Patterns of Amphotericin B Use and Factors Related to Mortality in a Low-Middle Income Country: An Observational and Longitudinal Study
Abstract
1. Introduction
2. Results
2.1. Sociodemographic
2.2. Clinics
2.3. Pharmacological Treatment
2.4. Laboratory
2.5. Complications
2.6. Multivariate Analysis
3. Discussion
4. Materials and Methods
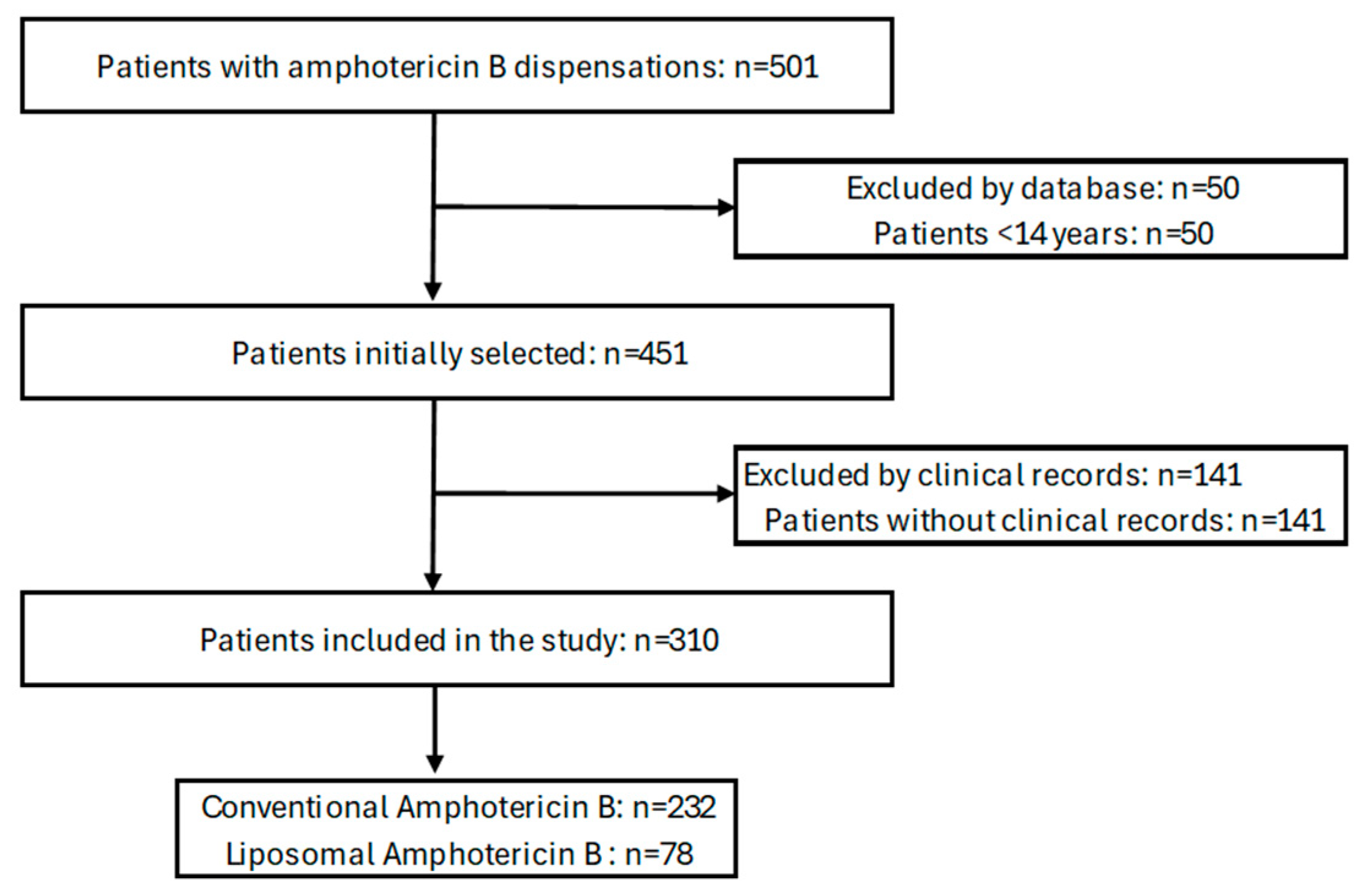
4.1. Study Design and Patients
4.2. Variables
- 1.
