Abstract
Chitosan derivatives and composites are the next generation polymers for biomedical applications. With their humble origins from the second most abundant naturally available polymer chitin, chitosan is currently one of the most promising polymer systems, with wide biological applications. This current review gives a bird’s eye view of the antimicrobial applications of chitosan composites and derivatives. The antiviral activity and the mechanisms behind the inhibitory activity of these components have been reviewed. Specifically, the anti-COVID-19 aspects of chitosan composites and their derivatives have been compiled from the existing scattered reports and presented. Defeating COVID-19 is the battle of this century, and the chitosan derivative-based combat strategies naturally become very attractive. The challenges ahead and future recommendations have been addressed.
1. Introduction
The interest in natural and man-made polymers for their use in biomedicine and related applications has seen a steady rise in recent years. Numerous polymers, irrespective of their biodegradability, have been examined in this respect. Some of the most preferred synthetic polymers were polylactic acid or PLA, polylactic-co-glycolic acid or PLGA, poly-caprolactone or PCL, acrylic polymers, and polyethylene glycol or PEG, whereas the most researched natural polymers were chitosan, gelatin, dextran, cellulose, starch, alginate, and hyaluronic acid [1,2,3]. The naturally occurring polysaccharide, chitin, was first extracted by French scientist Henri Braconnot from mushrooms and, thereby, laid the foundation for carbohydrate-based polymers [4]. Chitin was obtained from insects in the 1830s, before its successful transformation to chitosan in the late 1850s [4]. Deacetylation (removal of CH3-CO group) transforms chitin to chitosan [5], a special cationic polymer that is soluble in weak acids. The level of deacetylation determines how soluble chitosan will be. More than 80–85% of the product must be deacetylated in order to produce a soluble product [6,7,8].
Although chitosan is regarded to be eco-friendly and generally regarded as a benign and non-irritating substance, the FDA has not yet approved its usage in pharmaceutical compounds owing to a number of restrictions [9]. In the USA and European and Asian countries such as Finland, Italy, and Japan, it is legally in use as an obesity control supplement. The chitosan monograph was added to the US National Formulary in 2008 and the European Pharmacopoeia in 2011 [10]. It is currently recognized as a secure (GRAS) excipient for treating wounds. In addition, the FDA has approved a number of non-categorized chitosan devices for blood clotting and wound dressing [11]. Among them are Axiostat®, Celox™, and ChitoFlex®, chitosan-based hemostatic bandages (currently marketed in numerous countries) that hasten blood clotting following an injury or trauma. Another brand named TraumaStat® is a fabric-based dressing that helps surgical wound reparation, with ease to paste and remove at will [12]. Some products such as Anscare, which is a chitosan bandage in Taiwan, is available mainly to treat external wounds. In addition to having the property of initiating faster blood clots, chitosan possesses numerous biomedical applications: antibacterial [13,14,15], gene delivery [16], bio-composites [17,18,19,20], nanoengineering [21,22,23], and excipients [8,24]. Structurally chitosan is a positively charged polysaccharide, which makes it easier for it to adhere to the surfaces of the bacterium. By optimizing physical properties such as wettability, the hydrophobicity of chitosan is enhanced, helping it penetrate the lipid bilayer of the bacterium and affecting the integrity of the cell wall. Eventually, lysis in bacteria results due to cytoplasmic leakage [25,26].
Antimicrobial resistance (AMR) to drugs has raised the need for seeking alternative treatment possibilities. This need is further compounded by pragmatic limiting factors such as the difficulty in finding alternative antimicrobial medicines in consideration of emanating factors pertaining to the rapid rise of antimicrobial resistance, alternative antibiotic availability, and side effects of incessant antibiotics usage [27]. Some of the biggest threats to public health are the looming risk of increasing bacterial resistance to antibiotics and the faster spread of its resistant strain, slow progress of a new class of antibiotic development, and abuse of existing antibiotics [28,29]. All these factors act as inhibiting factors leading to therapeutic failures. The investigation of the antipathogenic of natural occurring compounds is significant since synthesis and clinical trials of alternative antibiotics are in high demand [30]. Abundance-wise chitosan is the second best available natural polymer, and it has already proven its utility in the medical, pharmaceutical, food industrial, and techno-textiles industries due to its exceptional properties of bio-friendliness (in terms of compatibility and toxicity), combined with eliciting other favorable physiological properties such as antioxidant, anti-cancerous, and immune-modulatory functions [31,32].
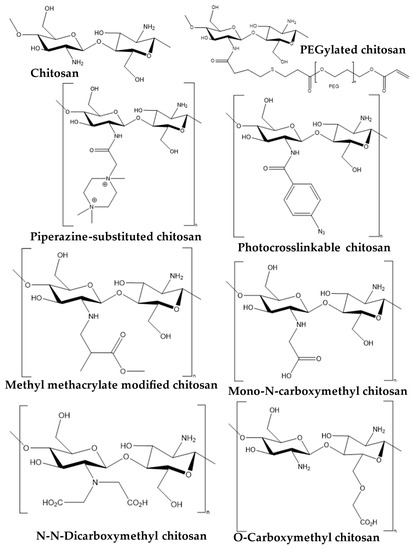
One of the barriers to the therapeutic application of chitosan is its limited solubility at body or physiological pH [33,34]. Various strategies have been sought after, in order to optimize the chitosan chemistry and to resolve the low solubility issue. Typically, chemical alterations in the structure are done at three active sites, including one at the main amine (-NH2-) group and two hydroxyl groups (-OH) on the glucosamine unit. Based on attached chemical moieties, the characteristics of chitosan have been manipulated. However, the modification in the main amine is crucial for successful transfection through the cell membrane. It has been observed that chitosan’s chemical alteration enhances its medical applications and pharmacological capabilities. For instance, p-azidebenzoic acid addition at the main amine of chitosan increases cohesiveness to the cell membrane, thereby enhancing the rate of healing abilities [35], whereas bactericidal potential of chitosan is increased through PEGylation [35,36]. For the respiratory administration of siRNA, piperazine-substituted chitosan that is soluble in polar solvents is utilized [37]. Moreover, the addition of methyl methacrylate moiety within chitosan has shown to be useful for drug delivery application [38]. Similarly, N-carboxymethyl chitosan has wider applications in biomedicine owing to its enhanced binding and water-soluble properties [4,39,40]. Several studies have examined the potency and biosafety of chitosan for use in applications, ranging from orthopedic tissue engineering [41,42,43] to targeted delivery [16,44], biomaterials [17,45], and medicinal excipients [24,32,46]. Equally there are reviews focusing on toxicity associated with chitosan [10] and chemically-modified chitosan [38,47,48,49,50].
COVID-19 or SARS-CoV belongs to the family of Coronaviridae that consists of single-stranded RNA viruses. Its symptoms include gastrointestinal, pulmonary, hepatological, and neurological symptoms, the effects of which span from moderate to lethal. The size of the COVID-19 virus measures roughly 60–160 nm in diameter including the periphery under an electron microscopy. An envelope of coronavirus consists of a structure containing single-stranded RNA (+ssRNA) with a genome size of 27–32 kb, with a 5’-cap structure and a 3’-poly A tail that interacts with the nucleoprotein. As a result, when the virus enters the recipient, it invades the cells by binding onto the ACE2 (angiotensin-converting enzyme) receptor on the cell’s surface through its surface-bound glycoprotein component (4–10). Consequently, after infection the RNA of virus is transferred into the host cell cytoplasm and begins replication involving the translation of two structural polyproteins. Replicated glycoprotein envelopes are stored in the Golgi complex or endoplasmic reticulum membrane. Finally, the nucleocapsid is created by combining genomic RNA and glycoprotein. Inside the Golgi complex, germination of viral particles takes place. Ultimately, the plasma membrane and the compartments containing the viral particles merge to discharge the virus. Currently, reverse transcription polymerase chain reaction (RT-PCR) kits and CT (computed tomography) scans taken at various angles in pulmonary area are being dominantly used to diagnose SARS-CoV-2 positive patients [51]. The drugs currently in use to treat COVID-19 are Remdesivir, Enoxaparin, Methyl Prednisolone, Dexamethasone, Tocilizumab, and Ivermectin (https://www.fda.gov/drugs/emergency-preparedness-drugs/coronavirus-covid-19-drugs (accessed on 4 February 2023).
In the following sections we present an overall perspective on the antiviral applications of chitosan and its derivatives. Chitosan composites and derivatives have been compiled and presented for the first time, specifically for anti-COVID-19 applications. The difficulties faced, its limitations, and suggestions for its future course have been presented. The obstacles facing the use of chitosan and the recommendations for its future have been briefly discussed in this review.
2. Snapshot of Antipathogenic Applications of Chitosan Composites and Its Derivatives
Chitosan is one of the compounds that has been predominantly studied for their various medicinal and biological functions. It has also been investigated as a potent antimicrobial agent that is effective against a large variety of microbes such as bacteria, viruses, and fungus [52]. In this section, we will present a snapshot of the specific antimicrobial applications of chitosan composites and derivatives. Chitosan has been demonstrated to exhibit fungicidal properties against Candida strains, which are responsible for a wide range of ailments in mammals, animals, and bacterial species. Similarly, chitosan has exhibited bactericidal activities against Staphylococcus aureus (gram-positive), E. coli (gram-negative) [53], and strains such as Bacillus megaterium, Salmonella typhimurium, and Pseudomonas fluorescens, to list a few [54]. Chitosan-bound linens are being tested in order to enhance quality of life by inhibiting Staphylococcus aureus growth when in contact with human skin. Various clinical testing is underway [55], with human trials [56]. A study is now being conducted on 165 subjects for testing the therapeutic potency of chitosan-based textile (DermaCura®, a brand that contains about 1% chitosan matrix) [56]. Apart from textiles, chitosan nanoparticle-loaded VESTA respirators were developed against pathogens. A clinical study (NCT04490200) (https://clinicaltrials.gov/ct2/show/NCT04490200 (accessed on 10 February 2023)) involving N95 masks with and without chitosan is underway on 700 clinical professionals to check for its effectiveness against COVID-19 infection, and whether the chitosan nanoparticles can adsorb and inactivate the virus with which come into contact. At Jinan Military General Hospital, 120 patients were enrolled in a clinical trial for anti-microbial chitosan dressing gel for the treatment of nonneoplastic epithelial diseases involving the skin and vulvar mucosa (NCT02890277) [57].
