Pharmacokinetic/Pharmacodynamic Target Attainment of Ceftazidime in Adult Patients on General Wards with Different Degrees of Renal Function: A Prospective Observational Bicenter Cohort Study
Abstract
:1. Introduction
2. Results
2.1. Patients and Ceftazidime Concentrations
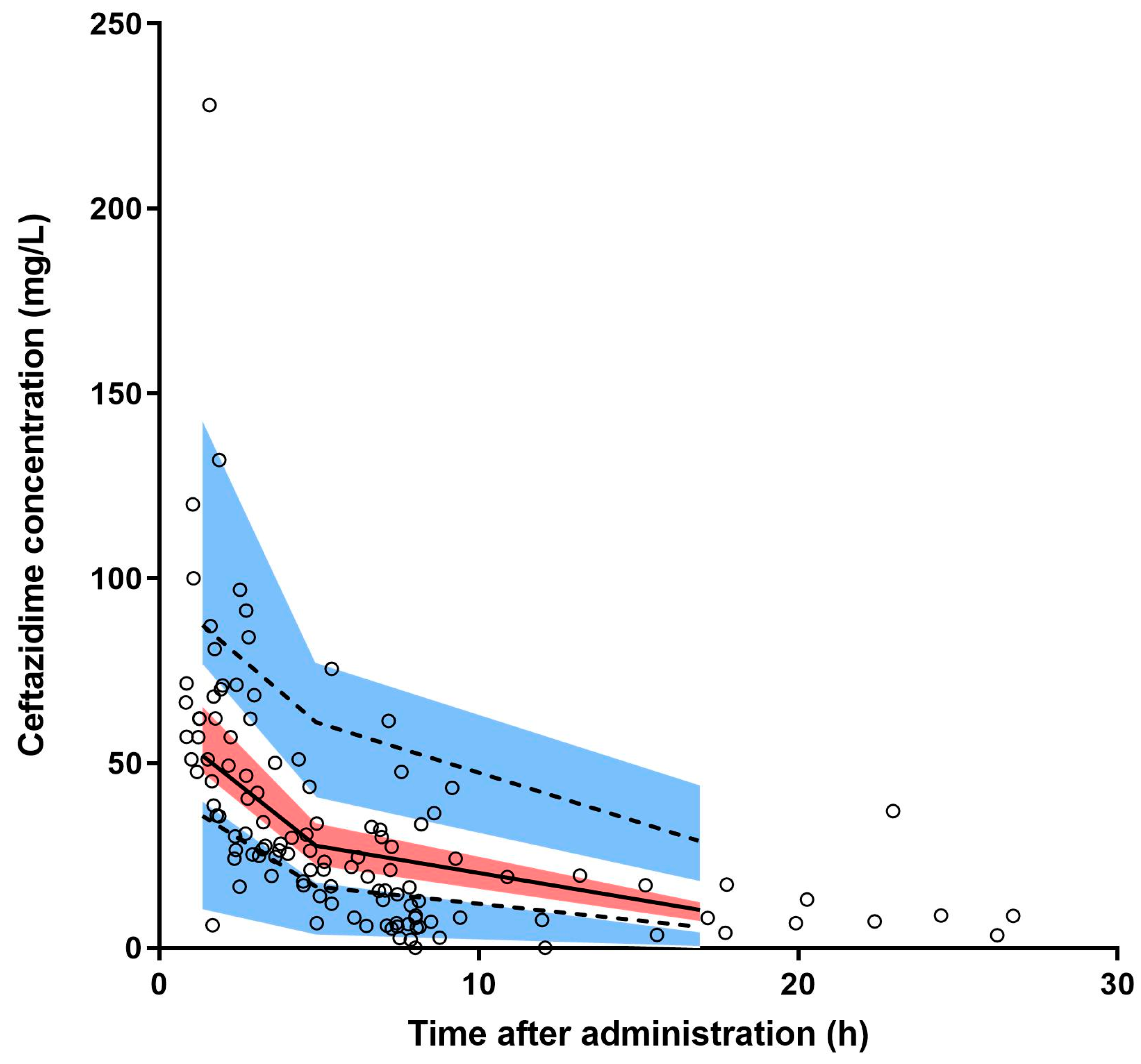
2.2. Population Pharmacokinetic Analysis
2.3. Pharmacokinetic/Pharmacodynamic Target Attainment
