Antimicrobial Resistance Profiles of Staphylococcus Isolated from Cows with Subclinical Mastitis: Do Strains from the Environment and from Humans Contribute to the Dissemination of Resistance among Bacteria on Dairy Farms in Colombia?
Abstract
1. Introduction
2. Results
2.1. Data on Farms, Prevention, and Treatment of Bovine Mastitis
2.2. Microbiological Identification
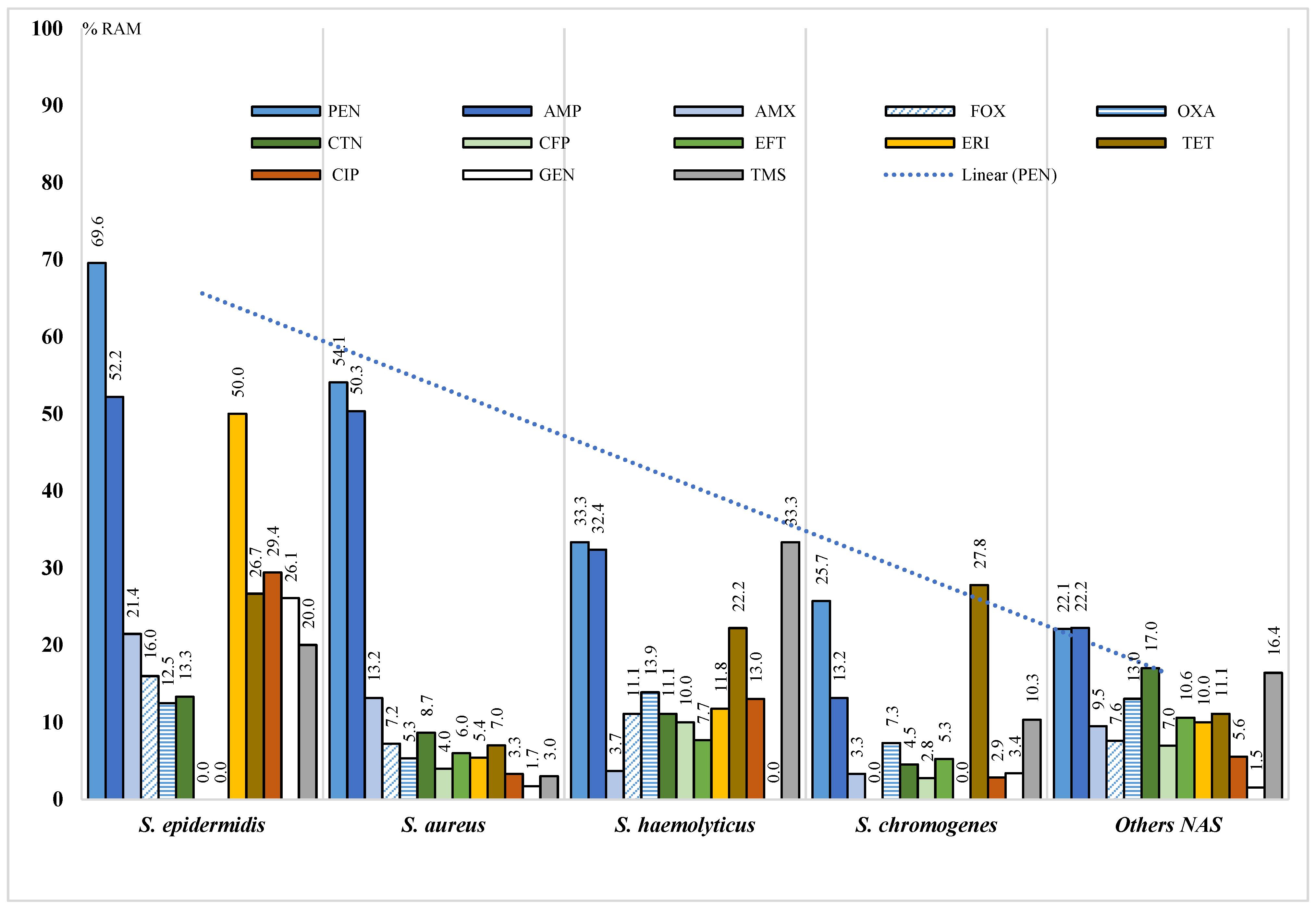
2.3. Antimicrobial Resistance Phenotype
2.4. S. aureus Antimicrobial Resistance Genotype
3. Discussion
4. Materials and Methods
4.1. Study Design and Bacterial Isolates
4.2. Antimicrobial Susceptibility Test
4.3. Identification of AMR Genes
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Balasubramanian, D.; Harper, L.; Shopsin, B.; Torres, V.J. Staphylococcus aureus Pathogenesis in Diverse Host Environments. Pathog. Dis. 2017, 75, ftx005. [Google Scholar] [CrossRef]
- Peton, V.; Le Loir, Y. Staphylococcus aureus in Veterinary Medicine. Infect. Genet. Evol. 2014, 21, 602–615. [Google Scholar] [CrossRef]
- Monistero, V.; Graber, H.U.; Pollera, C.; Cremonesi, P.; Castiglioni, B.; Bottini, E.; Ceballos-Marquez, A.; Lasso-Rojas, L.; Kroemker, V.; Wente, N.; et al. Staphylococcus aureus Isolates from Bovine Mastitis in Eight Countries: Genotypes, Detection of Genes Encoding Different Toxins and Other Virulence Genes. Toxins 2018, 10, 247. [Google Scholar] [CrossRef]
- Akkou, M.; Bouchiat, C.; Antri, K.; Bes, M.; Tristan, A.; Dauwalder, O.; Martins-Simoes, P.; Rasigade, J.P.; Etienne, J.; Vandenesch, F.; et al. New Host Shift from Human to Cows within Staphylococcus aureus Involved in Bovine Mastitis and Nasal Carriage of Animal’s Caretakers. Vet. Microbiol. 2018, 223, 173–180. [Google Scholar] [CrossRef]
- Elemo, K.K.; Bedada, B.A.; Kebeda, T. Prevalence, Risk Factors and Major Bacterial Causes of Bovine Mastitis in Smallholder Dairy Farms in and around Sinana District, Bale Zone, South Eastern Ethiopia. Glob. J. Sci. Front. Res. D Agric. Vet. 2018, 18, 1–14. [Google Scholar]
- Romero, J.; Benavides, E.; Meza, C. Assessing Financial Impacts of Subclinical Mastitis on Colombian Dairy Farms. Front. Vet. Sci. 2018, 5, 273. [Google Scholar] [CrossRef]
- Hoque, M.N.; Das, Z.C.; Rahman, A.N.M.A.; Haider, M.G.; Islam, M.A. Molecular Characterization of Staphylococcus aureus Strains in Bovine Mastitis Milk in Bangladesh. Int. J. Vet. Sci. Med. 2018, 6, 53–60. [Google Scholar] [CrossRef]
- He, Z.; Ren, L.; Yang, J.; Guo, L.; Feng, L.; Ma, C.; Wang, X.; Leng, Z.; Tong, X.; Zhou, W.; et al. Seroprevalence and Humoral Immune Durability of Anti-SARS-CoV-2 Antibodies in Wuhan, China: A Longitudinal, Population-Level, Cross-Sectional Study. Lancet 2021, 397, 1075–1084. [Google Scholar] [CrossRef]
