Macrolides at Clinically-Relevant Concentrations May Induce Biofilm Formation in Macrolide-Resistant Staphylococcus aureus
Abstract
1. Introduction
2. Results
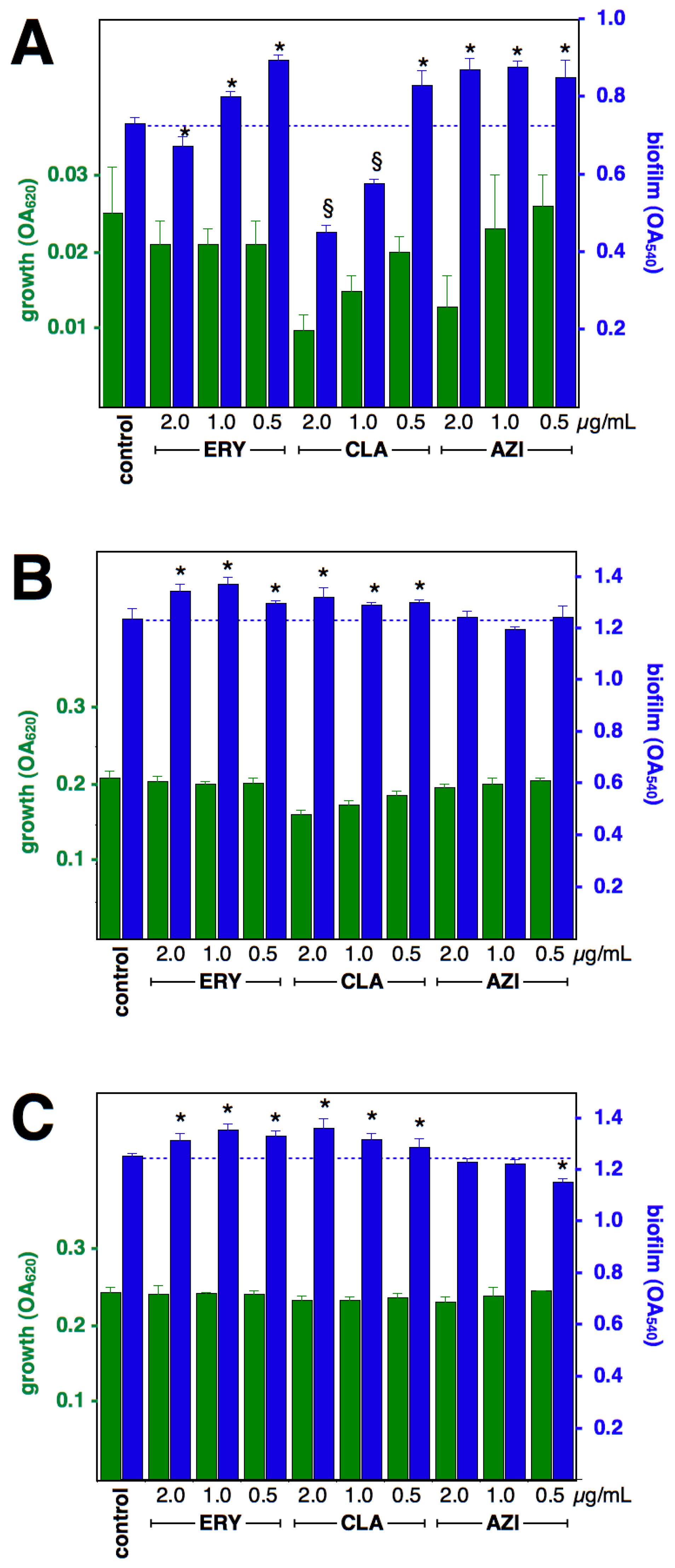
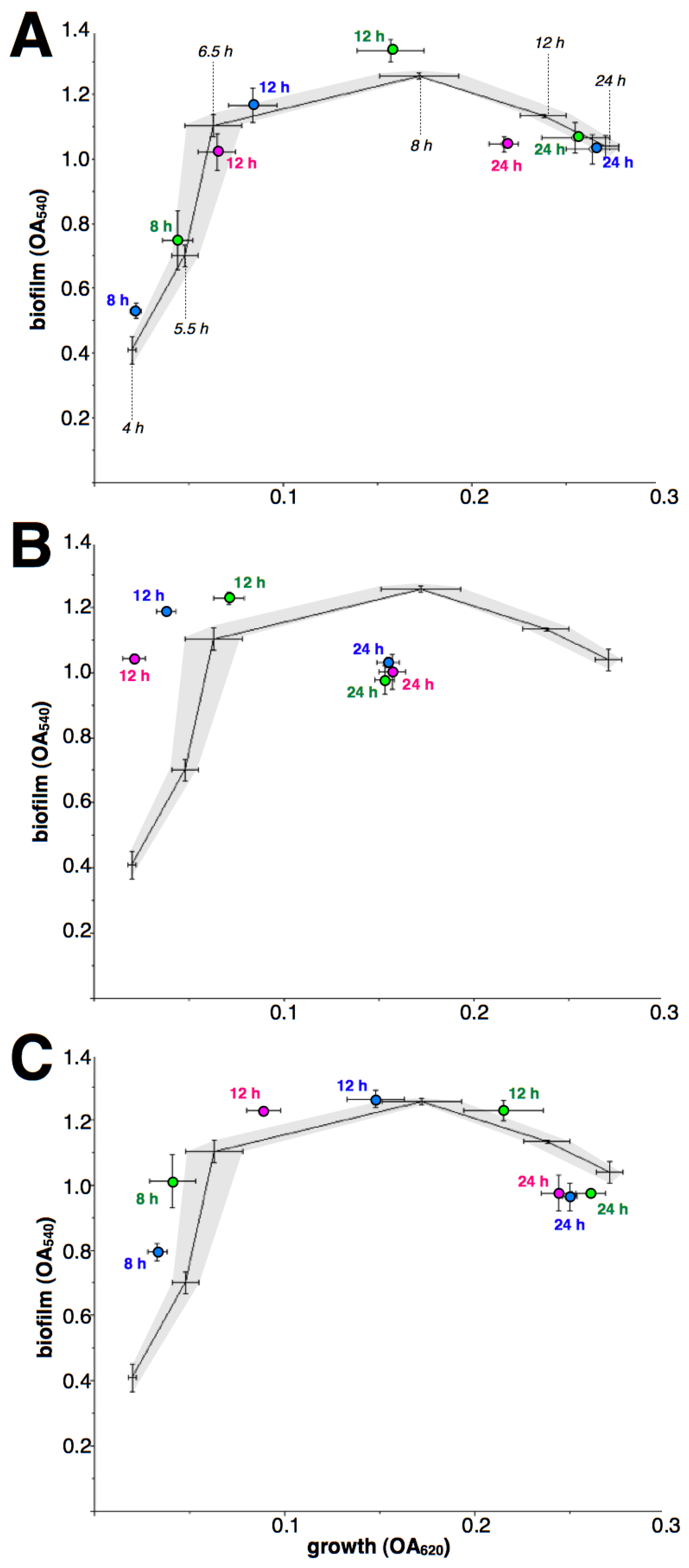
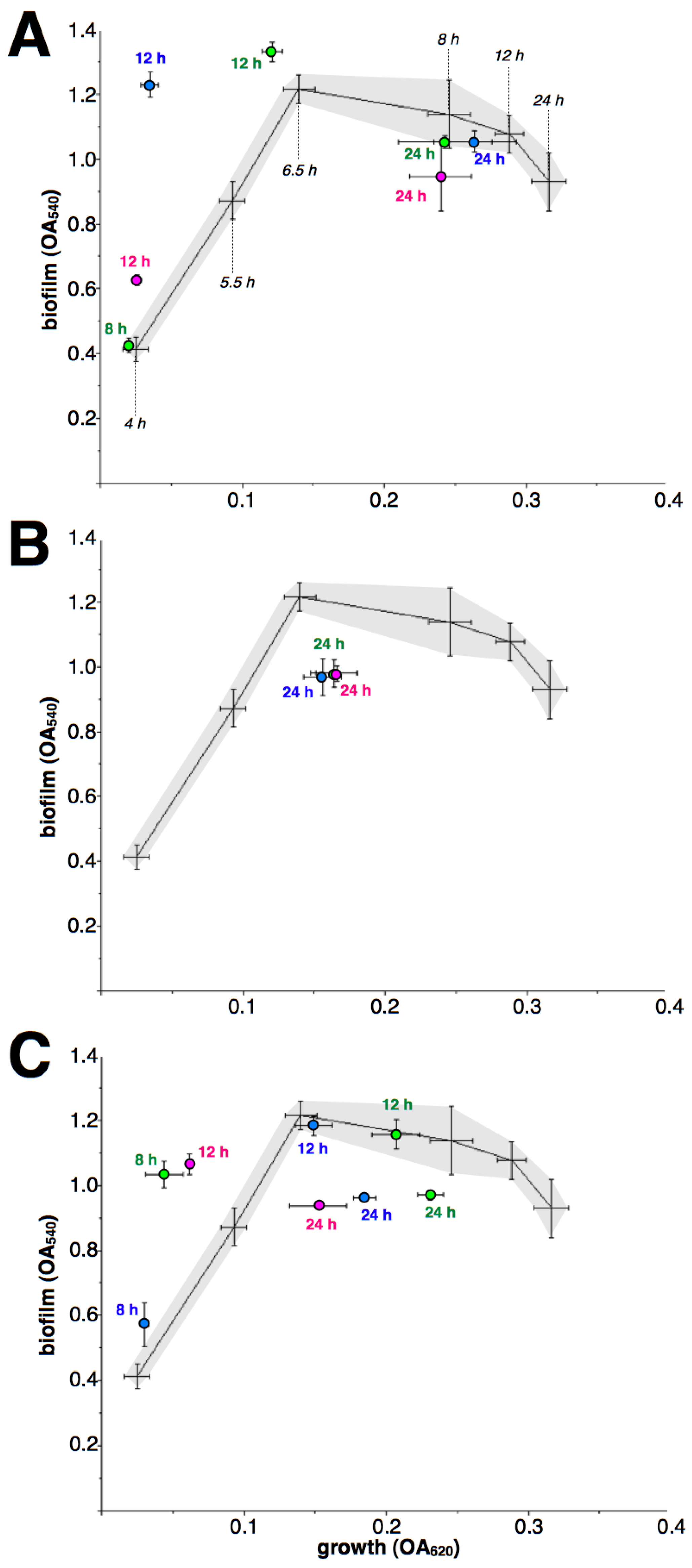
2.1. Effect of Macrolides upon Biofilm Formation by cMLSB Strains
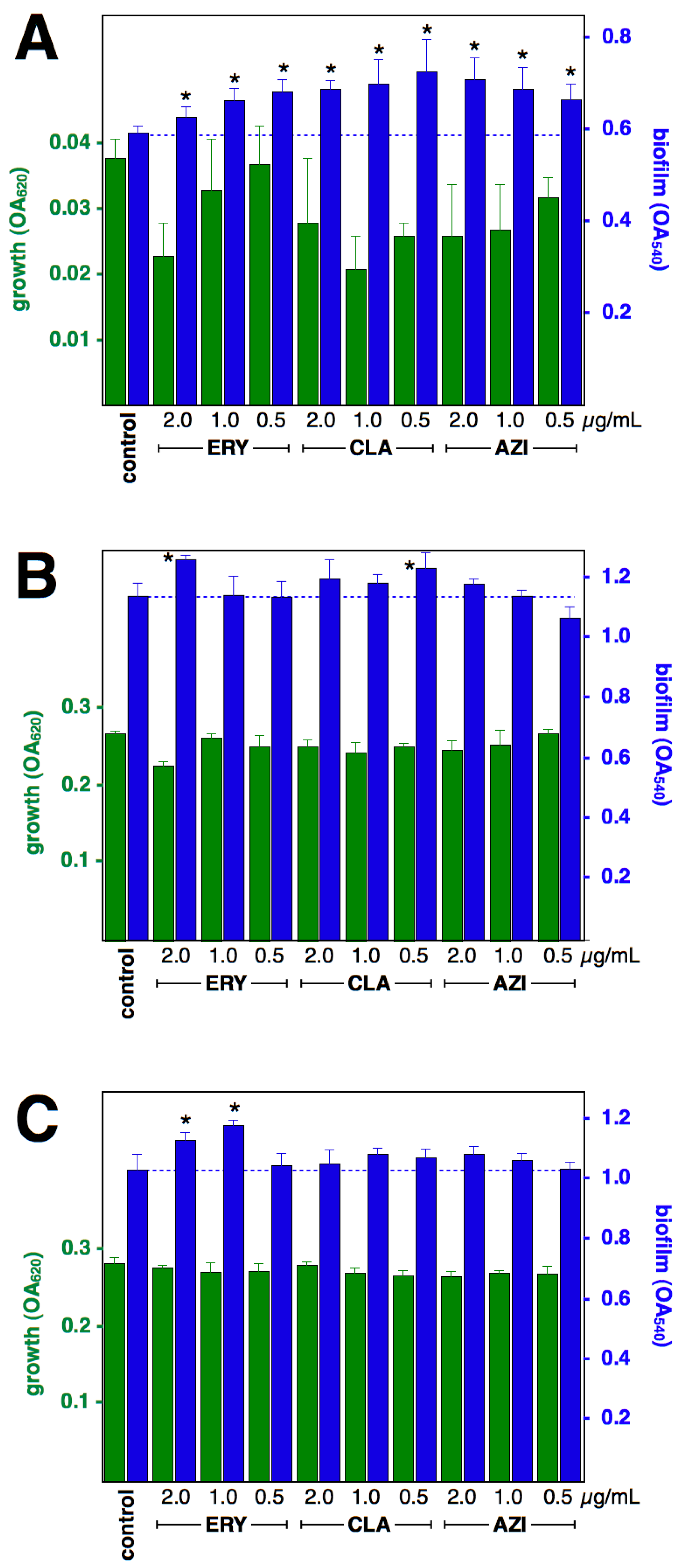
2.2. Effect of Macrolides upon Biofilm Formation by iMLSB Strains
2.3. Effect of Macrolides upon Biofilm Formation in Efflux-Mediated Resistant Strain
3. Discussion
4. Material and Methods
4.1. S. aureus Strains
4.2. Biofilm Assays
4.3. Statistical Analysis
Funding
Conflicts of Interest
References
- Schultz, M.J. Macrolide activities beyond their antimicrobial effects: Macrolides in diffuse panbronchiolitis and cystic fibrosis. J. Antimicrob. Chemother. 2004, 54, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Wozniak, D.J.; Keyser, R. Effects of subinhibitory concentrations of macrolide antibiotics on Pseudomonas aeruginosa. Chest 2004, 125, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Moshynets, O.V.; Baranovskyi, T.P.; Cameron, S.; Iungin, O.S.; Pokholenko, I.; Jerdan, R.; Kamyshnyi, A.; Krikunov, A.A.; Potochilova, V.V.; Rudnieva, K.L.; et