2.4. Monte Carlo Dosing Simulations
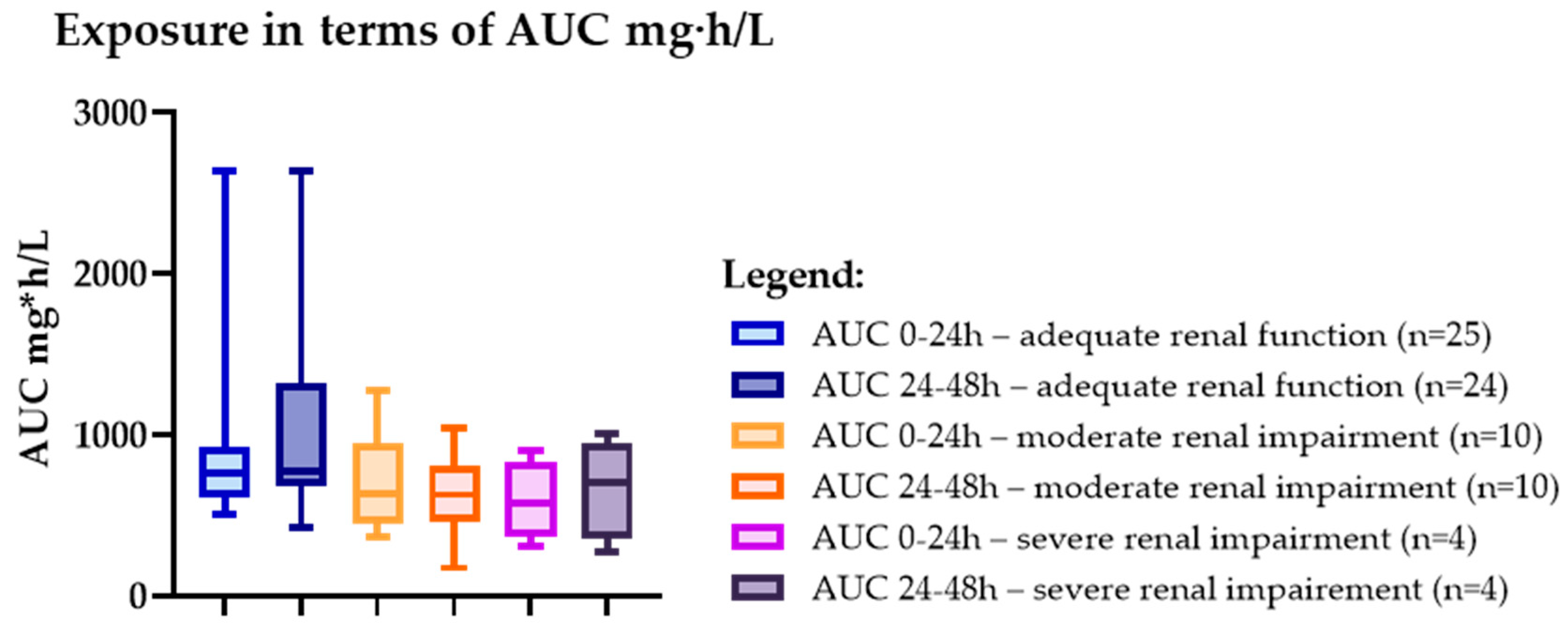
2.5. Drug Exposure
2.6. Clinical Outcome Measure
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. In- and Exclusion Criteria
4.3. Sample Size Calculation
4.4. Study Procedure
4.5. Study Outcomes
- Group I: adequate renal function; eGFR ≥ 50 mL/min/1.73 m2 treated with regular doses of ceftazidime (2000 mg q8).
