Phytochemistry, Mechanisms, and Preclinical Studies of Echinacea Extracts in Modulating Immune Responses to Bacterial and Viral Infections: A Comprehensive Review
Abstract
1. Introduction
2. Methodology
3. Phytochemistry
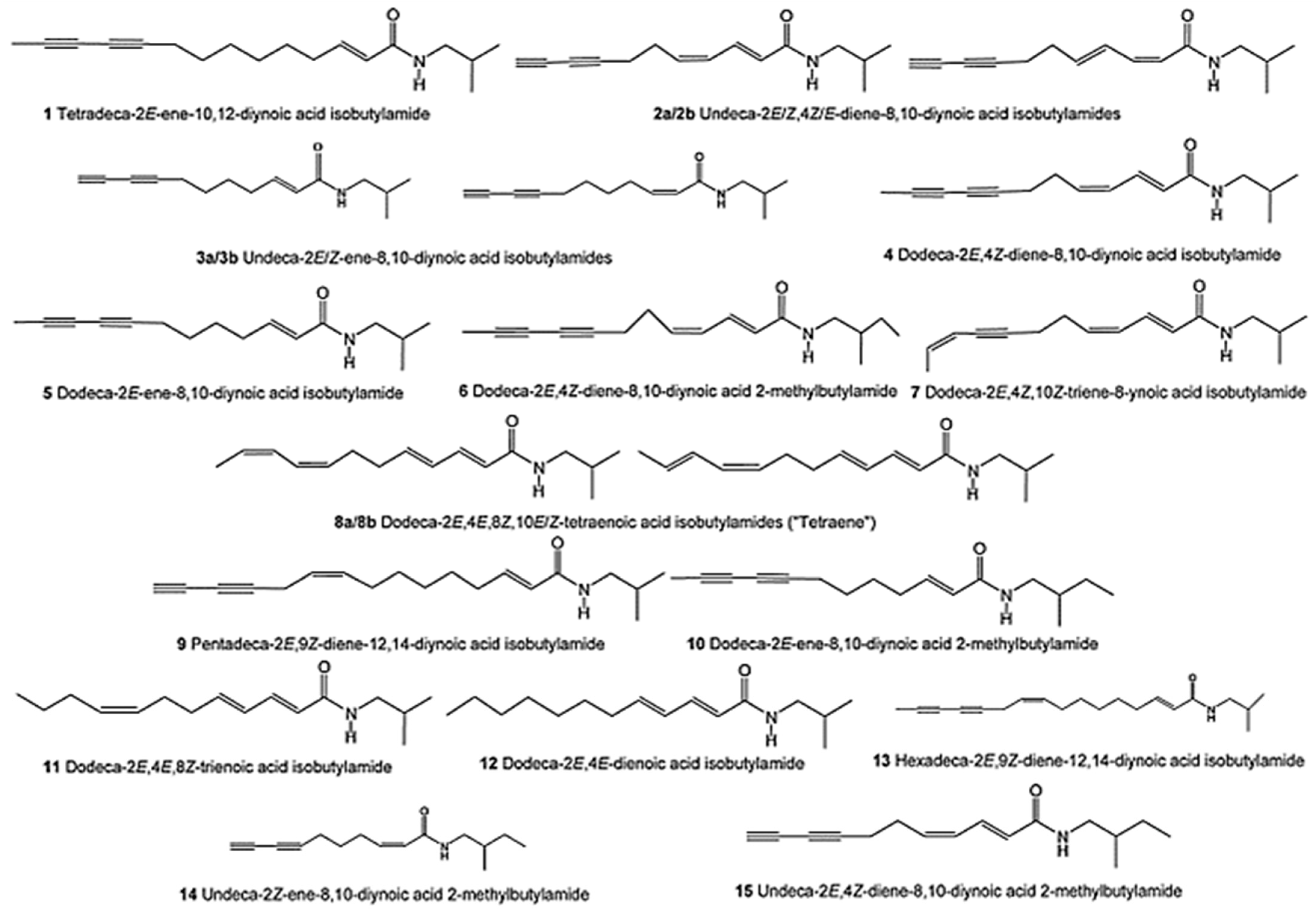
3.1. Alkamides
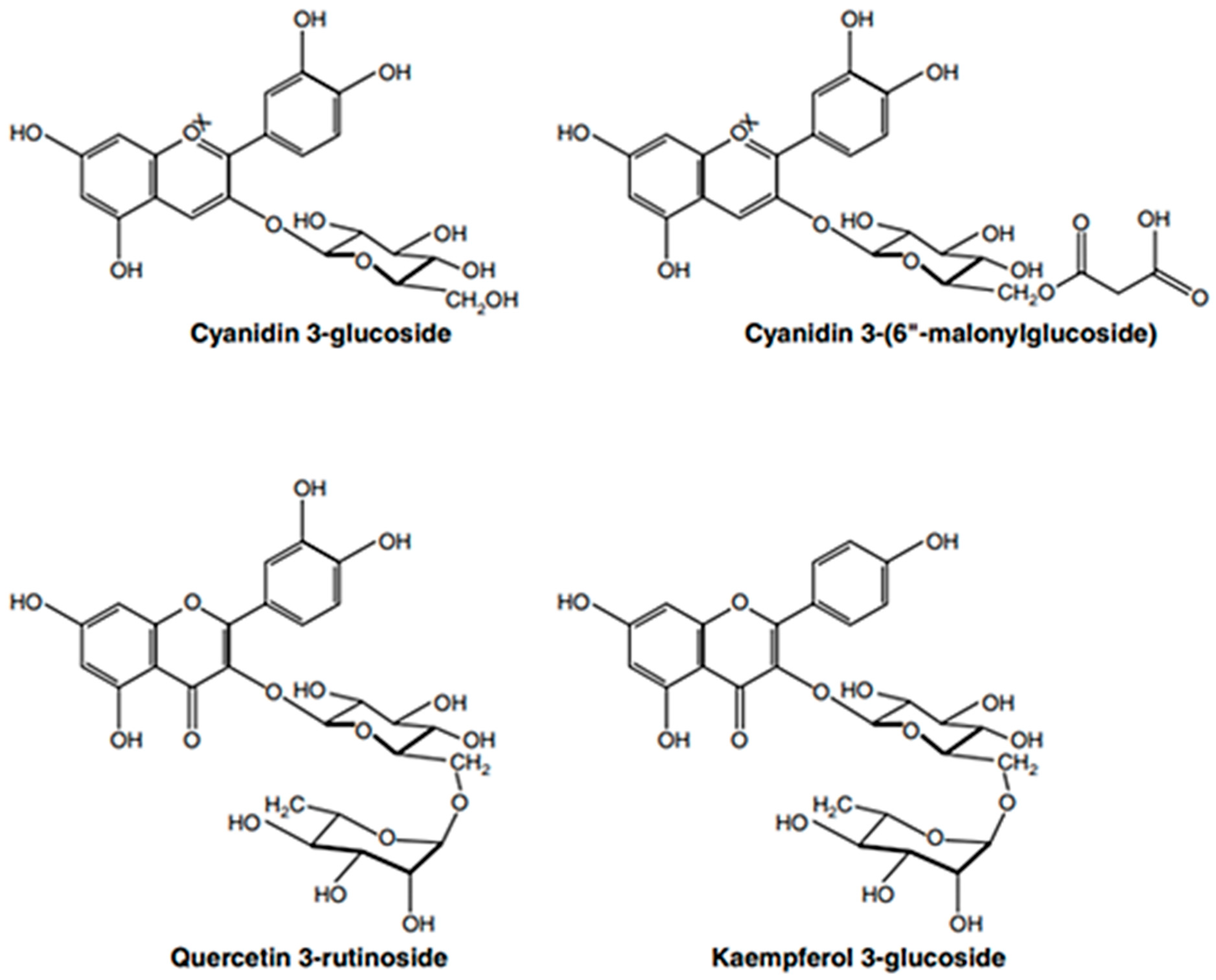
3.2. Flavonoids
3.3. Hydrocarbons
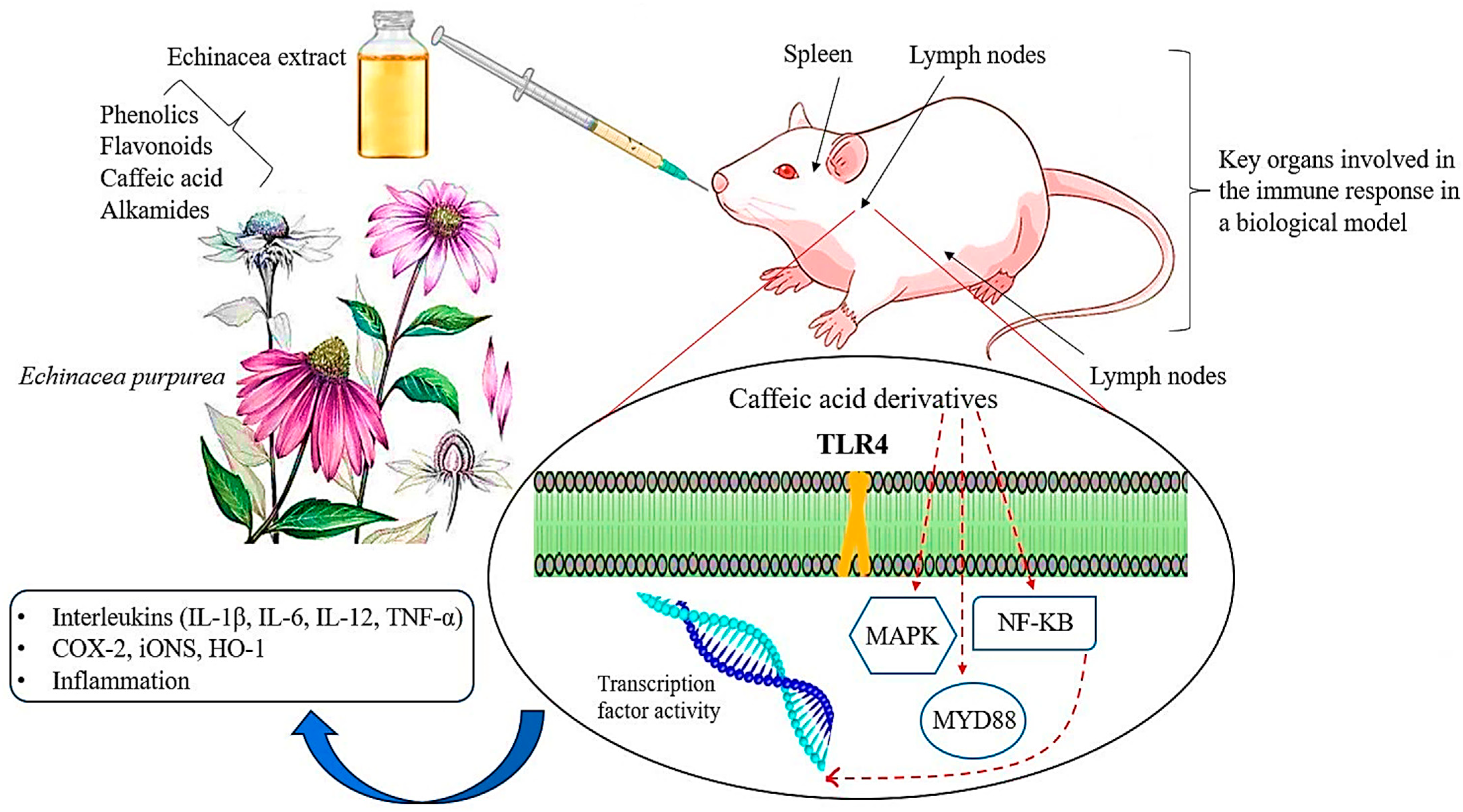
3.4. Polysaccharides
3.5. Caffeic Acid Derivatives (CADs)
4. Antibacterial Activities of Echinacea Species
5. Mechanism of Antibacterial Activity of Polyphenols
5.1. Reactions with Proteins
5.2. Inhibition of Bacterial DNA Synthesis and Interaction with Nucleic Acids
5.3. Interaction with the Bacterial Cell Wall or Inhibition of Cell Wall Formation
5.4. Alteration of Cytoplasmic Membrane Function
6. Antiviral Activities of Echinacea Species
7. Mechanism of Antiviral Activity of Polyphenols
7.1. Inhibition of Virus Entry
7.2. Inhibition of Viral Replication
7.3. Modulation of Host Immune Response
7.4. Antioxidant and Anti-Inflammatory Effects
7.5. Inhibition of Virus Release
8. Immunomodulatory Activity
9. Conclusions and Future Perspective on Echinacea Research
Funding
Data Availability Statement
Conflicts of Interest
References
- Ahmadi, F.; Kariman, K.; Mousavi, M.; Rengel, Z. Echinacea: Bioactive compounds and agronomy. Plants 2024, 13, 1235. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Zhu, H.; Hu, B.; Cheng, Y.; Guo, Y.; Yao, W.; Qian, H. Echinacea in hepatopathy: A review of its phytochemistry, pharmacology, and safety. Phytomedicine 2021, 87, 153572. [Google Scholar] [CrossRef] [PubMed]
- Kligler, B. Echinacea. Am. Fam. Physician 2003, 67, 77–80. [Google Scholar] [PubMed]
- Manayi, A.; Vazirian, M.; Saeidnia, S. Echinacea purpurea: Pharmacology, phytochemistry and analysis methods. Pharmacogn. Rev. 2015, 9, 63. [Google Scholar]
- Karg, C.A.; Wang, P.; Vollmar, A.M.; Moser, S. Re-opening the stage for Echinacea research-Characterization of phylloxanthobilins as a novel anti-oxidative compound class in Echinacea purpurea. Phytomedicine 2019, 60, 152969. [Google Scholar] [CrossRef] [PubMed]
- Miroshina, T.; Poznyakovskiy, V. Echinacea purpurea as a medicinal plant: Characteristics, use as a biologically active component of feed additives and specialized foods. E3S Web Conf. 2023, 380, 01005. [Google Scholar] [CrossRef]
- Ng, J.Y.; Chiong, J.D.; Liu, M.Y.M.; Pang, K.K. Characteristics of the Echinacea spp. research literature: A bibliometric analysis. Eur. J. Integr. Med. 2023, 57, 102216. [Google Scholar] [CrossRef]
- Hanifah, W.N.; Yunus, A.; Widiyastuti, Y. Morphological, agronomic characteristics, and flavonoid content of Echinacea purpurea at various gamma ray doses. Bulg. J. Agric. Sci. 2024, 30, 451. [Google Scholar]
- Freeman, C.; Spelman, K. A critical evaluation of drug interactions with Echinacea spp. Mol. Nut. Food Res. 2008, 52, 789–798. [Google Scholar] [CrossRef]
- Kakouri, E.; Talebi, M.; Tarantilis, P.A. Echinacea spp.: The cold-fighter herbal remedy? Pharmacol. Res.-Mod. Chin. Med. 2024, 10, 100397. [Google Scholar] [CrossRef]
- Saema, S.; Shaheen, N.; Pandey, V. Immunostimulatory properties of Echinacea purpurea and conservation strategy. In Plants for Immunity and Conservation Strategies; Springer Nature: Singapore, 2023; pp. 153–168. [Google Scholar]
- Petrova, A.; Ognyanov, M.; Petkova, N.; Denev, P. Phytochemical characterization of purple coneflower roots (Echinacea purpurea (L.) Moench.) and their extracts. Molecules 2023, 28, 3956. [Google Scholar] [CrossRef]
- İduğ, T. Herbal food supplements usage awareness of university students: Example of Echinacea and St. John’s Wort. Int. J. Agric. Environ. Food Sci. 2023, 7, 792–797. [Google Scholar] [CrossRef]
- Toselli, F.; Matthias, A.; Gillam, E.M. Echinacea metabolism and drug interactions: The case for standardization of a complementary medicine. Life Sci. 2009, 85, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.; Jenks, A.; Brinckmann, J. Echinacea purpurea. HerbalGram 2023, 138, 13569. [Google Scholar]
- Shahrajabian, M.H.; Sun, W. Seed biology and pharmacological benefits of fennel, lavender, thyme, and echinacea Species. Seeds 2023, 2, 290–308. [Google Scholar] [CrossRef]
- Kesar, V.; Ahmad, J.; Odin, J.; Kesar, V. Echinacea-induced acute hepatitis transitioning to autoimmune hepatitis. J. Am. Coll. Gastroenterol. ACG 2015, 110, S397. [Google Scholar] [CrossRef]
- Missenda, M.; Morris, D.; Nault, D. Herbal supplement Use for evidence-based indications in US aadults: An analysis of national survey data. J. Integr. Complement. Med. 2023, 29, 584–591. [Google Scholar] [CrossRef]
- Ghutke, T.D.; Parvin, K.; Rashida Banu, A.M.; Bansal, S.; Srivastava, A.; Rout, S.; Ramzan, U. A comprehensive review on the therapeutic properties of medicinal plants. Acta Tradit. Med. 2023, V2i01, 13–18. [Google Scholar]
- Chaughule, R.S.; Barve, R.S. Role of herbal medicines in the treatment of infectious diseases. Vegetos 2024, 37, 41–51. [Google Scholar] [CrossRef]
- Imtiaz, I.; Schloss, J.; Bugarcic, A. Traditional and contemporary herbal medicines in management of cancer: A scoping review. J. Ayurveda Integr. Med. 2024, 15, 100904. [Google Scholar] [CrossRef]
- Ahmadi, F.; Samadi, A.; Sepehr, E.; Rahimi, A.; Shabala, S. Morphological, phytochemical, and essential oil changes induced by different nitrogen supply forms and salinity stress in Echinacea purpurea L. Biocatal. Agric. Biotechnol. 2022, 43, 13932. [Google Scholar] [CrossRef]