- Sociodemographic data: sex, age, occupation, education, affiliation regime (contributory or subsidized) and place of origin. The place of origin was categorized by departments according to the regions of Colombia, considering the classification of the National Administrative Department of Statistics (DANE) of Colombia, as follows: Caribbean, Central, Bogotá–Cundinamarca, Pacific and Eastern-Orinoquia–Amazon.
- 2.
- Clinics:
- (a)
- Physiological variables: systolic blood pressure, diastolic blood pressure, heart rate, respiratory rate, oxygen saturation and state of consciousness (Glasgow) at the time of initial care.
- (b)
- Anthropometric measurements: weight, height and body mass index.
- (c)
- Diagnosis: The type of systemic fungal infection present in each patient was determined (Cryptococcus neoformans, Histoplasma capsulatum, Candida albicans and other Candidas, Aspergillus spp., Mucor spp., etc.), as well as other coinfections (Mycobacterium tuberculosis, Pneumocystis jirovecii, cytomegalovirus, and Toxoplasma gondii, among others). The diagnoses were taken from the patients’ clinical records, which were based on the clinical criteria of the internist or infectious disease physician, as well as laboratory studies (microscopic studies, cultures, molecular studies, etc.). Candida lusitaniae and Aspergillus terreus are not sensitive to amphotericin B.
- (d)
- Comorbidities: solid or hematological neoplasms, human immunodeficiency virus (HIV), rheumatological diseases (rheumatoid arthritis, systemic lupus erythematosus, vasculitis, and others), chronic kidney disease, liver cirrhosis, high blood pressure, and diabetes mellitus, among others. An age-adjusted Charlson Comorbidity Index (CCI) score was calculated.
- (e)
- Complications: sepsis, septic shock and in-hospital mortality were identified. A Quick Sequential Organ Failure Assessment (qSOFA) score was calculated.
- 3.
- Laboratory: complete blood count, total bilirubin, direct bilirubin, aspartate aminotransferase, alanine aminotransferase, lactate dehydrogenase, electrolytes (sodium and potassium), urea nitrogen, and creatinine, at the time of initial care, before starting amphotericin B therapy and at the end of therapy. The glomerular filtration rate (GFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) 2021 equation.
- 4.
- Therapeutics/Management:
- (a)
- Place of care: hospitalization in general wards and intensive care units (ICUs).
- (b)
- Use of supplemental oxygen: oxygen requirement, mechanical ventilation and need for tracheostomy.
- (c)
- Amphotericin B: type (conventional, lipid complex, liposomal or colloidal dispersion), dose used (mg per day), defined daily dose (DDD), duration of therapy, time of infusion, changes in the type of amphotericin B, indications (aspergillosis, candidiasis, cryptococcosis, and histoplasmosis, among others), monotherapy vs. combined antifungal therapy (azoles and echinocandins, among others), and prophylactic or therapeutic use.
- (d)
- Comedications: vasopressors and inotropics, antihypertensives and diuretics, normoglycemic agents, antiulcers, other systemic antimicrobials (antibiotics, antivirals, etc.), anticoagulants, analgesics and anti-inflammatories, benzodiazepines, systemic corticosteroids, antipsychotics, and antihistamines, among others.
4.3. Ethics Statement
4.4. Data Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Denning, D.W. Global incidence and mortality of severe fungal disease. Lancet Infect. Dis. 2024, 24, e428–e438. [Google Scholar] [CrossRef] [PubMed]
- WHO Fungal Priority Pathogens List to Guide Research, Development and Public Health Action; World Health Organization: Geneva, Switzerland, 2022; Licence: CC BY-NC-SA 3.0 IGO; Available online: https://www.who.int/publications/i/item/9789240060241 (accessed on 1 September 2023).