- Raspanti, C.G.; Bonetto, C.C.; Vissio, C.; Pellegrino, M.S.; Reinoso, E.B.; Dieser, S.A.; Bogni, C.I.; Larriestra, A.J.; Odierno, L.M. Prevalence and Antibiotic Susceptibility of Coagulase-Negative Staphylococcus Species from Bovine Subclinical Mastitis in Dairy Herds in the Central Region of Argentina. Rev. Argent. Microbiol. 2016, 48, 50–56. [Google Scholar] [CrossRef]
- Condas, L.A.Z.; De Buck, J.; Nobrega, D.B.; Carson, D.A.; Naushad, S.; De Vliegher, S.; Zadoks, R.N.; Middleton, J.R.; Dufour, S.; Kastelic, J.P.; et al. Prevalence of Non-aureus Staphylococci Species Causing Intramammary Infections in Canadian Dairy Herds. J. Dairy Sci. 2017, 100, 5592–5612. [Google Scholar] [CrossRef]
- Rossi, B.F.; Bonsaglia, E.C.R.; Castilho, I.G.; Dantas, S.T.A.; Salina, A.; Langoni, H.; Pantoja, J.C.F.; Budri, P.E.; Fitzgerald-Hughes, D.; Júnior, A.F.; et al. Genotyping of Long Term Persistent Staphylococcus aureus in Bovine Subclinical Mastitis. Microb. Pathog. 2019, 132, 45–50. [Google Scholar] [CrossRef]
- Phophi, L.; Petzer, I.M.; Qekwana, D.N. Antimicrobial Resistance Patterns and Biofilm Formation of Coagulase-Negative Staphylococcus Species Isolated from Subclinical Mastitis Cow Milk Samples Submitted to the Onderstepoort Milk Laboratory. BMC Vet. Res. 2019, 15, 420. [Google Scholar] [CrossRef] [PubMed]
- De Buck, J.; Ha, V.; Naushad, S.; Nobrega, D.B.; Luby, C.; Middleton, J.R.; De Vliegher, S.; Barkema, H.W. Non-Aureus Staphylococci and Bovine Udder Health: Current Understanding and Knowledge Gaps. Front. Vet. Sci. 2021, 8, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Ruegg, P.L. Making Antibiotic Treatment Decisions for Clinical Mastitis. Vet. Clin. N. Am.-Food Anim. Pract. 2018, 34, 413–425. [Google Scholar] [CrossRef]
- Royster, E.; Wagner, S. Treatment of Mastitis in Cattle. Vet. Clin. N. Am.-Food Anim. Pract. 2015, 31, 17–46. [Google Scholar] [CrossRef]
- Oliver, S.P.; Murinda, S.E. Antimicrobial Resistance of Mastitis Pathogens. Vet. Clin. N. Am.-Food Anim. Pract. 2012, 28, 165–185. [Google Scholar] [CrossRef]
- Olsen, J.E.; Christensen, H.; Aarestrup, F.M. Diversity and Evolution of BlaZ from Staphylococcus aureus and Coagulase-Negative Staphylococci. J. Antimicrob. Chemother. 2006, 57, 450–460. [Google Scholar] [CrossRef]
- Monistero, V.; Barberio, A.; Biscarini, F.; Cremonesi, P.; Castiglioni, B.; Graber, H.U.; Bottini, E.; Ceballos-Marquez, A.; Kroemker, V.; Petzer, I.M.; et al. Different Distribution of Antimicrobial Resistance Genes and Virulence Profiles of Staphylococcus aureus Strains Isolated from Clinical Mastitis in Six Countries. J. Dairy Sci. 2020, 103, 3431–3446. [Google Scholar] [CrossRef] [PubMed]