- Group II: moderately impaired renal function; eGFR 30–49 mL/min/1.73 m2 treated with reduced doses of ceftazidime (1000 mg q12).
- Group III: severely impaired renal function; eGFR 10–29 mL/min/1.73 m2 treated with reduced doses of ceftazidime (1000 mg q24).
4.6. Statistical Analysis & Pharmacokinetic Model
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Andersson, M.; Östholm-Balkhed, Å.; Fredrikson, M.; Holmbom, M.; Hällgren, A.; Berg, S.; Hanberger, H. Delay of appropriate antibiotic treatment is associated with high mortality in patients with community-onset sepsis in a Swedish setting. Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 1223–1234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schuts, E.C.; Hulscher, M.E.J.L.; Mouton, J.W.; Verduin, C.M.; Stuart, J.W.T.C.; Overdiek, H.W.P.M.; van der Linden, P.D.; Natsch, S.; Hertogh, C.M.P.M.; Wolfs, T.F.W.; et al. Current evidence on hospital antimicrobial stewardship objectives: A systematic review and meta-analysis. Lancet Infect. Dis. 2016, 16, 847–856. [Google Scholar] [CrossRef] [PubMed]
- McCabe, C.; Kirchner, C.; Zhang, H.; Daley, J.; Fisman, D.N. Guideline-concordant therapy and reduced mortality and length of stay in adults with community-acquired pneumonia: Playing by the rules. Arch. Intern. Med. 2009, 169, 1525–1531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Onufrak, N.J.; Forrest, A.; Gonzalez, D. Pharmacokinetic and Pharmacodynamic Principles of Anti-infective Dosing. Clin. Ther. 2016, 38, 1930–1947. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nielsen, E.I.; Cars, O.; Friberg, L.E. Pharmacokinetic/pharmacodynamic (PK/PD) indices of antibiotics predicted by a semimechanistic PKPD model: A step toward model-based dose optimization. Antimicrob. Agents Chemother. 2011, 55, 4619–4630. [Google Scholar] [CrossRef] [Green Version]
- Arumugham, V.B.; Gujarathi, R.; Cascella, M. Third Generation Cephalosporins. In StatPearls; StatPearls Publishing: Tampa, FL, USA, 2022. [Google Scholar]
- Dhaese, S.; Van Vooren, S.; Boelens, J.; De Waele, J. Therapeutic drug monitoring of β-lactam antibiotics in the ICU. Expert Rev. Anti Infect. Ther. 2020, 18, 1155–1164. [Google Scholar] [CrossRef]
- McKinnon, P.S.; Paladino, J.A.; Schentag, J.J. Evaluation of area under the inhibitory curve (AUIC) and time above the minimum inhibitory concentration (T>MIC) as predictors of outcome for cefepime and ceftazidime in serious bacterial infections. Int. J. Antimicrob. Agents 2008, 31, 345–351. [Google Scholar] [CrossRef]
- Muller, A.E.; Punt, N.; Mouton, J.W. Optimal exposures of ceftazidime predict the probability of microbiological and clinical outcome in the treatment of nosocomial pneumonia. J. Antimicrob. Chemother. 2013, 68, 900–906. [Google Scholar] [CrossRef] [Green Version]
- MacVane, S.H.; Crandon, J.L.; Nichols, W.W.; Nicolau, D.P. In vivo efficacy of humanized exposures of Ceftazidime-Avibactam in comparison with Ceftazidime against contemporary Enterobacteriaceae isolates. Antimicrob. Agents Chemother. 2014, 58, 6913–6919. [Google Scholar] [CrossRef] [Green Version]
- Mouton, J.W.; Muller, A.E.; Canton, R.; Giske, C.G.; Kahlmeter, G.; Turnidge, J. MIC-based dose adjustment: Facts and fables. J. Antimicrob. Chemother. 2018, 73, 564–568. [Google Scholar] [CrossRef] [Green Version]
- KNMP Kennisbank-Ceftazidime. Available online: https://kennisbank.knmp.nl/article/Informatorium_Medicamentorum/S1884.html (accessed on 13 January 2023).
