Comparison of Intravenous Microdialysis and Standard Plasma Sampling for Monitoring of Vancomycin and Meropenem Plasma Concentrations—An Experimental Porcine Study
Abstract
1. Introduction
2. Results
2.1. Vancomycin
2.2. Meropenem
3. Discussion
4. Materials and Methods
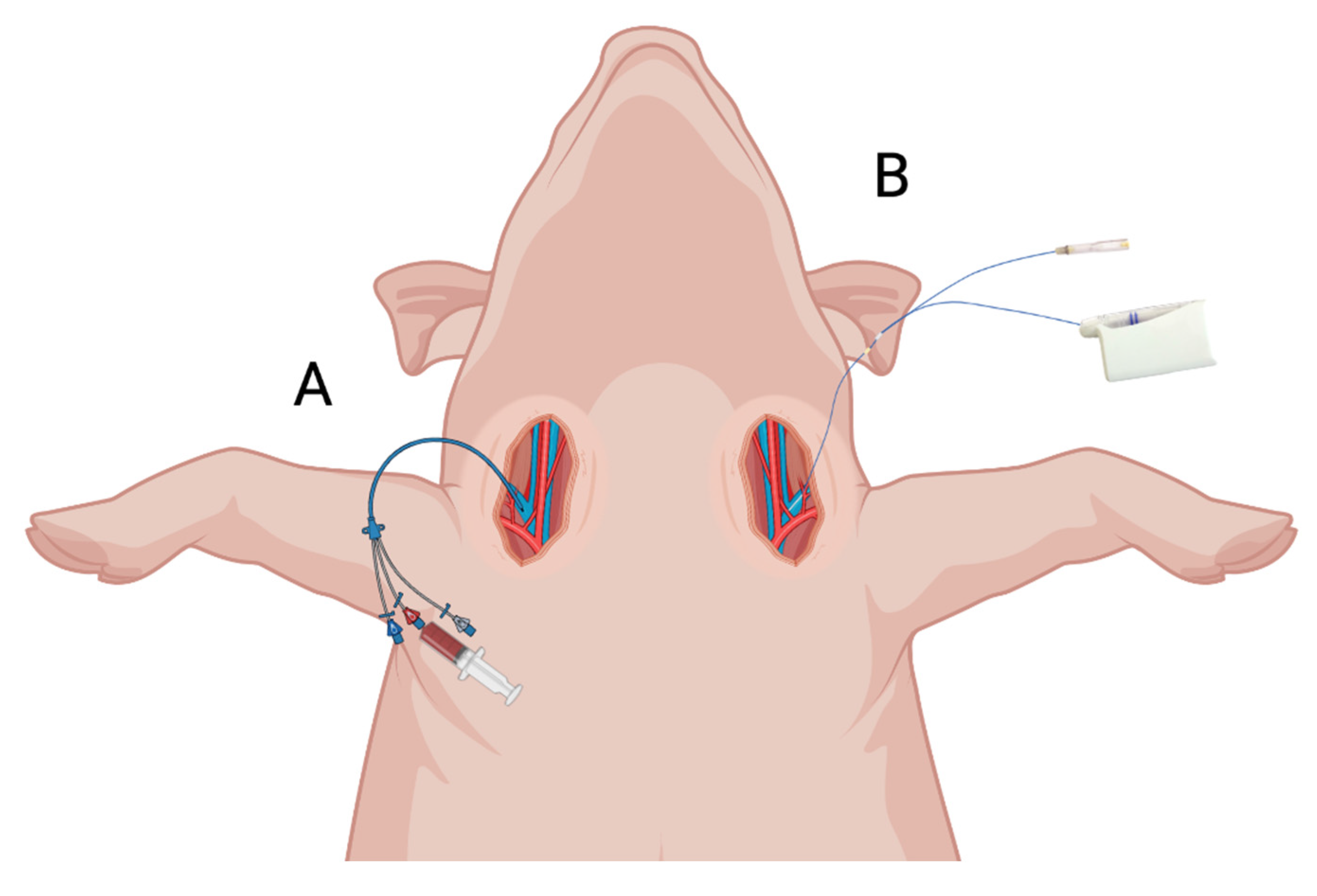
4.1. Microdialysis
4.2. Study Design, Anesthetic, and Intra-Vascular Procedure
4.3. Vancomycin and Meropenem Administration and Sampling Procedures
4.4. Quantification of Meropenem and Vancomycin Concentrations
4.5. Pharmacokinetic Analysis and Statistics
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Joukhadar, C.; Müller, M. Microdialysis: Current applications in clinical pharmacokinetic studies and its potential role in the future. Clin. Pharm. 2005, 44, 895–913. [Google Scholar] [CrossRef] [PubMed]
- Kehr, J. A survey on quantitative microdialysis: Theoretical models and practical implications. J. Neurosci. Methods 1993, 48, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Hammarlund-Udenaes, M. Microdialysis as an Important Technique in Systems Pharmacology—A Historical and Methodological Review. AAPS J. 2017, 19, 1294–1303. [Google Scholar] [CrossRef] [PubMed]
- Kho, C.M.; Enche Ab Rahim, S.K.; Ahmad, Z.A.; Abdullah, N.S. A Review on Microdialysis Calibration Methods: The Theory and Current Related Efforts. Mol. Neurobiol. 2017, 54, 3506–3527. [Google Scholar] [CrossRef] [PubMed]
- van der Mast, J.E.; Nijsten, M.W.; Alffenaar, J.C.; Touw, D.J.; Bult, W. In vitro evaluation of an intravenous microdialysis catheter for therapeutic drug monitoring of gentamicin and vancomycin. Pharmacol. Res. Perspect. 2019, 7, e00483. [Google Scholar] [CrossRef]
- al Jalali, V.; Bauer, M.; Wölfl-Duchek, M.; Sarhan, M.; Wicha, S.G.; Poschner, S.; Jäger, W.; König, F.; Male, C.; Zeitlinger, M. Pilot Pharmacokinetic Study in Healthy Adults Using Intravascular Microdialysis Catheters Modified for Use in Paediatric Patients to Assess Vancomycin Blood Levels. Clin. Pharmacokinet. 2022, 62, 77–87. [Google Scholar] [CrossRef]
- MDialysis. Available online: https://www.mdialysis.com (accessed on 27 March 2023).
- Stjernström, H.; Karlsson, T.; Ungerstedt, U.; Hillered, L. Chemical monitoring of intensive care patients using intravenous microdialysis. Intensive Care Med. 1993, 19, 423–428. [Google Scholar] [CrossRef]
- Elshoff, J.-P.; Läer, S. Development of an intravenous microdialysis method for pharmacokinetic investigations in humans. J. Pharmacol. Toxicol. Methods 2005, 52, 251–259. [Google Scholar] [CrossRef]
- O’Connell, M.T.; Tison, F.; Quinn, N.P.; Patsalos, P.N. Clinical drug monitoring by microdialysis: Application to levodopa therapy in Parkinson’s disease. Br. J. Clin. Pharmacol. 1996, 42, 765–769. [Google Scholar] [CrossRef]
- Johansen, M.J.; Newman, R.A.; Madden, T. The use of microdialysis in pharmacokinetics and pharmacodynamics. Pharmacotherapy 1997, 17, 464–481. [Google Scholar]