al. Azithromycin possesses biofilm-inhibitory activity and potentiates non-bactericidal colistin methanesulfonate (CMS) and polymyxin B against Klebsiella pneumonia. PLoS ONE 2022, 17, e0270983. [Google Scholar] [CrossRef] [PubMed]
- Yamabe, K.; Arakawa, Y.; Shoji, M.; Onda, M.; Miyamoto, K.; Tsuchiya, T.; Akeda, Y.; Terada, K.; Tomono, K. Direct anti-biofilm effects of macrolides on Acinetobacter baumannii: Comprehensive and comparative demonstration by a simple assay using microtiter plate combined with peg-lid. Biomed. Res. 2020, 41, 259–268. [Google Scholar] [CrossRef]
- Favre-Bonté, S.; Köhler, T.; van Delden, C. Biofilm formation by Pseudomonas aeruginosa: Role of the C4-HSL cell-to-cell signal and inhibition by azithromycin. J. Antimicrob. Chemother. 2003, 52, 598–604. [Google Scholar] [CrossRef]
- Gordon, C.L. Azythromycin. In Kucers’ The Use of Antibiotics, 7th ed.; Grayson, M.L., Ed.; CRC Press: Boca Raton, FL, USA, 2018; pp. 1122–1149. [Google Scholar]
- van Bambeke, F. Erythromycin. In Kucers’ The Use of Antibiotics, 7th ed.; Grayson, M.L., Ed.; CRC Press: Boca Raton, FL, USA, 2018; pp. 1065–1086. [Google Scholar]