- Fisarová, L.; Pantucek, R.; Botka, T.; Doskar, J. Variability of Resistance Plasmids in Coagulase-Negative Staphylococci and Their Importance as a Reservoir of Antimicrobial Resistance. Res. Microbiol. 2019, 170, 105–111. [Google Scholar] [CrossRef]
- Malachowa, N.; Deleo, F.R. Mobile Genetic Elements of Staphylococcus aureus. Cell. Mol. Life Sci. 2010, 67, 3057–3071. [Google Scholar] [CrossRef]
- Hanssen, A.M.; Ericson Sollid, J.U. SCCmec in Staphylococci: Genes on the Move. FEMS Immunol. Med. Microbiol. 2006, 46, 8–20. [Google Scholar] [CrossRef]
- Schnitt, A.; Tenhagen, B.A. Risk Factors for the Occurrence of Methicillin-Resistant Staphylococcus aureus in Dairy Herds: An Update. Foodborne Pathog. Dis. 2020, 17, 585–596. [Google Scholar] [CrossRef]
- Busche, T.; Hillion, M.; Van Loi, V.; Berg, D.; Walther, B.; Semmler, T.; Strommenger, B.; Witte, W.; Cuny, C.; Mellmann, A.; et al. Comparative Secretome Analyses of Human and Zoonotic Staphylococcus aureus Isolates CC8, CC22, and CC398. Mol. Cell. Proteom. 2018, 17, 2412–2433. [Google Scholar] [CrossRef]
- Jiménez Velásquez, S.d.C.; Torres Higuera, L.D.; Parra Arango, J.L.; Rodríguez Bautista, J.L.; García Castro, F.E.; Patiño Burbano, R.E. Profile of Antimicrobial Resistance in Isolates of Staphylococcus spp. Obtained from Bovine Milk in Colombia. Rev. Argent. Microbiol. 2019, 52, 121–130. [Google Scholar] [CrossRef]
- Leijon, M.; Atkins, E.; Persson Waller, K.; Artursson, K. Longitudinal Study of Staphylococcus aureus Genotypes Isolated from Bovine Clinical Mastitis. J. Dairy Sci. 2021, 104, 11945–11954. [Google Scholar] [CrossRef] [PubMed]
- Rüegsegger, F.; Ruf, J.; Tschuor, A.; Sigrist, Y.; Rosskopf, M.; Hässig, M. Antimicrobial Susceptibility of Mastitis Pathogens of Dairy Cows in Switzerland. Schweiz. Arch. Tierheilkd. 2013, 156, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Tan, X.; Zhang, X.; Xia, X.; Sun, H. The Diversities of Staphylococcal Species, Virulence and Antibiotic Resistance Genes in the Subclinical Mastitis Milk from a Single Chinese Cow Herd. Microb. Pathog. 2015, 88, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Li, Y.; Bao, H.; Wei, R.; Zhou, Y.; Zhang, H.; Wang, R. Population Structure and Antimicrobial Profile of Staphylococcus aureus Strains Associated with Bovine Mastitis in China. Microb. Pathog. 2016, 97, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Karzis, J.; Petzer, I.M.; Donkin, E.F.; Naidoo, V.; Etter, E.M.C. Climatic and Regional Antibiotic Resistance Patterns of Staphylococcus aureus in South African Dairy Herds. Onderstepoort J. Vet. Res. 2019, 86, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Saidi, R.; Mimoune, N.; Baazizi, R.; Benaissa, M.H.; Khelef, D.; Kaidi, R. Antibiotic Susceptibility of Staphylococci Isolated from Bovine Mastitis in Algeria. J. Adv. Vet. Anim. Res. 2019, 6, 231–235. [Google Scholar] [CrossRef]
