Effect of N-Acetyl-L-cysteine on Activity of Doxycycline against Biofilm-Forming Bacterial Strains
Abstract
1. Introduction
2. Results
2.1. Determination of the Minimum Inhibitory Concentrations (MICs) of Doxycycline Hyclate and N-Acetyl-L-cysteine
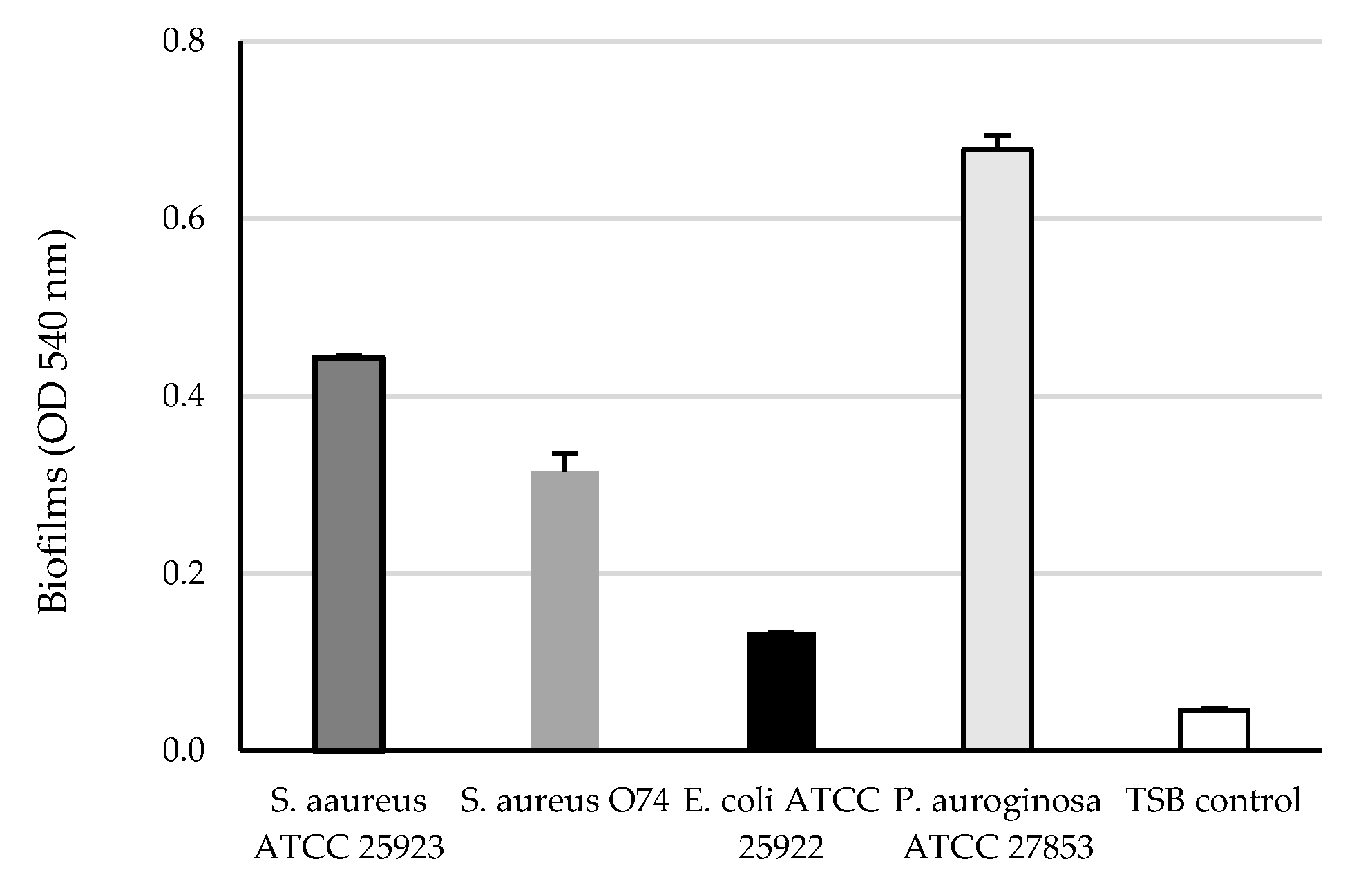
2.2. Biofilm Formation of Gram-Positive and Gram-Negative Pathogens
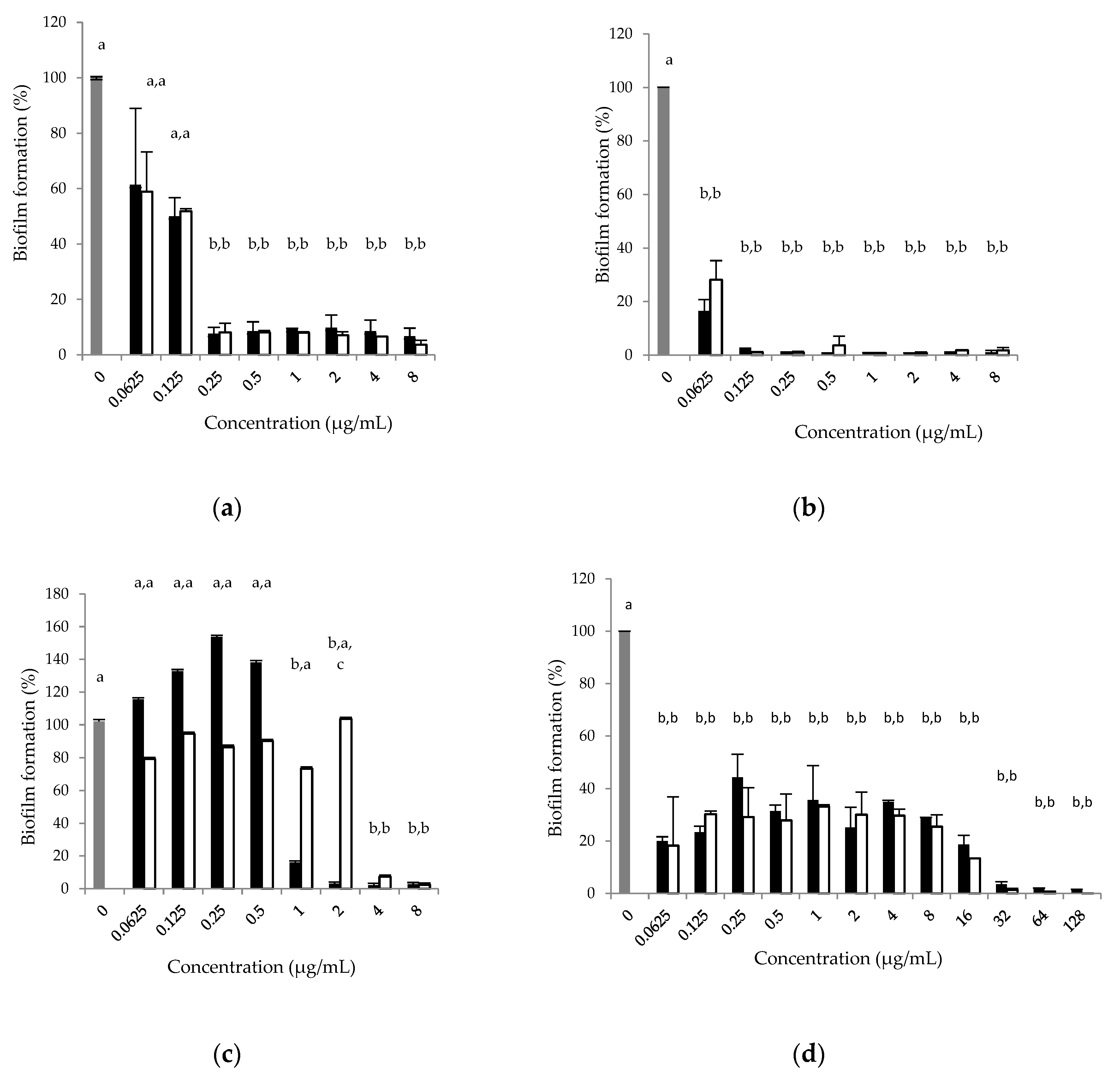
2.3. The Effect of Doxycycline and N-Acetyl-L-cysteine on Biofilm Formation
3. Discussion
4. Materials and Methods
4.1. Bacterial Strains, Culture Media and Conditions
4.2. Drugs and Reagents
4.3. The Determination of Minimum Inhibitory Concentrations (MICs)
4.4. In Vitro Biofilm Formation and the Determination of Minimum Biofilm Inhibitory Concentration (MBIC)
4.5. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jabra-Rizk, M.A.; Meiller, T.F.; James, C.E.; Shirtliff, M.E. Effect of farnesol on Staphylococcus aureus biofilm formation and antimicrobial susceptibility. Antimicrob. Agents Chemother. 2006, 50, 1463–1469. [Google Scholar] [CrossRef]
- Parrino, B.; Schillaci, D.; Carnevale, I.; Giovannetti, E.; Diana, P.; Cirrincione, G.; Cascioferro, S. Synthetic small molecules as anti-biofilm agents in the struggle against antibiotic resistance. Eur. J. Med. Chem. 2019, 161, 154–178. [Google Scholar] [CrossRef] [PubMed]
- Dhaouadi, S.; Romdhani, A.; Bouglita, W.; Chedli, S.; Chaari, S.; Soufi, L.; Cherif, A.; Mnif, W.; Abbassi, M.S.; Elandoulsi, R.B. High biofilm-forming ability and clonal dissemination among colistin-resistant Escherichia coli isolates recovered from cows with mastitis, diarrheic calves, and chickens with colibacillosis in Tunisia. Life 2023, 13, 299. [Google Scholar] [CrossRef] [PubMed]
- Vert, M.; Doi, Y.; Hellwich, K.; Hess, M.; Hodge, P.; Kubisa, P.; Rinaudo, M.; Schué, F. Terminology for biorelated polymers and applications. Chem. Int. Newsmag. 2011, 33, 377–410. [Google Scholar] [CrossRef]
- Mirzaei, R.; Mohammadzadeh, R.; Sholeh, M.; Karampoor, S.; Abdi, M.; Dogan, E.; Moghadam, M.S.; Kazemi, S.; Jalalifar, S.; Dalir, A.; et al. The importance of intracellular bacterial biofilm in infectious diseases. Microb. Pathog. 2020, 147, 104393. [Google Scholar] [CrossRef] [PubMed]
