. Inhibitory effect of antimicrobial agents and anisodamine on the staphylococcal superantigenic toxin-induced overproduction of proinflammatory cytokines by human peripheral blood mononuclear cells. J. Infect. Chemother. Off. J. Jpn. Soc. Chemother. 2005, 11, 192–195. [Google Scholar] [CrossRef]
- Pichereau, S.; Moran, J.J.M.; Hayney, M.S.; Shukla, S.K.; Sakoulas, G.; Rose, W.E. Concentration-dependent effects of antimicrobials on Staphylococcus aureus toxin-mediated cytokine production from peripheral blood mononuclear cells. J. Antimicrob. Chemother. 2012, 67, 123–129. [Google Scholar] [CrossRef]
- Kelesidis, T. The Interplay between Daptomycin and the Immune System. Front. Immunol. 2014, 5, 52. [Google Scholar] [CrossRef]
- Tirilomis, T. Daptomycin and Its Immunomodulatory Effect: Consequences for Antibiotic Treatment of Methicillin-Resistant Staphylococcus aureus Wound Infections after Heart Surgery. Front. Immunol. 2014, 5, 97. [Google Scholar] [CrossRef]
- Weiss, T.; Shalit, I.; Blau, H.; Werber, S.; Halperin, D.; Levitov, A.; Fabian, I. Anti-inflammatory effects of moxifloxacin on activated human monocytic cells: Inhibition of NF-kappaB and mitogen-activated protein kinase activation and of synthesis of proinflammatory cytokines. Antimicrob. Agents Chemother. 2004, 48, 1974–1982. [Google Scholar] [CrossRef]
- Williams, A.C.; Galley, H.F.; Watt, A.M.; Webster, N.R. Differential effects of three antibiotics on T helper cell cytokine expression. J. Antimicrob. Chemother. 2005, 56, 502–506. [Google Scholar] [CrossRef]
- Ziegeler, S.; Raddatz, A.; Hoff, G.; Buchinger, H.; Bauer, I.; Stockhausen, A.; Sasse, H.; Sandmann, I.; Hörsch, S.; Rensing, H. Antibiotics modulate the stimulated cytokine response to endotoxin in a human ex vivo, in vitro model. Acta Anaesthesiol. Scand. 2006, 50, 1103–1110. [Google Scholar] [CrossRef]
- Sauer, A.; Peukert, K.; Putensen, C.; Bode, C. Antibiotics as immunomodulators: A potential pharmacologic approach for ARDS treatment. Eur. Respir. Rev. 2021, 30, 210093. [Google Scholar] [CrossRef]
- Wang, J.; Shao, W.; Niu, H.; Yang, T.; Wang, Y.; Cai, Y. Immunomodulatory Effects of Colistin on Macrophages in Rats by Activating the p38/MAPK Pathway. Front. Pharmacol. 2019, 10, 729. [Google Scholar] [CrossRef]
- Lee, E.Y.; Lee, M.W.; Wong, G.C. Modulation of toll-like receptor signaling by antimicrobial peptides. Semin. Cell Dev. Biol. 2019, 88, 173–184. [Google Scholar] [CrossRef]
- Bode, C.; Diedrich, B.; Muenster, S.; Hentschel, V.; Weisheit, C.; Rommelsheim, K.; Hoeft, A.; Meyer, R.; Boehm, O.; Knuefermann, P.; et al. Antibiotics regulate the immune response in both presence and absence of lipopolysaccharide through modulation of Toll-like receptors, cytokine production and phagocytosis in vitro. Int. Immunopharmacol. 2014, 18, 27–34. [Google Scholar] [CrossRef]
- Bode, C.; Muenster, S.; Diedrich, B.; Jahnert, S.; Weisheit, C.; Steinhagen, F.; Boehm, O.; Hoeft, A.; Meyer, R.; Baumgarten, G. Linezolid, vancomycin and daptomycin modulate cytokine production, Toll-like receptors and phagocytosis in a human in vitro model of sepsis. J. Antibiot. 2015, 68, 485–490. [Google Scholar] [CrossRef]
- Algorri, M.; Wong-Beringer, A. Differential effects of antibiotics on neutrophils exposed to lipoteichoic acid derived from Staphylococcus aureus. Ann. Clin. Microbiol. Antimicrob. 2020, 19, 50. [Google Scholar] [CrossRef]