- Lionakis, M.S.; Drummond, R.A.; Hohl, T.M. Immune responses to human fungal pathogens and therapeutic prospects. Nat. Rev. Immunol. 2023, 23, 433–452. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Bills, G.F.; An, Z. Advances in the treatment of invasive fungal disease. PLoS Pathog. 2023, 19, e1011322. [Google Scholar] [CrossRef] [PubMed]
- Hamill, R.J. Amphotericin B formulations: A comparative review of efficacy and toxicity. Drugs 2013, 73, 919–934. [Google Scholar] [CrossRef] [PubMed]
- Cavassin, F.B.; Baú-Carneiro, J.L.; Vilas-Boas, R.R.; Queiroz-Telles, F. Sixty years of Amphotericin B: An Overview of the Main Antifungal Agent Used to Treat Invasive Fungal Infections. Infect. Dis. Ther. 2021, 10, 115–147. [Google Scholar] [CrossRef]
- Yang, Y.L.; Xiang, Z.J.; Yang, J.H.; Wang, W.J.; Xu, Z.C.; Xiang, R.L. Adverse Effects Associated With Currently Commonly Used Antifungal Agents: A Network Meta-Analysis and Systematic Review. Front. Pharmacol. 2021, 12, 697330. [Google Scholar] [CrossRef]
- Steimbach, L.M.; Tonin, F.S.; Virtuoso, S.; Borba, H.H.; Sanches, A.C.; Wiens, A.; Fernandez-Llimós, F.; Pontarolo, R. Efficacy and safety of amphotericin B lipid-based formulations—A systematic review and meta-analysis. Mycoses 2017, 60, 146–154. [Google Scholar] [CrossRef]
- Tonin, F.S.; Steimbach, L.M.; Borba, H.H.; Sanches, A.C.; Wiens, A.; Pontarolo, R.; Fernandez-Llimos, F. Efficacy and safety of amphotericin B formulations: A network meta-analysis and a multicriteria decision analysis. J. Pharm. Pharmacol. 2017, 69, 1672–1683. [Google Scholar] [CrossRef]
- Borba, H.H.L.; Steimbach, L.M.; Riveros, B.S.; Tonin, F.S.; Ferreira, V.L.; Bagatim, B.A.Q.; Balan, G.; Pontarolo, R.; Wiens, A. Cost-effectiveness of amphotericin B formulations in the treatment of systemic fungal infections. Mycoses 2018, 61, 754–763. [Google Scholar] [CrossRef]
- Valladales-Restrepo, L.F.; Ospina-Cano, J.A.; Aristizábal-Carmona, B.S.; López-Caicedo, D.F.; Toro-Londoño, M.; Gaviria-Mendoza, A.; Machado-Duque, M.E.; Machado-Alba, J.E. Study of Prescription-Indication of Outpatient Systemic Anti-Fungals in a Colombian Population. A Cross-Sectional Study. Antibiotics 2022, 11, 1805. [Google Scholar] [CrossRef]
- Andrew, E.C.; Curtis, N.; Coghlan, B.; Cranswick, N.; Gwee, A. Adverse effects of amphotericin B in children; A retrospective comparison of conventional and liposomal formulations. Br. J. Clin. Pharmacol. 2018, 84, 1006–1012. [Google Scholar] [CrossRef] [PubMed]
- Falci, D.R.; da Rosa, F.B.; Pasqualotto, A.C. Comparison of nephrotoxicity associated to different lipid formulations of amphotericin B: A real-life study. Mycoses 2015, 58, 104–112. [Google Scholar] [CrossRef] [PubMed]
- de Souza, M.C.; Santos, A.G.; Reis, A.M. Adverse Drug Reactions in Patients Receiving Systemic Antifungal Therapy at a High-Complexity Hospital. J. Clin. Pharmacol. 2016, 56, 1507–1515. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, M.; Tamura, K.; Masaoka, T.; Nakajo, E. A real-world prospective observational study on the efficacy and safety of liposomal amphotericin B in 426 patients with persistent neutropenia and fever. J. Infect. Chemother. 2021, 27, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Tashiro, M.; Takazono, T.; Ota, Y.; Wakamura, T.; Takahashi, A.; Sato, K.; Miyazaki, T.; Obata, Y.; Nishino, T.; Izumikawa, K. Efficacy of early administration of liposomal amphotericin B in patients with septic shock: A nationwide observational study. J. Infect. Chemother. 2021, 27, 1471–1476. [Google Scholar] [CrossRef]
- Takazono, T.; Tashiro, M.; Ota, Y.; Obata, Y.; Wakamura, T.; Miyazaki, T.; Nishino, T.; Izumikawa, K. Factor analysis of acute kidney injury in patients administered liposomal amphotericin B in a real-world clinical setting in Japan. Sci. Rep. 2020, 10, 15033. [Google Scholar] [CrossRef]
- Egger, M.; Hoenigl, M.; Thompson, G.R., III; Carvalho, A.; Jenks, J.D. Let’s talk about sex characteristics—As a risk factor for invasive fungal diseases. Mycoses 2022, 65, 599–612. [Google Scholar] [CrossRef]
- Amphotericin, B. Drug Point Summary [Database on the Internet]; IBM Corporation: Greenwood Village, CO, USA, 2023; Available online: www.micromedexsolutions.com (accessed on 5 June 2023).