- Rybak, M.J.; Le, J.; Lodise, T.P.; Levine, D.P.; Bradley, J.S.; Liu, C.; Mueller, B.A.; Pai, M.P.; Wong-Beringer, A.; Rotschafer, J.C.; et al. Therapeutic monitoring of vancomycin for serious methicillin-resistant Staphylococcus aureus infections: A revised consensus guideline and review by the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists. Am. J. Health-Syst. Pharm. 2020, 77, 835–864. [Google Scholar] [CrossRef] [PubMed]
- Cusumano, J.A.; Klinker, K.P.; Huttner, A.; Luther, M.K.; Roberts, J.A.; LaPlante, K.L. Towards precision medicine: Therapeutic drug monitoring-guided dosing of vancomycin and β-lactam antibiotics to maximize effectiveness and minimize toxicity. Am. J. Health-Syst. Pharm. 2020, 77, 1104–1112. [Google Scholar] [CrossRef] [PubMed]
- Van Der Heggen, T.; Buyle, F.M.; Claus, B.; Somers, A.; Schelstraete, P.; De Paepe, P.; Vanhaesebrouck, S.; De Cock, P. Vancomycin dosing and therapeutic drug monitoring practices: Guidelines versus real-life. Int. J. Clin. Pharm. 2021, 43, 1394–1403. [Google Scholar] [CrossRef] [PubMed]
- Weber, S.; Tombelli, S.; Giannetti, A.; Trono, C.; O’Connell, M.; Wen, M.; Descalzo, A.B.; Bittersohl, H.; Bietenbeck, A.; Marquet, P.; et al. Immunosuppressant quantification in intravenous microdialysate—Towards novel quasi-continuous therapeutic drug monitoring in transplanted patients. Clin. Chem. Lab. Med. CCLM 2021, 59, 935–945. [Google Scholar] [CrossRef]
- Hage, C.; Mellbin, L.; Rydén, L.; Wernerman, J. Glucose Monitoring by Means of an Intravenous Microdialysis Catheter Technique. Diabetes Technol. Ther. 2010, 12, 291–295. [Google Scholar] [CrossRef]
- Rooyackers, O.; Blixt, C.; Mattsson, P.; Wernerman, J. Continuous glucose monitoring by intravenous microdialysis. Acta Anaesthesiol. Scand. 2010, 54, 841–847. [Google Scholar] [CrossRef]
- Gouëzel, C.; Lorne, E.; Bonnet, V.; Fradin, S.; Saplacan, V.; Gérard, J.L.; Hanouz, J.L.; Fellahi, J.L.; Fischer, M.O. Assessment of changes in lactate concentration with intravascular microdialysis during high-risk cardiac surgery using the trend interchangeability method. Br. J. Anaesth. 2017, 119, 1110–1117. [Google Scholar] [CrossRef]
- Rooyackers, O.; Blixt, C.; Mattsson, P.; Wernerman, J. Continuous glucose monitoring by intravenous microdialysis: Influence of membrane length and dialysis flow rate. Acta Anaesthesiol. Scand. 2013, 57, 214–219. [Google Scholar] [CrossRef]
- Fischer, M.-O.; Gouëzel, C.; Fradin, S.; Saplacan, V.; Gérard, J.-L.; Fellahi, J.-L.; Hanouz, J.-L. Assessment of changes in blood glucose concentration with intravascular microdialysis. J. Clin. Monit. Comput. 2018, 32, 1135–1142. [Google Scholar] [CrossRef]
- Saisho, Y.; Umeda, T. Continuous monitoring of unbound flomoxef levels in rat blood using microdialysis and its new pharmacokinetic analysis. Chem. Pharm. Bull. 1991, 39, 808–810. [Google Scholar] [CrossRef]
