Provision of Microbiology, Infection Services and Antimicrobial Stewardship in Intensive Care: A Survey across the Critical Care Networks in England and Wales
Abstract
1. Introduction
- Microbiology services and surveillance: access to and input by microbiology and infection prevention and control specialists.
- Antibiotic prescription practices.
- The availability and use of diagnostics and biomarkers to influence antibiotic de-escalation and duration of antibiotics for common infections leading to ICU admissions.
- Availability of data management systems related to antibiotic use.
2. Methods
3. Results
3.1. Demographics
3.2. Availability of Microbiology Services and Surveillance
3.3. Antibiotic Prescribing
3.4. Local Antibiotic Consumption Data
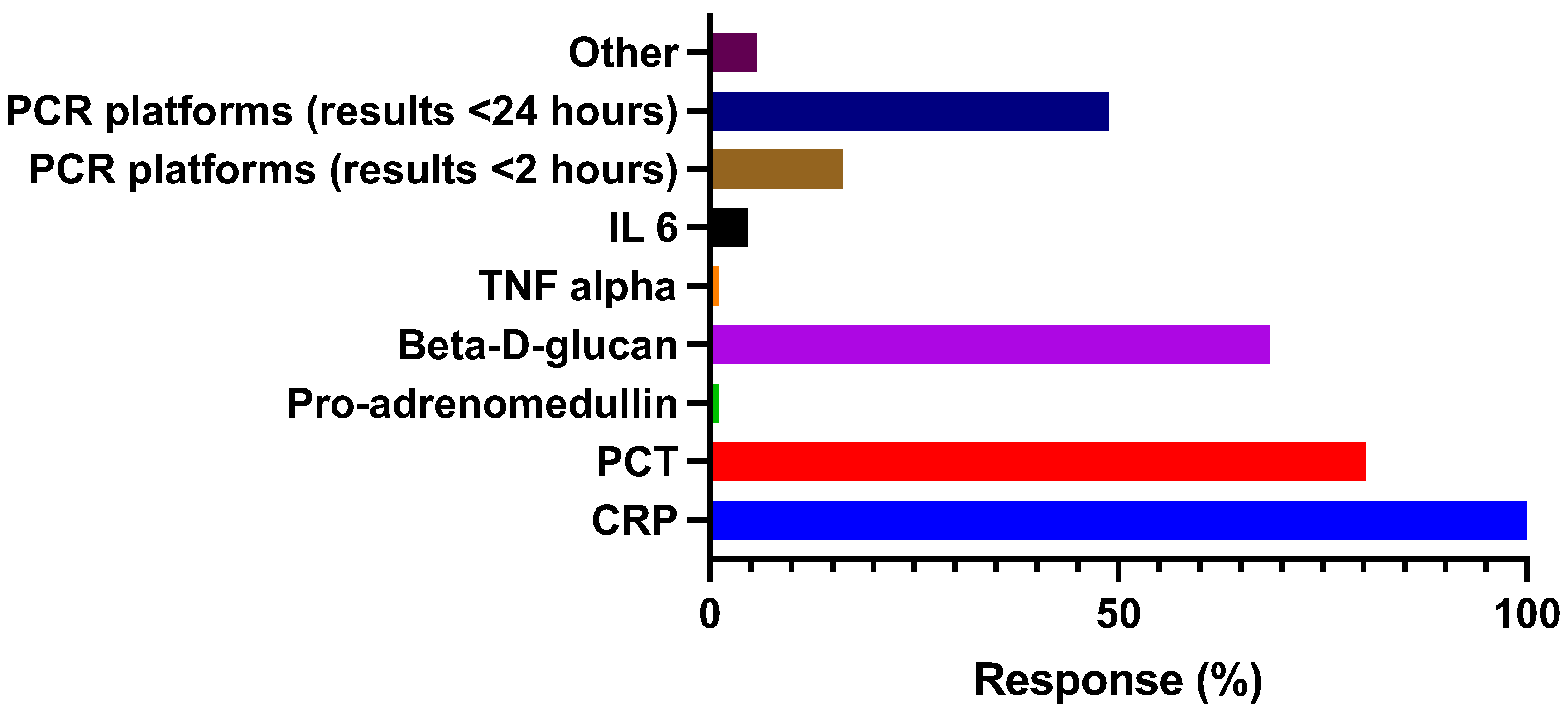
3.5. Routine Access to Biomarkers and Rapid Molecular Diagnostics
3.6. Audit and Participation in Clinical Research
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; Mcintyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Crit. Care Med. 2021, 49, 1063–1143. [Google Scholar] [CrossRef]
- Vincent, J.L.; Rello, J.; Marshall, J.; Silva, E.; Anzueto, A.; Martin, C.D.; Moreno, R.; Lipman, J.; Gomersall, C.; Sakr, Y.; et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA 2009, 302, 2323–2329. [Google Scholar] [CrossRef] [PubMed]
- Kollef, M.H.; Bassetti, M.; Francois, B.; Burnham, J.; Dimopoulos, G.; Garnacho-Montero, J.; Lipman, J.; Luyt, C.E.; Nicolau, D.P.; Postma, M.J.; et al. The intensive care medicine research agenda on multidrug-resistant bacteria, antibiotics, and stewardship. Intensive Care Med. 2017, 43, 1187–1197. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; Regional Office for Europe. Antimicrobial Stewardship Interventions: A Practical Guide; World Health Organization. Regional Office for Europe, 2021.