- Farmacotherapeutisch Kompas (FK)-Ceftazidime. Available online: https://www.farmacotherapeutischkompas.nl/bladeren/preparaatteksten/c/ceftazidim (accessed on 13 January 2023).
- SWAB-Ceftazidime. Available online: https://adult.nl.antibiotica.app/en/node/1176 (accessed on 13 January 2023).
- van Daalen, F.V.; Prins, J.M.; Opmeer, B.C.; Boermeester, M.A.; Visser, C.E.; van Hest, R.M.; Branger, J.; Mattsson, E.; van de Broek, M.F.M.; Roeleveld, T.C.; et al. Effect of an antibiotic checklist on length of hospital stay and appropriate antibiotic use in adult patients treated with intravenous antibiotics: A stepped wedge cluster randomized trial. Clin. Microbiol. Infect. 2017, 23, 485.e1–485.e8. [Google Scholar] [CrossRef]
- de Vroom, S.L.; van Daalen, F.V.; Zieck, S.E.; Mathôt, R.A.A.; van Hest, R.M.; Geerlings, S.E. Does dose reduction of renally cleared antibiotics in patients with impaired renal function lead to adequate drug exposure? A systematic review. Clin. Microbiol. Infect. 2021, 27, 352–363. [Google Scholar] [CrossRef] [PubMed]
- Welage, L.S.; Schultz, R.W.; Schentag, J.J. Pharmacokinetics of ceftazidime in patients with renal insufficiency. Antimicrob. Agents Chemother. 1984, 25, 201–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leroy, A.; Leguy, F.; Borsa, F.; Spencer, G.R.; Fillastre, J.P.; Humbert, G. Pharmacokinetics of ceftazidime in normal and uremic subjects. Antimicrob. Agents Chemother. 1984, 25, 638–642. [Google Scholar] [CrossRef] [Green Version]
- Ackerman, B.H.; Ross, J.; Tofte, R.W.; Rotschafer, J.C. Effect of decreased renal function on the pharmacokinetics of ceftazidime. Antimicrob. Agents Chemother. 1984, 25, 785–786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walstad, R.A.; Dahl, K.; Hellum, K.B.; Thurmann-Nielsen, E. The pharmacokinetics of ceftazidime in patients with impaired renal function and concurrent frusemide therapy. Eur. J. Clin. Pharmacol. 1988, 35, 273–279. [Google Scholar] [CrossRef]
- Roberts, J.A.; Lipman, J. Pharmacokinetic issues for antibiotics in the critically ill patient. Crit. Care Med. 2009, 37, 840–851. [Google Scholar] [CrossRef] [Green Version]
- European Committee on Antimicrobial Susceptibility Testing (EUCAST). Clinical Breakpoints Table for Bacteria (v 11.0). Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_11.0_Breakpoint_Tables.xlsx (accessed on 17 March 2021).
