Staphylococcus aureus and CA-MRSA Carriage among Brazilian Indians Living in Peri-Urban Areas and Remote Communities
Abstract
1. Introduction
2. Results
3. Discussion
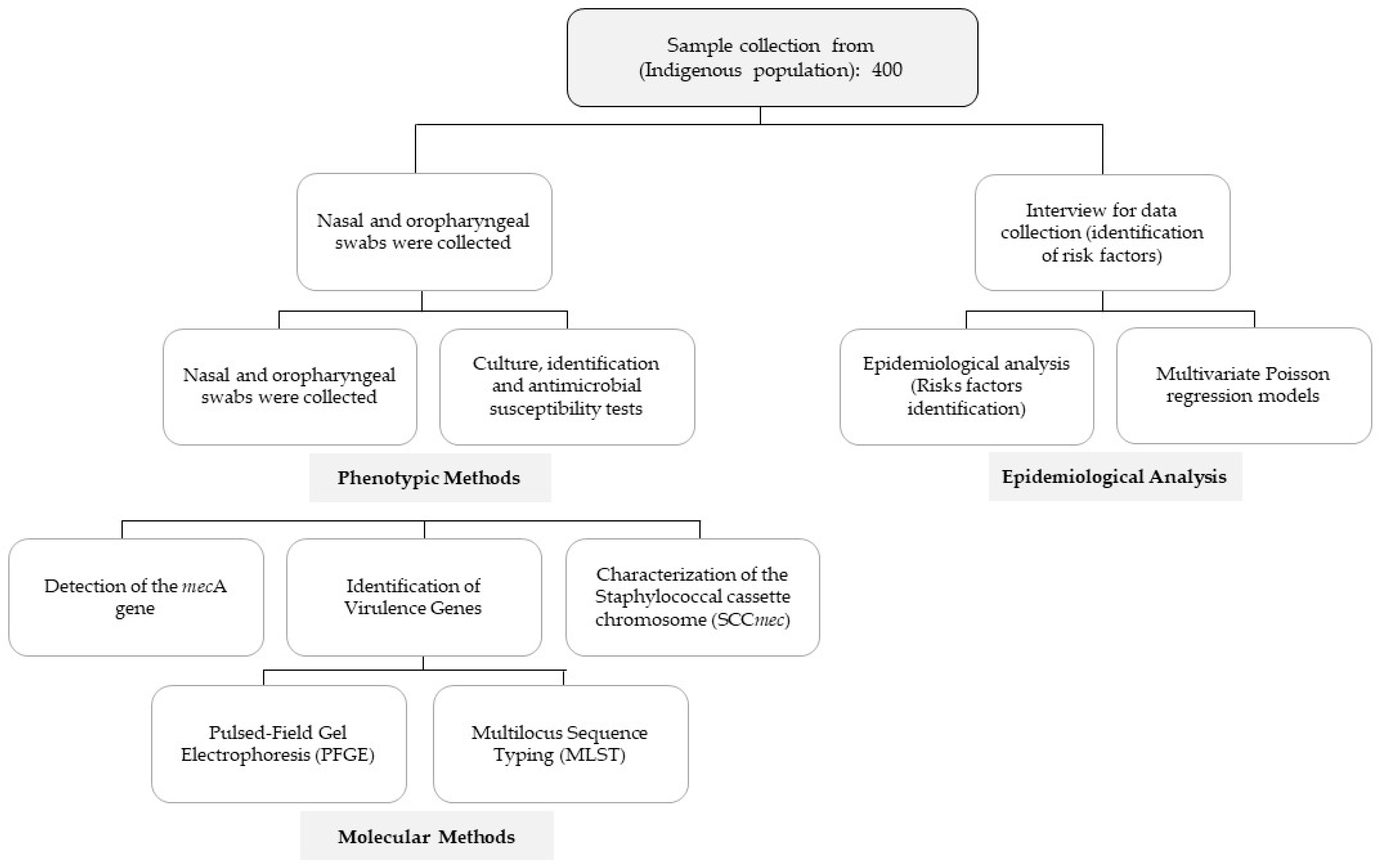
4. Materials and Methods
4.1. Study Design, Subjects, and Procedures
4.2. Specimen Collection, Culture, and Antimicrobial Susceptibility Tests
4.3. Identification of Virulence Genes
4.4. Molecular Methods
4.5. Epidemiological Analysis
4.6. Ethical Issues
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- David, M.Z.; Daum, R.S. Community-associated methicillin-resistant Staphylococcus aureus: Epidemiology and clinical consequences of an emerging epidemic. Clin. Microbiol. Rev. 2010, 23, 616–687. [Google Scholar] [CrossRef]
- Sutcliffe, C.G.; Grant, L.R. High Burden of Staphylococcus aureus Among Native American Individuals on the White Mountain Apache Tribal Lands. Open Forum Infect. Dis. 2020, 7, ofaa061. [Google Scholar] [CrossRef]
- Kanjilal, S.; Sater, M.R.A. Trends in antibiotic susceptibility in Staphylococcus aureus in Boston, Massachusetts, from 2000 to 2014. J. Clin. Microbiol. 2018, 56, e01160-17. [Google Scholar] [CrossRef]
- Sutcliffe, C.G.; Grant, L.R. The burden of Staphylococcus aureus among Native Americans on the Navajo Nation. PLoS ONE 2019, 14, e0213207. [Google Scholar] [CrossRef] [PubMed]
- Cella, C.; Sutcliffe, C.G. Carriage prevalence and genomic epidemiology of Staphylococcus aureus among Native American children and adults in the Southwestern USA. Microb. Genom. 2022, 8, mgen000806. [Google Scholar] [CrossRef] [PubMed]
- Mehraj, J.; Witte, W. Epidemiology of Staphylococcus aureus Nasal Carriage Patterns in the Community. Curr. Top. Microbiol. Immunol. 2016, 398, 55–87. [Google Scholar] [PubMed]
- Butler, J.C.; Crengle, S. Emerging infectious diseases among indigenous peoples. Emerg. Infect. Dis. 2001, 7, 554–555. [Google Scholar] [CrossRef] [PubMed]
- Landen, M.G.; McCumber, B.J. Asam ED, Egeland GM. Outbreak of boils in an Alaskan village: A case-control study. West. J. Med. 2000, 172, 235–239. [Google Scholar] [CrossRef]
- Groom, A.V.; Wolsey, D.H. Community-acquired methicillin-resistant Staphylococcus aureus in a rural American Indian community. JAMA 2001, 286, 1201–1205. [Google Scholar] [CrossRef] [PubMed]
- Muileboom, J.; Hamilton, M. Community-associated methicillin-resistant Staphylococcus aureus in northwest Ontario: A five-year report of incidence and antibiotic resistance. Can. J. Infect. Dis. Med. Microbiol. 2013, 24, e42–e44. [Google Scholar] [CrossRef] [PubMed]
- Abelson, W.H.; Banerji, A. Community-associated methicillin-resistant Staphylococcus aureus in indigenous communities in Canada. Paediatr. Child. Health 2012, 17, 395–398. [Google Scholar]