- Gilbert, D.N. Influence of an infectious diseases specialist on ICU multidisciplinary rounds. Crit. Care Res. Pract. 2014, 2014, 307817. [Google Scholar] [CrossRef] [PubMed]
- Available online: http://www.surveymonkey.com (accessed on 1 April 2023).
- Available online: https://www.acprc.org.uk/resources/critical-care/critical-care-networks/ (accessed on 1 April 2023).
- World Health Organization. Global Action Plan on Antimicrobial Resistance; World Health Organization: Geneva, Switzerland, 2015.
- Menéndez, R.; Ferrando, D.; Vallés, J.M.; Vallterra, J. Influence of deviation from guidelines on the outcome of community-acquired pneumonia. Chest 2002, 122, 612–617. [Google Scholar] [CrossRef] [PubMed]
- Frei, C.R.; Attridge, R.T.; Mortensen, E.M.; Restrepo, M.I.; Yu, Y.; Oramasionwu, C.U.; Ruiz, J.L.; Burgess, D.S. Guideline-concordant antibiotic use and survival among patients with community-acquired pneumonia admitted to the intensive care unit. Clin. Ther. 2010, 32, 293–299. [Google Scholar] [CrossRef]
- Lim, W.S.; Baudouin, S.V.; George, R.C.; Hill, A.T.; Jamieson, C.; Le Jeune, I.; Macfarlane, J.T.; Read, R.C.; Roberts, H.J.; Levy, M.L.; et al. British Thoracic Society guidelines for the management of community acquired pneumonia in adults: Update 2009. Thorax 2009, 64, 1–55. [Google Scholar] [CrossRef]
- Aardema, H.; Lisotto, P.; Kurilshikov, A.; Diepeveen, J.R.; Friedrich, A.W.; Sinha, B.; de Smet, A.M.G.; Harmsen, H.J. Marked Changes in Gut Microbiota in Cardio-Surgical Intensive Care Patients: A Longitudinal Cohort Study. Front. Cell. Infect. Microbiol. 2020, 9, 467. [Google Scholar] [CrossRef]
- Delannoy, M.; Agrinier, N.; Charmillon, A.; Degand, N.; Dellamonica, J.; Leone, M.; Pulcini, C.; Novy, E. Implementation of antibiotic stewardship programmes in French ICUs in 2018: A nationwide cross-sectional survey. J. Antimicrob. Chemother. 2019, 74, 2106–2114. [Google Scholar] [CrossRef]
- Maechler, F.; Schwab, F.; Geffers, C.; Meyer, E.; Leistner, R.; Gastmeier, P. Antibiotic stewardship in Germany: A cross-sectional questionnaire survey of 355 intensive care units. Infection 2014, 42, 119–125. [Google Scholar] [CrossRef]
- Binda, F.; Tebano, G.; Kallen, M.; Oever, J.T.; Hulscher, M.; Schouten, J.; Pulcini, C. Nationwide survey on hospital antibiotic stewardship programs in France. Med. Mal. Infect. 2019, 50, 414–422. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Antimicrobial Stewardship: Systems and Processes for Effective Antimicrobial Medicine Use; National Institute for Health and Care Excellence: London, UK, 2015. [Google Scholar]
- Dawson, S.J. The role of the infection control link nurse. J. Hosp. Infect. 2003, 54, 251–257. [Google Scholar] [CrossRef]
- Dekker, M.; Mansfeld, R.V.; Vandenbroucke-Grauls, C.M.; Lauret, T.E.; Schutijser, B.C.; de Bruijne, M.C.; Jongerden, I.P. Role perception of infection control link nurses; a multi-centre qualitative study. J. Infect. Prev. 2022, 23, 93–100. [Google Scholar] [CrossRef]
- Dekker, M.; Jongerden, I.P.; Van Mansfeld, R.; Ket, J.C.F.; Van Der Werff, S.D.; Vandenbroucke-Grauls, C.M.J.E.; De Bruijne, M.C. Infection control link nurses in acute care hospitals: A scoping review. Antimicrob. Resist. Infect. Control 2019, 8, 20. [Google Scholar] [CrossRef]