- Ahmadi, F.; Samadi, A.; Rahimi, A. Improving morphological properties and phytochemical compounds of Echinacea purpurea (L.) medicinal plant using novel nitrogen slow-release fertilizer under greenhouse conditions. Sci. Rep. 2020, 10, 13842. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, F.; Samadi, A.; Sepehr, E.; Rahimi, A.; Shabala, S. Perlite particle size and NO3−/NH4+ ratio affect the growth and chemical composition of purple coneflower (Echinacea purpurea L.) in hydroponics. Ind. Crops Prod. 2021, 162, 113285. [Google Scholar] [CrossRef]
- Micheli, L.; Maggini, V.; Ciampi, C.; Gallo, E.; Bogani, P.; Fani, R.; Firenzuoli, F. Echinacea purpurea against neuropathic pain: Alkamides versus polyphenols efficacy. Phytother. Res. 2023, 37, 1911–1923. [Google Scholar] [CrossRef] [PubMed]
- Vieira, S.F.; Fonseca-Rodrigues, D.; Mendanha, D.; Castro, V.I.B.; Pires, R.A.; Reis, R.L.; Pinto-Ribeiro, F. Echinacea purpurea roots extracts. Plant-Deriv. Bioact. Compd. Inflamm. Dis. 2023, 447, 56–63. [Google Scholar]
- AghaAlikhani, M.; Iranpour, A.; Naghdi Badi, H. Changes in agronomical and phytochemical yield of purple coneflower (Echinacea purpurea (L.) moench) under urea and three biofertilizers application. J. Med. Plants 2013, 12, 121–136. [Google Scholar]
- Chopra, H.; Bibi, S.; Gupta, S.K.; Hasan, M.M.; Zeb, M.A.; Khan, M.S.; Yousafi, Q. Alkamides as metabolites in plants. In Strigolactones, Alkamides and Karrikins in Plants; CRC Press: Boca Raton, FL, USA, 2023; pp. 177–193. [Google Scholar]
- Cai, F.; Wang, C. Comprehensive review of the phytochemistry, pharmacology, pharmacokinetics, and toxicology of alkamides (2016–2022). Phytochemistry 2024, 220, 114006. [Google Scholar] [CrossRef]
- Lee, S.K.; Lee, D.R.; Kim, H.L.; Choi, B.K.; Kwon, K.B. A randomized, double-blind, placebo-controlled study on immune improvement effects of ethanolic extract of Echinacea purpurea (L.) Moench in Korean adults. Phytother. Res. 2024, 5, 38–45. [Google Scholar] [CrossRef]
- Jose, A.; Karthika, C.; Athira, K.V.; Rahman, M.H.; Sweilam, S.H. Pharmacological potential of plant-derived alkylamides. In Strigolactones, Alkamides and Karrikins in Plants; CRC Press: Boca Raton, FL, USA, 2023; pp. 195–205. [Google Scholar]
- Wang, W.; Jiang, S.; Zhao, Y.; Zhu, G. Echinacoside: A promising active natural products and pharmacological agents. Pharmacol. Res. 2023, 197, 106951. [Google Scholar] [CrossRef]
- Vergun, O.; Svydenko, L.; Shymanska, O.; Hlushchenko, L.; Sedlačková, V.H.; Ivanišová, E.; Brindza, J. Accumulation of total content of polyphenol compounds and antioxidant activity of Echinacea moench species. Agrobiodivers. Improv. Nutr. Health Life Qual. 2024, 8, 63–71. [Google Scholar] [CrossRef]
- Karadağ, A.E.; Baydar, R.; Kırcı, D. Phytochemical quality analysis of commercial preparations containing Echinacea purpurea. Eur. J. Life Sci. 2024, 3, 45–54. [Google Scholar] [CrossRef]
- Choirunnisa, J.P.; Widiyastuti, Y.; Sakya, A.T.; Yunus, A. Morphological characteristics and flavonoid accumulation of Echinacea purpurea cultivated at various salinity. Biodiversitas: J. Biol. Divers. 2021, 22, 156–163. [Google Scholar] [CrossRef]
- Clifford, L.J.; Nair, M.G.; Rana, J.; Dewitt, D.L. Bioactivity of alkamides isolated from Echinacea purpurea (L.) Moench. Phytomedicine 2002, 9, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Coelho, J.; Barros, L.; Dias, M.I.; Finimundy, T.C.; Amaral, J.S.; Alves, M.J.; Ferreira, I.C. Echinacea purpurea (L.) Moench: Chemical characterization and bioactivity of its extracts and fractions. Pharmaceuticals 2020, 13, 125. [Google Scholar] [CrossRef] [PubMed]
- Dennehy, C. Need for additional, specific information in studies with Echinacea. Antimicrob. Agents Chemother. 2001, 45, 369–370. [Google Scholar] [CrossRef]
- Soltanbeigi, A.; Maral, H. Agronomic yield and essential oil properties of purple coneflower (Echinacea purpurea L. Moench) with different nutrient applications. Chil. J. Agric. Anim. Sci. 2022, 38, 164–175. [Google Scholar] [CrossRef]
- Maggini, V.; Bandeira Reidel, R.V.; De Leo, M.; Mengoni, A.; Rosaria Gallo, E.; Miceli, E.; Pistelli, L. Volatile profile of Echinacea purpurea plants after in vitro endophyte infection. Nat. Prod. Res. 2020, 34, 2232–2237. [Google Scholar] [CrossRef]
- Rousseaux, C.G. Herbal remedies. In Haschek and Rousseaux’s Handbook of Toxicologic Pathology; Academic Press: Cambridge, MA, USA, 2023; pp. 183–303. [Google Scholar]
- Pretorius, T.R.; Charest, C.; Kimpe, L.E.; Blais, J.M. The accumulation of metals, PAHs, and alkyl PAHs in the roots of Echinacea purpurea. PLoS ONE 2018, 13, e0208325. [Google Scholar] [CrossRef]
- Harborne, J.B.; Williams, C.A. Phytochemistry of the genus Echinacea. In Echinacea; CRC Press: Boca Raton, FL, USA, 2004; pp. 71–88. [Google Scholar]
- Mirjalili, M.H.; Salehi, P.; Badi, H.N.; Sonboli, A. Volatile constituents of the flowerheads of three Echinacea species cultivated in Iran. Flavour Fragr. J. 2006, 21, 355–358. [Google Scholar] [CrossRef]
- Woelkart, K.; Xu, W.; Pei, Y.; Makriyannis, A.; Picone, R.P.; Bauer, R. The endocannabinoid system as a target for alkamides from Echinacea angustifolia roots. Planta Medica 2005, 71, 701–705. [Google Scholar] [CrossRef]
- Perry, N.B.; Wills, R.B.; Stuart, D.L. Factors affecting echinacea quality: Agronomy and processing. In Echinacea; CRC Press: Boca Raton, FL, USA, 2004; pp. 127–142. [Google Scholar]
- Cozzolino, R.; Malvagna, P.; Spina, E.; Giori, A.; Fuzzati, N.; Anelli, A.; Impallomeni, G. Structural analysis of the polysaccharides from Echinacea angustifolia radix. Carbohydr. Polym. 2006, 65, 263–272. [Google Scholar] [CrossRef]
- Bone, K. Echinacea: What makes it work. Altern. Med. Rev. 1997, 2, 87–93. [Google Scholar]