- López Meza, J.E.; Higuera Ramos, J.E.; Ochoa Zarzosa, A.; Chassin Noria, O.; Valdez Alarcón, J.J.; Bravo Patiño, A.; Baizabal Aguirre, V.M. Caracterización Molecular de Aislamientos de Staphylococcus spp. Asociados a Mastitis Bovina en Tarímbaro, Michoacán. Técnica Pecu. Méx. 2006, 44, 91–106. [Google Scholar]
- Aponte, C. Perfil de Resistencia in Vitro a Antimicrobianos de Cepas Causantes de Mastitisaisladas de Leche Cruda Bovina En Establecimientos de Pequeña y Mediana Producción. Mem. Inst. Investig. Cienc. Salud 2007, 5, 19–25. [Google Scholar]
- León-Galván, M.F.; Barboza-Corona, J.E.; Lechuga-Arana, A.A.; Valencia-Posadas, M.; Aguayo, D.D.; Cedillo-Pelaez, C.; Martínez-Ortega, E.A.; Gutierrez-Chavez, A.J. Molecular Detection and Sensitivity to Antibiotics and Bacteriocins of Pathogens Isolated from Bovine Mastitis in Family Dairy Herds of Central Mexico. Biomed. Res. Int. 2015, 2015, 615153. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Barrera, J.; Angarita-Merchan, M.; Benavides-Sanchez, D.; Prada-Quiroga, C. Etiological Agents of Bovine Mastitis in Municipalities with Important Milk Production in the Department of Boyaca. Rev. Investig. Salud. Univ. Boyacá 2015, 2, 162–176. [Google Scholar] [CrossRef][Green Version]
- Kovačević, Z.; Samardžija, M.; Horvat, O.; Tomanić, D.; Radinović, M.; Bijelić, K.; Vukomanović, A.G.; Kladar, N. Is There a Relationship between Antimicrobial Use and Antibiotic Resistance of the Most Common Mastitis Pathogens in Dairy Cows? Antibiotics 2023, 12, 3. [Google Scholar] [CrossRef]
- Kikuchi, M.; Okabe, T.; Shimizu, H.; Matsui, T.; Matsuda, F.; Haga, T.; Fujimoto, K.; Endo, Y.; Sugiura, K. Antimicrobial Use and Its Association with the Presence of Methicillin-Resistant Staphylococci (MRS) and Extended-Spectrum Beta-Lactamases (ESBL)-Producing Coliforms in Mastitic Milk on Dairy Farms in the Chiba Prefecture, Japan. Heliyon 2022, 8, e12381. [Google Scholar] [CrossRef]
- FAO. Impact of Mastitis in Smal Scale Dairy Production Systems; Animal Production and Health Working Paper. N. 13; FAO: Roma, Italy, 2014; ISBN 978-92-5-107821-1. [Google Scholar]
- OIE. Estrategia de La OIE Sobre La Resistencia a Los Agentes Antimicrobianos y Su Uso Prudente. 2016. Available online: https://www.woah.org/app/uploads/2021/03/es-oie-amrstrategy.pdf (accessed on 27 October 2023).
