Impact of COVID-19 Pandemic on Antibiotic Utilisation in Malaysian Primary Care Clinics: An Interrupted Time Series Analysis
Abstract
1. Introduction
2. Results
2.1. Antibiotic Utilisation Trends
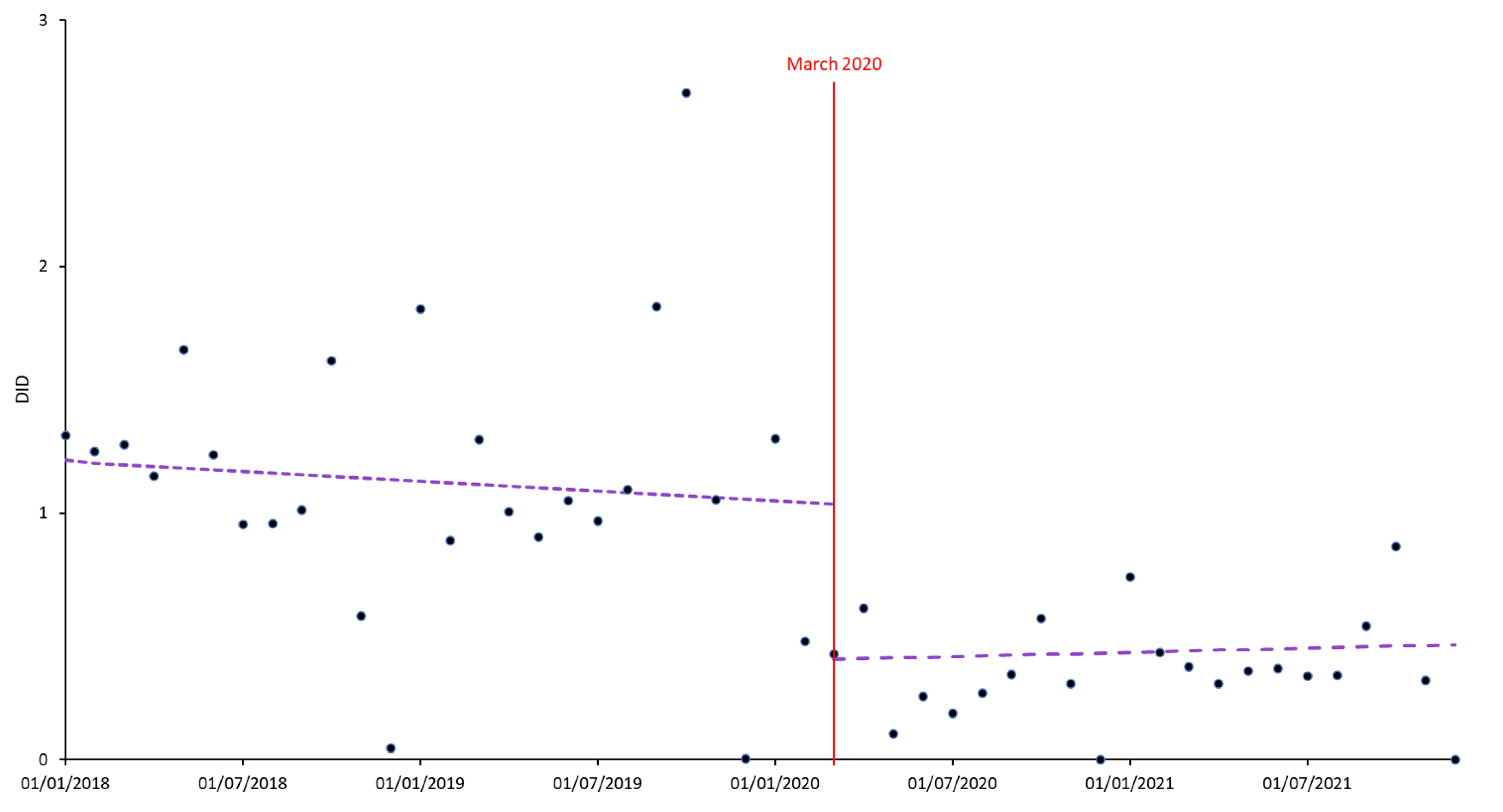
2.2. Impact of the COVID-19 Pandemic
3. Discussion
4. Materials and Methods
4.1. Setting
- Pre-COVID: January 2018–February 2020;
- Post-COVID onset: March 2020–December 2021.