- Matsumoto, T.; Tateda, K.; Miyazaki, S.; Furuya, N.; Ohno, A.; Ishii, Y.; Hirakata, Y.; Yamaguchi, K. Fosfomycin Alters Lipopolysaccharide-Induced Inflammatory Cytokine Production in Mice. Antimicrob. Agents Chemother. 1999, 43, 697–698. [Google Scholar] [CrossRef][Green Version]
- Cai, Y.; Cao, X.; Aballay, A. Whole-animal chemical screen identifies colistin as a new immunomodulator that targets conserved pathways. mBio 2014, 5, e01235-14. [Google Scholar] [CrossRef]
- Kim, D.H.; Feinbaum, R.; Alloing, G.; Emerson, F.E.; Garsin, D.A.; Inoue, H.; Tanaka-Hino, M.; Hisamoto, N.; Matsumoto, K.; Tan, M.W.; et al. A conserved p38 MAP kinase pathway in Caenorhabditis elegans innate immunity. Science 2002, 297, 623–626. [Google Scholar] [CrossRef]
- Niu, H.; Yang, T.; Wang, J.; Wang, R.; Cai, Y. Immunomodulatory Effect of Colistin and its Protective Role in Rats with Methicillin-Resistant Staphylococcus aureus-induced Pneumonia. Front Pharmacol. 2021, 11, 602054. [Google Scholar] [CrossRef]
- Lauhio, A.; Hästbacka, J.; Pettilä, V.; Tervahartiala, T.; Karlsson, S.; Varpula, T.; Varpula, M.; Ruokonen, E.; Sorsa, T.; Kolho, E. Serum MMP-8, -9 and TIMP-1 in sepsis: High serum levels of MMP-8 and TIMP-1 are associated with fatal outcome in a multicentre, prospective cohort study. Hypothetical impact of tetracyclines. Pharmacol. Res. 2011, 64, 590–594. [Google Scholar] [CrossRef]
- Hästbacka, J.; Linko, R.; Tervahartiala, T.; Varpula, T.; Hovilehto, S.; Parviainen, I.; Vaara, S.T.; Sorsa, T.; Pettilä, V. Serum MMP-8 and TIMP-1 in critically ill patients with acute respiratory failure: TIMP-1 is associated with increased 90-day mortality. Anesth. Analg. 2014, 118, 790–798. [Google Scholar] [CrossRef]
- Martin, G.; Asensi, V.; Montes, A.H.; Collazos, J.; Alvarez, V.; Carton, J.A.; Taboada, F.; Valle-Garay, E. Role of plasma matrix-metalloproteases (MMPs) and their polymorphisms (SNPs) in sepsis development and outcome in ICU patients. Sci. Rep. 2014, 4, 5002. [Google Scholar] [CrossRef]
- Cinelli, M.A.; Do, H.T.; Miley, G.P.; Silverman, R.B. Inducible nitric oxide synthase: Regulation, structure, and inhibition. Med. Res. Rev. 2020, 40, 158–189. [Google Scholar] [CrossRef]
- Hu, S.; Pi, Q.; Xu, X.; Yan, J.; Guo, Y.; Tan, W.; He, A.; Cheng, Z.; Luo, S.; Xia, Y. Disrupted eNOS activity and expression account for vasodilator dysfunction in different stage of sepsis. Life Sci. 2021, 264, 118606. [Google Scholar] [CrossRef]
- Dunston, C.R.; Griffiths, H.R.; Lambert, P.A.; Staddon, S.; Vernallis, A.B. Proteomic analysis of the anti-inflammatory action of minocycline. Proteomics 2011, 11, 42–51. [Google Scholar] [CrossRef]
- Tinker, A.C.; Wallace, A.V. Selective inhibitors of inducible nitric oxide synthase: Potential agents for the treatment of inflammatory diseases? Curr. Top. Med. Chem. 2006, 6, 77–92. [Google Scholar] [CrossRef]
- Gamcrlidze, M.M.; Intskirveli, N.A.; Vardosanidze, K.D.; Chikhladze, K.h.E.; Goliadze LSh Ratiani, L.R. Vasoplegia in septic shock (review). Georgian Med. News 2015, 56–62. [Google Scholar]