- Melchart, D.; Clemm, C.; Weber, B.; Draczynski, T.; Worku, F.; Linde, K.; Saller, R. Polysaccharides isolated from Echinacea purpurea herba cell cultures to counteract undesired effects of chemotherapy—A pilot study. Phytother. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2002, 16, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.T.; Huang, C.C.; Shieh, X.H.; Chen, C.L.; Chen, L.J.; Yu, B.I. Flavonoid, phenol and polysaccharide contents of Echinacea purpurea L. and its immunostimulant capacity in vitro. Int. J. Environ. Sci. Dev. 2010, 1, 5. [Google Scholar] [CrossRef]
- Li, Q.; Yang, F.; Hou, R.; Huang, T.; Hao, Z. Post-screening characterization of an acidic polysaccharide from Echinacea purpurea with potent anti-inflammatory properties in vivo. Food Funct. 2020, 11, 7576–7583. [Google Scholar] [CrossRef]
- Roesler, J.; Steinmüller, C.; Kiderlen, A.; Emmendörffer, A.; Wagner, H.; Lohmann-Matthes, M.L. Application of purified polysaccharides from cell cultures of the plant Echinacea purpurea to mice mediates protection against systemic infections with Listeria monocytogenes and Candida albicans. Int. J. Immunopharmacol. 1991, 13, 27–37. [Google Scholar] [CrossRef]
- Raso, G.M.; Pacilio, M.; Di Carlo, G.; Esposito, E.; Pinto, L.; Meli, R. In-vivo and in-vitro anti-inflammatory effect of Echinacea purpurea and Hypericum perforatum. J. Pharm Pharmacol. 2002, 54, 1379–1383. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Shi, Q.; Zhang, Y.; Gao, G.; Shen, P.; Gao, G.; Wu, N. Effects of Echinacea purpurea polysaccharide on IEC-6 cell proliferation. Agric. Sci. Technol. 2014, 15, 1876. [Google Scholar]
- Schöllhorn, C.; Schecklies, E.; Wagner, H. Immunochemical investigations of polysaccharides from Echinacea purpurea cell suspension cultures. Planta Medica 1993, 59, A662–A663. [Google Scholar] [CrossRef]
- Lee, J. Caffeic acid derivatives in dried Lamiaceae and Echinacea purpurea products. J. Funct. Foods 2010, 2, 158–162. [Google Scholar] [CrossRef]
- Kim, H.O.; Durance, T.D.; Scaman, C.H.; Kitts, D.D. Retention of caffeic acid derivatives in dried Echinacea purpurea. J. Agric. Food Chem. 2000, 48, 4182–4186. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.L.; Chiou, S.Y.; Chan, K.C.; Sung, J.M.; Lin, S.D. Caffeic acid derivatives, total phenols, antioxidant and antimutagenic activities of Echinacea purpurea flower extracts. LWT-Food Sci. Technol. 2012, 46, 169–176. [Google Scholar] [CrossRef]
- Wu, C.H.; Murthy, H.N.; Hahn, E.J.; Lee, H.L.; Paek, K.Y. Efficient extraction of caffeic acid derivatives from adventitious roots of Echinacea purpurea. Czech J. Food Sci. 2008, 26, 254–258. [Google Scholar] [CrossRef]
- Erkoyuncu, M.T.; Yorgancilar, M. Optimization of callus cultures at Echinacea purpurea L. for the amount of caffeic acid derivatives. Electron. J. Biotechnol. 2021, 51, 17–27. [Google Scholar] [CrossRef]
- Rady, M.R.; Aboul-Enein, A.M.; Ibrahim, M.M. Active compounds and biological activity of in vitro cultures of some Echinacea purpurea varieties. Bull. Natl. Res. Cent. 2018, 42, 1–12. [Google Scholar] [CrossRef]
- Paek, K.Y.; Murthy, H.N.; Hahn, E.J. Establishment of adventitious root cultures of Echinacea purpurea for the production of caffeic acid derivatives. Protocols for In Vitro Cult. Second. Metab. Anal. Aromat. Med. Plants 2009, 547, 3–16. [Google Scholar]
- Sharifi-Rad, M.; Mnayer, D.; Morais-Braga, M.F.B.; Carneiro, J.N.P.; Bezerra, C.F.; Coutinho, H.D.M.; Sharifi-Rad, J. Echinacea plants as antioxidant and antibacterial agents: From traditional medicine to biotechnological applications. Phytother. Res. 2018, 32, 1653–1663. [Google Scholar] [CrossRef]
- Chiellini, C.; Maida, I.; Maggini, V.; Bosireeman, E.; Mocali, S.; Emiliani, G.; Fani, R. Preliminary data on antibacterial activity of Echinacea purpurea-associated bacterial communities against Burkholderia cepacia complex strains, opportunistic pathogens of Cystic Fibrosis patients. Microbiol. Res. 2017, 196, 34–43. [Google Scholar] [CrossRef]
- Zaushintsena, A.V.; Milentyeva, I.; Babich, O.; Noskova, S.Y.; Kiseleva, T.F.; Popova, D.G.; Lukin, A. Quantitative and qualitative profile of biologically active substances extracted from purple echinacea (Echinacea purpurea L.) growing in the Kemerovo region: Functional foods application. Foods Raw Mater. 2019, 7, 84–92. [Google Scholar] [CrossRef]
- Burlou-Nagy, C.; Bănică, F.; Negrean, R.A.; Jurca, T.; Vicaș, L.G.; Marian, E.; Pallag, A. Determination of the bioactive compounds from Echinacea purpurea (L.) Moench leaves extracts in correlation with the antimicrobial activity and the in vitro wound healing potential. Molecules 2023, 28, 5711. [Google Scholar] [CrossRef]
- Barnes, J.; Anderson, L.A.; Gibbons, S.; Phillipson, J.D. Echinacea species (Echinacea angustifolia (DC.) Hell., Echinacea pallida (Nutt.) Nutt., Echinacea purpurea (L.) Moench): A review of their chemistry, pharmacology and clinical properties. J. Pharm. Pharmacol. 2005, 57, 929–954. [Google Scholar] [CrossRef] [PubMed]
- Aksoy, H.; Arslanoglu, S.; Edbeib, M.; Kaya, Y.; Marakli, S. Antibacterial activity of Calendula officinalis and Echinacea purpurea extracts against the causal agent of tomatoes’ bacterial canker: Clavibacter michiganensis subsp. michiganensis. Boletín Latinoam. Y Del Caribe De Plantas Med. Y Aromáticas 2021, 20, 496–502. [Google Scholar] [CrossRef]
- Daley, E. A Phytochemical and Antibacterial Analysis of Echinacea purpurea (L.) Moench throughout Seasonal Development. Doctoral Dissertation, Université d’Ottawa/University of Ottawa, Ottawa, ON, Canada, 2019. [Google Scholar]
- Taghizadeh, M.; Jarvandi, S.; Yasa, N. A review of Echinacea. J. Med. Plants. 2002, 1, 13–26. [Google Scholar]
- VAVERKOVÁ, L.B.P.O.Š. Antimicrobial and antimutagenic activities of extracts from different organs of Echinacea angustifolia DC (Asteraceae). J. Food Nutr. Res. 2012, 51, 201–206. [Google Scholar]