- de Vroom, S.L.; van Hest, R.M.; van Daalen, F.V.; Kuil, S.D.; Mathôt, R.A.A.; Geerlings, S.E.; Jager, N.G.L. Pharmacokinetic/pharmacodynamic target attainment of ciprofloxacin in adult patients on general wards with adequate and impaired renal function. Int. J. Antimicrob. Agents 2020, 56, 1061–1066. [Google Scholar] [CrossRef]
- Mazuski, J.E.; Gasink, L.B.; Armstrong, J.; Broadhurst, H.; Stone, G.G.; Rank, D.; Llorens, L.; Newell, P.; Pachl, J. Efficacy and Safety of Ceftazidime-Avibactam Plus Metronidazole Versus Meropenem in the Treatment of Complicated Intra-abdominal Infection: Results From a Randomized, Controlled, Double-Blind, Phase 3 Program. Clin. Infect. Dis. 2016, 62, 1380–1389. [Google Scholar] [CrossRef] [Green Version]
- Werumeus Buning, A.; Hodiamont, C.J.; Lechner, N.M.; Schokkin, M.; Elbers, P.W.G.; Juffermans, N.P.; Mathôt, R.A.A.; de Jong, M.D.; van Hest, R.M. Population Pharmacokinetics and Probability of Target Attainment of Different Dosing Regimens of Ceftazidime in Critically Ill Patients with a Proven or Suspected Pseudomonas aeruginosa Infection. Antibiotics 2021, 21, 612. [Google Scholar] [CrossRef]
- Vidal, L.; Shavit, M.; Fraser, A.; Paul, M.; Leibovici, L. Systematic comparison of four sources of drug information regarding adjustment of dose for renal function. BMJ 2005, 331, 263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crass, R.L.; Rodvold, K.A.; Mueller, B.A.; Pai, M.P. Renal Dosing of Antibiotics: Are We Jumping the Gun? Clin. Infect. Dis. 2019, 68, 1596–1602. [Google Scholar] [CrossRef] [PubMed]
- Camargo, M.S.; Mistro, S.; Oliveira, M.G.; Passos, L.C.S. Association between increased mortality rate and antibiotic dose adjustment in intensive care unit patients with renal impairment. Eur. J. Clin. Pharmacol. 2019, 75, 119–126. [Google Scholar] [CrossRef] [PubMed]
- WMA Declaration of Helsinki–Ethical Principles for Medical Research Involving Human Subjects, October 2013. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 12 February 2023).
- WMO Medical Research Involving Human Subjects Act. Available online: https://wetten.overheid.nl/BWBR0009408/2022-07-01 (accessed on 12 February 2023).
- Gómez, C.M.H.; Cordingly, J.J.; Palazzo, M.G.A. Altered pharmacokinetics of ceftazidime in critically ill patients. Antimicrob. Agents Chemother. 1999, 43, 1798–1802. [Google Scholar] [CrossRef] [Green Version]
- Pruskowski, K.A. Pharmacokinetics and Pharmacodynamics of Antimicrobial Agents in Burn Patients. Surg. Infect. 2021, 22, 77–82. [Google Scholar] [CrossRef]
- Kercsmar, C.M.; Stern, R.C.; Reed, M.D.; Myers, C.M.; Murdell, D.; Blumer, J.L. Ceftazidime in cystic fibrosis: Pharmacokinetics and therapeutic response. J. Antimicrob. Chemother. 1983, 12, 289–295. [Google Scholar] [CrossRef]