- Laurent, C.; Rodriguez-Villalobos, H.; Rost, F.; Strale, H.; Vincent, J.-L.; Deplano, A.; Struelens, M.J.; Byl, B. Intensive Care Unit Outbreak of Extended-Spectrum β-Lactamase–Producing Klebsiella Pneumoniae Controlled by Cohorting Patients and Reinforcing Infection Control Measures. Infect. Control Hosp. Epidemiol. 2008, 29, 517–524. [Google Scholar] [CrossRef]
- Austin, D.J.; Bonten, M.J.M.; Weinstein, R.A.; Slaughter, S.; Anderson, R.M. Vancomycin-resistant enterococci in intensive-care hospital settings: Transmission dynamics, persistence, and the impact of infection control programs. Proc. Natl. Acad. Sci. USA 1999, 96, 6908–6913. [Google Scholar] [CrossRef] [PubMed]
- Weier, N.; Tebano, G.; Thilly, N.; Demoré, B.; Pulcini, C.; Zaidi, S.T.R. Pharmacist participation in antimicrobial stewardship in Australian and French hospitals: A cross-sectional nationwide survey. J. Antimicrob. Chemother. 2017, 73, 804–813. [Google Scholar] [CrossRef] [PubMed]
- Pulcini, C.; Binda, F.; Lamkang, A.S.; Trett, A.; Charani, E.; Goff, D.A.; Harbarth, S.; Hinrichsen, S.L.; Levy-Hara, G.; Mendelson, M.; et al. Developing core elements and checklist items for global hospital antimicrobial stewardship programmes: A consensus approach. Clin. Microbiol. Infect. 2019, 25, 20–25. [Google Scholar] [CrossRef]
- Cairns, K.A.; Doyle, J.S.; Trevillyan, J.M.; Horne, K.; Stuart, R.L.; Bushett, N.; Yong, M.K.; Kelley, P.G.; Dooley, M.J.; Cheng, A.C. The impact of a multidisciplinary antimicrobial stewardship team on the timeliness of antimicrobial therapy in patients with positive blood cultures: A randomized controlled trial. J. Antimicrob. Chemother. 2016, 71, 3276–3283. [Google Scholar] [CrossRef]
- Lesprit, P.; Landelle, C.; Girou, E.; Brun-Buisson, C. Reassessment of intravenous antibiotic therapy using a reminder or direct counselling. J. Antimicrob. Chemother. 2010, 65, 789–795. [Google Scholar] [CrossRef]
- Engels, D.R.; Evans, G.E.; McKenna, S.M. Effect on duration of antimicrobial therapy of removing and reestablishing an automatic stop date policy. Can. J. Hosp. Pharm. 2004, 57, 214–219. [Google Scholar]
- Murray, C.; Shaw, A.; Lloyd, M.; Smith, R.P.; Fardon, T.C.; Schembri, S. and Chalmers, J.D. A multidisciplinary intervention to reduce antibiotic duration in lower respiratory tract infections. J. Antimicrob. Chemother. 2014, 69, 515–518. [Google Scholar] [CrossRef] [PubMed]
- Connor, D.M.; Binkley, S.; Fishman, N.O.; Gasink, L.B.; Linkin, D.; Lautenbach, E. Impact of automatic orders to discontinue vancomycin therapy on vancomycin use in an antimicrobial stewardship program. Infect. Control Hosp. Epidemiol. 2007, 28, 1408–1410. [Google Scholar] [CrossRef] [PubMed]
- Barlam, T.F.; Cosgrove, S.E.; Abbo, L.M.; MacDougall, C.; Schuetz, A.N.; Septimus, E.J.; Srinivasan, A.; Dellit, T.H.; Falck-Ytter, Y.T.; Fishman, N.O.; et al. Implementing an Antibiotic Stewardship Program: Guidelines by the Infectious Diseases Society of America and the Society of Healthcare Epidemiology of America. Clin. Infect. Dis. 2016, 62, 51–77. [Google Scholar] [CrossRef]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2016. Intensive Care Med. 2017, 43, 304–377. [Google Scholar] [CrossRef]