- Zazharskyi, V.V.; Davydenko, P.; Kulishenko, O.; Borovik, I.V.; Brygadyrenko, V.V. Antimicrobial activity of 50 plant extracts. Biosyst. Divers. 2019, 27, 163–169. [Google Scholar] [CrossRef]
- Kerem, S.; Özbek, Ö. Antimicrobial activities of some species in Asteraceae and Lamiaceae families from Türkiye. Int. J. Second. Metab. 2024, 11, 277–291. [Google Scholar] [CrossRef]
- Gotti, R.; Pomponio, R.; Bertucci, C.; Cavrini, V. Simultaneous analysis of the lipophilic and hydrophilic markers of Echinacea plant extracts by capillary electrophoresis. J. Separation Sci. 2002, 25, 1079–1086. [Google Scholar] [CrossRef]
- Sharma, S.M.; Anderson, M.; Schoop, S.R.; Hudson, J.B. Bactericidal and anti-inflammatory properties of a standardized Echinacea extract (Echinaforce®): Dual actions against respiratory bacteria. Phytomedicine 2010, 17, 563–568. [Google Scholar] [CrossRef]
- Garzoli, S.; Maggio, F.; Vinciguerra, V.; Rossi, C.; Donadu, M.G.; Serio, A. Chemical Characterization and Antimicrobial Properties of the Hydroalcoholic Solution of Echinacea purpurea (L.) Moench. and Propolis from Northern Italy. Molecules 2023, 28, 1380. [Google Scholar] [CrossRef]
- Rehman, F.; Sudhaker, M.; Roshan, S.; Khan, A. Antibacterial activity of Eachinacia angustfolia. Pharmacogn. J. 2012, 4, 67–70. [Google Scholar] [CrossRef]
- Giles, J.T.; Palat III, C.T.; Chien, S.H.; Chang, Z.G.; Kennedy, D.T. Evaluation of echinacea for treatment of the common cold. Pharmacotherapy: J. Hum. Pharmacol. Drug Ther. 2000, 20, 690–697. [Google Scholar] [CrossRef] [PubMed]
- Currier, N.L.; Miller, S.C. Echinacea purpurea and melatonin augment natural-killer cells in leukemic mice and prolong life span. J. Altern. Complement. Med. 2001, 7, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Hobbs, C. The Echinacea Handbook; Eclectic Medical Publications: Portland, OR, USA, 1989. [Google Scholar]
- Islam, J.; Carter, R. Use of Echinacea in upper respiratory tract infection. South Med. J. 2005, 98, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Jukić, H.; Habeš, S.; Aldžić, A.; Durgo, K.; Kosalec, I. Antioxidant and prooxidant activities of phenolic compounds of the extracts of Echinacea purpurea (L.). Bull. Chem. Technol. Bosnia Herzeg. 2015, 44, 43–52. [Google Scholar]
- Lee, M.; Lin, W.; Yu, B.; Lee, T. Antioxidant capacity of phytochemicals and their potential effects on oxidative status in animals—A review. Asian-Australas. J. Anim. Sci. 2017, 30, 299–308. [Google Scholar] [CrossRef]
- Yamada, K.; Hung, P.; Park, T.K.; Park, P.J.; Lim, B.O. A comparison of the immunostimulatory effects of the medicinal herbs Echinacea, Ashwagandha and Brahmi. J. Ethnopharmacol. 2011, 137, 231–235. [Google Scholar] [CrossRef]
- Tan, B.K.; Vanitha, J. Immunomodulatory and antimicrobial effects of some traditional Chinese medicinal herbs: A review. Curr. Med. Chem. 2004, 11, 1423–1430. [Google Scholar] [CrossRef]
- Sabouri, Z.; Barzegar, M.; Sahari, M.; Naghdi Badi, H. Antioxidant and antimicrobial potential of Echinacea purpurea extract and its effect on extension of cake shelf life. J. Med. Plants 2012, 3, 28–40. [Google Scholar]
- Pellati, F.; Benvenuti, S.; Magro, L.; Melegari, M.; Soragni, F. Analysis of phenolic compounds and radical scavenging activity of Echinacea spp. J. Pharm. Biomed. Anal. 2004, 35, 289–301. [Google Scholar] [CrossRef]
- Pellati, F.; Benvenuti, S.; Melegari, M.; Lasseigne, T. Variability in the composition of anti-oxidant compounds in Echinacea species by HPLC. Phytochem. Anal. 2005, 16, 77–85. [Google Scholar] [CrossRef]
- Hudson, J.B. Applications of the phytomedicine Echinacea purpurea (Purple Coneflower) in infectious diseases. BioMed Res. Int. 2012, 2012, 769896. [Google Scholar]
- Cruz, I.; Cheetham, J.J.; Arnason, J.T.; Yack, J.E.; Smith, M.L. Alkamides from Echinacea disrupt the fungal cell wall-membrane complex. Phytomedicine 2014, 21, 435–442. [Google Scholar] [CrossRef]
- Birt, D.F.; Widrlechner, M.P.; LaLone, C.A.; Wu, L.; Bae, J.; Solco, A.K.; Price, J.P. Echinacea in infection. Am. J. Clin. Nutr. 2008, 87, 488S–492S. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, A.M.; Laba, J.G.; Moore, J.A.; Lee, T.D. Echinacea-induced macrophage activation. Immunopharmacol. Immunotoxicol. 2008, 30, 553–574. [Google Scholar] [CrossRef] [PubMed]
- Tierra, M. Echinacea: An effective alternative to antibiotics. J. Herb. Pharmacother. 2008, 7, 79–89. [Google Scholar] [CrossRef]
- Bałan, B.J.; Sokolnicka, I.; SkopińSka-różEwSka, E.; Skopiński, P. The modulatory influence of some Echinacea-based remedies on antibody production and cellular immunity in mice. Central Eur. J. Immu. 2016, 41, 12–18. [Google Scholar] [CrossRef]
- Classen, B. Characterization of an arabinogalactan-protein from suspension culture of Echinacea purpurea. Plant Cell Tissue Organ Cult. 2007, 88, 267–275. [Google Scholar] [CrossRef]
- Balciunaite, G.; Juodsnukyte, J.; Savickas, A.; Ragazinskiene, O.; Siatkute, L.; Zvirblyte, G.; Savickiene, N. Fractionation and evaluation of proteins in roots of Echinacea purpurea (L.) Moench. Acta Pharm. 2015, 65, 473–479. [Google Scholar] [CrossRef]
- Bossy, A.; Blaschek, W.; Classen, B. Characterization and immunolocalization of arabinogalactan-proteins in roots of Echinacea Purpurea. Planta Medica 2009, 75, 1526–1533. [Google Scholar] [CrossRef]
- Gallo, M.; Ferracane, R.; Naviglio, D. Antioxidant addition to prevent lipid and protein oxidation in chicken meat mixed with supercritical extracts of Echinacea angustifolia. J. Supercrit. Fluids 2012, 72, 198–204. [Google Scholar] [CrossRef]
- Lim, H.S.; Sohn, E.; Kim, Y.J.; Kim, B.Y.; Kim, J.H.; Jeong, S.J. Ethanol Extract of Elaeagnus glabra f. oxyphylla Branches Alleviates the Inflammatory Response Through Suppression of Cyclin D3/Cyclin-Dependent Kinase 11p58 Coupled to Lipopolysaccharide-Activated BV-2 Microglia. Nat. Prod. Commun. 2022, 17. [Google Scholar] [CrossRef]