- Delattre, I.K.; Hites, M.; Laterre, P.F.; Dugernier, T.; Spapen, H.; Wallemacq, P.E.; Jacobs, F.; Taccone, F.S. What is the optimal loading dose of broad-spectrum β-lactam antibiotics in septic patients? Results from pharmacokinetic simulation modelling. Int. J. Antimicrob. Agents 2020, 56, 106–113. [Google Scholar] [CrossRef] [PubMed]

| Renal Function Group | Guideline-Recommended Dose of Ceftazidime |
|---|---|
| Adequate renal function (eGFR ≥ 50 mL/min/1.73 m2, (n = 25)) | 2000 mg q8h |
| Moderate renal impairment (eGFR ≥ 30–50 mL/min/1.73 m2, (n = 10)) | 1000 mg q12h |
| Severe renal impairment (eGFR < 30 mL/min/1.73 m2, (n = 5)) | 1000 mg q24h |
| Variable * | Overall | eGFR a | eGFR a | eGFR a |
|---|---|---|---|---|
| ≥50 mL/min/1.73 m2 | ≥30–50/1.73 m2 | <30 mL/min/1.73 m2 | ||
| n = 40 | n = 25 | n = 10 | n = 5 | |
| Female, n | 17 | 9 | 6 | 2 |
| Age, yrs | 62.0 | 56.0 (40.5–68.5) | 72.0 | 64.0 |
| (47.0–72.0) | (69.8–86.0) | (41.5–73.0) | ||
| Weight, kg | 79.6 | 80.0 | 78.5 | 71.7 |
| (69.7–92.3) | (71.8–89.0) | (67.2–94.3) | (57.1–140.6) | |
| Height, cm | 175.5 | 180.0 | 171.5 | 167.0 |
| (167.0–185.0) | (168.0–185.0) | (163.5–184.3) | (163.0–179.5) | |
| BMI, kg/m2 | 25.0 | 24.7 | 26.2 | 23.4 |
| (22.0–29.0) | (21.3–27.8) | (23.7–31.4) | (21.3–46.5) | |
| Ethnicity | ||||
| Caucasian | 32 | 22 | 8 | 2 |
| African American | 4 | 1 | 2 | 1 |
| Asian | 3 | 1 | 0 | 2 |
| Hispanic | 1 | 1 | 0 | 0 |
| Serum creatinine | 100.0 | 72.0 | 135 | 328.0 |
| (67.3–135.3) | (59.5–92.5) | (118–162) | (217.5–430.0) | |
| eGFR a, mL/min/1.73 m2 | 73.5 | 102.8 | 34.3 | 18.6 |
| (34.3–111.4) | (78.1–124.8) | (30.9–48.2) | (10.6–25.9) | |
| Fever at start of treatment, yes | 11 | 7 | 3 | 1 |
| Department of admission | ||||
| Cardiology | 1 | 1 | 0 | 0 |
| Hematology | 7 | 7 | 0 | 0 |
| Infectious diseases | 4 | 1 | 2 | 1 |
| Internal medicine | 5 | 1 | 3 | 1 |
| Nephrology | 2 | 0 | 0 | 2 |
| Neurology | 1 | 1 | 0 | 0 |
| Oncology | 1 | 1 | 0 | 0 |
| Orthopedic | 12 | 10 | 1 | 1 |
| Respiratory medicine | 4 | 1 | 3 | 0 |
| Surgery | 2 | 1 | 1 | 0 |
| Urology | 1 | 1 | 0 | 0 |
| Concomitant other antibiotic use | 27 | 19 | 6 | 2 |
| Length of hospital stay b | 10.0 | 11.0 | 12.0 | 10 |
| (7–20.3) | (7.5–28.0) | (7.0–21.8) | (5.5–10.5) |
| Parameter | Structural Model | Final Model * | Bootstrap | |||
|---|---|---|---|---|---|---|
| Estimate | RSE (%) [Shrinkage (%)] | Estimate | RSE (%) [Shrinkage (%)] | Estimate | 95% CI | |
| CL (L/h) | 4.50 | 11.7 | 3.74 | 9.80 | 3.74 | 3.03–4.41 |
| V (L) | 22.7 | 7.20 | 21.8 | 7.90 | 22.1 | 19.1–25.1 |
| Interindividual variability | ||||||
| CL (%CV) | 78.9 | 20.3 [1.3] | 31.3 | 29.6 [7] | 31.1 | 22.6–38.7 |
| V (%CV) | 40.5 | 64.7 [21] | 40.2 | 61.8 [18] | 40.9 | 10.0–59.2 |
| Residual variability | ||||||
| Proportional error (%) | 19.2 | 15.0 | 18.6 | 15.9 | 18.7 | 13.9–23.6 |
| Covariates | ||||||