- Busch, L.M.; Kadri, S.S. Antimicrobial Treatment Duration in Sepsis and Serious Infections. J. Infect. Dis. 2020, 222, 142–155. [Google Scholar] [CrossRef]
- Uranga, A.; España, P.P.; Bilbao, A.; Quintana, J.M.; Arriaga, I.; Intxausti, M.; Lobo, J.L.; Tomás, L.; Camino, J.; Nuñez, J.; et al. Duration of antibiotic treatment in community-acquired pneumonia: A multicenter randomized clinical trial. JAMA Intern. Med. 2016, 176, 1257–1265. [Google Scholar] [CrossRef]
- Chastre, J.; Wolff, M.; Fagon, J.Y.; Chevret, S.; Thomas, F.; Wermert, D.; Clementi, E.; Gonzalez, J.; Jusserand, D.; Asfar, P.; et al. Comparison of 8 vs. 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: A randomized trial. JAMA 2003, 290, 2588–2598. [Google Scholar] [CrossRef] [PubMed]
- Kalil, A.C.; Metersky, M.L.; Klompas, M.; Muscedere, J.; Sweeney, D.A.; Palmer, L.B.; Napolitano, L.M.; O’Grady, N.P.; Bartlett, J.G.; Carratalà, J.; et al. Management of Adults with Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin. Infect. Dis. 2016, 63, e61–e111. [Google Scholar] [CrossRef]
- Mermel, L.A.; Allon, M.; Bouza, E.; Craven, D.E.; Flynn, P.; O’Grady, N.P.; Raad, I.I.; Rijnders, B.J.; Sherertz, R.J.; Warren, D.K. Diagnosis and Management of Intravascular Catheter-Related Infection: 2009 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2009, 49, 1–45. [Google Scholar] [CrossRef]
- Blot, S.; De Waele, J.J. Critical issues in the clinical management of complicated intra-abdominal infections. Drugs 2005, 65, 1611–1620. [Google Scholar] [CrossRef]
- Bassetti, M.; Righi, E.; Ansaldi, F.; Merelli, M.; Scarparo, C.; Antonelli, M.; Garnacho-Montero, J.; Diaz-Martin, A.; Palacios-Garcia, I.; Luzzati, R.; et al. A multicenter multinational study of abdominal candidiasis: Epidemiology, outcomes and predictors of mortality. Intensive Care Med. 2015, 41, 1601–1610. [Google Scholar] [CrossRef]
- Sawyer, R.G.; Claridge, J.A.; Nathens, A.B.; Rotstein, O.D.; Duane, T.M.; Evans, H.L.; Cook, C.H.; O’Neill, P.J.; Mazuski, J.E.; Askari, R.; et al. Trial of short-course antimicrobial therapy for intraabdominal infection. N. Engl. J. Med. 2015, 372, 1996–2005. [Google Scholar] [CrossRef]
- Peterson, J.; Kaul, S.; Khashab, M.; Fisher, A.C.; Kahn, J.B. A double-blind, randomized comparison of levofloxacin 750 mg once-daily for five days with ciprofloxacin 400/500 mg twicedaily for 10 days for the treatment of complicated urinary tract infections and acute pyelonephritis. Urology 2008, 71, 17–22. [Google Scholar] [CrossRef]
- Sandberg, T.; Skoog, G.; Hermansson, A.B.; Kahlmeter, G.; Kuylenstierna, N.; Lannergård, A.; Otto, G.; Settergren, B.; Ekman, G.S. Ciprofloxacin for 7 days versus 14 days in women with acute pyelonephritis: A randomised, open-label and double-blind, placebo-controlled, non-inferiority trial. Lancet 2012, 380, 484–490. [Google Scholar] [CrossRef] [PubMed]