Right now, some of the notorious bacterial pathogens resisting antibiotic treatments are vancomycin-resistant S. aureus (VRSA), methicillin-resistant S. aureus (MRSA), methicillin-resistant S. epidermidis (MRSE), E. coli, vancomycin-resistant Enterococcus (VRE), Acinetobacter spp., Pseudomonas aeruginosa, and Klebsiella pneumoniae. Park et al. looked into the antibacterial effect of chitosan against drug immune Pseudomonas aeruginosa and S. aureus [58]. The findings demonstrated that all isolates of P. aeruginosa that were drug resistant, as well as some variants of S. aureus, were more susceptible to chitosan’s antibacterial activity [58]. Furthermore, an in vivo study of chitosan on mice that were infected by bacteria revealed a better survival rate and minimal bacterial colonization [58]. In another study, similar results of chitosan’s antibacterial potential against ATCC strains and E. faecalis have been noted [59]. In a cross comparison of available strains and clinical multi-resistant extracts, Costa et al. assessed the antibacterial effect of chitosan towards MSSA (methicillin-susceptible Staphylococcus aureus) and MRSA (methicillin-resistant Staphylococcus aureus). The findings demonstrated that methicillin resistance had no effect on chitosan’s activity. Additionally, MRSA seems more susceptible especially with a decrease in the molecular weight of chitosan [60]. Given the clinical significance and current treatment scenario for MRSA infections, these results are very positive. Acinetobacter spp. infections too pose grave concern as they have the extraordinary capacity to build resistance and spread in the hospital setting [61]. From this perspective, chitosan offers respite naturally, which makes its offer more attractive and appealing. In addition to chitosan itself, its derivatives and allied composites have also demonstrated their antimicrobial activity. In an attempt to combat P. aeruginosa, MRSA, and A. baumannii, Saito et al. produced chitosan conjugated with lysozyme-oligosaccharides to exert strong antibacterial activity [61]. Interestingly, the efficacy of chitosan nanofibers against multiple drug-resistant strains of Clostridium difficile was evaluated and found to be effective [62]. Zhang et al. [63] fabricated a chitosan nanoparticle encapsulated with antibacterial oils and tested its efficacy against multiple drug-resistant K. pneumoniae. The results suggested that chitosan with a lower molecular weight and deacetylation level of 75% tends to boost the bactericidal effects of oils [63]. Loading chitosan nanoparticles with drugs like cephalosporin, cefotaxime [64], and ceftriaxone for their application against isolates—including a wide range of multiple drug-resistant strains such as carbapenemase producing K. pneumoniae, E. coli, P. aeruginosa, and MRSA strains such as E. coli and P. aeruginosa [64]—has produced desirable antimicrobial properties. The findings showed significant improvement in antibacterial activity across various bacterial strains. Considering the current scenario of AMR, the fabrication of various novel chitosan derivatives-based drugs has become an extended application.
Chitosan of low molecular weight of about 70 kDa and an acetyl removal degree of about 75% showed promising antifungal efficacy [65]. A 15 kD chitosan-oligosaccharide with powerful synergistic actions against Candida spp. was described by Ganan et al., when used in conjunction with several antifungal medications such fluconazole, miconazole, voriconazole, and amphotericin B [66]. Lo et al. investigated the antifungal efficacy of chitosan by modifying the molecular weight and deacetylation degree in conjunction with drugs like caspofungin, fluconazole, and amphotericin B. A combination of chitosan and fluconazole produced impressive synergistic antifungal effects, while other antifungal drugs had no effect. In addition, chitosan and fluconazole worked well to treat drug-resistant strains of Candida species albicans and tropicalis strains [67]. The alarming incidence of fungal infections in recent times at a global scale is a serious concern, especially given their effect on vulnerable populations who already suffer from various diseases or disorders such as diabetes and are immunocompromised. Fungal infection, be it on its own or after initial bacterial/viral infections, creates a cascade of related issues, which worsens the outcome of treatment protocols [68,69]. The pathology reports of documented human deaths suggest over 90% lethality due to fungal infections attributed to the genus Candida, Pneumocystis, Aspergillus, and Cryptococcus [68]. According to the evidence in possession, fungi seem to be more vulnerable to chitosan’s antipathogenic activity than bacteria [14]. Chitosan’s fungicidal activity can be manipulated by varying factors like molecular weight, content or volume, formulation pH, and acetyl group removal level [67]. Based on the strain, factors such as deacetylation levels and their molecular weights vary and are able to affect its fungicidal effects [67]. Normally, chitosan concentrations between 1% and 5% were shown to guarantee optimum antifungal activity, especially at low pH [14,65]. The mechanism of chitosan’s fungicidal activity initiates rupturing of the fungal cell wall after its transfection across the yeast cell [70]. Chitosan antifungal effect against Candida spp. initiates through uptake of Ca2+, with efflux of K+ along with inhibition of respiration and other cell activity such as fermentation [70]. It must be noted that Candida species are the most frequently studied pathogenic yeast with respect to the fungicidal action of chitosan. The influence of the molecular weight of chitosan on 105 clinical Candida isolates, including their strains that were resistant to fluconazole, has been investigated. Results showed that chitosan had substantial antifungal effect, blocking >89.9% of the isolated strains. Additionally, chitosan demonstrated a similar antifungal effect at lower concentrations than fluconazole when evaluated on nine investigated patients [65]. However, the outcome of chitosan investigations in synergy with antifungal medications is contradictory. However, there is no doubt that it does possess strong antimicrobial attributes. Antimicrobial drugs have been delivered by controlled release mechanisms using chitin and its derivatives [71]. Pharmaceutical technology makes considerable use of chitin derivatives, including N-succinyl-chitosan, carboxymethyl-chitin, and hydroxyethyl-chitin [72]. More such systems have been developed by encapsulating several active principles with chitosan, including proteins and peptides, growth factors, anti-inflammatory chemicals, antibiotics, and molecules for anticancer therapy as well [73]. Thus, a lot has been achieved in the field of antimicrobial activity through chitosan and its derivates/composites.
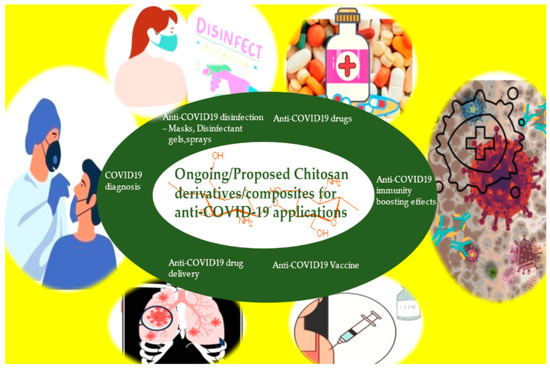
4. Anti-COVID-19 Applications of Chitosan Composites and Derivatives
During the pandemic, mutation strains of SARS-CoV-2/COVID-19 [129,130,131,132] have enhanced the risk of re-infection and undermine already built immunity and vaccination efficacy [133,134]. Alternately, vaccinations that induce broadly neutralizing antibodies could be developed [135,136]. About 23 COVID-19 vaccines were licensed under emergency conditions in humans by 2021, and the rest (about 329) were in clinical (111) or preclinical (218) stages [137]. These included inactivated whole viruses (such as CoronaVac and Covaxin), mRNA-loaded liposomes (such as BNT162b2 and mRNA-1273), adenovirus vectors (such as ChAdOx1 nCoV-19, CTII-nCoV, and Sputnik V), and virus-like particles (such as NVX-CoV2373) [138]. In phase 3 investigations, these vaccines demonstrated a 65–96% antiviral efficacy against illness and mortality [139,140,141,142,143]. The vaccinations work because the S protein extends from the virus’s surface and is recognized by angiotensin-converting enzyme 2, which enhances viral uptake [144]. Nonetheless, the specificity of vaccines towards S protein declines as a consequence of the rapid accumulation of mutations [145,146,147,148]. Mutations include L18F, D80A, D215G, and 242–244 in the N-terminal domain; K417N, E484K, and N501Y in the receptor-binding domain (RBD); and D614G and P681R in other places that sustain spike stability and function [149,150,151].
In light of the increasing incidence and mortality rates of COVID-19 infection worldwide, the development of treatment techniques has attracted the highest level of interest. The antiviral potential of marine resources is underutilized. Chitosan (polycarbohydrate) is a prevalent glycan that is bioactive and abundant in marine species. The structural availability of reactive amine/hydroxyl groups invoking minimum toxicity/allergenicity has caught attention to study the anti-SARS-CoV-2 activity of chitosan compound. Due to the strong docking affinity of the ligands (−6.0 to −6.6 kcal/mol) with SARS-CoV-2 spike protein RBD, N-benzyl-O-acetyl-chitosan, imino-chitosan, and sulfated chitosan oligosaccharides derivatives are ranked as promising antiviral candidates. In fact the results of the ADMET experiment are extremely favoring to conduct more clinical trials of the above mentioned chitosan compounds as an agent against SARS-CoV-2 treatment [152].
Milewska et al. created chitosan-based anti-coronavirus compounds that prevent in vitro and in vivo infection [113]. Indeed, investigation of the interaction between this chitosan derivative and the recombinant ectodomain of the S protein showed the development of polymer–protein complexes as a result of binding. They showed that the polymer inhibits the interaction between the spike protein of the coronavirus and the cellular receptor [113]. In 2020, the above group simulated cell culture models to simulate the coronavirus-replicating layer lining conductive airways. The model culture was loaded with virus and exposed to the chitosan compounds. The model investigation showed that the polymeric system successfully suppressed SARS-CoV-2 and MERS-CoV [153]. The combination of chitosan and DNA found to greatly reduce lung inflammation and boosts host antiviral mechanism. The intranasal delivery of a DNA vaccine containing SARS-CoV nucleocapsid protein and chitosan nanoparticles to present antigens to T cells by nasal-resident DCs has been tested [154]. This approach activates systemic IgG and nasal IgA antibodies targeting N protein of the virus, hence enhancing the immune response against SARS-CoV.
Milewska et al. studied the SARS-CoV-2 inhibitory factor of N-(2-hydroxypropyl)-3-trimethylammonium chitosan chloride (HTCC) and its hydrophobic derivative [113]. HCoV-NL63 and human murine virus were suppressed by these polymers. Extensive investigation into the pathways indicated that the chitosan polymer formed a compound with the ectodomain of the HCoV-spike NL63 protein without producing considerable cytotoxicity. In addition, it has been suggested that inhibition is entirely triggered by site-specific binding [155]. A later study on viral entry suppression by HTCC polymeric compound in the LLC-MK2 cell line revealed intriguing results of polymer disrupting the receptor cell signaling with a spike protein via aggregation of spike [114]. Additionally, it eliminates the colocalization of ACE-2 receptors with viruses. The spectrum of suppressed human coronavirus (HCoV-OC43, HCoV-229E, HCoV-NL63, and HCoV-HKU1) infections varied according to the degree of substitution. Later, the efficacy of HTCC was tested in pathogenic coronaviruses, MERS-CoV, and SARS-CoV-2 using Vero and Vero E6 cell lines and the human airway epithelial (HAE) model. The study report revealed that HTCC has the ability to suppress viral reproduction especially on the SARS-CoV-2 virus. Moreover, electrostatic attraction with viral spike protein significantly restricted the uptake of viruses into susceptible cells [156].
Even after recovery, COVID-19-caused respiratory disease is currently a major worldwide health concern. Since infected patients’ lung lesions are still characterized by acute respiratory distress syndrome, including alveolar septal edema, pneumonia, hyperplasia, and hyaline membranes, it is vital to uncover other options that can overcome the inflammatory process and improve COVID-19 treatments. The polyphenolic extracts were integrated into bovine serum albumin (BSA) molecules, which were then coated with chitosan, a polymer that promotes mucoadhesion [157].
The efficiency of the silver/chitosan coating system is boosted in combination with adhering curcumin from Curcuma longa rhizome extract, resulting in nanosilver particles. Curcuma longa rhizome aids in the nanobiotechnological manufacture of silver/chitosan nanocomposite antibacterial surface coating. Antiviral drugs including nanosilver and curcumin have a synergistic effect that minimizes contamination. A simple coating technology is suited to the maximum number of exposed contact surfaces with metallic, ceramic, polymeric, or wooden surfaces, etc. Handles, rails, switches, touch displays, keyboards, tabletops, etc. than self-sterilize and function normally. They are implementing preventative measures against the COVID-19 infection linked to SARS-CoV-2 [158].