- English, B.K.; Maryniw, E.M.; Talati, A.J.; Meals, E.A. Diminished macrophage inflammatory response to Staphylococcus aureus isolates exposed to daptomycin versus vancomycin or oxacillin. Antimicrob. Agents Chemother. 2006, 50, 2225–2227. [Google Scholar] [CrossRef]
- Mayumi, T.; Takezawa, J.; Takahashi, H.; Kuwayama, N.; Fukuoka, T.; Shimizu, K.; Yamada, K.; Kondo, S.; Aono, K. Low-dose intramuscular polymyxin B improves survival of septic rats. Shock Augusta Ga 1999, 11, 82–86. [Google Scholar] [CrossRef]
- Maybauer, M.O.; Maybauer, D.M.; Fraser, J.F.; Traber, L.D.; Westphal, M.; Cox, R.A.; Huda, R.; Nakano, Y.Y.; Enkhbaatar, P.; Hawkins, H.K.; et al. Ceftazidime improves hemodynamics and oxygenation in ovine smoke inhalation injury and septic shock. Intensive Care Med. 2007, 33, 1219–1227. [Google Scholar] [CrossRef]
- Aziz, M.; Jacob, A.; Yang, W.-L.; Matsuda, A.; Wang, P. Current trends in inflammatory and immunomodulatory mediators in sepsis. J. Leukoc. Biol. 2013, 93, 329–342. [Google Scholar] [CrossRef]
- Aziz, M.; Jacob, A.; Wang, P. Revisiting caspases in sepsis. Cell Death Dis. 2014, 5, e1526. [Google Scholar] [CrossRef]
- Hotchkiss, R.S.; Osmon, S.B.; Chang, K.C.; Wagner, T.H.; Coopersmith, C.M.; Karl, I.E. Accelerated lymphocyte death in sepsis occurs by both the death receptor and mitochondrial pathways. J. Immunol. Baltim. Md 1950 2005, 174, 5110–5118. [Google Scholar] [CrossRef]
- Nevière, R.; Fauvel, H.; Chopin, C.; Formstecher, P.; Marchetti, P. Caspase Inhibition Prevents Cardiac Dysfunction and Heart Apoptosis in a Rat Model of Sepsis. Am. J. Respir. Crit. Care Med. 2001, 163, 218–225. [Google Scholar] [CrossRef]
- Tao, R.; Kim, S.H.; Honbo, N.; Karliner, J.S.; Alano, C.C. Minocycline protects cardiac myocytes against simulated ischemia–reperfusion injury by inhibiting poly(ADP-ribose) polymerase-1. J. Cardiovasc. Pharmacol. 2010, 56, 659–668. [Google Scholar] [CrossRef]
- Li, J.; McCullough, L.D. Sex differences in minocycline-induced neuroprotection after experimental stroke. J. Cereb. Blood Flow Metab. Off. J. Int. Soc. Cereb. Blood Flow Metab. 2009, 29, 670–674. [Google Scholar] [CrossRef]
- Fan, L.C.; Lin, J.L.; Yang, J.W.; Mao, B.; Lu, H.W.; Ge, B.X.; Choi, A.M.K.; Xu, J.F. Macrolides protect against Pseudomonas aeruginosa infection via inhibition of inflammasomes. Am. J. Physiol. Lung Cell. Mol. Physiol. 2017, 313, L677–L686. [Google Scholar] [CrossRef]
- Busani, S.; De Biasi, S.; Nasi, M.; Paolini, A.; Venturelli, S.; Tosi, M.; Girardis, M.; Cossarizza, A. Increased Plasma Levels of Mitochondrial DNA and Normal Inflammasome Gene Expression in Monocytes Characterize Patients With Septic Shock Due to Multidrug Resistant Bacteria. Front. Immunol. 2020, 11, 768. [Google Scholar] [CrossRef]
- Peukert, K.; Fox, M.; Schulz, S.; Feuerborn, C.; Frede, S.; Putensen, C.; Wrigge, H.; Kümmerer, B.M.; David, S.; Seeliger, B.; et al. Inhibition of Caspase-1 with Tetracycline Ameliorates Acute Lung Injury. Am. J. Respir. Crit. Care Med. 2021, 204, 53–63. [Google Scholar] [CrossRef]
- Kullberg, R.F.J.; Wiersinga, W.J.; Haak, B.W. Gut microbiota and sepsis: From pathogenesis to novel treatments. Curr. Opin. Gastroenterol. 2021, 37, 578–585. [Google Scholar] [CrossRef]
- Khosravi, A.; Yáñez, A.; Price, J.G.; Chow, A.; Merad, M.; Goodridge, H.S.; Mazmanian, S.K. Gut microbiota promote hematopoiesis to control bacterial infection. Cell Host Microbe 2014, 15, 374–381. [Google Scholar] [CrossRef]