- Powell, N.; Howard, P.; Llewelyn, M.J.; Szakmany, T.; Albur, M.; Bond, S.E.; Euden, J.; Brookes-Howell, L.; Dark, P.; Hellyer, T.P.; et al. Use of Procalcitonin during the First Wave of COVID-19 in the Acute NHS Hospitals: A Retrospective Observational Study. Antibiotics 2021, 10, 516. [Google Scholar] [CrossRef] [PubMed]
- Heesom, L.; Rehnberg, L.; Nasim-Mohi, M.; Jackson, A.I.; Celinski, M.; Dushianthan, A.; Cook, P.; Rivinberg, W.; Saeed, K. Procalcitonin as an antibiotic stewardship tool in COVID-19 patients in the intensive care unit. J. Glob. Antimicrob. Resist. 2020, 22, 782–784. [Google Scholar] [CrossRef] [PubMed]
- Poole, S.; Tanner, A.R.; Naidu, V.V.; Borca, F.; Phan, H.; Saeed, K.; Grocott, M.P.; Dushianthan, A.; Moyses, H.; Clark, T.W. Molecular point-of-care testing for lower respiratory tract pathogens improves safe antibiotic de-escalation in patients with pneumonia in the ICU: Results of a randomised controlled trial. J. Infect. 2022, 22, 00533-3. [Google Scholar] [CrossRef]
- Carbonne, A.; Arnaud, I.; Maugat, S.; Marty, N.; Dumartin, C.; Bertrand, X.; Bajolet, O.; Savey, A.; Fosse, T.; Eveillard, M.; et al. National multidrug-resistant bacteria (MDRB) surveillance in France through the RAISIN network: A 9 year experience. J. Antimicrob. Chemother. 2013, 68, 954–959. [Google Scholar] [CrossRef]

| 1–3 Days | 4–5 Days | 6–7 Days | 8–10 Days | 11–14 Days | |
|---|---|---|---|---|---|
| Septic shock | 6.1% | 19.5% | 58.5% | 11.0% | 4.9% |
| Community acquired pneumonia | 2.4% | 53.0% | 36.2% | 6.0% | 2.4% |
| Ventilator associated pneumonia | 1.2% | 50.6% | 40.0% | 4.7% | 3.5% |
| Hospital acquired pneumonia | 1.2% | 45.9% | 45.9% | 4.7% | 2.3% |
| Proven line infection * | 18.8% | 18.8% | 42.4% | 10.6% | 9.4% |
| Primary-intraabdominal sepsis ** | 2.4% | 33.7% | 36.2% | 18.1% | 9.6% |
| Community acquired urinary sepsis (lower UTI) | 22.6% | 50.0% | 21.4% | 2.4% | 3.6% |
| Community acquired urinary sepsis (upper UTI) | 4.8% | 34.5% | 41.7% | 8.3% | 10.7% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Catton, T.; Umpleby, H.; Dushianthan, A.; Saeed, K. Provision of Microbiology, Infection Services and Antimicrobial Stewardship in Intensive Care: A Survey across the Critical Care Networks in England and Wales. Antibiotics 2023, 12, 768. https://doi.org/10.3390/antibiotics12040768
Catton T, Umpleby H, Dushianthan A, Saeed K. Provision of Microbiology, Infection Services and Antimicrobial Stewardship in Intensive Care: A Survey across the Critical Care Networks in England and Wales. Antibiotics. 2023; 12(4):768. https://doi.org/10.3390/antibiotics12040768
Chicago/Turabian StyleCatton, Tim, Helen Umpleby, Ahilanandan Dushianthan, and Kordo Saeed. 2023. "Provision of Microbiology, Infection Services and Antimicrobial Stewardship in Intensive Care: A Survey across the Critical Care Networks in England and Wales" Antibiotics 12, no. 4: 768. https://doi.org/10.3390/antibiotics12040768
APA StyleCatton, T., Umpleby, H., Dushianthan, A., & Saeed, K. (2023). Provision of Microbiology, Infection Services and Antimicrobial Stewardship in Intensive Care: A Survey across the Critical Care Networks in England and Wales. Antibiotics, 12(4), 768. https://doi.org/10.3390/antibiotics12040768