- Consulta de Datos de Productos [Internet]. Instituto Nacional de Vigilancia de Medicamentos y Alimentos (INVIMA). Available online: http://consultaregistro.invima.gov.co/Consultas/consultas/consreg_encabcum.jsp (accessed on 5 June 2023).
- Akinosoglou, K.; Rigopoulos, E.A.; Papageorgiou, D.; Schinas, G.; Polyzou, E.; Dimopoulou, E.; Gogos, C.; Dimopoulos, G. Amphotericin B in the Era of New Antifungals: Where Will It Stand? J. Fungi 2024, 10, 278. [Google Scholar] [CrossRef]
- Xie, P.; Wang, W.; Dong, M. Long-term mortality predictors of ICU fungaemia. Epidemiol. Infect. 2021, 149, e241. [Google Scholar] [CrossRef]
- Alves, P.G.V.; Melo, S.G.O.; Bessa, M.A.S.; Brito, M.O.; Menezes, R.P.; Araújo, L.B.; Penatti, M.P.A.; Pedroso, R.D.S.; Röder, D.V.D.B. Risk factors associated with mortality among patients who had candidemia in a university hospital. Rev. Soc. Bras. Med. Trop. 2020, 53, e20190206. [Google Scholar] [CrossRef]
- Gong, Y.; Li, C.; Wang, C.; Li, J.; Ding, M.; Chen, D.; Lao, M. Epidemiology and Mortality-Associated Factors of Invasive Fungal Disease in Elderly Patients: A 20-Year Retrospective Study from Southern China. Infect. Drug Resist. 2020, 13, 711–723. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Carrozzino, D.; Guidi, J.; Patierno, C. Charlson Comorbidity Index: A Critical Review of Clinimetric Properties. Psychother. Psychosom. 2022, 91, 8–35. [Google Scholar] [CrossRef] [PubMed]
- Serafim, R.; Gomes, J.A.; Salluh, J.; Póvoa, P. A Comparison of the Quick-SOFA and Systemic Inflammatory Response Syndrome Criteria for the Diagnosis of Sepsis and Prediction of Mortality: A Systematic Review and Meta-Analysis. Chest 2018, 153, 646–655. [Google Scholar] [CrossRef] [PubMed]
- Jia, L.; Wang, P.; Li, C.; Xie, J. The efficacy and safety of vasopressors for septic shock patients: A systemic review and network meta-analysis. Shock 2023, 60, 746–752. [Google Scholar] [CrossRef]
- Fang, F.; Zhang, Y.; Tang, J.; Lunsford, L.D.; Li, T.; Tang, R.; He, J.; Xu, P.; Faramand, A.; Xu, J.; et al. Association of Corticosteroid Treatment With Outcomes in Adult Patients With Sepsis: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2019, 179, 213–223. [Google Scholar] [CrossRef]
- Song, Y.; Hao, J.; Liu, Y. Role of corticosteroids in the treatment of critically ill sepsis patients: A meta-analysis review. Inflammopharmacology 2024, 32, 965–974. [Google Scholar] [CrossRef]
- Li, Z.; Denning, D.W. The Impact of Corticosteroids on the Outcome of Fungal Disease: A Systematic Review and Meta-analysis. Curr. Fungal Infect. Rep. 2023, 17, 54–70. [Google Scholar] [CrossRef]
| Variables | Total | |
|---|---|---|
| n = 310 | % | |
| Sociodemographic | ||
| Male | 220 | 71.0 |
| Age, median (IQR) | 44.0 (34.8–58.0) | |
| Region of origin | ||
| Pacific | 173 | 55.8 |
| Central | 112 | 36.1 |
| Bogotá–Cundinamarca | 22 | 7.1 |
| Eastern-Orinoquia-Amazon | 3 | 1.0 |
| Affiliation regime | - | - |
| Subsidized | 166 | 53.5 |