| eGFR (CKD-EPI) (mL/min/1.73 m2) on CL | - | - | 0.75 | 13.9 | 0.74 | 0.56–0.93 |
| Concomitant antibiotic use on CL | - | - | 1.56 | 12.4 | 1.57 | 1.20–1.94 |
| PTA (50% T0–24 > MIC) | |||||||
|---|---|---|---|---|---|---|---|
| MIC (mg/L) | 0.125 | 0.25 | 0.5 | 1 | 2 | 4 | 8 |
| Renal Function Group | |||||||
| Adequate renal function (eGFR ≥ 50 mL/min/1.73 m2, (n = 25)) | 100% | 100% | 100% | 100% | 100% | 100% | 100% |
| Moderate renal impairment (eGFR ≥ 30–50 mL/min/1.73 m2, (n = 10)) | 100% | 100% | 90% | 90% | 90% | 90% | 90% |
| Severe renal impairment (eGFR < 30 mL/min/1.73 m2, (n = 5)) | 100% | 100% | 100% | 100% | 100% | 100% | 100% |
| PTA (100% T0–24 > MIC) | |||||||
|---|---|---|---|---|---|---|---|
| MIC (mg/L) | 0.125 | 0.25 | 0.5 | 1 | 2 | 4 | 8 |
| Renal Function Group | |||||||
| Adequate renal function (eGFR ≥ 50 mL/min/1.73 m2, (n = 25)) | 100% | 100% | 100% | 100% | 56% | 48% | 24% |
| Moderate renal impairment (eGFR ≥ 30–50 mL/min/1.73 m2, (n = 10)) | 90% | 90% | 90% | 90% | 90% | 80% | 50% |
| Severe renal impairment (eGFR < 30 mL/min/1.73 m2, (n = 4)) | 100% | 100% | 100% | 100% | 100% | 100% | 75% |
| PTA (50% T24–48 > MIC) | |||||||
|---|---|---|---|---|---|---|---|
| MIC (mg/L) | 0.125 | 0.25 | 0.5 | 1 | 2 | 4 | 8 |
| Renal Function Group | |||||||
| Adequate renal function (eGFR ≥ 50 mL/min/1.73 m2, (n = 24)) | 100% | 100% | 100% | 100% | 100% | 100% | 100% |
| Moderate renal impairment (eGFR ≥ 30–50 mL/min/1.73 m2, (n = 10)) | 90% | 90% | 90% | 90% | 90% | 90% | 90% |
| Severe renal impairment (eGFR < 30 mL/min/1.73 m2, (n = 4)) | 100% | 100% | 100% | 100% | 100% | 100% | 100% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zieck, S.E.; de Vroom, S.L.; Mulder, F.P.; van Twillert, G.; Mathôt, R.A.A.; Geerlings, S.E.; van Hest, R.M. Pharmacokinetic/Pharmacodynamic Target Attainment of Ceftazidime in Adult Patients on General Wards with Different Degrees of Renal Function: A Prospective Observational Bicenter Cohort Study. Antibiotics 2023, 12, 469. https://doi.org/10.3390/antibiotics12030469
Zieck SE, de Vroom SL, Mulder FP, van Twillert G, Mathôt RAA, Geerlings SE, van Hest RM. Pharmacokinetic/Pharmacodynamic Target Attainment of Ceftazidime in Adult Patients on General Wards with Different Degrees of Renal Function: A Prospective Observational Bicenter Cohort Study. Antibiotics. 2023; 12(3):469. https://doi.org/10.3390/antibiotics12030469
Chicago/Turabian StyleZieck, Saskia E., Suzanne L. de Vroom, Frouke Ph. Mulder, Gitte van Twillert, Ron A. A. Mathôt, Suzanne E. Geerlings, and Reinier M. van Hest. 2023. "Pharmacokinetic/Pharmacodynamic Target Attainment of Ceftazidime in Adult Patients on General Wards with Different Degrees of Renal Function: A Prospective Observational Bicenter Cohort Study" Antibiotics 12, no. 3: 469. https://doi.org/10.3390/antibiotics12030469