4.2. Study Design and Data Source
4.3. Antibiotics
4.4. Outcome
4.5. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Elengoe, A. COVID-19 Outbreak in Malaysia. Osong Public Health Res. Perspect. 2020, 11, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Cong, W.; Poudel, A.N.; Alhusein, N.; Wang, H.; Yao, G.; Lambert, H. Antimicrobial Use in COVID-19 Patients in the First Phase of the SARS-CoV-2 Pandemic: A Scoping Review. Antibiotics 2021, 10, 745. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N.; Aylin, P.; Rawson, T.; Gilchrist, M.; Majeed, A.; Holmes, A. Investigating the impact of COVID-19 on primary care antibiotic prescribing in North West London across two epidemic waves. Clin. Microbiol. Infect. 2021, 27, 762–768. [Google Scholar] [CrossRef]
- Mamun, A.A.; Saatchi, A.; Xie, M.; Lishman, H.; Blondel-Hill, E.; Marra, F.; Patrick, D.M. Community Antibiotic Use at the Population Level During the SARS-CoV-2 Pandemic in British Columbia, Canada. In Open Forum Infectious Diseases; Oxford University Press: Newyork, NY, USA, 2021; Volume 8. [Google Scholar]
- Rawson, T.M.; Moore, L.; Castro-Sanchez, E.; Charani, E.; Davies, F.; Satta, G.; Ellington, M.J.; Holmes, A.H. COVID-19 and the potential long-term impact on antimicrobial resistance. J. Antimicrob. Chemother. 2020, 75, 1681–1684. [Google Scholar] [CrossRef] [PubMed]
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Wang, S.; Meng, R.; Liu, G.; Hu, J.; Zhang, H.; Yan, S.; Zhan, S. Appropriateness of Antibiotic Prescriptions in Chinese Primary Health Care and the Impact of the COVID-19 Pandemic: A Typically Descriptive and Longitudinal Database Study in Yinchuan City. Front. Pharmacol. 2022, 13, 861782. [Google Scholar] [CrossRef]
- Knight, B.D.; Shurgold, J.; Smith, G.; MacFadden, D.R.; Schwartz, K.L.; Daneman, N.; Tropper, D.G.; Brooks, J. The impact of COVID-19 on community antibiotic use in Canada: An ecological study. Clin. Microbiol. Infect. 2022, 28, 426–432. [Google Scholar] [CrossRef]
- Malcolm, W.; A Seaton, R.; Haddock, G.; Baxter, L.; Thirlwell, S.; Russell, P.; Cooper, L.; Thomson, A.; Sneddon, J. Impact of the COVID-19 pandemic on community antibiotic prescribing in Scotland. JAC Antimicrob. Resist. 2020, 2, dlaa105. [Google Scholar] [CrossRef]
- Al-Azzam, S.; Mhaidat, N.; Banat, H.; Alfaour, M.; Ahmad, D.; Muller, A.; Al-Nuseirat, A.; Lattyak, E.; Conway, B.; Aldeyab, M. An Assessment of the Impact of Coronavirus Disease (COVID-19) Pandemic on National Antimicrobial Consumption in Jordan. Antibiotics 2021, 10, 690. [Google Scholar] [CrossRef]
- Silva, T.M.; Estrela, M.; Gomes, E.R.; Piñeiro-Lamas, M.; Figueiras, A.; Roque, F.; Herdeiro, M.T. The Impact of the COVID-19 Pandemic on Antibiotic Prescribing Trends in Outpatient Care: A Nationwide, Quasi-Experimental Approach. Antibiotics 2021, 10, 1040. [Google Scholar] [CrossRef]
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behaviour. 2021, 5, 529–538. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. 2021 AWaRe Classification: World Health Organization. 2021. Available online: https://www.who.int/publications/i/item/2021-aware-classification (accessed on 16 January 2023).