- Antók, F.I.; Mayrhofer, R.; Marbach, H.; Masengesho, J.C.; Keinprecht, H.; Nyirimbuga, V.; Fischer, O.; Lepuschitz, S.; Ruppitsch, W.; Ehling-Schulz, M.; et al. Characterization of Antibiotic and Biocide Resistance Genes and Virulence Factors of Staphylococcus Species Associated with Bovine Mastitis in Rwanda. Antibiotics 2020, 9, 1. [Google Scholar] [CrossRef]
- Ren, Q.; Liao, G.; Wu, Z.; Lv, J.; Chen, W. Prevalence and Characterization of Staphylococcus aureus Isolates from Subclinical Bovine Mastitis in Southern Xinjiang, China. J. Dairy Sci. 2020, 103, 3368–3380. [Google Scholar] [CrossRef]
- Zayda, M.G.; Masuda, Y.; Hammad, A.M.; Honjoh, K.I.; Elbagory, A.M.; Miyamoto, T. Molecular Characterisation of Methicillin-Resistant (MRSA) and Methicillin-Susceptible (MSSA) Staphylococcus aureus Isolated from Bovine Subclinical Mastitis and Egyptian Raw Milk Cheese. Int. Dairy J. 2020, 104, 104646. [Google Scholar] [CrossRef]
- Girmay, W.; Gugsa, G.; Taddele, H.; Tsegaye, Y.; Awol, N.; Ahmed, M.; Feleke, A. Isolation and Identification of Methicillin-Resistant Staphylococcus aureus (MRSA) from Milk in Shire Dairy Farms, Tigray, Ethiopia. Vet. Med. Int. 2020, 2020, 8833973. [Google Scholar] [CrossRef]
- Li, T.; Lu, H.; Wang, X.; Gao, Q.; Dai, Y.; Shang, J.; Li, M. Molecular Characteristics of Staphylococcus aureus Causing Bovine Mastitis between 2014 and 2015. Front. Cell. Infect. Microbiol. 2017, 7, 127. [Google Scholar] [CrossRef]
- Costa, G.M.; Paiva, L.V.; Figueiredo, H.C.P.; Figueira, A.R.; Pereira, U.P.; Silva, N. Population Diversity of Staphylococcus aureus Isolated from Bovine Mastitis in Brazilian Dairy Herds. Res. Vet. Sci. 2012, 93, 733–735. [Google Scholar] [CrossRef] [PubMed]
- Feßler, A.T.; Wang, Y.; Wu, C.; Schwarz, S. Mobile Macrolide Resistance Genes in Staphylococci. Plasmid 2018, 99, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Bell, B.G.; Schellevis, F.; Stobberingh, E.; Goossens, H.; Pringle, M. A Systematic Review and Meta-Analysis of the Effects of Antibiotic Consumption on Antibiotic Resistance. BMC Infect. Dis. 2014, 14, 13. [Google Scholar] [CrossRef]
- Visciano, P.; Pomilio, F.; Tofalo, R.; Sacchini, L.; Saletti, M.A.; Tieri, E.; Schirone, M.; Suzzi, G. Detection of Methicillin-Resistant Staphylococcus aureus in Dairy Cow Farms. Food Control 2014, 46, 532–538. [Google Scholar] [CrossRef]
- Gizaw, F.; Kekeba, T.; Teshome, F.; Kebede, M.; Abreham, T.; Hayishe, H.; Waktole, H.; Tufa, T.B.; Edao, B.M.; Ayana, D.; et al. Distribution and Antimicrobial Resistance Profile of Coagulase-Negative Staphylococci from Cattle, Equipment, and Personnel on Dairy Farm and Abattoir Settings. Heliyon 2020, 6, e03606. [Google Scholar] [CrossRef]