| Contributory | 144 | 46.5 |
| Comorbidities | ||
| Charlson index, median (IQR) | 6 (2–7) | |
| 0 points | 40 | 12.9 |
| 1–2 points | 50 | 16.1 |
| ≥3 points | 220 | 71.0 |
| Human immunodeficiency virus infection | 173 | 55.8 |
| Arterial hypertension | 82 | 26.5 |
| Hematological or solid neoplasms | 63 | 20.3 |
| Chronic kidney disease | 58 | 18.7 |
| Diabetes mellitus | 47 | 15.2 |
| Vital signs (on admission), median (IQR) | ||
| Systolic blood pressure (mmHg) | 115.0 (100.0–125.0) | |
| Diastolic blood pressure (mmHg) | 70.0 (60.0–78.0) | |
| Heart rate (bpm) | 85.0 (78.0–98.3) | |
| Respiratory rate (rpm) | 20.0 (18.0–21.0) | |
| Temperature (°C) | 36.5 (36.0–36.9) | |
| Oxygen saturation (%) | 95.0 (94.0–97.0) | |
| State of consciousness (Glasgow) | 15.0 (15.0–15.0) | |
| Anthropometric measurements, median (IQR) | ||
| Weight (kg) | 57.0 (50.0–65.0) | |
| Height (m) | 1.7 (1.6–1.7) | |
| Body mass index (kg/m2) | 21.5 (18.8–24.2) | |
| Laboratory studies, median (IQR) | ||
| Hemogram | ||
| Hemoglobin (g/dL) | 11.0 (8.8–13.1) | |
| Hematocrit (%) | 32.9 (27.2–39.0) | |
| Leukocytes (/mm³) | 7250.0 (4040.0–11600) | |
| Neutrophils (/mm³) | 4545.0 (2235.0–8392.5) | |
| Lymphocytes (/mm³) | 840.0 (475.0–1500.0) | |
| Platelets (/mm³) | 204,000.0 (112,350.0–293,000.0) | |
| Renal function | ||
| Creatinine (mg/dL) | 0.82 (0.66–1.09) | |
| Glomerular filtration rate (mL/min) a | 104.8 (74.8–119.3) | |
| Urea nitrogen (mg/dL) | 15.3 (11.0–21.9) | |
| Liver function | ||
| Total bilirubin (mg/dL) | 0.59 (0.38–0.94) | |
| Direct bilirubin (mg/dL) | 0.33 (0.21–0.59) | |
| Alanine aminotransferase (U/L) | 33.0 (18.0–56.9) | |
| Aspartate aminotransferase (U/L) | 36.0 (22.0–75.0) | |
| Lactic acid dehydrogenase (U/L) | 308.0 (190.8–694.8) | |
| Electrolytes | ||
| Sodium (mEq/L) | 135.0 (131.0–139.0) | |
| Potassium (mEq/L) | 4.0 (3.6–4.4) | |
| Isolated microorganisms | ||
| Cryptococcus neoformans | 106 | 34.2 |
| Histoplasma capsulatum | 99 | 31.9 |
| Candida albicans | 63 | 20.3 |
| Other Candida | 28 | 9.0 |
| Aspergillus spp. | 17 | 5.5 |
| Cryptococcus spp. | 14 | 4.5 |
| Variables | Conventional Amphotericin B | Liposomal Amphotericin B | ||
|---|---|---|---|---|
| n = 232 | % | n = 78 | % | |
| Sex | ||||
| Men | 166 | 71.6 | 54 | 69.2 |
| Women | 66 | 28.4 | 24 | 30.8 |
| Age | ||||
| Mean ± SD | 47.9 ± 16.5 | 42.6 ± 16.2 | ||
| Median (IQR) | 46.0 (37.0–59.0) | 40.5 (29.0–51.3) | ||
| Prescribed dose | ||||
| Mean ± SD | 44.0 ± 10.9 | 191.3 ± 47.6 | ||
| Median (IQR) | 50.0 (35.0–50.0) | 197.5 (150.0–200.0) | ||
| Mode | 50.0 | 200.0 | ||
| nDDD a | 1.25 | |||
| Treatment days | ||||
| Mean ± SD | 8.5 ± 6.8 | 9.1 ± 7.3 | ||
| Median (IQR) | 6.0 (3.0–14.0) | 8.0 (2.0–14.0) | ||
| Indications | ||||
| Treatment | 214 | 92.2 | 74 | 94.9 |
| Cryptococcosis | 92 | 39.7 | 28 | 35.9 |
| Histoplasmosis | 69 | 29.7 | 30 | 38.5 |
| Candidiasis | 69 | 29.7 | 22 | 28.2 |
| Aspergillosis | 15 | 6.5 | 3 | 3.8 |