This work includes systematic research of the synthesis of chitosan hydrogels with dicarboxylic acids (malic and glutaric acid) and their detailed characterization (Fourier transform infrared spectroscopy, determination of cross-linking efficiency, rheological studies, thermal analysis, and swelling kinetics). Without additives or catalysts, chitosan hydrogels can be chemically cross-linked using malic or glutaric acid, as demonstrated by the results. In addition, the ability of hydrogels to adsorb three separate ACE2 inhibitors as active medicinal components has been investigated. The API content and mucoadhesive property of hydrogels can provide a suitable foundation for the development of a nasal formulation to reduce the risk of SARS-CoV 2 infection [136,159]. Extensive literature reviews on the biocompatibility of chitosan nanoparticles allow this experiment to be conducted quickly on humans. Moreover, it is easy to link antibodies to chitosan, hence we chose these nanoparticles [160].
Using chitosan/polycaprolactone bioink, the primary purpose of this study was to construct a biocompatible and mechanically sound 3D-printed scaffold for lung tissue engineering. Several 3D printing compositions were analyzed using the Design-Expert program. The selected scaffolds were tested for their ability to support MRC-5 cell growth, proliferation, and migration. Based on the results, the average diameter of the chitosan/polycaprolactone filaments was determined to be 360 mm. The printability was determined by the chitosan concentration, whereas polycaprolactone content had no effect. Despite the fact that the scaffolds’ polycaprolactone content may be modified, they exhibited promising swelling, degradation, and mechanical properties [161].
To determine a specific treatment for COVID-19, silymarin–chitosan nanoparticles (Sil–CNPs) were evaluated for their potential as antiviral agents against SARS-CoV-2 using in silico and in vitro techniques. Sil and CNPs were docked with SARS-CoV-2 spike protein using AutoDock Vina. Both Vero and Vero E6 cell lines were tested for cytotoxicity using the MTT assay. Using crystal violet, the IC50 was determined at doses of 0.91, 12.2, and 0.80 mg/mL for CNPs, Sil, and Sil–CNPs, respectively, in virucidal/replication studies. These findings reveal the antiviral activity of Sil–CNPs against SARS [162].
Electrospinning the fibers directly on the surface of the textile or fabric to create a composite fabric is an easy way for incorporating electrospun fibers into textile. This process of putting fibers on fabric is inexpensive and reduces manufacturing procedures, making it suited for mass production. In addition, electrospun chitosan nanofibers were effectively mass-produced, and their large-scale production with the Force spinning method was previously described [163].
The cytokine storm syndrome (CSS) leads to high patient mortality, especially those who have preconditions like ALI (acute lung infection) and ARDS (acute respiratory distress syndrome) resulting from COVID-19. Currently, no standard treatment model exists for ALI- or ALI/ARDS-triggered CSS. Consequently, the development of potent drugs and therapeutic protocols for CSS associated with ALI/ARDS is the need of the hour. Due to the targeted capability of drug delivery to organs like lungs via nasal inhalation, chitosan compounds holds promises for treating inflammatory lung diseases. Enhancing the absorption and bioavailability of poor water-soluble medications to therapeutic level in the nasal-mucosal region offers more promises in the treatment of ALI/ARDS. For example, anti-inflammatory hesperidin-loaded chitosan nanoparticles (HPD/NPs) were nasally administered to inflamed lungs. In an inflammatory context, HPD/NPs demonstrated higher cellular absorption in vitro and in vivo compared to HPD alone. In a mouse model, HPD/NPs greatly reduced lung damage by decreasing the levels of pro-inflammatory cytokines and decreased vascular permeability [164].
As a result of its better nanoscale characteristics, nanocomposites have garnered considerable interest in a variety of applications. Sol-gel technology was utilized to synthesize a chitosan–zeolite–ZnO nanocomposite, and a molecular docking study was conducted to assess its antiviral efficacy against SARS-CoV-2 [165].
Sun et al. (2009) manufactured biotinylated chitosan nanoparticles encapsulated with bovine coronavirus N-protein [166]. They examined the effectiveness of their vaccine against SARS-CoV-2. Researchers employed a bifunctional fusion protein vector to selectively target dendritic cells. The increase in mucosal IgA and systemic IgG against N-protein suggests that chitosan is a viable carrier for gene transfer [166,167]. Plasmid DNA encoding the nucleocapsid of SARS-CoV-2 was delivered intranasally through chitosan nanoparticles. This stimulates the release of SARS-CoV-2 spike protein, which competes with live coronavirus for ACE2 receptor binding. The results suggested that mice produce significant quantities of IgA and IgG. Chitosan reduces the breakdown of DNA vaccines, and its cationic nature enhances DNA binding. In addition, the mucoadhesive characteristics of chitosan stimulate its usage as a mucosal delivery adjuvant [168,169,170]. Table 1 summarizes the anti-COVID-19 applications of chitosan composites/derivatives.

Table 1.
Anti-COVID 19 applications of chitosan composites/derivatives.
5. Future Perspective and Recommendations
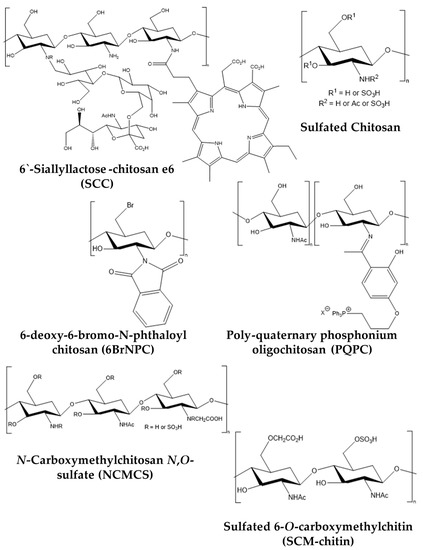
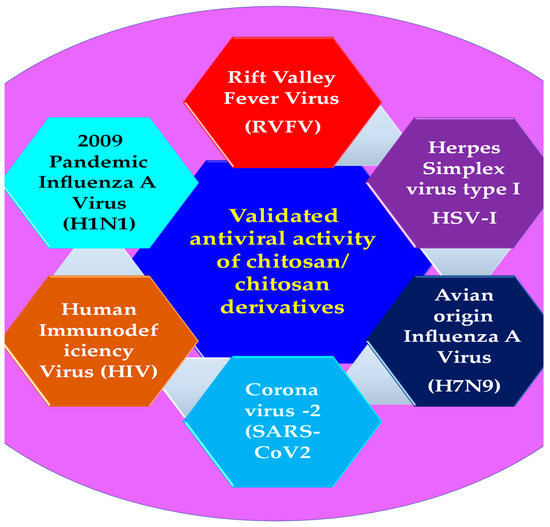
Figure 3 outlines the various facets of Anti-COVID-19 challenges that chitosan derivatives have been demonstrated to address. We have reviewed the various pioneering antiviral applications of chitosan and its derivatives, specifically anti-COVID-19 applications. Their antiviral properties depended on molecular weight, deacetylation, chitosan concentration, and ambient pH. This review shows that chitosan can be used to make broad-spectrum antiviral drugs. Chitosan’s antiviral action is improved by conjugating with hydroxypropyl trimethylammonium, sulphate, carboxymethyl, bromine, sialyllactose, peptide, and phosphonium moieties. Chitosan conjugates including HTCC, sulfated chitosan, SCM-chitin, NCMCS, 6BrNPC, and SCC have broad-spectrum antiviral action against human coronavirus, HIV, herpes simplex virus, influenza virus, NDV, human papillomavirus, and F-MuLV. Their antiviral activity relies on molecular weight, acetylation, conjugate substitution, and location. Chitosan monomeric residues have substituents. For nanomedical purposes, resultant conjugates have been mixed with silver nanoparticles and other antiviral drugs [125].
At effective in vitro therapeutic dosages, chitosan and its derivatives have negligible cytotoxicity. Chitosan and its derivatives are being studied as antiviral treatments in vitro. However, cell culture studies may not fully account for their antiviral actions in organs and complex systems within animals. To understand chitosan-based therapeutics’ potential and side effects, in vivo testing is needed.
Chitosan may inhibit SARS-CoV-2 by attaching to the spike glycoprotein trimer cavity [171]. SARS-CoV-2, an enveloped virus, can be treated with chitosan-based treatments that take into account the structure-activity relationship of chitosan derivatives substituted with carboxymethyl, sulphate, bromine, N-(2-hydroxypropyl)-3-trimethylammonium, phthaloyl, and sialyl-lactose moieties that are active against other enveloped viral variations. SARS-CoV-2-specific optimization studies must optimize molecular weight, degree of polymerization, acetylation, degree, and site of conjugate substitution of chitosan that will provide the greatest antiviral effect against SARS-CoV-2. Further, conjugating chitosan with optimal antiviral characteristics by other anti-SARS-CoV-2 ligands may confer additive or synergistic effects and greater effectiveness in inhibiting SARS-CoV-2 replication.
Pandemic preparations include accelerating vaccine research and reusing approved antivirals and other medications [175]. COVID-19 may spread too quickly with such a method. Since the medicine may not function against a mutation, developing an antiviral treatment for a single virus may not be worthwhile [175]. The Omicron version SARS-CoV-2 mutated quickly. Thus, a broad-spectrum antiviral technique will be the next-generation remedy for COVID-19 and other new viruses. This strategy could enable viable treatments to dramatically improve pandemic preparedness in early outbreaks. These antiviral chitosan compounds are broad-spectrum. They may create novel anti-SARS-CoV-2 therapies in the future. Currently, only a few laboratory experiments support the broad-spectrum efficacy of chitosan derivatives. More validated and optimized studies, supported by clinical trials, are needed.
Chitosan-based nanomedicines have various advantages that potentially give target-specific and cost-effective treatments for respiratory disorders such asthma, COPD, lung cancer, pneumonia, COVID-19, and others. Chitosan-based nanomedicines can be made in solid, liquid, or gel form and directly affect lungs. Nanomedicines can efficiently enter the respiratory system, target the lungs, and continually release API from the vehicles, making them vital in treating respiratory illnesses. Despite its benefits, few nanomedicines have been employed clinically for daily usage. Chitosan derivative-based nanomedicines could boost antiviral capabilities, another topic for research. Value-added chitosan derivative medicinal compounds are few. Chitosan is a stable and effective pharmacological excipient because of its solubility, stability, gene transport to the lungs, and controlled release of medicines, proteins, and peptides. This natural resource has plenty to be utilized. This review encourages researchers to expand chitosan derivatives and composites for anti-COVID-19 uses and pharmaceutical formulations.
6. Conclusions
The various antiviral activities of chitosan composites and derivatives were discussed. Their mode of action and the list of chitosan derivatives that have been proven for their antiviral effects were listed. The anti-COVID 19 potential of chitosan composites and derivatives was summarized. The gaps in the existing knowledge and the recommendations for future direction have been put forth.