- Farias, D.; Monte, M.; Dias, W.; Júnior, L.; Abley, M. Antimicrobial Resistance and Genotypic Relatedness of Environmental Staphylococci in Semi-Extensive Dairy Farms. Vet. Anim. Sci. 2018, 6, 103–106. [Google Scholar] [CrossRef]
- Krukowski, H.; Bakuła, Z.; Iskra, M.; Olender, A.; Bis-Wencel, H.; Jagielski, T. The First Outbreak of Methicillin-Resistant Staphylococcus aureus in Dairy Cattle in Poland with Evidence of on-Farm and Intrahousehold Transmission. J. Dairy Sci. 2020, 103, 10577–10584. [Google Scholar] [CrossRef]
- Papadopoulos, P.; Papadopoulos, T.; Angelidis, A.S.; Boukouvala, E.; Zdragas, A.; Papa, A.; Hadjichristodoulou, C.; Sergelidis, D. Prevalence of Staphylococcus aureus and of Methicillin-Resistant S. aureus (MRSA) along the Production Chain of Dairy Products in North-Western Greece. Food Microbiol. 2018, 69, 43–50. [Google Scholar] [CrossRef]
- De Visscher, A.; Supré, K.; Haesebrouck, F.; Zadoks, R.N.; Piessens, V.; Van Coillie, E.; Piepers, S.; De Vliegher, S. Further Evidence for the Existence of Environmental and Host-Associated Species of Coagulase-Negative Staphylococci in Dairy Cattle. Vet. Microbiol. 2014, 172, 466–474. [Google Scholar] [CrossRef]
- Hamel, J.; Zhang, Y.; Wente, N.; Krömker, V. Non-S. aureus Staphylococci (NAS) in Milk Samples: Infection or Contamination? Vet. Microbiol. 2020, 242, 108594. [Google Scholar] [CrossRef]
- Schoenfelder, S.M.K.; Dong, Y.; Feßler, A.T.; Schwarz, S.; Schoen, C.; Köck, R.; Ziebuhr, W. Antibiotic Resistance Profiles of Coagulase-Negative Staphylococci in Livestock Environments. Vet. Microbiol. 2017, 200, 79–87. [Google Scholar] [CrossRef]
- Schoenfelder, S.M.K.; Lange, C.; Eckart, M.; Hennig, S.; Kozytska, S.; Ziebuhr, W. Success through Diversity-How Staphylococcus Epidermidis Establishes as a Nosocomial Pathogen. Int. J. Med. Microbiol. 2010, 300, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Argudín, M.A.; Vanderhaeghen, W.; Vandendriessche, S.; Vandecandelaere, I.; André, F.X.; Denis, O.; Coenye, T.; Butaye, P. Antimicrobial Resistance and Population Structure of Staphylococcus Epidermidis Recovered from Animals and Humans. Vet. Microbiol. 2015, 178, 105–113. [Google Scholar] [CrossRef]
- Wall, B.A.; Mateus, A.; Marshall, L.; Pfeiffer, D.U.; Lubroth, J.; Ormel, H.J.; Otto, P.; Patriarch, A. Drivers, Dynamics and Epidemiology of Antimicrobial Resistance in Animal Production; FAO: Rome, Italy, 2016; ISBN 9789251090718. [Google Scholar]