- Yang, H.; Wang, Q.; Elmquist, W.F. The Design and Validation of a Novel Intravenous Microdialysis Probe: Application to Fluconazole Pharmacokinetics in the Freely-Moving Rat Model. Pharm. Res. 1997, 14, 1455–1460. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Codina, M.; Wicha, S.G.; Wulkersdorfer, B.; Al Jalali, V.; Van Os, W.; Vossen, M.G.; Bauer, M.; Lackner, E.; Dorn, C.; Zeitlinger, M. Comparison of ultrafiltration and microdialysis for ceftriaxone protein-binding determination. J. Antimicrob. Chemother. 2023, 78, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Xin, H.-L.; He, X.-R.; Li, W.; Zhou, Z.-D.; Zhang, S.; Wang, G.-J. The effect of borneol on the concentration of meropenem in rat brain and blood. J. Asian Nat. Prod. Res. 2014, 16, 648–657. [Google Scholar] [CrossRef]
- Fei, Y.; Wu, S.; Wang, Y.; Shen, F.; Fan, G. A fast and high-sensitivity liquid chromatography–tandem mass spectrometry method combined with in vivo microdialysis for quantification of meropenem in rabbits with sepsis under the simultaneous infusion of total parenteral nutrition: Application to a pharmacokinetic study. Biomed. Chromatogr. 2021, 35, e5100. [Google Scholar] [CrossRef] [PubMed]
- Schroepf, S.; Burau, D.; Muench, H.-G.; Derendorf, H.; Zeitlinger, M.; Genzel-Boroviczény, O.; Adam, D.; Kloft, C. Microdialysis sampling to monitor target-site vancomycin concentrations in septic infants: A feasible way to close the knowledge gap. Int. J. Antimicrob. Agents 2021, 58, 106405. [Google Scholar] [CrossRef]
- Verbeeck, R.K. Blood microdialysis in pharmacokinetic and drug metabolism studies. Adv. Drug Deliv. Rev. 2000, 45, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Schneider, F.; Gessner, A.; El-Najjar, N. Efficacy of Vancomycin and Meropenem in Central Nervous System Infections in Children and Adults: Current Update. Antibiotics 2022, 11, 173. [Google Scholar] [CrossRef]
- Vittrup, S.Ø.; Hanberg, P.; Knudsen, M.B.; Tøstesen, S.K.; Kipp, J.O.; Hansen, J.; Jørgensen, N.P.; Stilling, M.; Bue, M. Tibial bone and soft-tissue concentrations following combination therapy with vancomycin and meropenem—Evaluated by microdialysis in a porcine model. Bone Jt. Res. 2022, 11, 112–120. [Google Scholar] [CrossRef]
- Vittrup, S.; Stilling, M.; Hanberg, P.; Tøstesen, S.K.; Knudsen, M.B.; Kipp, J.O.; Bue, M. Concentrations of co-administered vancomycin and meropenem in the internal dead space of a cannulated screw and in cancellous bone adjacent to the screw—Evaluated by microdialysis in a porcine model. Injury 2022, 53, 2734–2740. [Google Scholar] [CrossRef]
- Chaurasia, C.S.; Müller, M.; Bashaw, E.D.; Benfeldt, E.; Bolinder, J.; Bullock, R.; Bungay, P.M.; De Lange, E.C.; Derendorf, H.; Elmquist, W.F.; et al. AAPS-FDA workshop white paper: Microdialysis principles, application and regulatory perspectives. Pharm. Res. 2007, 24, 1014–1025. [Google Scholar] [CrossRef]
- Biorender. Available online: https://biorender.com (accessed on 27 March 2023).