Author Contributions
M.M., J.G. and S.S.C.P. prepared the original draft, and revisions; I.S., participated in the review, revisions, and funding. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Fonte, P.; Araújo, F.; Silva, C.; Pereira, C.; Reis, S.; Santos, H.A.; Sarmento, B. Polymer-Based Nanoparticles for Oral Insulin Delivery: Revisited Approaches. Biotechnol. Adv. 2015, 33, 1342–1354. [Google Scholar] [CrossRef]
- Elsabee, M.Z.; Abdou, E.S. Chitosan Based Edible Films and Coatings: A Review. Mater. Sci. Eng. C Mater. Biol. Appl. 2013, 33, 1819–1841. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, U.; Sharma, R.; Gupta, M.; Vyas, S.P. Is Nanotechnology a Boon for Oral Drug Delivery? Drug Discov. Today 2014, 19, 1530–1546. [Google Scholar] [CrossRef]
- Muzzarelli, R.A.A.; Boudrant, J.; Meyer, D.; Manno, N. Current Views on Fungal Chitin/Chitosan, Human Chitinases, Food Preservation, Glucans, Pectins and Inulin: A Tribute to Henri Braconnot, Precursor of the Carbohydrate polymers science, on the chitin bicentennial. Carbohydrate 2012, 87, 995–1012. [Google Scholar] [CrossRef]
- Sivashankari, P.R.; Prabaharan, M. Deacetylation Modification Techniques of Chitin and Chitosan. In Chitosan Based Biomaterials; Jennings, J.A., Bumgardner, J.D., Eds.; Woodhead Publishing: Cambridge, UK, 2017; Volume 1, pp. 117–133. ISBN 9780081002308. [Google Scholar]
- Xia, Z.; Wu, S.; Chen, J. Preparation of Water Soluble Chitosan by Hydrolysis Using Hydrogen Peroxide. Int. J. Biol. Macromol. 2013, 59, 242–245. [Google Scholar] [CrossRef]
- Lu, S.; Song, X.; Cao, D.; Chen, Y.; Yao, K. Preparation of Water-Soluble Chitosan. J. Appl. Polym. Sci. 2004, 91, 3497–3503. [Google Scholar] [CrossRef]
- Ilium, L. Chitosan and Its Use as a Pharmaceutical Excipient. Pharm. Res. 1998, 15, 1326–1331. [Google Scholar] [CrossRef]
- Kean, T.; Thanou, M. Biodegradation, Biodistribution and Toxicity of Chitosan. Adv. Drug Deliv. Rev. 2010, 62, 3–11. [Google Scholar] [CrossRef]
- Bellich, B.; D’Agostino, I.; Semeraro, S.; Gamini, A.; Cesàro, A. “The Good, the Bad and the Ugly” of Chitosans. Mar. Drugs 2016, 14, 99. [Google Scholar] [CrossRef]
- Wedmore, I.; McManus, J.G.; Pusateri, A.E.; Holcomb, J.B. A Special Report on the Chitosan-Based Hemostatic Dressing: Experience in Current Combat Operations. J. Trauma 2006, 60, 655–658. [Google Scholar] [CrossRef]
- Arnaud, F.; Teranishi, K.; Okada, T.; Parreño-Sacdalan, D.; Hupalo, D.; McNamee, G.; Carr, W.; Burris, D.; McCarron, R. Comparison of Combat Gauze and TraumaStat in Two Severe Groin Injury Models. J. Surg. Res. 2011, 169, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Carlson, R.P.; Taffs, R.; Davison, W.M.; Stewart, P.S. Anti-Biofilm Properties of Chitosan-Coated Surfaces. J. Biomater. Sci. Polym. Ed. 2008, 19, 1035–1046. [Google Scholar] [CrossRef] [PubMed]
- Kong, M.; Chen, X.G.; Xing, K.; Park, H.J. Antimicrobial Properties of Chitosan and Mode of Action: A State of the Art Review. Int. J. Food Microbiol. 2010, 144, 51–63. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Mu, H.; Zhang, W.; Cui, G.; Zhu, J.; Duan, J. Chitosan Coupling Makes Microbial Biofilms Susceptible to Antibiotics. Sci. Rep. 2013, 3, 3364. [Google Scholar] [CrossRef]
- Chuan, D.; Jin, T.; Fan, R.; Zhou, L.; Guo, G. Chitosan for Gene Delivery: Methods for Improvement and Applications. Adv. Colloid Interface Sci. 2019, 268, 25–38. [Google Scholar] [CrossRef]
- Chandy, T.; Sharma, C.P. Chitosan—As a Biomaterial. Biomater. Artif. Cells Artif. Organs 1990, 18, 1–24. [Google Scholar] [CrossRef]
- Kurakula, M. Prospection of Recent Chitosan Biomedical Trends: Evidence from Patent Analysis (2009–2020). Int. J. Biol. Macromol. 2020, 165, 1924–1938. [Google Scholar] [CrossRef]
- Lavanya, K.; Chandran, S.V.; Balagangadharan, K.; Selvamurugan, N. Temperature- and PH-Responsive Chitosan-Based Injectable Hydrogels for Bone Tissue Engineering. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 111, 110862. [Google Scholar] [CrossRef]
- Saravanan, S.; Leena, R.S.; Selvamurugan, N. Chitosan Based Biocomposite Scaffolds for Bone Tissue Engineering. Int. J. Biol. Macromol. 2016, 93, 1354–1365. [Google Scholar] [CrossRef]
- Blecher, K.; Nasir, A.; Friedman, A. The Growing Role of Nanotechnology in Combating Infectious Disease. Virulence 2011, 2, 395–401. [Google Scholar] [CrossRef]
- Bowman, K.; Leong, K.W. Chitosan Nanoparticles for Oral Drug and Gene Delivery. Int. J. Nanomed. 2006, 1, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Escamilla-García, M.; Calderón-Domínguez, G.; Chanona-Pérez, J.J.; Farrera-Rebollo, R.R.; Andraca-Adame, J.A.; Arzate-Vázquez, I.; Mendez-Mendez, J.V.; Moreno-Ruiz, L.A. Physical and Structural Characterisation of Zein and Chitosan Edible Films Using Nanotechnology Tools. Int. J. Biol. Macromol. 2013, 61, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Baldrick, P. The Safety of Chitosan as a Pharmaceutical Excipient. Regul. Toxicol. Pharmacol. 2010, 56, 290–299. [Google Scholar] [CrossRef] [PubMed]
- Samal, S.K.; Dash, M.; Van Vlierberghe, S.; Kaplan, D.L.; Chiellini, E.; van Blitterswijk, C.; Moroni, L.; Dubruel, P. Cationic Polymers and Their Therapeutic Potential. Chem. Soc. Rev. 2012, 41, 7147–7194. [Google Scholar] [CrossRef]
- Yang, Y.; Cai, Z.; Huang, Z.; Tang, X.; Zhang, X. Antimicrobial Cationic Polymers: From Structural Design to Functional Control. Polym. J. 2017, 50, 33–44. [Google Scholar] [CrossRef]
- Sharland, M.; Saroey, P.; Berezin, E.N. The Global Threat of Antimicrobial Resistance—The Need for Standardized Surveillance Tools to Define Burden and Develop Interventions. J. Pediatr. 2015, 91, 410–412. [Google Scholar] [CrossRef]
- Bertesteanu, S.; Chifiriuc, M.C.; Grumezescu, A.M.; Printza, A.G.; Marie-Paule, T.; Grumezescu, V.; Mihaela, V.; Lazar, V.; Grigore, R. Biomedical Applications of Synthetic, Biodegradable Polymers for the Development of Anti-Infective Strategies. Curr. Med. Chem. 2014, 21, 3383–3390. [Google Scholar] [CrossRef]
- O’Rourke, A.; Beyhan, S.; Choi, Y.; Morales, P.; Chan, A.P.; Espinoza, J.L.; Dupont, C.L.; Meyer, K.J.; Spoering, A.; Lewis, K.; et al. Mechanism-of-Action Classification of Antibiotics by Global Transcriptome Profiling. Antimicrob. Agents Chemother. 2020, 64, e01207-19. [Google Scholar] [CrossRef]
- Kamaruzzaman, N.F.; Tan, L.P.; Hamdan, R.H.; Choong, S.S.; Wong, W.K.; Gibson, A.J.; Chivu, A.; Pina, M.d.F. Antimicrobial Polymers: The Potential Replacement of Existing Antibiotics? Int. J. Mol. Sci. 2019, 20, 2747. [Google Scholar] [CrossRef]
- Ngo, D.-H.; Vo, T.-S.; Ngo, D.-N.; Kang, K.-H.; Je, J.-Y.; Pham, H.N.-D.; Byun, H.-G.; Kim, S.-K. Biological Effects of Chitosan and Its Derivatives. Food Hydrocoll. 2015, 51, 200–216. [Google Scholar] [CrossRef]
- Shariatinia, Z. Pharmaceutical Applications of Chitosan. Adv. Colloid Interface Sci. 2019, 263, 131–194. [Google Scholar] [CrossRef] [PubMed]
- Cheung, R.C.F.; Ng, T.B.; Wong, J.H.; Chan, W.Y. Chitosan: An Update on Potential Biomedical and Pharmaceutical Applications. Mar. Drugs 2015, 13, 5156–5186. [Google Scholar] [CrossRef]
- Garg, P.; Kumar, S.; Pandey, S.; Seonwoo, H.; Choung, P.-H.; Koh, J.; Chung, J.H. Triphenylamine Coupled Chitosan with High Buffering Capacity and Low Viscosity for Enhanced Transfection in Mammalian Cells, in Vitro and in Vivo. J. Mater. Chem. B Mater. Biol. Med. 2013, 1, 6053–6065. [Google Scholar] [CrossRef]
- Davidovich-Pinhas, M.; Danin-Poleg, Y.; Kashi, Y.; Bianco-Peled, H. Modified Chitosan: A Step toward Improving the Properties of Antibacterial Food Packages. Food Packag. Shelf Life 2014, 1, 160–169. [Google Scholar] [CrossRef]
- Ishihara, M.; Nakanishi, K.; Ono, K.; Sato, M.; Kikuchi, M.; Saito, Y.; Yura, H.; Matsui, T.; Hattori, H.; Uenoyama, M.; et al. Photocrosslinkable Chitosan as a Dressing for Wound Occlusion and Accelerator in Healing Process. Biomaterials 2002, 23, 833–840. [Google Scholar] [CrossRef] [PubMed]