- Ng, J.W.S.; Holt, D.C. Phylogenetically distinct Staphylococcus aureus lineage prevalent among indigenous communities in northern Australia. J. Clin. Microbiol. 2009, 47, 2295–2300. [Google Scholar] [CrossRef] [PubMed]
- Tong, S.Y.C.; Varrone, L. Progressive increase in community-associated methicillin-resistant Staphylococcus aureus in indigenous populations in northern Australia from 1993 to 2012. Epidemiol. Infect. 2015, 143, 1519–1523. [Google Scholar] [CrossRef]
- IBGE. Instituto Brasileiro de Geografia e Estatística [Internet]. Brazil: Censo Polulações Indígenas. Available online: https://www.gov.br/funai/pt-br/assuntos/noticias/2022-02/ultimo-censo-do-ibge-registrou-quase-900-mil-indigenas-no-pais-dados-serao-atualizados-em-2022#:~:text=%C3%9Altimo%20censo%20do%20IBGE%20regi-trou,Funda%C3%A7%C3%A3o%20Nacional%20dos%20Povos%20Ind%C3%ADgenas (accessed on 12 February 2023).
- Tong, S.Y.; McDonald, M.I. Global implications of the emergence of community-associated methicillin-resistant Staphylococcus aureus in Indigenous populations. Clin. Infect. Dis. 2008, 46, 1871–1878. [Google Scholar] [CrossRef]
- Wertheim, H.F.; Melles, D.C. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect. Dis. 2005, 12, 751–762. [Google Scholar] [CrossRef] [PubMed]
- Verhagen, L.M.; Hermsen, M. Nasopharyngeal carriage of respiratory pathogens in Warao Amerindians: Significant relationship with stunting. Trop. Med. Int. Health 2017, 22, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Daley, P.; Bajgai, J. A cross sectional study of animal and human colonization with methicillin-resistant Staphylococcus aureus (MRSA) in an Aboriginal community. BMC Public. Health 2016, 16, 1–7. [Google Scholar] [CrossRef]
- Ruimy, R.; Angebault, C.C. Are host genetics the predominant determinant of persistent nasal Staphylococcus aureus carriage in humans? J. Infect. Dis. 2010, 202, 924–934. [Google Scholar] [CrossRef]
- Pires, F.V.; Da Cunha, M.D.L.R.D.S. Nasal carriage of Staphylococcus aureus in Botucatu, Brazil: A population-based survey. PLoS ONE 2014, 9, e92537. [Google Scholar] [CrossRef]
- Sader, H.S.; Gales, A.C. Pathogen frequency and resistance patterns in Brazilian hospitals: Summary of results from three years of the SENTRY Antimicrobial Surveillance Program. Braz. J. Infect. Dis. 2001, 5, 200–214. [Google Scholar] [CrossRef]
- Abraão, L.M. Detection of Virulence Genes and Identification of the Clonal Profile of Staphylococcus aureus Isolates Colonizing the Nasopharynx Obtained in a Popular Base Study. Master’s Degree. Paulista State University “Júlio de Mesquita Filho” (UNESP), Botucatu, São Paulo State, Brazil, February 2013. Available online: https://repositorio.unesp.br/handle/11449/110458?show=full (accessed on 20 February 2023).