- Andrews, A.; Budd, E.; Hendrick, A.; Ashiru-Oredope, D.; Beech, E.; Hopkins, S.; Gerver, S.; Muller-Pebody, B.; The AMU COVID-19 Stakeholder Group. Surveillance of Antibacterial Usage during the COVID-19 Pandemic in England, 2020. Antibiotics 2021, 10, 841. [Google Scholar] [CrossRef]
- Del Fiol, F.D.S.; Bergamaschi, C.D.C.; De Andrade, I.P.; Lopes, L.C.; Silva, M.T.; Barberato-Filho, S. Consumption Trends of Antibiotics in Brazil During the COVID-19 Pandemic. Front. Pharmacol. 2022, 13, 844818. [Google Scholar] [CrossRef]
- Izzatur Rahmi, M.U.; Normaizira, H.; Samsiah, A.; Nur Wahida, Z.; Jabrullah, A.H.; Divya Nair, N.; Khalidah, M.; Nurhayati, S.; Roslina, S.; Mariyah, M.; et al. The impact of COVID-19 pandemic on outpatient service in public primary care clinics in Malaysia. In Proceedings of the 7th Asia-Pacific Conference on Public Health (APCPH), Shah Alam, Malaysia, 2–4 August 2022. [Google Scholar]
- Ng, S.W.; Hwong, W.Y.; Husin, M.; Ab Rahman, N.; Nasir, N.H.; Juval, K.; Sivasampu, S. Assessing the Availability of Teleconsultation and the Extent of Its Use in Malaysian Public Primary Care Clinics: Cross-sectional Study. JMIR Res. 2022, 6, e34485. [Google Scholar] [CrossRef] [PubMed]
- Tanislav, C.; Kostev, K. Investigation of the prevalence of non-COVID-19 infectious diseases during the COVID-19 pandemic. Public Health 2022, 203, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. National Antimicrobial Guideline 2019; Pharmaceutical Services Programme; Ministry of Health: Petaling Jaya, Malaysia, 2019.
- Ministry of Health. National Antibiotic Guideline 2014; Pharmaceutical Services Programme; Ministry of Health: Petaling Jaya, Malaysia, 2014.
- Lopez Bernal, J.; Cummins, S.; Gasparrini, A. The use of controls in interrupted time series studies of public health interventions. Int. J. Epidemiol. 2018, 47, 2082–2093. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Health Indicators; Health Informatic Centre, Planning Division, Ministry of Heatlh Malaysia: Putrajaya, Malaysia, 2020.
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef]
- Ong, S.M.; Lim, M.T.; Fah Tong, S.; Kamaliah, M.N.; Groenewegen, P.; Sivasampu, S. Comparative performance of public and private primary care service delivery in Malaysia: An analysis of findings from QUALICOPC. PLoS ONE 2022, 17, e0276480. [Google Scholar] [CrossRef]
- Ministry of Health. Malaysian Statistics on Medicine 2015–2016; Pharmaceutical Services Programme: Petaling Jaya, Malaysia, 2020.
- Department of Statistics Malaysia. Population Quick Info 2022. Available online: https://pqi.stats.gov.my/search.php?tahun=2021&kodData=2&kodJadual=1&kodCiri=2&kodNegeri=Semua (accessed on 1 October 2022).
- World Health Organization. Guidelines for ATC Classification and DDD Assignment 2013. 2020. Available online: https://www.who.int/classifications/atcddd/en/ (accessed on 29 December 2020).
- World Health Organization. Defined Daily Dose (DDD). 2023. Available online: https://www.who.int/tools/atc-ddd-toolkit/about-ddd#:~:text=Defined%20Daily%20Dose%20(DDD)%3A,medicines%20given%20an%20ATC%20codes (accessed on 29 December 2020).
- Wagner, A.K.; Soumerai, S.B.; Zhang, F.; Ross-Degnan, D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Ther. 2002, 27, 299–309. [Google Scholar] [CrossRef]
- Penfold, R.B.; Zhang, F. Use of Interrupted Time Series Analysis in Evaluating Health Care Quality Improvements. Acad. Pediatr. 2013, 13 (Suppl. 6), S38–S44. [Google Scholar] [CrossRef]
- Jandoc, R.; Burden, A.M.; Mamdani, M.; Lévesque, L.E.; Cadarette, S.M. Interrupted time series analysis in drug utilization research is increasing: Systematic review and recommendations. J. Clin. Epidemiol. 2015, 68, 950–956. [Google Scholar] [CrossRef]