- Capel, V.; Vllasaliu, D.; Watts, P.; Clarke, P.A.; Luxton, D.; Grabowska, A.M.; Mantovani, G.; Stolnik, S. Water-Soluble Substituted Chitosan Derivatives as Technology Platform for Inhalation Delivery of SiRNA. Drug Deliv. 2018, 25, 644–653. [Google Scholar] [CrossRef] [PubMed]
- Jaiswal, S.; Dutta, P.K.; Kumar, S.; Koh, J.; Pandey, S. Methyl Methacrylate Modified Chitosan: Synthesis, Characterization and Application in Drug and Gene Delivery. Carbohydr. Polym. 2019, 211, 109–117. [Google Scholar] [CrossRef]
- Muzzarelli, R.A.A.; Ramos, V.; Stanic, V.; Dubini, B.; Mattioli-Belmonte, M.; Tosi, G.; Giardino, R. Osteogenesis Promoted by Calcium Phosphate N,N-Dicarboxymethyl Chitosan. Carbohydr. Polym. 1998, 36, 267–276. [Google Scholar] [CrossRef]
- Kantak, M.N.; Bharate, S.S. Analysis of Clinical Trials on Biomaterial and Therapeutic Applications of Chitosan: A Review. Carbohydr. Polym. 2022, 278, 118999. [Google Scholar] [CrossRef]
- Kim, C.-H.; Park, S.J.; Yang, D.H.; Chun, H.J. Chitosan for Tissue Engineering. Adv. Exp. Med. Biol. 2018, 1077, 475–485. [Google Scholar]
- Kim, I.-Y.; Seo, S.-J.; Moon, H.-S.; Yoo, M.-K.; Park, I.-Y.; Kim, B.-C.; Cho, C.-S. Chitosan and Its Derivatives for Tissue Engineering Applications. Biotechnol. Adv. 2008, 26, 1–21. [Google Scholar] [CrossRef] [PubMed]
- LogithKumar, R.; KeshavNarayan, A.; Dhivya, S.; Chawla, A.; Saravanan, S.; Selvamurugan, N. A Review of Chitosan and Its Derivatives in Bone Tissue Engineering. Carbohydr. Polym. 2016, 151, 172–188. [Google Scholar] [CrossRef] [PubMed]
- Hejazi, R.; Amiji, M. Chitosan-Based Gastrointestinal Delivery Systems. J. Control. Release 2003, 89, 151–165. [Google Scholar] [CrossRef] [PubMed]
- Fakhri, E.; Eslami, H.; Maroufi, P.; Pakdel, F.; Taghizadeh, S.; Ganbarov, K.; Yousefi, M.; Tanomand, A.; Yousefi, B.; Mahmoudi, S.; et al. Chitosan Biomaterials Application in Dentistry. Int. J. Biol. Macromol. 2020, 162, 956–974. [Google Scholar] [CrossRef] [PubMed]
- Ray, S.D. Potential Aspects of Chitosan as Pharmaceutical Excipient. Acta Pol. Pharm. 2011, 68, 619–622. [Google Scholar]
- Muxika, A.; Etxabide, A.; Uranga, J.; Guerrero, P.; de la Caba, K. Chitosan as a Bioactive Polymer: Processing, Properties and Applications. Int. J. Biol. Macromol. 2017, 105, 1358–1368. [Google Scholar] [CrossRef]
- Shariatinia, Z. Carboxymethyl Chitosan: Properties and Biomedical Applications. Int. J. Biol. Macromol. 2018, 120, 1406–1419. [Google Scholar] [CrossRef]
- Wang, W.; Meng, Q.; Li, Q.; Liu, J.; Zhou, M.; Jin, Z.; Zhao, K. Chitosan Derivatives and Their Application in Biomedicine. Int. J. Mol. Sci. 2020, 21, 487. [Google Scholar] [CrossRef]
- Zhang, J.; Xia, W.; Liu, P.; Cheng, Q.; Tahirou, T.; Gu, W.; Li, B. Chitosan Modification and Pharmaceutical/Biomedical Applications. Mar. Drugs 2010, 8, 1962–1987. [Google Scholar] [CrossRef]
- Kumar, U.S.; Afjei, R.; Ferrara, K.; Massoud, T.F.; Paulmurugan, R. Gold-Nanostar-Chitosan-Mediated Delivery of SARS-CoV-2 DNA Vaccine for Respiratory Mucosal Immunization: Development and Proof-of-Principle. ACS Nano 2021, 15, 17582–17601. [Google Scholar] [CrossRef]
- Beniac, D.R.; Andonov, A.; Grudeski, E.; Booth, T.F. Architecture of the SARS Coronavirus Prefusion Spike. Nat. Struct. Mol. Biol. 2006, 13, 751–752. [Google Scholar] [CrossRef]
- Collins, A.R.; Knobler, R.L.; Powell, H.; Buchmeier, M.J. Monoclonal Antibodies to Murine Hepatitis Virus-4 (Strain JHM) Define the Viral Glycoprotein Responsible for Attachment and Cell—Cell Fusion. Virology 1982, 119, 358–371. [Google Scholar] [CrossRef]
- Luytjes, W.; Sturman, L.S.; Bredenbeek, P.J.; Charite, J.; van der Zeijst, B.A.; Horzinek, M.C.; Spaan, W.J. Primary Structure of the Glycoprotein E2 of Coronavirus MHV-A59 and Identification of the Trypsin Cleavage Site. Virology 1987, 161, 479–487. [Google Scholar] [CrossRef]
- Eigenmann, P.A. Clinical Features and Diagnostic Criteria of Atopic Dermatitis in Relation to Age. Pediatr. Allergy Immunol. 2001, 12 (Suppl. 14), 69–74. [Google Scholar] [CrossRef]
- Lopes, C.; Soares, J.; Tavaria, F.; Duarte, A.; Correia, O.; Sokhatska, O.; Severo, M.; Silva, D.; Pintado, M.; Delgado, L.; et al. Chitosan Coated Textiles May Improve Atopic Dermatitis Severity by Modulating Skin Staphylococcal Profile: A Randomized Controlled Trial. PLoS ONE 2015, 10, e0142844. [Google Scholar] [CrossRef] [PubMed]
- Hemmingsen, L.M.; Škalko-Basnet, N.; Jøraholmen, M.W. The Expanded Role of Chitosan in Localized Antimicrobial Therapy. Mar. Drugs 2021, 19, 697. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-C.; Nam, J.-P.; Kim, J.-H.; Kim, Y.-M.; Nah, J.-W.; Jang, M.-K. Antimicrobial Action of Water-Soluble β-Chitosan against Clinical Multi-Drug Resistant Bacteria. Int. J. Mol. Sci. 2015, 16, 7995–8007. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Ji, Y.; Zhu, Y.; Wu, X.; Mei, L.; Zhang, H.; Deng, J.; Wang, S. Antibacterial Effect of Chitosan and Its Derivative on Enterococcus Faecalis Associated with Endodontic Infection. Exp. Ther. Med. 2020, 19, 3805–3813. [Google Scholar] [CrossRef] [PubMed]
- Costa, E.M.; Silva, S.; Tavaria, F.K.; Pintado, M.M. Insights into Chitosan Antibiofilm Activity against Methicillin-Resistant Staphylococcus Aureus. J. Appl. Microbiol. 2017, 122, 1547–1557. [Google Scholar] [CrossRef]
- Saito, H.; Sakakibara, Y.; Sakata, A.; Kurashige, R.; Murakami, D.; Kageshima, H.; Saito, A.; Miyazaki, Y. Antibacterial Activity of Lysozyme-Chitosan Oligosaccharide Conjugates (LYZOX) against Pseudomonas Aeruginosa, Acinetobacter Baumannii and Methicillin-Resistant Staphylococcus Aureus. PLoS ONE 2019, 14, e0217504. [Google Scholar] [CrossRef]
- Abadi, M.S.S.; Mirzaei, E.; Bazargani, A.; Gholipour, A.; Heidari, H.; Hadi, N. Antibacterial Activity and Mechanism of Action of Chitosan Nanofibers against Toxigenic Clostridioides (Clostridium) Difficile Isolates. Ann. Ig. 2020, 32, 72–80. [Google Scholar]
- Zhang, F.; Ramachandran, G.; Mothana, R.A.; Noman, O.M.; Alobaid, W.A.; Rajivgandhi, G.; Manoharan, N. Anti-Bacterial Activity of Chitosan Loaded Plant Essential Oil against Multi Drug Resistant K. Pneumoniae. Saudi J. Biol. Sci. 2020, 27, 3449–3455. [Google Scholar] [CrossRef] [PubMed]
- Jamil, B.; Habib, H.; Abbasi, S.A.; Ihsan, A.; Nasir, H.; Imran, M. Development of Cefotaxime Impregnated Chitosan as Nano-Antibiotics: De Novo Strategy to Combat Biofilm Forming Multi-Drug Resistant Pathogens. Front. Microbiol. 2016, 7, 330. [Google Scholar] [CrossRef]
- Alburquenque, C.; Bucarey, S.A.; Neira-Carrillo, A.; Urzúa, B.; Hermosilla, G.; Tapia, C.V. Antifungal Activity of Low Molecular Weight Chitosan against Clinical Isolates of Candida Spp. Med. Mycol. 2010, 48, 1018–1023. [Google Scholar] [CrossRef]
- Ganan, M.; Lorentzen, S.B.; Aam, B.B.; Eijsink, V.G.H.; Gaustad, P.; Sørlie, M. Antibiotic Saving Effect of Combination Therapy through Synergistic Interactions between Well-Characterized Chito-Oligosaccharides and Commercial Antifungals against Medically Relevant Yeasts. PLoS ONE 2019, 14, e0227098. [Google Scholar] [CrossRef] [PubMed]
- Lo, W.-H.; Deng, F.-S.; Chang, C.-J.; Lin, C.-H. Synergistic Antifungal Activity of Chitosan with Fluconazole against Candida Albicans, Candida Tropicalis, and Fluconazole-Resistant Strains. Molecules 2020, 25, 5114. [Google Scholar] [CrossRef] [PubMed]
- Schmiedel, Y.; Zimmerli, S. Common Invasive Fungal Diseases: An Overview of Invasive Candidiasis, Aspergillosis, Cryptococcosis, and Pneumocystis Pneumonia. Swiss Med. Wkly. 2016, 146, w14281. [Google Scholar] [CrossRef]
- Paramythiotou, E.; Frantzeskaki, F.; Flevari, A.; Armaganidis, A.; Dimopoulos, G. Invasive Fungal Infections in the ICU: How to Approach, How to Treat. Molecules 2014, 19, 1085–1119. [Google Scholar] [CrossRef]