- Campbell, C.; Kandalgaonkar, M.R.; Golonka, R.M.; Yeoh, B.S.; Vijay-Kumar, M.; Saha, P. Crosstalk between Gut Microbiota and Host Immunity: Impact on Inflammation and Immunotherapy. Biomedicines 2023, 11, 294. [Google Scholar] [CrossRef]
- Clarke, T.B.; Davis, K.M.; Lysenko, E.S.; Zhou, A.Y.; Yu, Y.; Weiser, J.N. Recognition of peptidoglycan from the microbiota by Nod1 enhances systemic innate immunity. Nat. Med. 2010, 16, 228–231. [Google Scholar] [CrossRef]
- Clarke, T.B. Early innate immunity to bacterial infection in the lung is regulated systemically by the commensal microbiota via nod-like receptor ligands. Infect. Immun. 2014, 82, 4596–4606. [Google Scholar] [CrossRef]
- Ganal, S.C.; Sanos, S.L.; Kallfass, C.; Oberle, K.; Johner, C.; Kirschning, C.; Lienenklaus, S.; Weiss, S.; Staeheli, P.; Aichele, P.; et al. Priming of natural killer cells by nonmucosal mononuclear phagocytes requires instructive signals from commensal microbiota. Immunity 2012, 37, 171–186. [Google Scholar] [CrossRef]
- Hill, D.A.; Hoffmann, C.; Abt, M.C.; Du, Y.; Kobuley, D.; Kirn, T.J.; Bushman, F.D.; Artis, D. Metagenomic analyses reveal antibiotic-induced temporal and spatial changes in intestinal microbiota with associated alterations in immune cell homeostasis. Mucosal Immunol. 2010, 3, 148–158. [Google Scholar] [CrossRef]
- Ichinohe, T.; Pang, I.K.; Kumamoto, Y.; Peaper, D.R.; Ho, J.H.; Murray, T.S.; Iwasaki, A. Microbiota regulates immune defense against respiratory tract influenza A virus infection. Proc. Natl. Acad. Sci. USA 2011, 108, 5354–5359. [Google Scholar] [CrossRef]
- Schuijt, T.J.; Lankelma, J.M.; Scicluna, B.P.; de Sousa e Melo, F.; Roelofs, J.J.; de Boer, J.D.; Hoogendijk, A.J.; de Beer, R.; de Vos, A.; Belzer, C.; et al. The gut microbiota plays a protective role in the host defence against pneumococcal pneumonia. Gut 2016, 65, 575–583. [Google Scholar] [CrossRef]
- Chen, L.-W.; Chen, P.-H.; Hsu, C.-M. Commensal microflora contribute to host defense against Escherichia coli pneumonia through Toll-like receptors. Shock Augusta Ga 2011, 36, 67–75. [Google Scholar] [CrossRef]
- Sun, S.; Wang, D.; Dong, D.; Xu, L.; Xie, M.; Wang, Y.; Ni, T.; Jiang, W.; Zhu, X.; Ning, N.; et al. Altered intestinal microbiome and metabolome correspond to the clinical outcome of sepsis. Crit. Care Lond. Engl. 2023, 27, 127. [Google Scholar] [CrossRef]
- Xiao, K.; Sun, Y.; Song, J.; Li, L.; Mao, W.; Jiang, C. Gut microbiota involved in myocardial dysfunction induced by sepsis. Microb. Pathog. 2023, 175, 105984. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, F.; Ye, X.; Hu, J.J.; Yang, X.; Yao, L.; Zhao, B.C.; Deng, F.; Liu, K.X. Association Between Gut Dysbiosis and Sepsis-Induced Myocardial Dysfunction in Patients With Sepsis or Septic Shock. Front. Cell. Infect. Microbiol. 2022, 12, 857035. [Google Scholar] [CrossRef]
- Schirmer, M.; Smeekens, S.P.; Vlamakis, H.; Jaeger, M.; Oosting, M.; Franzosa, E.A.; Ter Horst, R.; Jansen, T.; Jacobs, L.; Bonder, M.J.; et al. Linking the Human Gut Microbiome to Inflammatory Cytokine Production Capacity. Cell 2016, 167, 1125–1136.e8. [Google Scholar] [CrossRef]