- Mittal, S.; Sharma, M.; Chaudhary, U. Biofilm and multidrug resistance in uropathogenic Escherichia coli. Pathog. Glob. Health 2015, 109, 26–29. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Datta, S.; Narayanan, K.B.; Rajnish, K.N. Bacterial exo-polysaccharides in biofilms: Role in antimicrobial resistance and treatments. J. Genet. Eng. Biotechnol. 2021, 19, 140. [Google Scholar] [CrossRef]
- Ciofu, O.; Tolker-Nielsen, T. Tolerance and resistance of Pseudomonas aeruginosa biofilms to antimicrobial agents—How P. aeruginosa can escape antibiotics. Front. Microbiol. 2019, 10, 913. [Google Scholar] [CrossRef]
- Bowler, P.; Murphy, C.; Wolcott, R. Biofilm exacerbates antibiotic resistance: Is this a current oversight in antimicrobial stewardship? Antimicrob. Resist. Infect. Control 2020, 9, 162. [Google Scholar] [CrossRef]
- Buur, J.L.; Diniz, P.; Roderick, K.V.; KuKanich, B.; Tegzes, J. Pharmacokinetics of N-acetylcysteine after oral and intravenous administration to healthy cats. Am. J. Vet. Res. 2013, 74, 290–293. [Google Scholar] [CrossRef]
- May, E.R.; Ratliff, B.E.; Bemis, D.A. Antibacterial effect of N-acetylcysteine in combination with antimicrobials on common canine otitis externa bacterial isolates. Vet. Dermatol. 2019, 30, 531-e161. [Google Scholar] [CrossRef]
- Walter, H.; Verspohl, J.; Meißner, J.; Oltmanns, H.; Geks, A.K.; Busse, C. In vitro antimicrobial activity of N-acetylcysteine against pathogens most commonly associated with infectious keratitis in dogs and cats. Antibiotics 2023, 12, 559. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.H.; Jang, E.Y.; Shim, K.S.; Lee, J.Y. In vitro effects of N-acetyl cysteine alone and in combination with antibiotics on Prevotella intermedia. J. Microbiol. 2015, 53, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Caissie, M.D.; Gartley, C.J.; Scholtz, E.L.; Hewson, J.; Johnson, R.; Chenier, T. The effects of treatment with N-acetyl cysteine on clinical signs in persistent breeding-induced endometritis susceptible mares. J. Equine Vet. Sci. 2020, 92, 103142. [Google Scholar] [CrossRef] [PubMed]