- Peña, A.; Sánchez, N.S.; Calahorra, M. Effects of Chitosan on Candida Albicans: Conditions for Its Antifungal Activity. Biomed Res. Int. 2013, 2013, 527549. [Google Scholar] [CrossRef]
- Tao, F.; Ma, S.; Tao, H.; Jin, L.; Luo, Y.; Zheng, J.; Xiang, W.; Deng, H. Chitosan-Based Drug Delivery Systems: From Synthesis Strategy to Osteomyelitis Treatment—A Review. Carbohydr. Polym. 2021, 251, 117063. [Google Scholar] [CrossRef]
- Dev, A.; Mohan, J.C.; Sreeja, V.; Tamura, H.; Patzke, G.R.; Hussain, F.; Weyeneth, S.; Nair, S.V.; Jayakumar, R. Novel Carboxymethyl Chitin Nanoparticles for Cancer Drug Delivery Applications. Carbohydr. Polym. 2010, 79, 1073–1079. [Google Scholar] [CrossRef]
- Lupascu, F.G.; Dash, M.; Samal, S.K.; Dubruel, P.; Lupusoru, C.E.; Lupusoru, R.-V.; Dragostin, O.; Profire, L. Development, Optimization and Biological Evaluation of Chitosan Scaffold Formulations of New Xanthine Derivatives for Treatment of Type-2 Diabetes Mellitus. Eur. J. Pharm. Sci. 2015, 77, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M.; Qu, D.; Wang, H.; Sun, Z.; Liu, X.; Chen, J.; Li, C.; Li, X.; Chen, Z. Intranasal Administration of Chitosan Against Influenza A (H7N9) Virus Infection in a Mouse Model. Sci. Rep. 2016, 6, 28729. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Modak, C.; Singh, P.K.; Kumar, R.; Khatri, D.; Singh, S.B. Underscoring the Immense Potential of Chitosan in Fighting a Wide Spectrum of Viruses: A Plausible Molecule against SARS-CoV-2? Int. J. Biol. Macromol. 2021, 179, 33–44. [Google Scholar] [CrossRef]
- Safarzadeh, M.; Sadeghi, S.; Azizi, M.; Rastegari-Pouyani, M.; Pouriran, R.; Hoseini, M.H.M. Chitin and Chitosan as Tools to Combat COVID-19: A Triple Approach. Int. J. Biol. Macromol. 2021, 183, 235–244. [Google Scholar] [CrossRef]
- Russo, E.; Gaglianone, N.; Baldassari, S.; Parodi, B.; Cafaggi, S.; Zibana, C.; Donalisio, M.; Cagno, V.; Lembo, D.; Caviglioli, G. Preparation, Characterization and in Vitro Antiviral Activity Evaluation of Foscarnet-Chitosan Nanoparticles. Colloids Surf. B Biointerfaces 2014, 118, 117–125. [Google Scholar] [CrossRef]
- Kubbinga, M.; Nguyen, M.A.; Staubach, P.; Teerenstra, S.; Langguth, P. The Influence of Chitosan on the Oral Bioavailability of Acyclovir—A Comparative Bioavailability Study in Humans. Pharm. Res. 2015, 32, 2241–2249. [Google Scholar] [CrossRef]
- Giuliani, A.; Balducci, A.G.; Zironi, E.; Colombo, G.; Bortolotti, F.; Lorenzini, L.; Galligioni, V.; Pagliuca, G.; Scagliarini, A.; Calzà, L.; et al. In Vivo Nose-to-Brain Delivery of the Hydrophilic Antiviral Ribavirin by Microparticle Agglomerates. Drug Deliv. 2018, 25, 376–387. [Google Scholar] [CrossRef]
- Lungare, S.; Bowen, J.; Badhan, R. Development and Evaluation of a Novel Intranasal Spray for the Delivery of Amantadine. J. Pharm. Sci. 2016, 105, 1209–1220. [Google Scholar] [CrossRef]
- WuDunn, D.; Spear, P.G. Initial Interaction of Herpes Simplex Virus with Cells Is Binding to Heparan Sulfate. J. Virol. 1989, 63, 52–58. [Google Scholar] [CrossRef]
- Compton, T.; Nowlin, D.M.; Cooper, N.R. Initiation of Human Cytomegalovirus Infection Requires Initial Interaction with Cell Surface Heparan Sulfate. Virology 1993, 193, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Su, C.M.; Liao, C.L.; Lee, Y.L.; Lin, Y.L. Highly Sulfated Forms of Heparin Sulfate Are Involved in Japanese Encephalitis Virus Infection. Virology 2001, 286, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Klimstra, W.B.; Ryman, K.D.; Johnston, R.E. Adaptation of Sindbis Virus to BHK Cells Selects for Use of Heparan Sulfate as an Attachment Receptor. J. Virol. 1998, 72, 7357–7366. [Google Scholar] [CrossRef] [PubMed]
- Byrnes, A.P.; Griffin, D.E. Binding of Sindbis Virus to Cell Surface Heparan Sulfate. J. Virol. 1998, 72, 7349–7356. [Google Scholar] [CrossRef]
- Chen, Y.; Maguire, T.; Hileman, R.E.; Fromm, J.R.; Esko, J.D.; Linhardt, R.J.; Marks, R.M. Dengue Virus Infectivity Depends on Envelope Protein Binding to Target Cell Heparan Sulfate. Nat. Med. 1997, 3, 866–871. [Google Scholar] [CrossRef]
- Kroschewski, H.; Allison, S.L.; Heinz, F.X.; Mandl, C.W. Role of Heparan Sulfate for Attachment and Entry of Tick-Borne Encephalitis Virus. Virology 2003, 308, 92–100. [Google Scholar] [CrossRef]
- Artan, M.; Karadeniz, F.; Karagozlu, M.Z.; Kim, M.-M.; Kim, S.-K. Anti-HIV-1 Activity of Low Molecular Weight Sulfated Chitooligosaccharides. Carbohydr. Res. 2010, 345, 656–662. [Google Scholar] [CrossRef]
- Kochkina, Z.M.; Chirkov, S.N. Influence of the Chitosan Oligomer on the Phage Particles and Reproduction of Phage 1-97A in the Culture of Bacillus Thuringiensis. Microbiology 2001, 70, 706–710. [Google Scholar] [CrossRef]
- No, H.K.; Park, N.Y.; Lee, S.H.; Meyers, S.P. Antibacterial Activity of Chitosans and Chitosan Oligomers with Different Molecular Weights. Int. J. Food Microbiol. 2002, 74, 65–72. [Google Scholar] [CrossRef]
- Confederat, L.G.; Tuchilus, C.G.; Dragan, M.; Sha’at, M.; Dragostin, O.M. Preparation and Antimicrobial Activity of Chitosan and Its Derivatives: A Concise Review. Molecules 2021, 26, 3694. [Google Scholar] [CrossRef]
- Stepanov, O.A.; Prokof’eva, M.M.; Stocking, K.; Varlamov, V.P.; Levov, A.N.; Vikhoreva, G.A.; Spirin, P.V.; Mikhailov, S.N.; Prassolov, V.S. Replication-Competent Gamma-Retrovirus Mo-MuLV Expressing Green Fluorescent Protein as Efficient Tool for Screening of Inhibitors of Retroviruses That Use Heparan Sulfate as Primary Cell Receptor. Mol. Biol. 2012, 46, 457–466. [Google Scholar] [CrossRef]
- Nishimura, S.I.; Kai, H.; Shinada, K.; Yoshida, T.; Tokura, S.; Kurita, K.; Nakashima, H.; Yamamoto, N.; Uryu, T. Regioselective Syntheses of Sulfated Polysaccharides: Specific Anti-HIV-1 Activity of Novel Chitin Sulfates. Carbohydr. Res. 1998, 306, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Luo, K.; Li, D.; Yu, S.; Cai, J.; Chen, L.; Du, Y. Preparation, Characterization and in Vitro Anticoagulant Activity of Highly Sulfated Chitosan. Int. J. Biol. Macromol. 2013, 52, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Sosa, M.A.G.; Fazely, F.; Koch, J.A.; Vercellotti, S.V.; Ruprecht, R.M. N-Carboxymethylchitosan-N, O-Sulfate as an Anti-HIV-1 Agent. Biochem. Biophys. Res. Commun. 1991, 174, 489–496. [Google Scholar] [CrossRef]
- Jayakumar, R.; Nwe, N.; Tokura, S.; Tamura, H. Sulfated Chitin and Chitosan as Novel Biomaterials. Int. J. Biol. Macromol. 2007, 40, 175–181. [Google Scholar] [CrossRef]
- Dimassi, S.; Tabary, N.; Chai, F.; Blanchemain, N.; Martel, B. Sulfonated and Sulfated Chitosan Derivatives for Biomedical Applications: A Review. Carbohydr. Polym. 2018, 202, 382–396. [Google Scholar] [CrossRef]
- Karagozlu, M.Z.; Karadeniz, F.; Kim, S.-K. Anti-HIV Activities of Novel Synthetic Peptide Conjugated Chitosan Oligomers. Int. J. Biol. Macromol. 2014, 66, 260–266. [Google Scholar] [CrossRef]
- Wu, D.; Ensinas, A.; Verrier, B.; Primard, C.; Cuvillier, A.; Champier, G.; Paul, S.; Delair, T. Zinc-Stabilized Colloidal Polyelectrolyte Complexes of Chitosan/Hyaluronan: A Tool for the Inhibition of HIV-1 Infection. J. Mater. Chem. B Mater. Biol. Med. 2016, 4, 5455–5463. [Google Scholar] [CrossRef]
- Ishihara, M.; Nguyen, V.Q.; Mori, Y.; Nakamura, S.; Hattori, H. Adsorption of Silver Nanoparticles onto Different Surface Structures of Chitin/Chitosan and Correlations with Antimicrobial Activities. Int. J. Mol. Sci. 2015, 16, 13973–13988. [Google Scholar] [CrossRef]
- Mori, Y.; Ono, T.; Miyahira, Y.; Nguyen, V.Q.; Matsui, T.; Ishihara, M. Antiviral Activity of Silver Nanoparticle/Chitosan Composites against H1N1 Influenza A Virus. Nanoscale Res. Lett. 2013, 8, 93. [Google Scholar] [CrossRef]