- Lankelma, J.M.; Belzer, C.; Hoogendijk, A.J.; de Vos, A.F.; de Vos, W.M.; van der Poll, T.; Wiersinga, W.J. Antibiotic-Induced Gut Microbiota Disruption Decreases TNF-α Release by Mononuclear Cells in Healthy Adults. Clin. Transl. Gastroenterol. 2016, 7, e186. [Google Scholar] [CrossRef]
- Dufour, V.; Millon, L.; Faucher, J.F.; Bard, E.; Robinet, E.; Piarroux, R.; Vuitton, D.A.; Meillet, D. Effects of a short-course of amoxicillin/clavulanic acid on systemic and mucosal immunity in healthy adult humans. Int. Immunopharmacol. 2005, 5, 917–928. [Google Scholar] [CrossRef]
- Shimizu, K.; Ogura, H.; Hamasaki, T.; Goto, M.; Tasaki, O.; Asahara, T.; Nomoto, K.; Morotomi, M.; Matsushima, A.; Kuwagata, Y.; et al. Altered gut flora are associated with septic complications and death in critically ill patients with systemic inflammatory response syndrome. Dig. Dis. Sci. 2011, 56, 1171–1177. [Google Scholar] [CrossRef]
- Prescott, H.C.; Dickson, R.P.; Rogers MA, M.; Langa, K.M.; Iwashyna, T.J. Hospitalization Type and Subsequent Severe Sepsis. Am. J. Respir. Crit. Care Med. 2015, 192, 581–588. [Google Scholar] [CrossRef]
- Shimizu, K.; Ogura, H.; Tomono, K.; Tasaki, O.; Asahara, T.; Nomoto, K.; Morotomi, M.; Matsushima, A.; Nakahori, Y.; Yamano, S.; et al. Patterns of Gram-Stained Fecal Flora as a Quick Diagnostic Marker in Patients with Severe SIRS. Dig. Dis. Sci. 2011, 56, 1782–1788. [Google Scholar] [CrossRef]
- Ojima, M.; Shimizu, K.; Motooka, D.; Ishihara, T.; Nakamura, S.; Shintani, A.; Ogura, H.; Iida, T.; Yoshiya, K.; Shimazu, T. Gut Dysbiosis Associated with Antibiotics and Disease Severity and Its Relation to Mortality in Critically Ill Patients. Dig. Dis. Sci. 2022, 67, 2420–2432. [Google Scholar] [CrossRef]
- Zimmermann, P.; Ziesenitz, V.C.; Curtis, N.; Ritz, N. The Immunomodulatory Effects of Macrolides—A Systematic Review of the Underlying Mechanisms. Front. Immunol. 2018, 9, 302. [Google Scholar] [CrossRef] [PubMed]
- Kyprianou, M.; Dakou, K.; Aktar, A.; Aouina, H.; Behbehani, N.; Dheda, K.; Juvelekian, G.; Khattab, A.; Mahboub, B.; Nyale, G.; et al. Macrolides for better resolution of community-acquired pneumonia: A global meta-analysis of clinical outcomes with focus on microbial aetiology. Int. J. Antimicrob. Agents 2023, 62, 106942. [Google Scholar] [CrossRef]
- Nie, W.; Li, B.; Xiu, Q. β-Lactam/macrolide dual therapy versus β-lactam monotherapy for the treatment of community-acquired pneumonia in adults: A systematic review and meta-analysis. J. Antimicrob. Chemother. 2014, 69, 1441–1446. [Google Scholar] [CrossRef]
- Garin, N.; Genné, D.; Carballo, S.; Chuard, C.; Eich, G.; Hugli, O.; Lamy, O.; Nendaz, M.; Petignat, P.A.; Perneger, T.; et al. β-Lactam monotherapy vs β-lactam-macrolide combination treatment in moderately severe community-acquired pneumonia: A randomized noninferiority trial. JAMA Intern. Med. 2014, 174, 1894–1901. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo, M.J.; Moret, I.; Sarria, B.; Cases, E.; Cortijo, J.; Méndez, R.; Molina, J.; Gimeno, A.; Menéndez, R. Lung inflammatory pattern and antibiotic treatment in pneumonia. Respir. Res. 2015, 16, 15. [Google Scholar] [CrossRef]
- Ceccato, A.; Cilloniz, C.; Martin-Loeches, I.; Ranzani, O.T.; Gabarrus, A.; Bueno, L.; Garcia-Vidal, C.; Ferrer, M.; Niederman, M.S.; Torres, A. Effect of Combined β-Lactam/Macrolide Therapy on Mortality According to the Microbial Etiology and Inflammatory Status of Patients With Community-Acquired Pneumonia. Chest 2019, 155, 795–804. [Google Scholar] [CrossRef]