- Anastasi, E.; Scaramuzzino, S.; Viscardi, M.F.; Viggiani, V.; Piccioni, M.G.; Cacciamani, L.; Merlino, L.; Angeloni, A.; Muzii, L.; Porpora, M.G. Efficacy of N-acetylcysteine on endometriosis-related pain, size reduction of ovarian endometriomas, and fertility outcomes. Int. J. Environ. Res. Public Health 2023, 20, 4686. [Google Scholar] [CrossRef]
- Wang, X.; Svedin, P.; Nie, C.; Lapatto, R.; Zhu, C.; Gustavsson, M.; Sandberg, M.; Karlsson, J.O.; Romero, R.; Hagberg, H.; et al. N-acetylcysteine reduces lipopolysaccharide-sensitized hypoxic–ischemic brain injury. Ann. Neurol. 2007, 61, 263–271. [Google Scholar] [CrossRef]
- Sadowska, A.M. N-Acetylcysteine mucolysis in the management of chronic obstructive pulmonary disease. Ther. Adv. Respir. Dis. 2012, 6, 127–135. [Google Scholar] [CrossRef]
- Cammarota, G.; Sanguinetti, M.; Gallo, A.; Posteraro, B. Review article: Biofilm formation by Helicobacter pylori as a target for eradication of resistant infection. Aliment. Pharmacol. Ther. 2012, 36, 222–230. [Google Scholar] [CrossRef]
- Dincola, S.; De Grazia, S.; Carlomagno, G.; Pintucci, J.P. N-acetylcysteine as powerful molecule to destroy bacterial biofilms. A systematic review. Eur. Rev. Med Pharmacol. Sci. 2014, 18, 2942–2948. [Google Scholar]
- Yang, F.; Liu, L.H.; Li, X.P.; Luo, J.Y.; Zhang, Z.; Yan, Z.T.; Zhang, S.D.; Li, H.S. N-Acetylcysteine-mediated modulation of antibiotic susceptibility of bovine mastitis pathogens. J. Dairy Sci. 2016, 99, 4300–4302. [Google Scholar] [CrossRef]
- del Castillo, J.R.E. Tetracyclines. In Antimicrobial Therapy in Veterinary Medicine, 5th ed.; Giguère, S., Prescott, J.F., Dowling, P.M., Eds.; Wiley Blackwel: Hoboken, NJ, USA, 2013; pp. 257–268. [Google Scholar]
- European Medicines Agency (EMA): Categorisation of Antibiotics Used in Animals Promotes Responsible Use to Protect Public and Animal Health. Available online: https://www.ema.europa.eu/en/news/categorisation-antibiotics-used-animals-promotes-responsible-use-protect-public-animal-health (accessed on 14 April 2023).