- van Ingen, J. Clarithromycin. In Kucers’ The Use of Antibiotics, 7th ed.; Grayson, M.L., Ed.; CRC Press: Boca Raton, FL, USA, 2018; pp. 1097–1121. [Google Scholar]
- Gillis, R.J.; Iglewski, B.H. Azithromycin retards Pseudomonas aeruginosa biofilm formation. J. Clin. Microbiol. 2004, 42, 5842–5845. [Google Scholar] [CrossRef] [PubMed]
- El Haj, C.; Murillo, O.; Ribera, A.; Garcia-Somoza, D.; Tubau, F.; Cabellos, C.; Cabo, J.; Ariza, J. The anti-biofilm effect of macrolides in a rat model of S. aureus foreign-body infection: Might it be of clinical relevance? Med. Microbiol. Immunol. 2017, 206, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Parra-Ruiz, J.; Vidaillac, C.; Rybak, M.J. Macrolides and staphylococcal biofilms. Rev. Esp. Quimioter. 2012, 25, 10–16. [Google Scholar] [PubMed]
- Wang, Q.; Sun, F.J.; Liu, Y.; Xiong, L.R.; Xie, L.L.; Xia, P.Y. Enhancement of biofilm formation by subinhibitory concentrations of macrolides in icaADBC-positive and -negative clinical isolates of Staphylococcus epidermidis. Antimicrob. Agents Chemother. 2010, 54, 2707–2711. [Google Scholar] [CrossRef] [PubMed]