| Mucormycosis | 9 | 3.9 | 1 | 1.3 |
| Blastomycosis | 1 | 0.4 | 1 | 1.3 |
| Sporotrichosis | 1 | 0.4 | 1 | 1.3 |
| Coccidioidomycosis | 0 | 0.0 | 1 | 1.3 |
| Leishmaniasis | 1 | 0.4 | 0 | 0.0 |
| Microsporidiasis | 1 | 0.4 | 0 | 0.0 |
| Trichosporonosis | 1 | 0.4 | 0 | 0.0 |
| No data | 3 | 1.3 | 1 | 1.3 |
| Prophylaxis | 18 | 7.8 | 4 | 5.1 |
| Variables | Sig. | HR | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Man (yes/no) | 0.774 | 1.062 | 0.704 | 1.603 |
| Age (continuous) | 0.231 | 0.990 | 0.974 | 1.006 |
| Central-region origin (yes/no) | 0.249 | 0.766 | 0.487 | 1.205 |
| Arterial hypertension (yes/no) | 0.880 | 1.037 | 0.644 | 1.670 |
| Charlson Comorbidity Index (continuous) | <0.001 | 1.136 | 1.058 | 1.220 |
| qSOFA (continuous) | 0.020 | 1.348 | 1.049 | 1.731 |
| Glomerular filtration rate on admission (continuous) | 0.599 | 1.002 | 0.995 | 1.009 |
| Mycobacterium tuberculosis infection (yes/no) | 0.002 | 2.095 | 1.326 | 3.311 |
| Cryptococcosis (yes/no) | 0.804 | 1.051 | 0.709 | 1.558 |
| Conventional amphotericin B (yes/no) | 0.200 | 0.767 | 0.512 | 1.150 |
| Fluconazole (yes/no) | 0.422 | 0.852 | 0.577 | 1.259 |
| Systemic corticosteroids (yes/no) | 0.001 | 0.434 | 0.267 | 0.706 |
| Vasopressors and/or inotropes (yes/no) | <0.001 | 4.205 | 2.167 | 8.157 |
| Invasive mechanical ventilation (yes/no) | 0.003 | 2.734 | 1.401 | 5.332 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valladales-Restrepo, L.F.; Soto-Romero, L.M.; Navarrete-Santa, L.F.; Montoya-García, R.; Ríos-Montoya, J.A.; Sabogal-Ortiz, A.; Machado-Alba, J.E. Patterns of Amphotericin B Use and Factors Related to Mortality in a Low-Middle Income Country: An Observational and Longitudinal Study. Antibiotics 2024, 13, 1015. https://doi.org/10.3390/antibiotics13111015
Valladales-Restrepo LF, Soto-Romero LM, Navarrete-Santa LF, Montoya-García R, Ríos-Montoya JA, Sabogal-Ortiz A, Machado-Alba JE. Patterns of Amphotericin B Use and Factors Related to Mortality in a Low-Middle Income Country: An Observational and Longitudinal Study. Antibiotics. 2024; 13(11):1015. https://doi.org/10.3390/antibiotics13111015
Chicago/Turabian StyleValladales-Restrepo, Luis Fernando, Lian Manuela Soto-Romero, Luis Fernando Navarrete-Santa, Rodrigo Montoya-García, Jaime Andrés Ríos-Montoya, Alejandra Sabogal-Ortiz, and Jorge Enrique Machado-Alba. 2024. "Patterns of Amphotericin B Use and Factors Related to Mortality in a Low-Middle Income Country: An Observational and Longitudinal Study" Antibiotics 13, no. 11: 1015. https://doi.org/10.3390/antibiotics13111015
APA StyleValladales-Restrepo, L. F., Soto-Romero, L. M., Navarrete-Santa, L. F., Montoya-García, R., Ríos-Montoya, J. A., Sabogal-Ortiz, A., & Machado-Alba, J. E. (2024). Patterns of Amphotericin B Use and Factors Related to Mortality in a Low-Middle Income Country: An Observational and Longitudinal Study. Antibiotics, 13(11), 1015. https://doi.org/10.3390/antibiotics13111015