- Bride, L.L.; Pereira, M.F. Differences in resistance profiles and virulence genes among methicillin-resistant and methicillin-susceptible Staphylococcus aureus of different lineages at a public tertiary hospital. Rev. Soc. Bras. Med. Trop. 2019, 52, e20190095. [Google Scholar] [CrossRef]
- Boan, P.; Tan, H. Epidemiological, clinical, outcome and antibiotic susceptibility differences between PVL positive and PVL negative Staphylococcus aureus infections in Western Australia: A case control study. BMC Infect. Dis. 2015, 15, 10. [Google Scholar] [CrossRef] [PubMed]
- Robinson, D.A.; Enright, M.C. Evolutionary models of the emergence of methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 2003, 47, 3926–3934. [Google Scholar] [CrossRef] [PubMed]
- Enright, M.C.; Day, N.P.J. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J. Clin. Microbiol. 2000, 38, 1008–1015. [Google Scholar] [CrossRef] [PubMed]
- Shettigar, K.; Murali, T.S. Virulence factors and clonal diversity of Staphylococcus aureus in colonization and wound infection with emphasis on diabetic foot infection. Eur. J. Clin. Microbiol. Infect. Dis. 2020, 39, 2235–2246. [Google Scholar] [CrossRef]
- McGuinness, S.L.; Holt, D.C. Clinical and molecular epidemiology of an emerging Panton Valentine leukocidin-positive ST5 methicillin-resistant Staphylococcus aureus clone in northern Australia. mSphere 2021, 6, e00651-20. [Google Scholar] [CrossRef] [PubMed]
- Jian, Y.; Zhao, L. Increasing Prevalence of Hypervirulent ST5 Methicillin Susceptible Staphylococcus aureus Subtype Poses a Serious Clinical Threat. Emerg. Microbes Infect. 2020, 10, 109–122. [Google Scholar] [CrossRef] [PubMed]
- Witzel, C.; Fortaleza, C.M.C.B. Nasopharyngeal carriage of Staphylococcus aureus among imprisoned males from Brazil without exposure to healthcare: Risk factors and molecular characterization. Ann. Clin. Microbiol. Antimicrob. 2014, 13, 25. [Google Scholar] [CrossRef] [PubMed]
- Sola, C.; Paganini, H. Spread of epidemic MRSA-ST5-IV clone encoding PVL as a major cause of community onset staphylococcal infections in Argentinean children. PLoS ONE 2012, 7, e30487. [Google Scholar] [CrossRef] [PubMed]
- Konemman, E.V.; Allen, S.D. Introdução à microbiologia médica. In Diagnóstico Microbiológico: Texto e Atlas Colorido, 5th ed.; Medsi: Rio de Janeiro, Brazil, 2001; pp. 200–210. [Google Scholar]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Disk Susceptibility Tests, 31st ed.; CLSI Supplement M100; Clinical and Laboratory Standards Institute: Wayne, PE, USA, 2021. [Google Scholar]
- Johnson, W.M.; Tyler, S.D. Detection of genes for enterotoxins, exfoliative toxins, and toxic shock syndrome toxin 1 in Staphylococcus aureus by the polymerase chain reaction. J. Clin. Microbiol. 1991, 29, 426–430. [Google Scholar] [CrossRef]
- Cunha, M.D.L.R.S.; Calsolari, R.O. Detection of enterotoxin and toxic shock syndrome toxin 1 genes in Staphylococcus, with emphasis on coagulase-negative staphylococci. Microbiol. Immunol. 2007, 51, 381–390. [Google Scholar] [CrossRef] [PubMed]
- Marconi, C.; Cunha, M.L.R.S. Standardization of the PCR technique for the detection of delta toxin in Staphylococcus spp. J. Venom. Anim. Toxins Incl. Trop. Dis. 2005, 11, 117–128. [Google Scholar] [CrossRef]