- Boehm, A.; Steiner, S.; Zaehringer, F.; Casanova, A.; Hamburger, F.; Ritz, D.; Keck, W.; Ackermann, M.; Schirmer, T.; Jenal, U. Second messenger signalling governs Escherichia coli biofilm induction upon ribosomal stress. Mol. Microbiol. 2009, 72, 1500–1516. [Google Scholar] [CrossRef] [PubMed]
- Trizna, E.Y.; Yarullina, M.N.; Baidamshina, D.R.; Mironova, A.V.; Akhatova, F.S.; Rozhina, E.V.; Fakhrullin, R.F.; Khabibrakhmanova, A.M.; Kurbangalieva, A.R.; Bogachev, M.I.; et al. Bidirectional alterations in antibiotics susceptibility in Staphylococcus aureus-Pseudomonas aeruginosa dual-species biofilm. Sci. Rep. 2020, 10, 14849. [Google Scholar] [CrossRef] [PubMed]
- Toutain, P.L.; Gandia, P.; Pelligand, L.; Ferran, A.A.; Lees, P.; Bousquet-Mélou, A.; Concordet, D. Biased computation of probability of target attainment for antimicrobial drugs. CPT Pharmacomet. Syst. Pharmacol. 2023, 12, 681–689. [Google Scholar] [CrossRef] [PubMed]
- Agwuh, K.N.; MacGowan, A. Pharmacokinetics and pharmacodynamics of the tetracyclines including glycylcyclines. J. Antimicrob. Chemother. 2006, 58, 256–265. [Google Scholar] [CrossRef]
- Petkova, T.; Yordanova, A.; Milanova, A. Population pharmacokinetics of doxycycline, administered alone or with N-acetylcysteine, in chickens with experimental Mycoplasma gallisepticum infection. Pharmaceutics 2022, 14, 2440. [Google Scholar] [CrossRef]
- Goswami, M.; Jawali, N. N-acetylcysteine-mediated modulation of bacterial antibiotic susceptibility. Antimicrob. Agents Chemother. 2010, 54, 3529–3530. [Google Scholar] [CrossRef]
- Landini, G.; Di Maggio, T.; Sergio, F.; Docquier, J.D.; Rossolini, G.M.; Pallecchi, L. Effect of High N-acetylcysteine concentrations on antibiotic activity against a large collection of respiratory pathogens. Antimicrob. Agents Chemother. 2016, 60, 7513–7517. [Google Scholar] [CrossRef]
- European Committee on Antimicrobial Susceptibility Testing: Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 13.0, Valid from 2023-01-01. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_13.0_Breakpoint_Tables.pdf (accessed on 15 April 2023).