- Cheng, S.; Zhao, H.; Xu, Y.; Yang, Y.; Lv, X.; Wu, P.; Li, X. Inhibition of Influenza Virus Infection with Chitosan–Sialyloligosaccharides Ionic Complex. Carbohydr. Polym. 2014, 107, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Collins, B.E.; Paulson, J.C. Cell Surface Biology Mediated by Low Affinity Multivalent Protein–Glycan Interactions. Curr. Opin. Chem. Biol. 2004, 8, 617–625. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.C.; Lee, R.T. Carbohydrate-Protein Interactions: Basis of Glycobiology. Acc. Chem. Res. 1995, 28, 321–327. [Google Scholar] [CrossRef]
- Lin, Y.-C.; Lin, S.-T.; Chen, C.-Y.; Wu, S.-C. Enterovirus 71 Adsorption on Metal Ion-Composite Chitosan Beads. Biotechnol. Prog. 2012, 28, 206–214. [Google Scholar] [CrossRef] [PubMed]
- Pauls, T. Chitosan as an Antiviral. Bachelor’s Thesis, University of Arkansas, Fayetteville, NC, USA, 2016. [Google Scholar]
- Gao, Y.; Liu, W.; Wang, W.; Zhang, X.; Zhao, X. The Inhibitory Effects and Mechanisms of 3,6-O-Sulfated Chitosan against Human Papillomavirus Infection. Carbohydr. Polym. 2018, 198, 329–338. [Google Scholar] [CrossRef]
- Ishihara, C.; Yoshimatsu, K.; Tsuji, M.; Arikawa, J.; Saiki, I.; Tokura, S.; Azuma, I. Anti-Viral Activity of Sulfated Chitin Derivatives against Friend Murine Leukaemia and Herpes Simplex Type-1 Viruses. Vaccine 1993, 11, 670–674. [Google Scholar] [CrossRef]
- Hassan, M.; Mohamed, A.; Taher, F.; Kamel, M. Antimicrobial Activities of Chitosan Nanoparticles Prepared from Lucilia Cuprina Maggots (Diptera: Calliphoridae). J. Egypt. Soc. Parasitol. 2016, 46, 563–570. [Google Scholar]
- Bai, B.; Mi, X.; Xiang, X.; Heiden, P.A.; Heldt, C.L. Non-Enveloped Virus Reduction with Quaternized Chitosan Nanofibers Containing Graphene. Carbohydr. Res. 2013, 380, 137–142. [Google Scholar] [CrossRef]
- Mi, X.; Vijayaragavan, K.S.; Heldt, C.L. Virus Adsorption of Water-Stable Quaternized Chitosan Nanofibers. Carbohydr. Res. 2014, 387, 24–29. [Google Scholar] [CrossRef]
- Ciejka, J.; Wolski, K.; Nowakowska, M.; Pyrc, K.; Szczubiałka, K. Biopolymeric Nano/Microspheres for Selective and Reversible Adsorption of Coronaviruses. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 76, 735–742. [Google Scholar] [CrossRef]
- Milewska, A.; Ciejka, J.; Kaminski, K.; Karewicz, A.; Bielska, D.; Zeglen, S.; Karolak, W.; Nowakowska, M.; Potempa, J.; Bosch, B.J.; et al. Novel Polymeric Inhibitors of HCoV-NL63. Antivir. Res. 2013, 97, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Milewska, A.; Kaminski, K.; Ciejka, J.; Kosowicz, K.; Zeglen, S.; Wojarski, J.; Nowakowska, M.; Szczubiałka, K.; Pyrc, K. HTCC: Broad Range Inhibitor of Coronavirus Entry. PLoS ONE 2016, 11, e0156552. [Google Scholar] [CrossRef] [PubMed]
- Briz, V.; Poveda, E.; Soriano, V. HIV Entry Inhibitors: Mechanisms of Action and Resistance Pathways. J. Antimicrob. Chemother. 2006, 57, 619–627. [Google Scholar] [CrossRef] [PubMed]
- Vo, T.-S.; Kim, S.-K. Potential Anti-HIV Agents from Marine Resources: An Overview. Mar. Drugs 2010, 8, 2871–2892. [Google Scholar] [CrossRef]
- Baranova, E.O.; Shastina, N.S.; Shvets, V.I. Polyanionic Inhibitors of HIV Adsorption. Russ. J. Bioorganic Chem. 2011, 37, 527. [Google Scholar] [CrossRef]
- Boroumand, H.; Badie, F.; Mazaheri, S.; Seyedi, Z.S.; Nahand, J.S.; Nejati, M.; Baghi, H.B.; Abbasi-Kolli, M.; Badehnoosh, B.; Ghandali, M.; et al. Chitosan-Based Nanoparticles Against Viral Infections. Front. Cell. Infect. Microbiol. 2021, 11, 643953. [Google Scholar] [CrossRef] [PubMed]
- Karthik, R.; Manigandan, V.; Saravanan, R.; Rajesh, R.P.; Chandrika, B. Structural Characterization and in Vitro Biomedical Activities of Sulfated Chitosan from Sepia Pharaonis. Int. J. Biol. Macromol. 2016, 84, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Xing, R.; Liu, S.; Qin, Y.; Li, K.; Yu, H.; Li, P. Immunostimulatory Effects of Sulfated Chitosans on RAW 264.7 Mouse Macrophages via the Activation of PI3 K/Akt Signaling Pathway. Int. J. Biol. Macromol. 2018, 108, 1310–1321. [Google Scholar] [CrossRef]
- Kim, J.-H.; Kim, Y.-S.; Hwang, J.-W.; Han, Y.-K.; Lee, J.-S.; Kim, S.-K.; Jeon, Y.-J.; Moon, S.-H.; Jeon, B.-T.; Bahk, Y.Y.; et al. Sulfated Chitosan Oligosaccharides Suppress LPS-Induced NO Production via JNK and NF-ΚB Inactivation. Molecules 2014, 19, 18232–18247. [Google Scholar] [CrossRef]
- Chirkov, S.N. The Antiviral Activity of Chitosan. Appl. Biochem. Microbiol. 2002, 38, 1–8. [Google Scholar] [CrossRef]
- He, X.; Xing, R.; Liu, S.; Qin, Y.; Li, K.; Yu, H.; Li, P. The Improved Antiviral Activities of Amino-Modified Chitosan Derivatives on Newcastle Virus. Drug Chem. Toxicol. 2021, 44, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wu, P.; Gao, G.F.; Cheng, S. Carbohydrate-Functionalized Chitosan Fiber for Influenza Virus Capture. Biomacromolecules 2011, 12, 3962–3969. [Google Scholar] [CrossRef] [PubMed]
- Sofy, A.R.; Hmed, A.A.; Abd El Haliem, N.F.; Zein, M.A.-E.; Elshaarawy, R.F.M. Polyphosphonium-Oligochitosans Decorated with Nanosilver as New Prospective Inhibitors for Common Human Enteric Viruses. Carbohydr. Polym. 2019, 226, 115261. [Google Scholar] [CrossRef] [PubMed]
- Tan, R.S.L.; Hassandarvish, P.; Chee, C.F.; Chan, L.W.; Wong, T.W. Chitosan and Its Derivatives as Polymeric Anti-Viral Therapeutics and Potential Anti-SARS-CoV-2 Nanomedicine. Carbohydr. Polym. 2022, 290, 119500. [Google Scholar] [CrossRef]
- Davis, R.; Zivanovic, S.; D’Souza, D.H.; Davidson, P.M. Effectiveness of Chitosan on the Inactivation of Enteric Viral Surrogates. Food Microbiol. 2012, 32, 57–62. [Google Scholar] [CrossRef]
- Kochkina, Z.M.; Surgucheva, N.A.; Chirkov, S.N. Coliphages inactivation using chitosan derivatives. Mikrobiologiia 2000, 69, 261–265. [Google Scholar]
- Sabino, E.C.; Buss, L.F.; Carvalho, M.P.S.; Prete, C.A., Jr.; Crispim, M.A.E.; Fraiji, N.A.; Pereira, R.H.M.; Parag, K.V.; da Silva Peixoto, P.; Kraemer, M.U.G.; et al. Resurgence of COVID-19 in Manaus, Brazil, despite High Seroprevalence. Lancet 2021, 397, 452–455. [Google Scholar] [CrossRef]
- Davies, N.G.; Abbott, S.; Barnard, R.C.; Jarvis, C.I.; Kucharski, A.J.; Munday, J.D.; Pearson, C.A.B.; Russell, T.W.; Tully, D.C.; Washburne, A.D.; et al. Estimated Transmissibility and Impact of SARS-CoV-2 Lineage B.1.1.7 in England. Science 2021, 372, eabg3055. [Google Scholar] [CrossRef]
- Callaway, E. Delta Coronavirus Variant: Scientists Brace for Impact. Nature 2021, 595, 17–18. [Google Scholar] [CrossRef]
- Challen, R.; Brooks-Pollock, E.; Read, J.M.; Dyson, L.; Tsaneva-Atanasova, K.; Danon, L. Risk of Mortality in Patients Infected with SARS-CoV-2 Variant of Concern 202012/1: Matched Cohort Study. BMJ 2021, 372, n579. [Google Scholar] [CrossRef]
- Chen, Y.; Zuiani, A.; Fischinger, S.; Mullur, J.; Atyeo, C.; Travers, M.; Lelis, F.J.N.; Pullen, K.M.; Martin, H.; Tong, P.; et al. Quick COVID-19 Healers Sustain Anti-SARS-CoV-2 Antibody Production. Cell 2020, 183, 1496–1507.e16. [Google Scholar] [CrossRef]
- Burioni, R.; Topol, E.J. Assessing the Human Immune Response to SARS-CoV-2 Variants. Nat. Med. 2021, 27, 571–572. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Schmidt, F.; Weisblum, Y.; Muecksch, F.; Barnes, C.O.; Finkin, S.; Schaefer-Babajew, D.; Cipolla, M.; Gaebler, C.; Lieberman, J.A.; et al. MRNA Vaccine-Elicited Antibodies to SARS-CoV-2 and Circulating Variants. Nature 2021, 592, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Nie, J.; Wu, J.; Zhang, L.; Ding, R.; Wang, H.; Zhang, Y.; Li, T.; Liu, S.; Zhang, M.; et al. SARS-CoV-2 501Y.V2 Variants Lack Higher Infectivity but Do Have Immune Escape. Cell 2021, 184, 2362–2371.e9. [Google Scholar] [CrossRef]
- London School of Hygiene & Tropical Medicine COVID-19 Vaccine Tracker. Available online: https://vac-lshtm.shinyapps.io/ncov_vaccine_landscape/ (accessed on 5 August 2022).