- Yang, F.; Zhang, S.; Shang, X.; Li, H.; Zhang, H.; Cui, D.; Wang, X.; Wang, L.; Yan, Z.; Sun, Y. Short Communication: Detection and Molecular Characterization of Methicillin-Resistant Staphylococcus aureus Isolated from Subclinical Bovine Mastitis Cases in China. J. Dairy Sci. 2020, 103, 840–845. [Google Scholar] [CrossRef] [PubMed]
- Aires-de-Sousa, M. Methicillin-Resistant Staphylococcus aureus among Animals: Current Overview. Clin. Microbiol. Infect. 2017, 23, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Morejón-García, M. Staphylococcus aureus Resistente a Meticilina. Un Problema Actual. Dermatol. PERU 2012, 22, 29–33. [Google Scholar]
- Miller, D.D.; Kearns, J.V. Effectiveness of the California Mastitis Test as a Measurement of the Leucocyte Content of Quarter Samples of Milk. J. Dairy Sci. 1967, 50, 683–686. [Google Scholar] [CrossRef]
- Ceballos-Garzón, A.; Cortes, G.; Morio, F.; Zamora-Cruz, E.L.; Linares, M.Y.; Ariza, B.E.; Valderrama, S.L.; Garzón, J.R.; Alvarez-Moreno, C.A.; Le Pape, P.; et al. Comparison between MALDI-TOF MS and MicroScan in the Identification of Emerging and Multidrug Resistant Yeasts in a Fourth-Level Hospital in Bogotá, Colombia. BMC Microbiol. 2019, 19, 106. [Google Scholar] [CrossRef]
- Document M100–S10; CLSI National Committee for Clinical Laboratory Standards, Performance Standard for Antimicrobial Susceptibility Testing, 27th ed. Clinical and Laboratory Standars Institute: Wayne, PA, USA, 2017; ISBN 1-56238-804-5.
- CLSI. Performance Standards for Antimicrobial Disk and Dilution Susceptibility Tests for Bacteria Isolated From Animals, VET01, 5th ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018; ISBN 9781684400096. [Google Scholar]
- Geha, D.J.; Uhl, J.R.; Gustaferro, C.A.; Persing, D.H. Multiplex PCR for Identification of Methicillin-Resistant Staphylococci in the Clinical Laboratory. J. Clin. Microbiol. 1994, 32, 1768–1772. [Google Scholar] [CrossRef]
- Duran, N.; Ozer, B.; Duran, G.; Onlen, Y.; Demir, C. Antibiotic Resistance Genes & Susceptibility Patterns in Staphylococci. Indian J. Med. Res. 2012, 135, 389. [Google Scholar] [PubMed]
| Tier (n Cows) | Farm | S. aureus n | NAS n | Total Isolates n | Treatment Bovine Mastitis | Treatment Dry Cow | Prescription of Antibiotics | Withdrawal Periods of Antibiotics | MPCP * | Lab ** |
|---|---|---|---|---|---|---|---|---|---|---|
| Small: 10–35 | P1 | 5 | 5 | 10 | EFT | SP, N | NC | NC | NC | NC |
| P2 | 8 | 20 | 28 | TY, OT, TET | Not used | NC | C | NC | NC | |
| P3 | 0 | 8 | 8 | Not used | Not used | C | C | C | NC | |
| P4 | 1 | 27 | 28 | OB, AMP | OB, AMP | NC | NC | NC | C | |
| Medium: 36–100 | M1 | 2 | 6 | 8 | CEF | LN, N | C | C | C | NC |
| M2 | 14 | 27 | 41 | EFT, SP, N | SP, N | NC | C | NC | NC | |
| M3 | 0 | 5 | 5 | PEN | OB, AMP | C | C | C | NC | |