- Haron, M.H.; Tyler, H.L.; Pugh, N.D.; Moraes, R.M.; Maddox, V.L.; Jackson, C.R.; Pasco, D.S. Activities and prevalence of Proteobacteria members colonizing Echinacea purpurea fully account for macrophage activation exhibited by extracts of this botanical. Planta Medica 2016, 82, 1258–1265. [Google Scholar] [CrossRef] [PubMed]
- Maggini, V.; Miceli, E.; Fagorzi, C.; Maida, I.; Fondi, M.; Perrin, E.; Fani, R. Antagonism and antibiotic resistance drive a species-specific plant microbiota differentiation in Echinacea spp. FEMS Microbiol. Ecol. 2018, 94, fiy118. [Google Scholar] [CrossRef] [PubMed]
- Vaou, N.; Stavropoulou, E.; Voidarou, C.; Tsigalou, C.; Bezirtzoglou, E. Towards advances in medicinal plant antimicrobial activity: A review study on challenges and future perspectives. Microorganisms 2021, 9, 2041. [Google Scholar] [CrossRef] [PubMed]
- Mir-Rashed, N.; Cruz, I.; Jessulat, M.; Dumontier, M.; Chesnais, C.; Juliana, N.G.; Smith, M.L. Disruption of the fungal cell wall by antifungal Echinacea extracts. Med. Mycol. 2010, 48, 949–958. [Google Scholar] [CrossRef]
- Spelman, K. The extraction, stability, metabolism, and bioactivity of the alkylamides in Echinacea spp. Microbiology 2009, 3, 534–540. [Google Scholar]
- Luettig, B.; Steinmüller, C.; Gifford, G.E.; Wagner, H.; Lohmann-Matthes, M.L. Macrophage activation by the polysaccharide arabinogalactan isolated from plant cell cultures of Echinacea purpurea. JNCI J. Natl. Cancer Inst. 1989, 81, 669–675. [Google Scholar] [CrossRef]
- Chicca, A.; Pellati, F.; Adinolfi, B.; Matthias, A.; Massarelli, I.; Benvenuti, S.; Nieri, P. Cytotoxic activity of polyacetylenes and polyenes isolated from roots of Echinacea pallida. Br. J. Pharmacol. 2008, 153, 879–885. [Google Scholar] [CrossRef]
- Sestáková, H.; Turek, B. Effect of Echinacea on cells involved in disease defense. In Echinacea; CRC Press: Boca Raton, FL, USA, 2004; pp. 179–184. [Google Scholar]
- Kindscher, K. (Ed.) Echinacea: Herbal Medicine with a Wild History; Springer: Cham, Switzerland, 2016. [Google Scholar]
- Qu, L.; Chen, Y.; Wang, X.; Scalzo, R.; Davis, J.M. Patterns of variation in alkamides and cichoric acid in roots and aboveground parts of Echinacea purpurea (L.) Moench. HortScience 2005, 40, 1239. [Google Scholar] [CrossRef]
- Senchina, D.S.; Martin, A.E.; Buss, J.E.; Kohut, M.L. Effects of Echinacea extracts on macrophage antiviral activities. Phytother. Res. 2010, 24, 810–816. [Google Scholar] [CrossRef] [PubMed]
- Vimalanathan, S.; Kang, L.; Amiguet, V.T.; Livesey, J.; Arnason, J.T.; Hudson, J. Echinacea purpurea. aerial parts contain multiple antiviral compounds. Pharm. Biol. 2005, 43, 740–745. [Google Scholar] [CrossRef]
- Wu, L.; Bae, J.; Kraus, G.; Wurtele, E.S. Diacetylenic isobutylamides of Echinacea: Synthesis and natural distribution. Phytochemistry 2004, 65, 2477–2484. [Google Scholar] [CrossRef] [PubMed]
- Signer, J.; Jonsdottir, H.R.; Albrich, W.C.; Strasser, M.; Züst, R.; Ryter, S.; Engler, O.B. In vitro virucidal activity of Echinaforce®, an Echinacea purpurea preparation, against coronaviruses, including common cold coronavirus 229E and SARS-CoV-2. Virol. J. 2020, 17, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Mistrikova, I.; Vaverkova, S. Echinacea—Chemical composition, immunostimulatory activities and uses. Thaiszia J. Bot. 2006, 16, 11–26. [Google Scholar]
- Farahani, M. Inhibition of HSV-1 multiplication by five species of medicinal plants. J. Microbiol. Biotechnol. Food Sci. 2013, 3, 69–71. [Google Scholar]
- De Oliveira, J.R.; Antunes, B.S.; do Nascimento, G.O.; Kawall, J.C.D.S.; Oliveira, J.V.B.; Silva, K.G.D.S.; Oliveira, C.R. Antiviral activity of medicinal plant-derived products against SARS-CoV-2. Exp. Biol. Med. 2022, 247, 1797–1809. [Google Scholar] [CrossRef]
- Percaccio, E.; De Angelis, M.; Acquaviva, A.; Nicotra, G.; Ferrante, C.; Mazzanti, G.; Di Sotto, A. ECHOPvir: A Mixture of Echinacea and hop extracts endowed with cytoprotective, immunomodulatory and antiviral properties. Nutrients 2023, 15, 4380. [Google Scholar] [CrossRef] [PubMed]
- Awang, D.V. Immune stimulants and antiviral botanicals: Echinacea and ginseng. Perspectives on new crops and new uses. ASHS Press Alex. 1999, 5, 450–456. [Google Scholar]
- Bergner, P. Antiviral botanicals in herbal medicine. Med. Herbal. 2005, 14, 1–12. [Google Scholar]
- Bruni, R.; Brighenti, V.; Caesar, L.K.; Bertelli, D.; Cech, N.B.; Pellati, F. Analytical methods for the study of bioactive compounds from medicinally used Echinacea species. J. Pharm. Biomed. Anal. 2018, 160, 443–477. [Google Scholar] [CrossRef]
- Aucoin, M.; Cooley, K.; Saunders, P.R.; Carè, J.; Anheyer, D.; Medina, D.N.; Garber, A. The effect of Echinacea spp. on the prevention or treatment of COVID-19 and other respiratory tract infections in humans: A rapid review. Adv. Int. Med. 2020, 7, 203. [Google Scholar] [CrossRef] [PubMed]
- Novika, R.G.; Wahidah, N.J.; Yunus, A.; Sumarno, L.; Ilyas, M.F. Clinical effect of Echinacea purpurea as an antiviral and its effect on reproductive hormones. J. Pharm. Pharmacogn. Res. 2024, 12, 255–263. [Google Scholar] [CrossRef]
- Sun, Y.; Li, C.; Liu, Z.; Zeng, W.; Ahmad, M.J.; Zhang, M.; He, Q. Chinese herbal extracts with antiviral activity: Evaluation, mechanisms, and potential for preventing PRV, PEDV and PRRSV infections. Anim. Dis. 2023, 3, 35. [Google Scholar] [CrossRef]
- Turner, R.B.; Bauer, R.; Woelkart, K.; Hulsey, T.C.; Gangemi, J.D. An evaluation of Echinacea angustifolia in experimental rhinovirus infections. N. Engl. J. Med. 2005, 353, 341–348. [Google Scholar] [CrossRef]