- Zhang, Y.-N.; Paynter, J.; Sou, C.; Fourfouris, T.; Wang, Y.; Abraham, C.; Ngo, T.; Zhang, Y.; He, L.; Zhu, J. Mechanism of a COVID-19 Nanoparticle Vaccine Candidate That Elicits a Broadly Neutralizing Antibody Response to SARS-CoV-2 Variants. Sci. Adv. 2021, 7, eabj3107. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.C.; Burgers, W.A. SARS-CoV-2 Evolution and Vaccines: Cause for Concern? Lancet Respir. Med. 2021, 9, 333–335. [Google Scholar] [CrossRef]
- Logunov, D.Y.; Dolzhikova, I.V.; Shcheblyakov, D.V.; Tukhvatulin, A.I.; Zubkova, O.V.; Dzharullaeva, A.S.; Kovyrshina, A.V.; Lubenets, N.L.; Grousova, D.M.; Erokhova, A.S.; et al. Safety and Efficacy of an RAd26 and RAd5 Vector-Based Heterologous Prime-Boost COVID-19 Vaccine: An Interim Analysis of a Randomised Controlled Phase 3 Trial in Russia. Lancet 2021, 397, 671–681. [Google Scholar] [CrossRef]
- Heath, P.T.; Galiza, E.P.; Baxter, D.N.; Boffito, M.; Browne, D.; Burns, F.; Chadwick, D.R.; Clark, R.; Cosgrove, C.; Galloway, J.; et al. Safety and Efficacy of NVX-CoV2373 COVID-19 Vaccine. N. Engl. J. Med. 2021, 385, 1172–1183. [Google Scholar] [CrossRef]
- Thompson, M.G.; Burgess, J.L.; Naleway, A.L.; Tyner, H.; Yoon, S.K.; Meece, J.; Olsho, L.E.W.; Caban-Martinez, A.J.; Fowlkes, A.L.; Lutrick, K.; et al. Prevention and Attenuation of COVID-19 with the BNT162b2 and MRNA-1273 Vaccines. N. Engl. J. Med. 2021, 385, 320–329. [Google Scholar] [CrossRef]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and Safety of the MRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef]
- Lupala, C.S.; Kumar, V.; Su, X.-D.; Wu, C.; Liu, H. Computational Insights into Differential Interaction of Mammalian Angiotensin-Converting Enzyme 2 with the SARS-CoV-2 Spike Receptor Binding Domain. Comput. Biol. Med. 2022, 141, 105017. [Google Scholar] [CrossRef]
- Garcia-Beltran, W.F.; Lam, E.C.; St Denis, K.; Nitido, A.D.; Garcia, Z.H.; Hauser, B.M.; Feldman, J.; Pavlovic, M.N.; Gregory, D.J.; Poznansky, M.C.; et al. Multiple SARS-CoV-2 Variants Escape Neutralization by Vaccine-Induced Humoral Immunity. Cell 2021, 184, 2523. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Nair, M.S.; Liu, L.; Iketani, S.; Luo, Y.; Guo, Y.; Wang, M.; Yu, J.; Zhang, B.; Kwong, P.D.; et al. Antibody Resistance of SARS-CoV-2 Variants B.1.351 and B.1.1.7. Nature 2021, 593, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Andreano, E.; Piccini, G.; Licastro, D.; Casalino, L.; Johnson, N.V.; Paciello, I.; Dal Monego, S.; Pantano, E.; Manganaro, N.; Manenti, A.; et al. SARS-CoV-2 Escape from a Highly Neutralizing COVID-19 Convalescent Plasma. Proc. Natl. Acad. Sci. USA 2021, 118, e2103154118. [Google Scholar] [CrossRef] [PubMed]
- Wibmer, C.K.; Ayres, F.; Hermanus, T.; Madzivhandila, M.; Kgagudi, P.; Oosthuysen, B.; Lambson, B.E.; de Oliveira, T.; Vermeulen, M.; van der Berg, K.; et al. SARS-CoV-2 501Y.V2 Escapes Neutralization by South African COVID-19 Donor Plasma. Nat. Med. 2021, 27, 622–625. [Google Scholar] [CrossRef]
- Cherian, S.; Potdar, V.; Jadhav, S.; Yadav, P.; Gupta, N.; Das, M.; Rakshit, P.; Singh, S.; Abraham, P.; Panda, S.; et al. SARS-CoV-2 Spike Mutations, L452R, T478K, E484Q and P681R, in the Second Wave of COVID-19 in Maharashtra, India. Microorganisms 2021, 9, 1542. [Google Scholar] [CrossRef]
- Tegally, H.; Wilkinson, E.; Giovanetti, M.; Iranzadeh, A.; Fonseca, V.; Giandhari, J.; Doolabh, D.; Pillay, S.; San, E.J.; Msomi, N.; et al. Detection of a SARS-CoV-2 Variant of Concern in South Africa. Nature 2021, 592, 438–443. [Google Scholar] [CrossRef]
- Nkanga, C.I.; Ortega-Rivera, O.A.; Shin, M.D.; Moreno-Gonzalez, M.A.; Steinmetz, N.F. Injectable Slow-Release Hydrogel Formulation of a Plant Virus-Based COVID-19 Vaccine Candidate. Biomacromolecules 2022, 23, 1812–1825. [Google Scholar] [CrossRef]
- Modak, C.; Jha, A.; Sharma, N.; Kumar, A. Chitosan Derivatives: A Suggestive Evaluation for Novel Inhibitor Discovery against Wild Type and Variants of SARS-CoV-2 Virus. Int. J. Biol. Macromol. 2021, 187, 492–512. [Google Scholar] [CrossRef]
- Milewska, A.; Chi, Y.; Szczepanski, A.; Barreto-Duran, E.; Liu, K.; Liu, D.; Guo, X.; Ge, Y.; Li, J.; Cui, L.; et al. HTCC as a Highly Effective Polymeric Inhibitor of SARS-CoV-2 and MERS-CoV. bioRxiv 2020. preprint. [Google Scholar] [CrossRef]
- Raghuwanshi, D.; Mishra, V.; Das, D.; Kaur, K.; Suresh, M.R. Dendritic Cell Targeted Chitosan Nanoparticles for Nasal DNA Immunization against SARS CoV Nucleocapsid Protein. Mol. Pharm. 2012, 9, 946–956. [Google Scholar] [CrossRef] [PubMed]
- Borges, O.; Tavares, J.; de Sousa, A.; Borchard, G.; Junginger, H.E.; Cordeiro-da-Silva, A. Evaluation of the Immune Response Following a Short Oral Vaccination Schedule with Hepatitis B Antigen Encapsulated into Alginate-Coated Chitosan Nanoparticles. Eur. J. Pharm. Sci. 2007, 32, 278–290. [Google Scholar] [CrossRef] [PubMed]
- Lopes, P.D.; Okino, C.H.; Fernando, F.S.; Pavani, C.; Casagrande, V.M.; Lopez, R.F.V.; Montassier, M.d.F.S.; Montassier, H.J. Inactivated Infectious Bronchitis Virus Vaccine Encapsulated in Chitosan Nanoparticles Induces Mucosal Immune Responses and Effective Protection against Challenge. Vaccine 2018, 36, 2630–2636. [Google Scholar] [CrossRef]
- Hanafy, N.A.N.; El-Kemary, M.A. Silymarin/Curcumin Loaded Albumin Nanoparticles Coated by Chitosan as Muco-Inhalable Delivery System Observing Anti-Inflammatory and Anti COVID-19 Characterizations in Oleic Acid Triggered Lung Injury and in Vitro COVID-19 Experiment. Int. J. Biol. Macromol. 2022, 198, 101–110. [Google Scholar] [CrossRef]
- Dwivedi, P.; Tiwary, D.; Narvi, S.S.; Tewari, R.P.; Shukla, K.P. Curcuma Longa Aided Ag/CS Nanocomposite Coating of Surfaces as SARS-CoV-2 Contamination Minimizing Measure towards Containment of COVID-19: A Perspective. Lett. Appl. NanoBioSci 2020, 9, 1485–1493. [Google Scholar]
- Vörös-Horváth, B.; Živković, P.; Bánfai, K.; Bóvári-Biri, J.; Pongrácz, J.; Bálint, G.; Pál, S.; Széchenyi, A. Preparation and Characterization of ACE2 Receptor Inhibitor-Loaded Chitosan Hydrogels for Nasal Formulation to Reduce the Risk of COVID-19 Viral Infection. ACS Omega 2022, 7, 3240–3253. [Google Scholar] [CrossRef]
- Orkhan, F.; Melike, U.; Cihan, G.; Faruk, D.O.; Samet, B.; Ilknur, U.; Alemdar, J. Others RBD and ACE2 Embedded Chitosan Nanoparticles as a Prevention Approach for SARS-CoV 2. Biomed. J. Sci. Tech. Res. 2021, 37, 29193–29197. [Google Scholar]
- Rezaei, F.S.; Khorshidian, A.; Beram, F.M.; Derakhshani, A.; Esmaeili, J.; Barati, A. 3D Printed Chitosan/Polycaprolactone Scaffold for Lung Tissue Engineering: Hope to Be Useful for COVID-19 Studies. RSC Adv. 2021, 11, 19508–19520. [Google Scholar] [CrossRef]
- Loutfy, S.A.; Abdel-Salam, A.I.; Moatasim, Y.; Gomaa, M.R.; Abdel Fattah, N.F.; Emam, M.H.; Ali, F.; ElShehaby, H.A.; Ragab, E.A.; Alam El-Din, H.M.; et al. Antiviral Activity of Chitosan Nanoparticles Encapsulating Silymarin (Sil-CNPs) against SARS-CoV-2 (in Silico and in Vitro Study). RSC Adv. 2022, 12, 15775–15786. [Google Scholar] [CrossRef]
- Hathout, R.M.; Kassem, D.H. Positively Charged Electroceutical Spun Chitosan Nanofibers Can Protect Health Care Providers From COVID-19 Infection: An Opinion. Front. Bioeng. Biotechnol. 2020, 8, 885. [Google Scholar] [CrossRef]
- Wang, I.-J.; Chen, Y.-C.; Su, C.; Tsai, M.-H.; Shen, W.-T.; Bai, C.-H.; Yu, K.-P. Effectiveness of the Nanosilver/TiO2-Chitosan Antiviral Filter on the Removal of Viral Aerosols. J. Aerosol Med. Pulm. Drug Deliv. 2021, 34, 293–302. [Google Scholar] [CrossRef] [PubMed]
- Maharani, D.K.; Sanjaya, I.G.M.; Amaria, A.; Anggraeni, M.A.; Jannah, L.R. Molecular Docking Analysis Chitosan-Zeolite-ZnO Nanocomposite and Its Potency Against SARS-CoV-2. IOP Conf. Ser. Mater. Sci. Eng. 2021, 1125, 012006. [Google Scholar] [CrossRef]
- Sun, Q.; Li, X.; Che, X.; Chang, J.; Yang, Y.; Yu, L. Evaluation on the Immune Efficiency of Bovine Coronavirus N Protein-Loaded Chitosan Microspheres. Zhongguo Yufang Shouyi Xuebao/Chin. J. Prev. Vet. Med. 2009, 31, 882–886. [Google Scholar]
- Mohammadi, Z.; Eini, M.; Rastegari, A.; Tehrani, M.R. Chitosan as a Machine for Biomolecule Delivery: A Review. Carbohydr. Polym. 2021, 256, 117414. [Google Scholar] [CrossRef] [PubMed]
- Ejeromedoghene, O.; Oderïnde, O.; Egejuru, G.; Adewuyï, S. Chitosan-Drug Encapsulation as a Potential Candidate for COVID-19 Drug Delivery Systems: A Review. J. Turk. Chem. Soc. Sect. Chem. 2020, 7, 851–864. [Google Scholar] [CrossRef]
- Tatlow, D.; Tatlow, C.; Tatlow, S.; Tatlow, S. A Novel Concept for Treatment and Vaccination against COVID-19 with an Inhaled Chitosan-Coated DNA Vaccine Encoding a Secreted Spike Protein Portion. Clin. Exp. Pharmacol. Physiol. 2020, 47, 1874–1878. [Google Scholar] [CrossRef]
- Jaber, N.; Al-Remawi, M.; Al-Akayleh, F.; Al-Muhtaseb, N.; Al-Adham, I.S.I.; Collier, P.J. A Review of the Antiviral Activity of Chitosan, Including Patented Applications and Its Potential Use against COVID-19. J. Appl. Microbiol. 2022, 132, 41–58. [Google Scholar] [CrossRef]
- Kalathiya, U.; Padariya, M.; Mayordomo, M.; Lisowska, M.; Nicholson, J.; Singh, A.; Baginski, M.; Fahraeus, R.; Carragher, N.; Ball, K.; et al. Highly Conserved Homotrimer Cavity Formed by the SARS-CoV-2 Spike Glycoprotein: A Novel Binding Site. J. Clin. Med. Res. 2020, 9, 1473. [Google Scholar] [CrossRef]
- Alitongbieke, G.; Li, X.-M.; Wu, Q.-C.; Lin, Z.-C.; Huang, J.-F.; Xue, Y.; Liu, J.-N.; Lin, J.-M.; Pan, T.; Chen, Y.-X.; et al. Effect of β-Chitosan on the Binding Interaction between SARS-CoV-2 S-RBD and ACE2. bioRxiv 2020. preprint. [Google Scholar] [CrossRef]
- Itani, R.; Tobaiqy, M.; Al Faraj, A. Optimizing Use of Theranostic Nanoparticles as a Life-Saving Strategy for Treating COVID-19 Patients. Theranostics 2020, 10, 5932–5942. [Google Scholar] [CrossRef]
- Pyrć, K.; Milewska, A.; Duran, E.B.; Botwina, P.; Lopes, R.; Arenas-Pinto, A.; Badr, M.; Mellor, R.; Kalber, T.L.; Fernandes-Reyes, D.; et al. SARS-CoV-2 Inhibition in Human Airway Epithelial Cells Using a Mucoadhesive, Amphiphilic Chitosan That May Serve as an Anti-Viral Nasal Spray. bioRxiv 2020. preprint. [Google Scholar] [CrossRef]
- Cho, N.J.; Glenn, J.S. Materials Science Approaches in the Development of Broad-Spectrum Antiviral Therapies. Nat. Mater. 2020, 19, 813–816. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).