- Koning, S.; Van, B.A. Severity of nonbullous Staphylococcus aureus impetigo in children is associated with strains harboring genetic markers for exfoliative toxin B, Panton-Valentine leukocidin, and the multidrug resistance plasmid pSK41. J. Clin. Microbiol. 2003, 41, 3017–3021. [Google Scholar] [CrossRef] [PubMed]
- Arciola, C.R.; Gamberini, S. A multiplex PCR method for the detection of all five individual genes of ica locus in Staphylococcus epidermidis. A survey on 400 clinical isolates from prosthesis-associated infections. J. Biomed. Mater. Res. A 2005, 75, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Fang, H.; Hedin, G. Rapid Screening and Identification of Methicillin-Resistant Staphylococcus aureus from Clinical Samples by Selective-Broth and Real-Time PCR Assay. J. Clin. Microbiol. 2003, 41, 2894–2899. [Google Scholar] [CrossRef]
- Milheirico, C.; Oliveira, D.C. Update to the multiplex PCR strategy for assignment of mec element types in Staphylococcus aureus. Antimicrob. Agents Chemother. 2007, 51, 4537. [Google Scholar] [CrossRef]
- McDougal, L.K.; Steward, C.D. Pulsed-field gel electrophoresis typing of oxacillin-resistant Staphylococcus aureus isolates from the United States: Establishing a National Database. J. Clin. Microbiol. 2003, 41, 5113–5120. [Google Scholar] [CrossRef]
- Coutinho, L.M.S.; Scazufca, M. Methods for estimating prevalence ratios in cross-sectional studies. Rev. Saude Publica 2008, 42, 992–998. [Google Scholar] [CrossRef] [PubMed]
- Barros, A.J.D.; Hirakata, V.N. Alternatives for logistic regression in cross-sectional studies: An empirical comparison of models that directly estimate the prevalence ratio. BMC Med. Res. Methodol. 2003, 21, 21. [Google Scholar] [CrossRef]

| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| Predictors | S. aureus | Negative | (95% CI) | p Value | RR (95% CI) | p Value |
| Demographic Variables | ||||||
| Women | 113 (59.5) | 112 (53.6) | 1.12 (0.93–1.35) | 0.24 | ||
| Age, median (quartiles) | 21 (11.5–34) | 27 (14–43) | … | 0.03 * | 0.99 (0.98–1.00) | 0.08 |
| Ethnicity | ||||||
| Shanenawa (reference) * | 78 (41.1) | 57 (27.3) | … | … | 1.36 (CI, 1.02–1.82) | 0.03 * |
| Puyanawas I | 22 (11.1) | 30 (14.4) | 0.73 (0.52–1.04) | 0.06 | 0,74 (0.46–1.20) | 0.22 |
| Kaxinawa | 16 (8.4) | 34 (16.3) | 0.55 (0.36–0.85) | 0.002 * | 0.55 (0.32–0.94) | 0.03 * |
| Kopenoti | 31 (16.3) | 33 (15.8) | 0.84 (0.63–1.12) | 0.22 | 0.87 (0.57–1.32) | 0.52 |
| Teregua | 19 (10.0) | 33 (15.8) | 0.63 (0.43–0.93) | 0.009 * | 0.67 (0.40–1.11) | 0.11 |
| Ashaninka | 4 (2.1) | 1 (10.5) | 1.34 (0.87–2.20) | 0.32 | 1.32 (0.48–3.62) | 0.58 |
| Puyanawas II | 21 (11.1) | 21 (10.1) | 0.87 (0.62–1.21) | 0.38 | 0.91 (0.56–1.38) | 0.7 |
| Group (São Paulo x Acre) | 50 (26.3) | 66 (31.6) | 0.89 (0.73–1.08) | 0.25 | ||
| Income in R$, median (quartiles) | 688 (430–800) | 700 (422–815) | 0.97 | |||
| Schooling | ||||||
| Illiterate (reference) | 13 (6.8) | 23 (11.0) | … | … | ||
| Incomplete elementary school | 77 (40.5) | 91 (43.5) | 1.27 (0.80–2.002) | 0.29 | ||
| Continuing | ||||||
| Univariate Analysis | Multivariate Analysis | Univariate Analysis | Multivariate Analysis | Univariate Analysis | Multivariate Analysis | Univariate Analysis |