- Bue, M.; Hanberg, P.; Tøttrup, M.; Thomassen, M.B.; Birke-Sørensen, H.; Thillemann, T.M.; Andersson, T.L.; Søballe, K. Vancomycin concentrations in the cervical spine after intravenous administration: Results from an experimental pig study. Acta Orthop. 2018, 89, 683–688. [Google Scholar] [CrossRef] [PubMed]
- Hanberg, P.; Lund, A.; Søballe, K.; Bue, M. Single-dose pharmacokinetics of meropenem in porcine cancellous bone determined by microdialysis. Bone Jt. Res. 2019, 8, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Bue, M.; Birke-Sørensen, H.; Thillemann, T.M.; Hardlei, T.F.; Søballe, K.; Tøttrup, M. Single-dose pharmacokinetics of vancomycin in porcine cancellous and cortical bone determined by microdialysis. Int. J. Antimicrob. Agents 2015, 46, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Hanberg, P.; Öbrink-Hansen, K.; Thorsted, A.; Bue, M.; Tøttrup, M.; Friberg, L.E.; Hardlei, T.F.; Søballe, K.; Gjedsted, J. Population Pharmacokinetics of Meropenem in Plasma and Subcutis from Patients on Extracorporeal Membrane Oxygenation Treatment. Antimicrob. Agents Chemother. 2018, 62, e02390-17. [Google Scholar] [CrossRef]

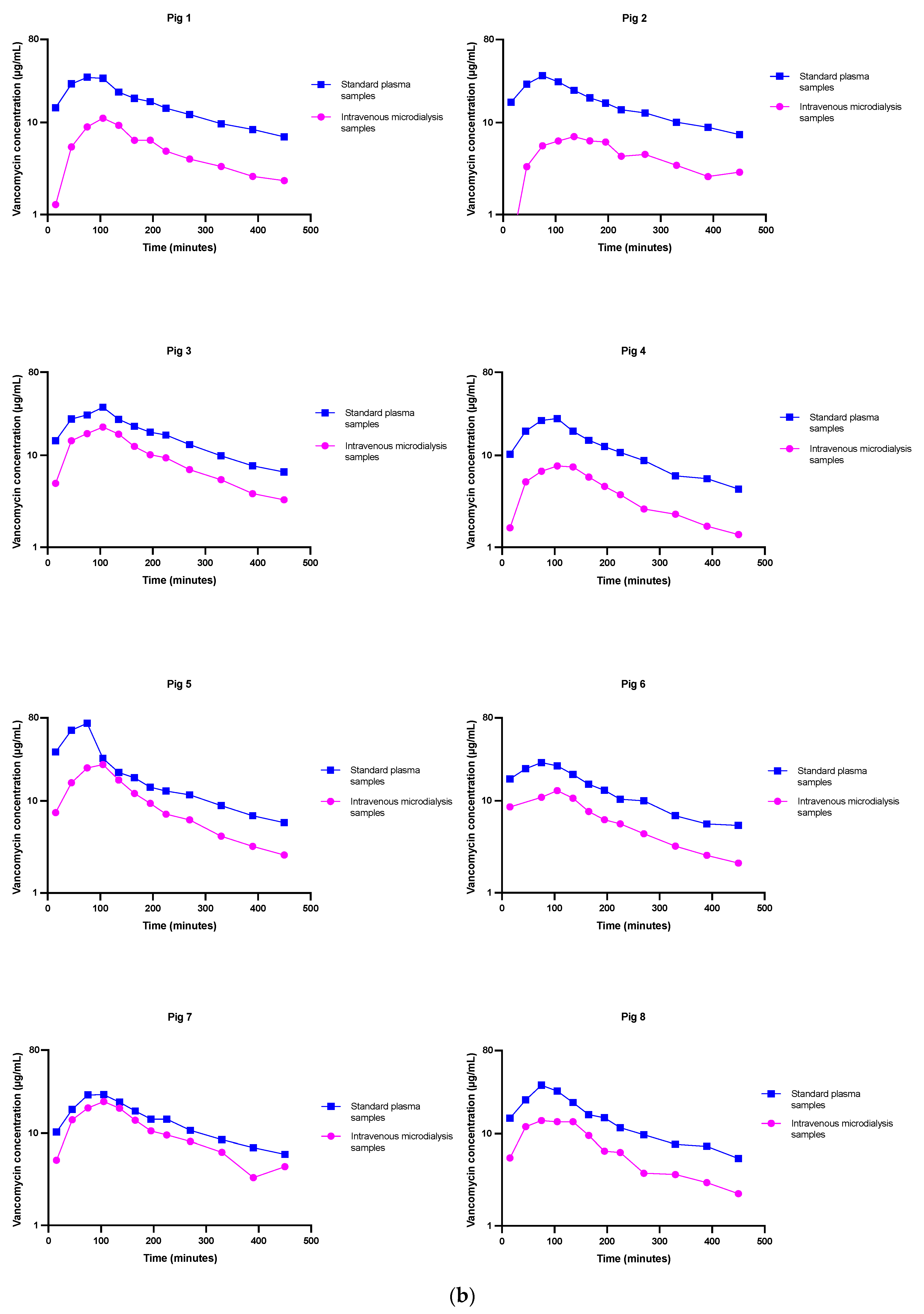


| Vancomycin | Standard Plasma Samples | Intravenous Microdialysis Samples | Difference between Methods |
|---|---|---|---|
| AUC0–8h, min µg/mL | 7014 (5779; 8249) | 2874 (1639; 4109) | −4140 (−5202; −3077) |
| Cmax, µg/mL | 36 (24; 49) | 14 (2; 26) | −22 (−35; −97) |
| T1/2, min | 197 (124; 270) | 242 (162; 322) | 45 (−55; 146) |
| Tmax, min | 85 (72; 98) | 110 (97; 123) | 25 (4.3; 46) |
| Meropenem | Standard Plasma Samples | Intravenous Microdialysis Samples | Difference between Methods |