- Gakhar, A. Anti-viral phyto medicine: A review. J. Pharmacogn. Phytochem. 2021, 10, 2002–2004. [Google Scholar] [CrossRef]
- Kindscher, K. Ethnobotany of purple coneflower (Echinacea angustifolia, Asteraceae) and other Echinacea species. Econ. Bot. 1989, 43, 498–507. [Google Scholar] [CrossRef]
- Naithani, R.; Mehta, R.G.; Shukla, D.; Chandersekera, S.N.; Moriarty, R.M. Antiviral activity of phytochemicals: A current perspective. In Dietary Components and Immune Function; Humana Press: Totowa, NJ, USA, 2010; pp. 421–468. [Google Scholar]
- Lelešius, R.; Karpovaitė, A.; Mickienė, R.; Drevinskas, T.; Tiso, N.; Ragažinskienė, O.; Šalomskas, A. In vitro antiviral activity of fifteen plant extracts against avian infectious bronchitis virus. BMC Vet. Res. 2019, 15, 1–10. [Google Scholar] [CrossRef]
- Vimalanathan, S.; Shehata, M.; Sadasivam, K.; Delbue, S.; Dolci, M.; Pariani, E.; D’Alessandro, S.; Pleschka, S. Broad antiviral effects of Echinacea purpurea against SARS-CoV-2 variants of concern and potential mechanism of action. Microorganisms 2022, 10, 2145. [Google Scholar] [CrossRef]
- LaLone, C.A.; Hammer, K.D.; Wu, L.; Bae, J.; Leyva, N.; Liu, Y.; Birt, D.F. Echinacea species and alkamides inhibit prostaglandin E2 production in RAW264. 7 mouse macrophage cells. J. Agric. Food Chem. 2007, 55, 7314–7322. [Google Scholar] [CrossRef]
- Foster, S. Herbal Remedies: Echinacea: The Cold and Flu Remedy. Alter Compl Therapies. 1995, 1, 254–257. [Google Scholar] [CrossRef]
- Ogal, M.; Johnston, S.L.; Klein, P.; Schoop, R. Echinacea reduces antibiotic usage in children through respiratory tract infection prevention: A randomized, blinded, controlled clinical trial. Eur. J. Med. Res. 2021, 26, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ghio, S.; Brincat, J.P.; Cetin, Y.; Lia, F. Antiviral activity of natural compounds extracted from Mediterranean medicinal plants against SARS-CoV-2. Acad. Biol. 2024, 2, 41–49. [Google Scholar] [CrossRef]
- Nicolussi, S.; Ardjomand-Woelkart, K.; Stange, R.; Gancitano, G.; Klein, P.; Ogal, M. Echinacea as a potential force against coronavirus infections? A mini-review of randomized controlled trials in adults and children. Microorganisms 2022, 10, 211. [Google Scholar] [CrossRef]
- Mohamadi, N.; Sharififar, F.; Rameshk, M.; Khandani, S.K. A Global Perspective on Medicinal Plants and Phytochemicals with Antiviral Potentials in the Respiratory System. Anti-Infect. Agents 2023, 21, 56–78. [Google Scholar] [CrossRef]
- Hassan, S.T.; Masarčíková, R.; Berchová, K. Bioactive natural products with anti-herpes simplex virus properties. J. Pharm. Pharmacol. 2015, 67, 1325–1336. [Google Scholar] [CrossRef]
- Wagner, L.; Cramer, H.; Klose, P.; Lauche, R.; Gass, F.; Dobos, G.; Langhorst, J. Herbal medicine for cough: A systematic review and meta-analysis. Forsch. Komplementärmedizin/Res. Complement. Med. 2015, 22, 359–368. [Google Scholar] [CrossRef]
- Sadeek, A.; Abdallah, E. Medicinal Plants with Antiviral Properties to Tackle Covid-19 Pandemic: A Short-Review. Antivirals 2021, 2, 122–127. [Google Scholar]
- Wu, Y.H.; Chen, Y.; Zhuang, A.Q.; Chen, S.M. Natural Phenolic Acids and Their Derivatives against Human Viral Infections; InTechOpen: Rijeka, Croatia, 2023. [Google Scholar]
- Saifulazmi, N.F.; Rohani, E.R.; Harun, S.; Bunawan, H.; Hamezah, H.S.; Nor Muhammad, N.A.; Sarian, M.N. A review with updated perspectives on the antiviral potentials of traditional medicinal plants and their prospects in antiviral therapy. Life 2022, 12, 1287. [Google Scholar] [CrossRef]
- Hudson, J.; Vimalanathan, S.; Kang, L.; Amiguet, V.T.; Livesey, J.; Arnason, J.T. Characterization of antiviral activities in Echinacea. Root preparations. Pharm. Biol. 2005, 43, 790–796. [Google Scholar] [CrossRef]
- Venu, L.N.; Austin, A. Antiviral efficacy of medicinal plants against respiratory viruses: Respiratory Syncytial Virus (RSV) and Coronavirus (CoV)/COVID 19. J. Pharmacol. 2020, 9, 281–290. [Google Scholar] [CrossRef]
- Ghaemi, A.; Soleimanjahi, H.; Farshbaf Moghaddam, M.; Yazdani, N. Evaluation of antiviral activity of aerial part of Echinacea purpurea extract against herpes. Hakim Res. J. 2007, 9, 59–64. [Google Scholar]
- Khan, F.; Bamunuarachchi, N.I.; Tabassum, N.; Kim, Y.M. Caffeic acid and its derivatives: Antimicrobial drugs toward microbial pathogens. J. Agric. Food Chem. 2021, 69, 2979–3004. [Google Scholar] [CrossRef] [PubMed]
- Ghaemi, A.; Soleimanjahi, H.; Gill, P.; Arefian, E.; Soudi, S.; Hassan, Z. Echinacea purpurea polysaccharide reduces the latency rate in herpes simplex virus type-1 infections. Intervirology 2009, 52, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Hudson, J.; Vimalanathan, S. Echinacea—A source of potent antivirals for respiratory virus infections. Pharmaceuticals 2011, 4, 1019–1031. [Google Scholar] [CrossRef]
- Vimalanathan, S.; Schoop, R.; Suter, A.; Hudson, J. Prevention of influenza virus-induced bacterial superinfection by standardized Echinacea purpurea, via regulation of surface receptor expression in human bronchial epithelial cells. Virus Res. 2017, 233, 51–59. [Google Scholar] [CrossRef]
- Meeran, M.N.; Javed, H.; Sharma, C.; Goyal, S.N.; Kumar, S.; Jha, N.K.; Ojha, S. Can Echinacea be a potential candidate to target immunity, inflammation, and infection-The trinity of coronavirus disease 2019. Heliyon 2021, 7, 65–72. [Google Scholar]
- Sharma, M.; Anderson, S.A.; Schoop, R.; Hudson, J.B. Induction of multiple pro-inflammatory cytokines by respiratory viruses and reversal by standardized Echinacea, a potent antiviral herbal extract. Antivir. Res. 2009, 83, 165–170. [Google Scholar] [CrossRef]