| Complemente elementary school | 56 (29.5) | 46 (22.0) | 1.52 (0.45–2.43) | 0.052 | ||
| Complete high school | 39 (20.5) | 41(19.6) | 1.35 (0.83–2.20) | 0.21 | ||
| College degree | 5 (2.6) | 8 (3.8) | 1.07 (0.47–2.40) | 1.0 | ||
| Brickhouse | 60 (31.6) | 71 (33.9) | 0.95 (0.78–1.16) | 0.61 | ||
| Sewerage system | 85 (44.7) | 83 (39.7) | 1.10 (0.91–1.51) | 0.31 | ||
| Number of household members, median (quartiles) | 5.5 (4.5–7) | 5.0 (3.0–7.5) | ||||
| Distance from the health unit, median (quartiles) | 2.5 (2.5–5.0) | 2.0 (2.0–5.5) | 0.52 | |||
| Habits and Customs | ||||||
| Tattoo Collective sports | 18 (9.4) 87 (45.7) | 24 (11.4) 93 (44.5) | 0.90 (0.68–1.20) 1.02 (0.84–1.23) | 0.62 0.80 | ||
| Earrings | 45 (32.3) | 23 (44.2) | 0.69 (0.44–1.10) | 0.17 | ||
| Skin pigmentation | 70 (36.8) | 76 (36.3) | 1.00 (0.83–1.22) | 0.92 | ||
| Urucum | 55 (29.0) | 68 (32.5) | 0.92 (0.75–1.12) | 0.50 | ||
| Jenipapo | 67 (35.2) | 38 (59.3) | 0.85 (0.68–1.08) | 0.22 | ||
| Number of daily baths, median (quartiles) | 3.5 (2.5–4.0) | 3.0 (2.0–4.0) | … | 0.04 * | ||
| Baths in the river | 61 (43.7) | 79 (37.8) | 0.88 (0.73–1.07) | 0.27 | ||
| Showers | 131 (68.9) | 135 (64.5) | 1.09 (0.90–1.32) | 0.35 | ||
| Use of medicinal herbs | 33 (17.) | 40 (19.1) | 0.94 (0.74–1.19) | 0.64 | ||
| Use of herbal drink for rituals | 1 (0.53) | 6 (2.87) | 0.60 (0.44–0.82) | 0.07 | ||
| Use of topical medicinal substances | 26 (40.6) | 38 (59.3) | 0.85 (0.68–1.08) | 0.22 | ||
| Drinking | 29 (15.2) | 32 (15.3) | 0.99 (0.77–1.29) | 0.98 | ||
| Smoking | 34 (17.8) | 42 (20.1) | 0.93 (0.74–1.17) | 0.57 | ||
| Clinical Variables | ||||||
| Diabetes | 8 (4.2) | 11 (5.2) | 0.90 (0.60–1.33) | 0.62 | ||
| Skin infections A | 3 (1.58) | 2 (0.96) | 1.31 (0.44–3.85) | 0.57 | ||
| Skin infections R | 6 (3.16) | 8 (3.83) | 0.91 (0.57–1.45) | 0.71 | ||
| Antibiotics | 22 (11.5) | 19 (9.0) | 1.14 (0.81–1.61) | 0.41 | ||
| Recent outpatient consultations | 32 (16.8) | 26 (12.4) | 1.19 (0.88–1.61) | 0.21 | ||
| Surgery | 17 (8.95) | 11 (5.26) | 1.35 (0.84–2.17) | 0.15 | ||
| Hospitalization | 27 (14.2) | 34 (16.2) | 0.92 (0.72–1.18) | 0.56 | ||
| Pneumonia | 1 (0.53) | 1 (0.48) | 1.04 (0.26–4.20) | 0.94 | ||
| Shanenawa | Puyanawas I | Puyanawas II | Kaxinawa | Kopenoti | Teregua | |
|---|---|---|---|---|---|---|
| Age | 21 (11–33) | 27 (11–38) | 27 (11–49) * | 20 (10–34) * | 27 (13–42) | 31 (13–54) * |
| Women | 71 (52.6%) | 24 (47.1%) | 29 (69.0%) | 28 (56%) | 40 (62.5%) | 30 (57.7%) |
| S. aureus | 78 (57.8%) | 21 (41.2%) | 21 (50.0%) | 16 (32.0%) * | 31 (48.4%) | 19 (36.5%) |
| MRSA | 3 (2.2%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Number of household members, median (quartiles) | 6 (4–8) | 5 (4–5) * | 4 (3–8) * | 6 (4–8) * | 4 (4–6) * | 4 (3–6) * |
| Number of baths, median (quartiles) | 3 (3–4) | 3 (3–4) | 4 (3–4) | 3 (3–4) | 2 (1–2) * | 2 (2–3) * |
| Baths in the river | 68 (50.4%) | 15 (29.4%) | 9 (21.4%) * | 43 (86.0%) * | 0 (0.0%) * | 0 (0.0%) * |
| Tattoo | 31 (23%) | 3 (5.9%) * | 1 (2.4%) * | 4 (8.0%) * | 0 (0.0%) * | 3 (5.8%) * |
| Skin pigmentation | 76 (56.3%) | 22 (43.1%) | 17 (40.5%) | 26 (52.0%) | 0 (0.0%) * | 0 (0.0%) * |