|---|---|---|---|
| AUC0–8h, min µg/mL | 2980 (2437; 3523) | 1501 (958; 2044) | −1479 (−2209; 749) |
| Cmax, µg/mL | 69 (50; 88) | 29 (10; 47) | −40 (−66; −15) |
| T1/2, min | 44 (39; 49) | 36 (32; 41) | −7.6 (−14; 1.6) |
| Tmax, min | 15 (7; 23) | 20 (12; 28) | 5 (−8; 18) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lilleøre, J.G.; Vittrup, S.; Tøstesen, S.K.; Hanberg, P.; Stilling, M.; Bue, M. Comparison of Intravenous Microdialysis and Standard Plasma Sampling for Monitoring of Vancomycin and Meropenem Plasma Concentrations—An Experimental Porcine Study. Antibiotics 2023, 12, 791. https://doi.org/10.3390/antibiotics12040791
Lilleøre JG, Vittrup S, Tøstesen SK, Hanberg P, Stilling M, Bue M. Comparison of Intravenous Microdialysis and Standard Plasma Sampling for Monitoring of Vancomycin and Meropenem Plasma Concentrations—An Experimental Porcine Study. Antibiotics. 2023; 12(4):791. https://doi.org/10.3390/antibiotics12040791
Chicago/Turabian StyleLilleøre, Johanne Gade, Sofus Vittrup, Sara Kousgaard Tøstesen, Pelle Hanberg, Maiken Stilling, and Mats Bue. 2023. "Comparison of Intravenous Microdialysis and Standard Plasma Sampling for Monitoring of Vancomycin and Meropenem Plasma Concentrations—An Experimental Porcine Study" Antibiotics 12, no. 4: 791. https://doi.org/10.3390/antibiotics12040791
APA StyleLilleøre, J. G., Vittrup, S., Tøstesen, S. K., Hanberg, P., Stilling, M., & Bue, M. (2023). Comparison of Intravenous Microdialysis and Standard Plasma Sampling for Monitoring of Vancomycin and Meropenem Plasma Concentrations—An Experimental Porcine Study. Antibiotics, 12(4), 791. https://doi.org/10.3390/antibiotics12040791