- Pleschka, S.; Stein, M.; Schoop, R.; Hudson, J.B. Anti-viral properties and mode of action of standardized Echinacea purpurea extract against highly pathogenic avian influenza virus (H5N1, H7N7) and swine-origin H1N1 (S-OIV). Virol. J. 2009, 6, 1–9. [Google Scholar] [CrossRef]
- Farahani, M. Inhibition of HSV-1 multiplication by aqueous extract of Echinacea purpurea root. J. Mashhad Dent. Sch. 2015, 39, 71–80. [Google Scholar]
- Stevenson, L.M.; Matthias, A.; Banbury, L.; Penman, K.G.; Bone, K.M.; Leach, D.; Lehmann, R.P. Modulation of macrophage immune responses by Echinacea. Molecules 2005, 10, 1279–1285. [Google Scholar] [CrossRef]
- Kembuan, G.; Lie, W.; Tumimomor, A. Potential usage of immune modulating supplements of the Echinacea genus for COVID-19 infection. Int. J. Med. Rev. Case Rep 2020, 4, 2020. [Google Scholar]
- Di Sotto, A.; Vitalone, A.; Di Giacomo, S. Plant-derived nutraceuticals and immune system modulation: An evidence-based overview. Vaccines 2020, 8, 468. [Google Scholar] [CrossRef] [PubMed]
- Zhai, Z.; Solco, A.; Wu, L.; Wurtele, E.S.; Kohut, M.L.; Murphy, P.A.; Cunnick, J.E. Echinacea increases arginase activity and has anti-inflammatory properties in RAW 264.7 macrophage cells, indicative of alternative macrophage activation. J. Ethnopharmacol. 2009, 122, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.; Yuan, Y.; Jiang, L.; Tai, Y.; Yang, X.; Hu, F.; Xie, Z. Anti-inflammatory effects of essential oil in Echinacea purpurea L. Pak. J. Pharm. Sci. 2013, 26, 403–408. [Google Scholar]
- Mohammedsaleh, Z.M.; Aljadani, H.M. Echinacea purpurea root extract modulates diabetes-induced renal dysfunction in rats through hypoglycemic, antioxidant, and anti-inflammatory activities. Med. Sci. 2021, 25, 1033–1043. [Google Scholar]
- Dobrange, E.; Peshev, D.; Loedolff, B.; Van den Ende, W. Fructans as immunomodulatory and antiviral agents: The case of Echinacea. Biomolecules 2019, 9, 615. [Google Scholar] [CrossRef]
- Bajrai, L.H.; El-Kafrawy, S.A.; Hassan, A.M.; Tolah, A.M.; Alnahas, R.S.; Sohrab, S.S.; Azhar, E.I. In vitro screening of anti-viral and virucidal effects against SARS-CoV-2 by Hypericum perforatum and Echinacea. Sci. Rep. 2022, 12, 21723. [Google Scholar] [CrossRef]
- Lim, T.K.; Lim, T.K. Echinacea purpurea. Edible Medicinal and Non-Medicinal Plants. Flowers 2014, 7, 340–371. [Google Scholar]
- Melchart, D.; Linde, K.; Worku, F.; Bauer, R.; Wagner, H. Immunomodulation with Echinacea—A systematic review of controlled clinical trials. Phytomedicine 1994, 1, 245–254. [Google Scholar] [CrossRef]
- Oliveira, B.G.D.; Santos, L.F.F.; Costa, M.C.D.; Bastos, R.W.; Carmo, P.H.F.D.; Santos, D.D.A.; César, I.C. Antimicrobial, and immunomodulatory activities of dried extracts of Echinacea Purpurea. Braz. J. Pharm. Sci. 2022, 58, e21026. [Google Scholar] [CrossRef]
- Senchina, D.S.; McCann, D.A.; Asp, J.M.; Johnson, J.A.; Cunnick, J.E.; Kaiser, M.S.; Kohut, M.L. Changes in immunomodulatory properties of Echinacea spp. root infusions and tinctures stored at 4 C for four days. Clin. Chim. Acta 2005, 355, 67–82. [Google Scholar] [CrossRef] [PubMed]
- Bone, K. Echinacea: Quality, uses, and immunomodulating activity from a phytotherapist’s perspective. In Echinacea; CRC Press: Boca Raton, FL, USA, 2004; pp. 219–230. [Google Scholar]
- Mahmoud, S.H.; Mahmoud, R.M.; Ashoush, I.S.; Attia, M.Y. Immunomodulatory and antioxidant activity of pomegranate juice incorporated with spirulina and echinacea extracts sweetened by stevioside. J. Agric. Vet. Sci. (Qassim Univ.) 2015, 8, 161–174. [Google Scholar]
- Ibrahim, A.; Saleh, R.; Hassan, A.; Amer, M. Immunomodulatory effect of Echinacea purpurea and Curcuma longa in rabbits. Mansoura. Vet. Med. J. 2020, 22, 2. [Google Scholar]
- Raduner, S.; Majewska, A.; Chen, J.Z.; Xie, X.Q.; Hamon, J.; Faller, B.; Gertsch, J. Alkylamides from Echinacea are a new class of cannabinomimetics: Cannabinoid type 2 receptor-dependent and-independent immunomodulatory effects. J. Biol. Chem. 2006, 281, 14192–14206. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Lee, M.; Kim, D.; Oh, D.H.; Prasad, K.S.; Eun, S.; Lee, J. Echinacea purpurea extract enhances natural killer cell activity in vivo by upregulating MHC II and Th1-type CD4+ T cell responses. J. Med. Food 2021, 24, 1039–1049. [Google Scholar] [CrossRef] [PubMed]
- Matthias, A.; Banbury, L.; Stevenson, L.M.; Bone, K.M.; Leach, D.N.; Lehmann, R.P. Alkylamides from Echinacea modulate induced immune responses in macrophages. Immunol. Investig. 2007, 36, 117–130. [Google Scholar] [CrossRef]
- Coeugniet, E.G.; Elek, E. Immunomodulation with Viscum album and Echinacea purpurea extracts. Oncol. Res. Treat. 1987, 10, 27–33. [Google Scholar] [CrossRef]
- Aarland, R.C.; Bañuelos-Hernández, A.E.; Fragoso-Serrano, M.; Sierra-Palacios, E.D.C.; Díaz de León-Sánchez, F.; Pérez-Flores, L.J.; Mendoza-Espinoza, J.A. Studies on phytochemical, antioxidant, anti-inflammatory, hypoglycaemic and antiproliferative activities of Echinacea purpurea and Echinacea angustifolia extracts. Pharm. Biol. 2017, 55, 649–656. [Google Scholar] [CrossRef]
- Dall’Acqua, S.; Perissutti, B.; Grabnar, I.; Farra, R.; Comar, M.; Agostinis, C.; Voinovich, D. Pharmacokinetics and immunomodulatory effect of lipophilic Echinacea extract formulated in softgel capsules. Eur. J. Pharm. Biopharm. 2015, 97, 8–14. [Google Scholar] [CrossRef]
- Classen, B.; Csávás, M.; Borbás, A.; Dingermann, T.; Zündorf, I. Monoclonal antibodies against an arabinogalactan-protein from pressed juice of Echinacea purpurea. Planta Medica 2004, 70, 861–865. [Google Scholar] [CrossRef]
- Zorig, A.; Toko, R.; Sukhbold, E.; Takasugi, M.; Arai, H. Echinacea purpurea water extracts suppress the release of chemical mediators from mast cells. Biosci. Biotechnol. Biochem. 2021, 85, 931–940. [Google Scholar] [CrossRef] [PubMed]