- Jones, R.N.; Stilwell, M.G. Contemporary Doxycycline and Tetracycline Susceptibility Testing Using CLSI and EUCAST Criteria for Gram-Positive Pathogens: Results from SENTRY Program. In Proceedings of the 22nd ECCMID 2012, London, UK, 31 March–3 April 2012; p. 675. Available online: https://www.jmilabs.com/data/posters/ECCMID2012/P675.PDF (accessed on 15 April 2023).
- Petkova, T.; Milanova, A. Absorption of N-acetylcysteine in healthy and Mycoplasma gallisepticum-infected chickens. Vet. Sci. 2021, 8, 244. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute. Performance standards for antimicrobial disk and dilution susceptibility tests for bacteria isolated from animals. In CLSI Document VET01–A4, 4th ed.; approved standard; CLSI: Wayne, PA, USA, 2013. [Google Scholar]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. In CLSI Document M100-S27; Twenty-Seventh Informational Supplement; CLSI: Wayne, PA, USA, 2016. [Google Scholar]
- Kidsley, A.K.; Abraham, S.; Bell, J.M.; O’Dea, M.; Laird, T.J.; Jordan, D.; Mitchell, P.; McDevitt, C.A.; Trott, D.J. Antimicrobial susceptibility of Escherichia coli and Salmonella spp. isolates from healthy pigs in Australia: Results of a pilot national survey. Front. Microbiol. 2018, 9, 1207. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. In CLSI Document M100-S28; 28th Informational Supplement; CLSI: Wayne, PA, USA, 2018. [Google Scholar]
- Meng, L.; Liu, H.; Lan, T.; Dong, L.; Hu, H.; Zhao, S.; Zhang, Y.; Zheng, N.; Wang, J. Antibiotic resistance patterns of Pseudomonas spp. isolated from raw milk revealed by whole genome sequencing. Front. Microbiol. 2020, 11, 1005. [Google Scholar] [CrossRef]
- Manner, S.; Goeres, D.M.; Skogman, M.; Vuorela, P.; Fallarero, A. Prevention of Staphylococcus aureus biofilm formation by antibiotics in 96-Microtiter well plates and drip flow reactors: Critical factors influencing outcomes. Sci. Rep. 2017, 7, 43854. [Google Scholar] [CrossRef] [PubMed]