- Turner, S.L.; Forbes, A.B.; Karahalios, A.; Taljaard, M.; McKenzie, J.E. Evaluation of statistical methods used in the analysis of interrupted time series studies: A simulation study. BMC Med. Res. Methodol. 2021, 21, 181. [Google Scholar] [CrossRef] [PubMed]
- Jalil, A.; Rao, N.H. Chapter 8—Time Series Analysis (Stationarity, Cointegration, and Causality). In Environmental Kuznets Curve (EKC); Özcan, B., Öztürk, I., Eds.; Academic Press: Cambridge, MA, USA, 2019; pp. 85–99. [Google Scholar]
- Shively, T.S.; Ansley, C.F.; Kohn, R. Fast Evaluation of the Distribution of the Durbin-Watson and Other Invariant Test Statistics in Time Series Regression. J. Am. Stat. Assoc. 1990, 85, 676–685. [Google Scholar] [CrossRef]
- Cumby, R.; Huizinga, J. Testing the Autocorrelation Structure of Disturbances in Ordinary Least Squares and Instrumental Variables Regressions. Econometrica 1992, 60, 185–195. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 15; StataCorp LLC: College Station, TX, USA, 2017. [Google Scholar]


| Antibiotic Class | Drug | Annual DID * | |||
|---|---|---|---|---|---|
| 2018 | 2019 | 2020 | 2021 | ||
| Cephalosporin | Ceftriaxone | <0.001 | <0.001 | <0.001 | <0.001 |
| Cefuroxime | 0.007 | 0.011 | 0.004 | 0.012 | |
| Cephalexin | 0.045 | 0.057 | 0.029 | 0.048 | |
| Macrolide | Azithromycin | 0.001 | 0.007 | 0.001 | 0.004 |
| Erythromycin ethylsuccinate | 0.087 | 0.063 | 0.018 | 0.009 | |
| Nitrofuran | Nitrofurantoin | 0.001 | 0.003 | 0.002 | 0.002 |
| Nitroimidazole | Metronidazole | 0.062 | 0.035 | 0.018 | 0.022 |
| Penicillin | Amoxycillin | 0.629 | 0.691 | 0.207 | 0.126 |
| Ampicillin | 0.001 | 0.002 | 0.001 | 0.003 | |
| Amoxycillin–clavulanic acid | 0.010 | 0.026 | 0.007 | 0.016 | |
| Benzathine penicillin | <0.001 | 0.001 | <0.001 | 0.001 | |
| Benzylpenicillin | <0.001 | <0.001 | <0.001 | <0.001 | |
| Cloxacillin | 0.197 | 0.238 | 0.086 | 0.118 | |
| Phenoxymethyl penicillin | 0.007 | 0.019 | 0.003 | 0.005 | |
| Sulfonamide | Trimethoprim–sulfamethoxazole | 0.002 | 0.004 | 0.002 | 0.004 |
| Tetracycline | Doxycycline | 0.023 | 0.045 | 0.022 | 0.040 |
| Tetracycline | <0.001 | <0.001 | <0.001 | <0.001 | |
| Independent Variables | Coefficient | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Trend before COVID-19 * | −0.007 | −0.037 to 0.023 | 0.659 |
| Level change | −0.707 | −1.309 to −0.105 | 0.022 |
| Slope change | 0.009 | −0.025 to 0.044 | 0.583 |
| Intercept | 1.217 | 0.930 to 1.503 | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, A.H.; Ab Rahman, N.; Hashim, H.; Kamal, M.; Velvanathan, T.; Chok, M.C.F.; Sivasampu, S. Impact of COVID-19 Pandemic on Antibiotic Utilisation in Malaysian Primary Care Clinics: An Interrupted Time Series Analysis. Antibiotics 2023, 12, 659. https://doi.org/10.3390/antibiotics12040659
Lim AH, Ab Rahman N, Hashim H, Kamal M, Velvanathan T, Chok MCF, Sivasampu S. Impact of COVID-19 Pandemic on Antibiotic Utilisation in Malaysian Primary Care Clinics: An Interrupted Time Series Analysis. Antibiotics. 2023; 12(4):659. https://doi.org/10.3390/antibiotics12040659
Chicago/Turabian StyleLim, Audrey Huili, Norazida Ab Rahman, Hazimah Hashim, Mardhiyah Kamal, Tineshwaran Velvanathan, Mary Chiew Fong Chok, and Sheamini Sivasampu. 2023. "Impact of COVID-19 Pandemic on Antibiotic Utilisation in Malaysian Primary Care Clinics: An Interrupted Time Series Analysis" Antibiotics 12, no. 4: 659. https://doi.org/10.3390/antibiotics12040659
APA StyleLim, A. H., Ab Rahman, N., Hashim, H., Kamal, M., Velvanathan, T., Chok, M. C. F., & Sivasampu, S. (2023). Impact of COVID-19 Pandemic on Antibiotic Utilisation in Malaysian Primary Care Clinics: An Interrupted Time Series Analysis. Antibiotics, 12(4), 659. https://doi.org/10.3390/antibiotics12040659