- Cilloniz, C.; Albert, R.K.; Liapikou, A.; Gabarrus, A.; Rangel, E.; Bello, S.; Marco, F.; Mensa, J.; Torres, A. The Effect of Macrolide Resistance on the Presentation and Outcome of Patients Hospitalized for Streptococcus pneumoniae Pneumonia. Am. J. Respir. Crit. Care Med. 2015, 191, 1265–1272. [Google Scholar] [CrossRef]
- Giamarellos-Bourboulis, E.J.; Siampanos, A.; Bolanou, A.; Doulou, S.; Kakavoulis, N.; Tsiakos, K.; Katopodis, S.; Schinas, G.; Skorda, L.; Alexiou, Z.; et al. Clarithromycin for early anti-inflammatory responses in community-acquired pneumonia in Greece (ACCESS): A randomised, double-blind, placebo-controlled trial. Lancet Respir. Med. 2024, 12, 294–304. [Google Scholar] [CrossRef]
- Kong, M.; Zhang, W.W.; Sewell, K.; Gorman, G.; Kuo, H.C.; Aban, I.; Ambalavanan, N.; Whitley, R.J. Azithromycin Treatment vs Placebo in Children With Respiratory Syncytial Virus–Induced Respiratory Failure: A Phase 2 Randomized Clinical Trial. JAMA Netw. Open 2020, 3, e203482. [Google Scholar] [CrossRef]
- Spyridaki, A.; Raftogiannis, M.; Antonopoulou, A.; Tsaganos, T.; Routsi, C.; Baziaka, F.; Karagianni, V.; Mouktaroudi, M.; Koutoukas, P.; Pelekanou, A.; et al. Effect of clarithromycin in inflammatory markers of patients with ventilator-associated pneumonia and sepsis caused by Gram-negative bacteria: Results from a randomized clinical study. Antimicrob. Agents Chemother. 2012, 56, 3819–3825. [Google Scholar] [CrossRef]
- Reijnders, T.D.Y.; Peters-Sengers, H.; van Vught, L.A.; Uhel, F.; Bonten, M.J.M.; Cremer, O.L.; Schultz, M.J.; Stuiver, M.M.; van der Poll, T.; MARS consortium. Effect of erythromycin on mortality and the host response in critically ill patients with sepsis: A target trial emulation. Crit. Care Lond. Engl. 2022, 26, 151. [Google Scholar] [CrossRef] [PubMed]
- Zhao, P.; Yao, R.; Yang, J.; Wen, W.; Yao, Y.; Du, X. Efficacy and safety of clarithromycin for patients with sepsis or septic shock: A systematic review and meta-analysis. Emerg. Crit. Care Med. 2023, 11, 26. [Google Scholar] [CrossRef]
- Karakike, E.; Scicluna, B.P.; Roumpoutsou, M.; Mitrou, I.; Karampela, N.; Karageorgos, A.; Psaroulis, K.; Massa, E.; Pitsoulis, A.; Chaloulis, P.; et al. Effect of intravenous clarithromycin in patients with sepsis, respiratory and multiple organ dysfunction syndrome: A randomized clinical trial. Crit. Care Lond. Engl. 2022, 26, 183. [Google Scholar] [CrossRef] [PubMed]
- Simonis, F.D.; de Iudicibus, G.; Cremer, O.L.; Ong, D.S.Y.; van der Poll, T.; Bos, L.D.; Schultz, M.J.; MARS consortium. Macrolide therapy is associated with reduced mortality in acute respiratory distress syndrome (ARDS) patients. Ann. Transl. Med. 2018, 6, 24. [Google Scholar] [CrossRef]
- Berti, A.; Rose, W.; Nizet, V.; Sakoulas, G. Antibiotics and Innate Immunity: A Cooperative Effort Towards the Successful Treatment of Infections. Open Forum Infect. Dis. 2020, 7, ofaa302. [Google Scholar] [CrossRef]
| Antibiotic’s Class | Pro-Inflammatory Cytokines Production | TLRs Expression Modulation | MMPs and NO | Apoptosis Regulation |
|---|---|---|---|---|