- Di Bonaventura, G.; Pompilio, A.; Monaco, M.; Pimentel de Araujo, F.; Baldassarri, L.; Pantosti, A.; Gherardi, G. Adhesion and biofilm formation by Staphylococcus aureus clinical isolates under conditions relevant to the host: Relationship with macrolide resistance and clonal lineages. J. Med. Microbiol. 2019, 68, 148–160. [Google Scholar] [CrossRef] [PubMed]
- Gomes, D.L.R.; Peixoto, R.S.; Barbosa, E.A.B.; Napoleão, F.; Sabbadini, P.S.; dos Santos, K.R.N.; Mattos-Guaraldi, A.L.; Hirata, R. SubMICs of penicillin and erythromycin enhance biofilm formation and hydrophobicity of Corynebacterium diphtheriae strains. J. Med. Microbiol. 2013, 62, 754–760. [Google Scholar] [CrossRef] [PubMed]
- DiCicco, M.; Neethirajan, S.; Singh, A.; Weese, J.S. Efficacy of clarithromycin on biofilm formation of methicillin-resistant Staphylococcus pseudintermedius. BMC Vet. Res. 2012, 8, 225. [Google Scholar] [CrossRef] [PubMed]
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing, 30th ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2020. [Google Scholar]
- Delialioglu, N.; Aslan, G.; Ozturk, C.; Baki, V.; Sen, S.; Emekdas, G. Inducible clindamycin resistance in staphylococci isolated from clinical samples. Jpn. J. Infect. Dis. 2005, 58, 104–106. [Google Scholar] [PubMed]
- Novick, R.P.; Murphy, E.; Gryczan, T.J.; Baron, E.; Edelman, I. Penicillinase plasmids of Staphylococcus aureus: Restriction-deletion maps. Plasmid 1979, 2, 109–129. [Google Scholar] [CrossRef] [PubMed]