- Blasi, F.; Page, C.; Rossolini, G.M.; Pallecchi, L.; Matera, M.G.; Rogliani, P.; Cazzola, M. The effect of N-acetylcysteine on biofilms: Implications for the treatment of respiratory tract infections. Respir. Med. 2016, 117, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Giraldo, C.; Rodríguez-Benito, A.; Morán, F.J.; Hurtado, C.; Blanco, M.T.; Gómez-García, A.C. Influence of N-acetylcysteine on the formation of biofilm by Staphylococcus epidermidis. J. Antimicrob. Chemother. 1997, 39, 643–646. [Google Scholar] [CrossRef]
- Zhao, T.; Liu, Y. N-acetylcysteine inhibit biofilms produced by Pseudomonas aeruginosa. BMC Microbiol. 2010, 10, 140. [Google Scholar] [CrossRef] [PubMed]
- Marchese, A.; Bozzolasco, M.; Gualco, L.; Debbia, E.A.; Schito, G.C.; Schito, A.M. Effect of fosfomycin alone and in combination with N-acetylcysteine on E. coli biofilms. Int. J. Antimicrob. Agents 2003, 22, 95–100. [Google Scholar] [CrossRef]
- Li, X.; Kim, J.; Wu, J.; Ahamed, A.I.; Wang, Y.; Martins-Green, M. N-Acetyl-cysteine and mechanisms involved in resolution of chronic wound biofilm. J. Diabetes Res. 2020, 27, 9589507. [Google Scholar] [CrossRef]
- Maaland, M.G.; Papich, M.G.; Turnidge, J.; Guardabassi, L. Pharmacodynamics of doxycycline and tetracycline against Staphylococcus pseudintermedius: Proposal of canine-specific breakpoints for doxycycline. J. Clin. Microbiol. 2013, 51, 3547–3554. [Google Scholar] [CrossRef]
- de Boer, M.; Heuer, C.; Hussein, H.; McDougall, S. Minimum inhibitory concentrations of selected antimicrobials against Escherichia coli and Trueperella pyogenes of bovine uterine origin. J. Dairy Sci. 2015, 98, 4427–4443. [Google Scholar] [CrossRef]
- Yang, F.; Yang, F.; Wang, G.; Kong, T. Pharmacokinetics of doxycycline after oral administration of single and multiple dose in broiler chickens. J. Vet. Pharmacol. Ther. 2018, 41, 919–923. [Google Scholar] [CrossRef]
- Wu, X.; Santos, R.R.; Fink-Gremmels, J. Staphylococcus epidermidis biofilm quantification: Effect of different solvents and dyes. J. Microbiol. Methods 2014, 101, 63–66. [Google Scholar] [CrossRef]