- Hou, C.C.; Chen, C.H.; Yang, N.S.; Chen, Y.P.; Lo, C.P.; Wang, S.Y.; Shyur, L.F. Comparative metabolomics approach coupled with cell-and gene-based assays for species classification and anti-inflammatory bioactivity validation of Echinacea plants. J. Nutr. Biochem. 2010, 21, 1045–1059. [Google Scholar] [CrossRef] [PubMed]
- Randolph, R.K.; Gellenbeck, K.; Stonebrook, K.; Brovelli, E.; Qian, Y.; Bankaitis-Davis, D.; Cheronis, J. Regulation of human immune gene expression as influenced by a commercial blended Echinacea product: Preliminary studies. Exp. Biol. Med. 2003, 228, 1051–1056. [Google Scholar] [CrossRef] [PubMed]
- Barnes, J.; Anderson, L.A.; Phillipson, J.D. Herbal Medicines. A Guide for Healthcare Professionals, updated CDROM of 2nd ed.; Pharmaceutical Press: London, UK, 2004. [Google Scholar]
- Binns, S.E.; Hudson, J.; Merali, S.; Arnason, J.T. Antiviral activity of characterized extracts from Echinacea spp. (Heliantheae: Asteraceae) against Herpes simplex virus (HSV-1). Planta Med. 2002, 68, 780–783. [Google Scholar] [CrossRef] [PubMed]
- Christakis, D.A.; Lehmann, H.P. Can an herbal preparation of echinacea, propolis, and vitamin C reduce respiratory illnesses in children? Arch. Pediatr. Adolesc. Med. 2004, 158, 222–224. [Google Scholar]
- Cohen, H.A.; Varsano, I.; Kahan, E.; Sarrell, M.; Uziel, Y. Effectiveness of an herbal preparation containing Echinacea, propolis, and vitamin C in preventing respiratory tract infections in children. A randomized, double-blind, placebo-controlled, multicenter study. Arch. Pediatr. Adolesc. Med. 2004, 158, 217–221. [Google Scholar] [CrossRef]
- Grimm, W.; Muller, H.H. A randomized controlled trial of the effect of fluid extract of Echinacea purpurea on the incidence and severity of colds and respiratory infections. Am. J. Med. 1999, 106, 138–143. [Google Scholar] [CrossRef]
- Lee, A.N.; Werth, V.P. Activation of autoimmunity following use of immunostimulatory herbal supplements. Arch. Dermatol 2004, 140, 723–727. [Google Scholar] [CrossRef]
- Matthias, A.; Penman, K.G.; Addison, R.S.; Dickinson, R.G.; Bone, K.M.; Lehmann, R.P. Bioavailability and pharmacokinetics of alkylamides from Echinacea. Int. Congr. Nat. Prod. Res. Phoenix Ariz. 2004, 57, p133. [Google Scholar]
- Wichtl, M. (Ed.) Herbal Drugs and Phytopharmaceuticals. A Handbook for Practice on a Scientific Basis, 3rd ed.; Medpharm Scientific Publishers: Stuttgart, Germany, 2004. [Google Scholar]
- Parsons, J.L.; Cameron, S.I.; Harris, C.S.; Smith, M.L. Echinacea biotechnology: Advances, commercialization, and future considerations. Pharm. Biol. 2018, 56, 485–494. [Google Scholar] [CrossRef]
- Catanzaro, M.; Corsini, E.; Rosini, M.; Racchi, M.; Lanni, C. Immunomodulators inspired by nature: A review on curcumin and echinacea. Molecules 2018, 23, 2778. [Google Scholar] [CrossRef] [PubMed]
- Burlou-Nagy, C.; Bănică, F.; Jurca, T.; Vicaș, L.G.; Marian, E.; Muresan, M.E.; Pallag, A. Echinacea purpurea (L.) Moench: Biological and pharmacological properties. A review. Plants 2022, 11, 1244. [Google Scholar] [CrossRef] [PubMed]
- Justus, W.; Hossain, M.F. Echinacea, The Immune-Boosting Potential of Nature’s Herbal Remedy: A Systematic Review. Am. J. Nat. Med. Facts 2024, 1, 1–4. [Google Scholar]
- Manohar, K.A.; Shahina, N.N.; Sarkar, B.C.; Shukla, G.; Das, S.; Singh, M.; Chakravarty, S. Ethnomedicinal plants: Medicine and nutrition for future generations. In Bioprospecting of Ethnomedicinal Plant Resources; Apple Academic Press: Palm Bay, FL, USA, 2025; pp. 11–34. [Google Scholar]
- McNeil, B.K.; Renaud, D.L.; Steele, M.A.; Keunen, A.J.; DeVries, T.J. Effects of Echinacea purpurea supplementation on markers of immunity, health, intake, and growth of dairy calves. J. Dairy Sci. 2023, 106, 4949–4965. [Google Scholar] [CrossRef] [PubMed]
- Sperber, S.J.; Shah, L.P.; Gilbert, R.D.; Ritchey, T.W.; Monto, A.S. Echinacea purpurea for prevention of experimental rhinovirus colds. Clin. Infect. Dis. 2004, 38, 1367–1371. [Google Scholar] [CrossRef]



| Species | Hydrocarbon |
|---|---|
| E. angustifolia | Dodeca-2,4-dien-1yl isovalerate (Z)-Pentadeca-1,8 diene Pentadec-1-ene |
| E. pallida | (Z)-Pentadec-8-en-2-one |
| (Z)-Pentadeca-1,8-diene Pentadec-1-ene | |
| (8Z,11Z)-Pentadeca-8,11-dien-2-one | |
| (8Z,13Z)-Pentadeca-8,13-dien-11-yn-2-one | |
| (Z)-Tetradeca-8-diene-11,13-diyn-2-one | |
| (E)-10-Hydroxy -4,10-dimethydodeca-4, 11-dien-2-one (echinolone) | |
| (Z)-Pentadeca-8-ene-11,13-diyn-2-one | |
| (8Z,11Z,13E)-Pentadeca-8,11,13-trien-2-one | |
| (8Z,11E,13Z)-Pentadeca-8,11-trien-2-one | |
| E. purpurea | Dodeca-2,4-dien-1-yl isovalerate |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmadi, F. Phytochemistry, Mechanisms, and Preclinical Studies of Echinacea Extracts in Modulating Immune Responses to Bacterial and Viral Infections: A Comprehensive Review. Antibiotics 2024, 13, 947. https://doi.org/10.3390/antibiotics13100947
Ahmadi F. Phytochemistry, Mechanisms, and Preclinical Studies of Echinacea Extracts in Modulating Immune Responses to Bacterial and Viral Infections: A Comprehensive Review. Antibiotics. 2024; 13(10):947. https://doi.org/10.3390/antibiotics13100947
Chicago/Turabian StyleAhmadi, Fatemeh. 2024. "Phytochemistry, Mechanisms, and Preclinical Studies of Echinacea Extracts in Modulating Immune Responses to Bacterial and Viral Infections: A Comprehensive Review" Antibiotics 13, no. 10: 947. https://doi.org/10.3390/antibiotics13100947
APA StyleAhmadi, F. (2024). Phytochemistry, Mechanisms, and Preclinical Studies of Echinacea Extracts in Modulating Immune Responses to Bacterial and Viral Infections: A Comprehensive Review. Antibiotics, 13(10), 947. https://doi.org/10.3390/antibiotics13100947