| Earrings | 1 (0.7%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (1.6%) | 2 (3.8%) |
| Smoking | 40 (29.6%) | 4 (7.8%) * | 7 (16.7%) | 10 (20.0%) | 7 (10.9%) * | 7 (13.5%) |
| Use of snuff for rituals | 1 (0.7%) | 1 (2.0) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Use of herbal drink for rituals | 1 (0.7%) | 6 (11.8%) * | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Use of medicinal herbs ** | 39 (28.9%) | 19 (37.3%) | 5 (11.9%) | 7 (14%) | 0 (0.0%) * | 1 (1.9%) * |
| Drinking | 39 (28.9%) | 5 (9.8%) * | 3 (7.1%) * | 9 (18.0%) | 3 (4.7%) * | 1 (1.9%) * |
| Collective sports | 80 (59.3%) | 31 (60.8%) | 20 (47.6%) | 33 (66%) | 5 (7.8%) * | 10 (19.2%) * |
| Brickhouse | 2 (1.5%) | 4 (7.8%) | 8 (19.0%) * | 3 (6.0%) | 63 (98.4%) * | 51 (98.1%) * |
| Income in R$, median (quartiles) | 632 (334–800) * | 600 (400–700) * | 670 (490–1000) * | 550 (200–684) * | 700 (550–750) * | 760 (700–1150) |
| Ethnicities—São Paulo & Acre | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Shanenawa (%) | Puyanawa I (%) | Kaxinawa (%) | Kopenoti (%) | Teregua (%) | Ashaninka (%) | Puyanawas II (%) | p Value | ||||||||
| Habits and Customs | Positive | Negative | Positive | Negative | Positive | Negative | Positive | Negative | Positive | Negative | Positive | Negative | Positive | Negative | |
| Skin pigmentation | 76 (52.1) | 59 (23.3) | 22 (15.1) | 29 (11.5) | 26 (17.8) | 24 (9.5) | - | 64 25.6) | - | 52 (20.6) | 5 (3.4) | - | 17 (11.6) | 25 (9.9) | <0.01 * |
| Use of medicinal herbs ** | 39 (53.4) | 96 (29.4) | 19 (26.0) | 32 (9.8) | 7 (9.6) | 43 (13.2) | - | 64 (19.6) | 1 (1.4) | 51 (15.6) | 2 (2.7) | 3 (0.9) | 5 (6.8) | 37 (11.3) | <0.01 * |
| Baths in the river | 68 (48.6) | 67 (25.9) | 15 (10.7) | 36 (13.9) | 43 (30.7) | 7 (2.7) | - | 64 (24.7) | - | 52 (20.1) | 5 (3.6) | - | 9 (6.4) | 33 (12.7) | <0.01 * |
| Number of baths, median (quartiles) | 3.2 (1–4) | 3.1 (1–4) | 3.2 (1–4) | 1.7 (1–4) | 2.1 (1–4) | 3.0 (2–4) | 3.5 (2–4) | ||||||||
| Income in R$, median (quartiles) | 696 (50–4000) | 781 (70–3550) | 505 (60–2000) | 810 (134–4000) | 1013 (300–2500) | 710 (250–1400) | 837 (649–4000) | <0.01 * | |||||||
| Household members, median (quartiles) | 6.3 (1–20) | 4.0 (1–9) | 6.0 (2–11) | 4.6 (1–9) | 3.9 (1–6) | 8.0 (8–8) | 5.2 (2–11) | <0.01 * | |||||||
| Univariate Analysis-Ethnicities—Acre & Sao Paulo State | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Shanenawa (%) | Puyanawa I (%) | Kaxinawa (%) | Ashaninka (%) | Puyanawas II (%) | Kopenoti-Sp (%) | Teregua-Sp (%) | |||||||||
| Genes | Positive | Negative | Positive | Negative | Positive | Negative | Positive | Negative | Positive | Negative | Positive | Negative | Positive | Negative | p Value |
| S. aureus (sau) | 78 (41.1) | 57 (27.3) | 21 (11.1) | 30 (14.4) | 16 (8.4) | 34 (16.3) | 4 (2.1) | 1 (0.5) | 21 (11.1) | 21 (10.0) | 31 (16.3) | 33 (15.8) | 19 (10.0) | 33 (15.8) | 0.01 * |
| Sea | 7 (38.9) | 72 (41.6) | 1 (5.6) | 20 (11.6) | - | 16 (9.2) | 1 (5.6) | 3 (1.7) | 1 (5.6) | 20 (11.6) | 6 (33.3) | 25 (14.5) | 2 (11.1) | 17 (9.8) | 0.27 |
| Seb | 10 (37.0) | 69 (42.1) | 1 (3.7) | 20 (12.2) | 3 (11.1) | 13 (7.9) | - | 4 (2.4) | 2 (7.4) | 19 (11.6) | 7 (25.9) | 24 (14.6) | 4 (14.8) | 15 (9.1) | 0.47 |