| Macrolides | Suppression (Clarithromycin, Azithromycin) | Modulation in TLRs and control of phagocytic activity (Erythromycin). | Reduced production (all macrolides) | Suppression of caspases activity resulting in enhanced bacterial clearance (Azithromycin) |
| Tigecycline | Suppression in concentration-dependent manner | Inhibition of NO production induced by LPS | ||
| Tetracyclines | Modulation in TLRs expression and regulation of phagocytic activity (Doxycycline) | Decreased MMPs activity, mitigating inflammation. Reduced NO production | Inhibition of caspases against apoptosis (Minocycline) | |
| Clindamycin | Suppression in concentration-dependent manner | |||
| Trimethoprim-Sulfamethoxazole | Suppression in concentration-dependent manner | |||
| Linezolid | Suppression in concentration-dependent manner | Upregulation of TLRs expression resulting in pro-inflammatory effect | ||
| Glycopeptides | Stimulation of anti-inflammatory cytokines (Vancomycin) | Upregulation of TLRs expression resulting in pro-inflammatory effect (Vancomycin) | ||
| Daptomycin | Suppression | Downregulation of TLRs transcription resulting in anti-inflammatory effect | Reduction of accumulation | |
| Quinolones | Suppression (Ciprofloxacin) | Modulation in TLRs expression and regulation of phagocytic activity (Moxifloxacin) | Inhibition of NO production induced by LPS | |
| Cephalosporins | Stimulation (Cefuroxime, Cefotaxime) | Downregulation of TLRs transcription resulting in anti-inflammatory effect (Cefuroxime, Cefotaxime) Immunostimulatory effects on neutrophil phagocytosis (Ceftaroline) | Reduction of nitrosative stress (Ceftazidime) | |
| Polymyxins | Stimulation (Colistin) | Enhance macrophages’ phagocytic function (Colistin) Innate immunity activation via a p38/PMK-1-pathway (Colistin) | Reduced NO production (Polymyxin B) | |
| Fosfomycin | Reduction of synthesis | Decreased the expression of TLR-4 and TNF in lung tissue during sepsis and ARDS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tosi, M.; Coloretti, I.; Meschiari, M.; De Biasi, S.; Girardis, M.; Busani, S. The Interplay between Antibiotics and the Host Immune Response in Sepsis: From Basic Mechanisms to Clinical Considerations: A Comprehensive Narrative Review. Antibiotics 2024, 13, 406. https://doi.org/10.3390/antibiotics13050406
Tosi M, Coloretti I, Meschiari M, De Biasi S, Girardis M, Busani S. The Interplay between Antibiotics and the Host Immune Response in Sepsis: From Basic Mechanisms to Clinical Considerations: A Comprehensive Narrative Review. Antibiotics. 2024; 13(5):406. https://doi.org/10.3390/antibiotics13050406
Chicago/Turabian StyleTosi, Martina, Irene Coloretti, Marianna Meschiari, Sara De Biasi, Massimo Girardis, and Stefano Busani. 2024. "The Interplay between Antibiotics and the Host Immune Response in Sepsis: From Basic Mechanisms to Clinical Considerations: A Comprehensive Narrative Review" Antibiotics 13, no. 5: 406. https://doi.org/10.3390/antibiotics13050406
APA StyleTosi, M., Coloretti, I., Meschiari, M., De Biasi, S., Girardis, M., & Busani, S. (2024). The Interplay between Antibiotics and the Host Immune Response in Sepsis: From Basic Mechanisms to Clinical Considerations: A Comprehensive Narrative Review. Antibiotics, 13(5), 406. https://doi.org/10.3390/antibiotics13050406