- O’Toole, G.A.; Pratt, L.A.; Watnick, P.I.; Newman, D.K.; Weaver, V.B.; Kolter, R. Genetic approaches to study of biofilms. Meth. Enzymol. 1999, 310, 91–109. [Google Scholar]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amábile-Cuevas, C.F. Macrolides at Clinically-Relevant Concentrations May Induce Biofilm Formation in Macrolide-Resistant Staphylococcus aureus. Antibiotics 2023, 12, 187. https://doi.org/10.3390/antibiotics12020187
Amábile-Cuevas CF. Macrolides at Clinically-Relevant Concentrations May Induce Biofilm Formation in Macrolide-Resistant Staphylococcus aureus. Antibiotics. 2023; 12(2):187. https://doi.org/10.3390/antibiotics12020187
Chicago/Turabian StyleAmábile-Cuevas, Carlos F. 2023. "Macrolides at Clinically-Relevant Concentrations May Induce Biofilm Formation in Macrolide-Resistant Staphylococcus aureus" Antibiotics 12, no. 2: 187. https://doi.org/10.3390/antibiotics12020187
APA StyleAmábile-Cuevas, C. F. (2023). Macrolides at Clinically-Relevant Concentrations May Induce Biofilm Formation in Macrolide-Resistant Staphylococcus aureus. Antibiotics, 12(2), 187. https://doi.org/10.3390/antibiotics12020187