| Sec | 18 (47.4) | 61 (39.9) | 5 (13.2) | 16 (10.5) | 3 (7.9) | 13 (8.5) | 3 (7.9) | 1 (0.7) | 4 (10.5) | 17 (11.1) | 5 (13.2) | 26 (17.0) | - | 19 (12.4) | 0.03 * |
| Hla | 75 (40.8) | 4 (57.1) | 20 (10.9) | 1 (1.3) | 15 (8.2) | 1 (14.3) | 4 (2.2) | - | 20 (10.9) | 1 (14.3) | 31 (16.8) | - | 19 (10.3) | - | 0.81 |
| Hld | 66 (42.9) | 13 (35.1) | 13 (8.4) | 8 (21.6) | 11 (7.1) | 5 (13.5) | 3 (1.9) | 1 (2.7) | 14 (9.1) | 7 (18.9) | 29 (18.8) | 2 (5.4) | 18 (11.7) | 1 (2.7) | 0.02 * |
| PVL | 14 (38.9) | 65 (41.7) | 3 (8.3) | 18 (11.5) | 2 (5.6) | 14 (9.0) | 1 (2.8) | 3 (1.9) | 5 (13.9) | 16 (10.3) | 9 (25.0) | 22 (14.1) | 2 (5.6) | 18 (11.5) | 0.62 |
| Eta | 5 (71.4) | 74 (40.2) | - | 21 (11.4) | 1 (14.3) | 15 (8.2) | - | 4 (2.2) | - | 21 (11.4) | 1 (14.3) | 30 (16.3) | - | 19 (10.3) | 0.62 |
| Etd | 5 (38.5) | 74 (41.6) | - | 21 (11.8) | 2 (15.4) | 14 (7.9) | - | 4 (2.2) | - | 21 (11.8) | 6 (46.2) | 25 (14.0) | - | 19 (10.7) | 0.03 |
| TSST-1 | 1 (8.3) | 75 (43.6) | - | 21 (12.2) | - | 15 (8.7) | - | 3 (1.7) | - | 20 (11.6) | 4 (33.3) | 26 (15.1) | 7 (58.3) | 12 (7.0) | <0.01 * |
| icaA | 65 (41.4) | 14 (41.2) | 20 (12.7) | 1 (2.9) | 15 (9.6) | 1 (2.9) | - | 4 (11.8) | 20 (12.7) | 1 (2.9) | 22 (14.0) | 9 (26.5) | 15 (9.6) | 4 (11.8) | <0.01 * |
| icaD | 53 (38.1) | 26 (50.0) | 17 (12.2) | 4 (7.7) | 13 (9.4) | 3 (5.8) | 1 (0.7) | 3 (5.8) | 20 (14.4) | 1 (1.9) | 21 (15.1) | 10 (19.2) | 14 (10.1) | 10 (19.2) | 004 * |
| Variables Analyzed | ||
|---|---|---|
| Category | Description | Examples or Additional Information |
| Demographic | Gender, age | |
| Ethnicity | ||
| Income in R$ | ||
| Schooling | Illiterate, incomplete elementary school, complete elementary school, complete high school, college degree | |
| Type of housing | Brickhouse (house built with bricks and cement), houses made of wood/straw or rammed earth | |
| Sewerage system | ||
| Median number of household members | ||
| Distance from the health unit in kilometers | ||
| Habits and customs | Tattoo | |
| Collective sports | ||
| Earrings | ||
| Skin pigmentation | In general, indigenous peoples have the habit of body painting. In Brazil, dyes are made from natural compounds, such as Urucum and Jenipapo. These dyes remain on the skin for a period of 15 to 20 days. | |
| Urucum | ||
| Jenipapo | ||
| Number of daily baths | Indigenous people living in remote areas have the habit of bathing in the river, and they commonly take many baths throughout the day. | |
| Baths in the river | ||
| Use of medicinal herbs | ||
| Use of herbal drink for rituals | Ayahuasca | |
| Use of topical medicinal substances | ||
| Drinking | ||
| Smoking | Snuff, cigarette | |
| Clinical variables | Diabetes | |
| Skin infections A (in the last year) | ||
| Skin infections R (recent) | ||
| Antibiotic use | ||
| Recent outpatient consultations | ||
| Surgery | ||
| Hospitalization | ||
| Pneumonia | ||
| Virulence Factor | Gene | Primer | Sequence (5′-3′) | Product | Control | References |
|---|---|---|---|---|---|---|
| Enterotoxin A | Sea | SEA-1 | TTGGAAACGGTTAAAACGAA | 120 bp | ATCC13565 | [34,35] |
| SEA-2 | GAACCTTCCATCAAAAACA | |||||
| Enterotoxin B | seb | SEB-1 | TCGCATCAAACTGACAAACG | 478 bp | ATCC 14458 | [34,35] |
| SEB-2 | GACGGTACTCTATAAGTGCC | |||||