- Stepanovic, S.; Vukovic, D.; Dakic, I.; Savic, B.; Svabic-Vlahovic, M. A modified microtiter-plate test for quantification of staphylococcal biofilm formation. J. Microbiol. Methods 2000, 40, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Schiebel, J.; Böhm, A.; Nitschke, J.; Burdukiewicz, M.; Weinreich, J.; Ali, A.; Roggenbuck, D.; Rödiger, S.; Schierack, P. Genotypic and phenotypic characteristics associated with biofilm formation by human clinical Escherichia coli isolates of different pathotypes. Appl. Environ. Microbiol. 2017, 83, e01660-17. [Google Scholar] [CrossRef] [PubMed]
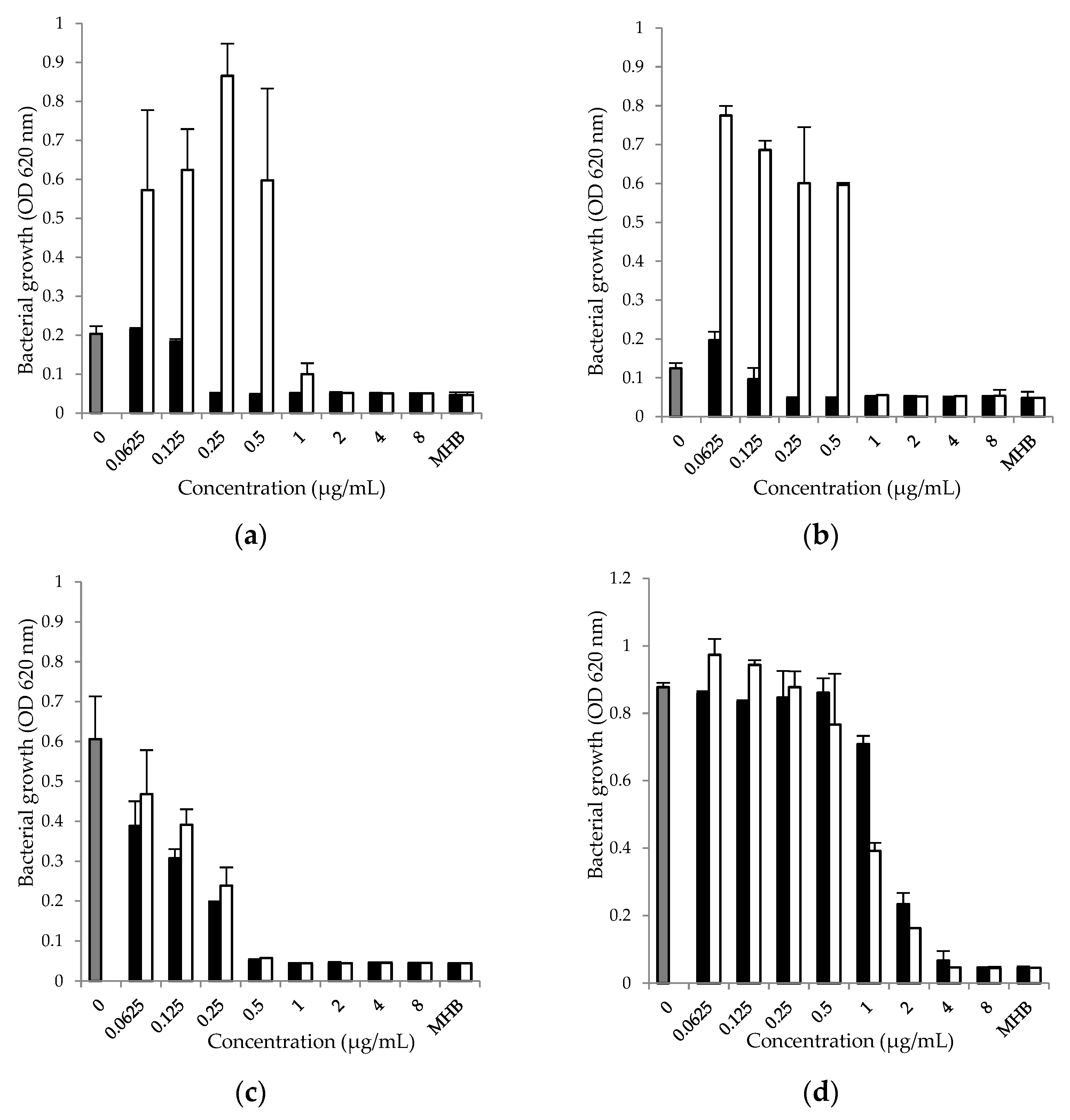
| Tested Strains | MIC | ||
|---|---|---|---|
| Doxycycline | Doxycycline and N-Acetyl-L-cysteine | N-Acetyl-L-cysteine | |
| S. aureus ATCC 25923 | 0.25 μg/mL | 1 μg/mL | 4000 µg/mL |
| S. aureus O74 | 0.25 μg/mL | 1 μg/mL | 4000 µg/mL |
| E. coli ATCC 25922 | 0.5 μg/mL | 0.5 μg/mL | 4000 µg/mL |
| P. aeruginosa ATCC 27853 | 4 μg/mL | 4 μg/mL | 4000 µg/mL |
| Tested Strains | MBIC | ||
|---|---|---|---|
| Doxycycline | Doxycycline and N-Acetyl-L-cysteine | N-Acetyl-L-cysteine | |
| S. aureus ATCC 25923 | 0.25 μg/mL | 0.25 μg/mL | 4000 µg/mL |
| S. aureus O74 | 0.125 μg/mL | 0.125 μg/mL | 4000 µg/mL |
| E. coli ATCC 25922 | 2 μg/mL | 4 μg/mL | 4000 µg/mL |
| P. aeruginosa ATCC 27853 | 32 μg/mL | 32 μg/mL | 4000 µg/mL |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petkova, T.; Rusenova, N.; Danova, S.; Milanova, A. Effect of N-Acetyl-L-cysteine on Activity of Doxycycline against Biofilm-Forming Bacterial Strains. Antibiotics 2023, 12, 1187. https://doi.org/10.3390/antibiotics12071187
Petkova T, Rusenova N, Danova S, Milanova A. Effect of N-Acetyl-L-cysteine on Activity of Doxycycline against Biofilm-Forming Bacterial Strains. Antibiotics. 2023; 12(7):1187. https://doi.org/10.3390/antibiotics12071187
Chicago/Turabian StylePetkova, Tsvetelina, Nikolina Rusenova, Svetla Danova, and Aneliya Milanova. 2023. "Effect of N-Acetyl-L-cysteine on Activity of Doxycycline against Biofilm-Forming Bacterial Strains" Antibiotics 12, no. 7: 1187. https://doi.org/10.3390/antibiotics12071187
APA StylePetkova, T., Rusenova, N., Danova, S., & Milanova, A. (2023). Effect of N-Acetyl-L-cysteine on Activity of Doxycycline against Biofilm-Forming Bacterial Strains. Antibiotics, 12(7), 1187. https://doi.org/10.3390/antibiotics12071187