| Enterotoxin C | Sec | SEC-1 | GACATAAAAGCTAGGAATTT | 257 bp | ATCC 19095 | [34,35] |
| SEC-2 | AAATCGGATTAACATTATCC | |||||
| SEE-2 | TAACTTACCGTGGACCCTTC | |||||
| Toxic shock syndrome toxin 1 | Tst | TSST-1 | ATGGCAGCATCAGCTTGATA | 350 bp | N315 | [36] |
| TSST-2 | TTTCCAATAACCACCCGTTT | |||||
| Exfoliative toxin A | Eta | ETA-1 | CTAGTGCATTTGTTATTCAA | 119 bp | N5 | [37] |
| ETA-2 | TGCATTGACACCATAGTACT | |||||
| Exfoliative toxin B | Etb | ETB-1 | ACGGCTATATACATTCAATT | 200 bp | ZM | [37] |
| ETB-2 | TCCATCGATAATATACCTAA | |||||
| Exfoliative toxin D | Etd | ETD-1 | AACTATCATGTATCAAGG | 376 bp | [37] | |
| ETD-2 | CAGAATTTCCCGACTCAG | |||||
| Hemolysin α | hla | HLA-1 | CTGATTACTATCCAAGAAATTCGATTG | 209 bp | N315 | [38] |
| HLA-2 | CTTTCCAGCCTACTTTTTTATCAGT | |||||
| Hemolysin β | hlb | HLB-1 | GTGCACTTACTGACAATAGTGC | 309 bp | RN4420 | [38] |
| HLB-2 | GTTGATGAGTAGCTACCTTCAGT | |||||
| Hemolysin δ | hld | HLD-1 | ATGGCAGCAGATATCATTTC | 357 bp | N315 | [38] |
| HLD-2 | CGTGAGCTTGGGAGAGAC | |||||
| Biofilm | icaA | icaA-1 | ACA GTC GCT ACG AAA AGA AA | 103 bp | [39] | |
| icaA-2 | GGA AAT GCC ATA ATG AGA AC | |||||
| Biofilm | icaB | icaB-1 | CTG ATC AAG AAT TTA AAT CAC AAA | 302 bp | [39] | |
| icaB-2 | AAA GTC CCA TAA GCC TGT TT | |||||
| Biofilm | icaC | icaC-1 | TAA CTT TAG GCG CAT ATG TTT | 400 bp | [39] | |
| icaC-2 | TTC CAG TTA GGC TGG TAT TG | |||||
| Biofilm | icaD | icaD-1 | ATG GTC AAG CCC AGA CAG AG | 198 bp | [39] | |
| icaD-2 | CGT GTT TTC AAC ATT TAA TGC AA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abraão, L.M.; Fortaleza, C.M.C.B.; Camargo, C.H.; Barbosa, T.A.; Pereira-Franchi, E.P.L.; Riboli, D.F.M.; Hubinger, L.; Bonesso, M.F.; Medeiros de Souza, R.; Ribeiro de Souza da Cunha, M.d.L. Staphylococcus aureus and CA-MRSA Carriage among Brazilian Indians Living in Peri-Urban Areas and Remote Communities. Antibiotics 2023, 12, 862. https://doi.org/10.3390/antibiotics12050862
Abraão LM, Fortaleza CMCB, Camargo CH, Barbosa TA, Pereira-Franchi EPL, Riboli DFM, Hubinger L, Bonesso MF, Medeiros de Souza R, Ribeiro de Souza da Cunha MdL. Staphylococcus aureus and CA-MRSA Carriage among Brazilian Indians Living in Peri-Urban Areas and Remote Communities. Antibiotics. 2023; 12(5):862. https://doi.org/10.3390/antibiotics12050862
Chicago/Turabian StyleAbraão, Lígia Maria, Carlos Magno Castelo Branco Fortaleza, Carlos Henrique Camargo, Thaís Alves Barbosa, Eliane Patrícia Lino Pereira-Franchi, Danilo Flávio Moraes Riboli, Luiza Hubinger, Mariana Fávero Bonesso, Rodrigo Medeiros de Souza, and Maria de Lourdes Ribeiro de Souza da Cunha. 2023. "Staphylococcus aureus and CA-MRSA Carriage among Brazilian Indians Living in Peri-Urban Areas and Remote Communities" Antibiotics 12, no. 5: 862. https://doi.org/10.3390/antibiotics12050862
APA StyleAbraão, L. M., Fortaleza, C. M. C. B., Camargo, C. H., Barbosa, T. A., Pereira-Franchi, E. P. L., Riboli, D. F. M., Hubinger, L., Bonesso, M. F., Medeiros de Souza, R., & Ribeiro de Souza da Cunha, M. d. L. (2023). Staphylococcus aureus and CA-MRSA Carriage among Brazilian Indians Living in Peri-Urban Areas and Remote Communities. Antibiotics, 12(5), 862. https://doi.org/10.3390/antibiotics12050862