| M4 | 6 | 11 | 17 | PEN, CT, OT | OB, AMP | C | C | C | NC | |
| M5 | 6 | 25 | 31 | CEF | SP, N, OB, AMP | C | C | NC | NC | |
| Large: >100 | G1 | 10 | 14 | 24 | AMX | OB, AMP | NC | C | NC | NC |
| G2 | 24 | 37 | 61 | AMX, TY, OT | OB, AMP | C | C | C | NC | |
| G3 | 8 | 29 | 37 | OB, AMP, CEF | OB, AMP | NC | C | C | C | |
| G4 | 33 | 18 | 51 | OB, AMP, CFL, OT | OB, AMP | NC | C | NC | C |
| Species (n) | S. aureus (152) | NAS (n = 197) | Total (349) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Antibiotics (%) | R | I | S | R | I | S | R | I | S |
| Cefoxitin | 7.2 | 0 | 92.8 | 7.7 | 0 | 92.3 | 7.5 | 0 | 92.5 |
| Oxacillin | 5.3 | 0 | 94.7 | 11.4 | 0.5 | 88.1 | 8.7 | 0.3 | 91.0 |
| Penicillin | 54.1 | 0 | 45.9 | 32.4 | 0.0 | 67.6 | 42.0 | 0 | 58.0 |
| Ampicillin | 50.3 | 0 | 49.7 | 27.0 | 0.0 | 73.0 | 37.2 | 0 | 62.8 |
| Amoxycillin | 13.2 | 0 | 86.8 | 8.9 | 0.0 | 91.1 | 10.7 | 0 | 89.3 |
| Cefoperazone | 2.0 | 2.0 | 95.9 | 2.3 | 3.4 | 94.3 | 2.2 | 2.8 | 95.1 |
| Cephalothin | 8.7 | 0.0 | 91.3 | 10.5 | 2.9 | 86.7 | 9.5 | 1.3 | 89.2 |
| Ceftiofur | 3.4 | 2.6 | 94.0 | 6.6 | 1.6 | 91.8 | 5.0 | 2.1 | 92.9 |
| Erythromycin | 3.4 | 2.0 | 94.6 | 9.0 | 4.3 | 86.7 | 6.5 | 3.3 | 90.2 |
| Tetracycline | 3.5 | 3.5 | 92.9 | 8.8 | 5.4 | 85.8 | 6.5 | 4.6 | 88.9 |
| Ciprofloxacin | 2.5 | 0.8 | 96.7 | 4.6 | 4.6 | 90.8 | 3.6 | 2.8 | 93.6 |
| Gentamicin | 1.7 | 0.0 | 98.3 | 4.2 | 2.8 | 93.0 | 3.1 | 1.5 | 95.4 |
| Trimethoprim/sulfamethoxazole | 2.0 | 1.0 | 97.1 | 16.1 | 3.5 | 80.4 | 10.2 | 2.4 | 87.3 |
| Resistant to at least one antibiotic (%) | 96/152 (63.2%) | 110/197 (55.8%) | 206/349 (59.0%) | ||||||
| Multidrug resistance rate (%) | 7/152 (4.6%) | 23/197 (11.7%) | 30/349 (8.6%) | ||||||
| Species | Sources | *RI n (%) | FOX | OXA | PEN | AMP | AMX | CFP | CTN | EFT | ERI | TET | CIP | GEN | TMS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S. aureus | Workers | 9/10 (90.0) | 40.0 | 10.0 | 77.8 | 66.7 | 50.0 | 20.0 | 0.0 | 0.0 | 20.0 | 66.3 | 0.0 | 16.7 | 10.0 |
| Environmental | 7/7 (100) | 0.0 | 14.3 | 66.7 | 100.0 | 40.0 | 0.0 | 33.3 | 0.0 | 28.6 | 0.0 | 0.0 | 0.0 | -- | |
| QMS | 69/117 (59.0) | 5.1 | 4.3 | 53.4 | 46.8 | 9.8 | 1.8 | 13.4 | 5.6 | 3.6 | 2.5 | 3.2 | 1.1 | 1.4 | |
| Teats | 11/18 (61.1) | 5.6 | 5.6 | 41.2 | 41.2 | 0.0 | 10.5 | 0.0 | 14.3 | 0.0 | -- | 0.0 | 0.0 | 5.9 | |
| NAS | Workers | 10/15 (61.1) | 14.3 | 7.1 | 27.3 | 30.8 | 42.9 | 0.0 | 16.7 | 0.0 | 28.6 | 33.3 | 0.0 | 0.0 | 36.4 |
| Environmental | 19/25 (76.0) | 15.4 | 23.1 | 34.8 | 36.0 | 23.1 | 4.2 | 22.2 | 16.7 | 23.1 | 25.0 | 12.5 | 13.0 | 21.1 | |
| QMS | 31/59 (52.5) | 7.0 | 8.8 | 36.2 | 25.0 | 6.1 | 6.3 | 11.1 | 8,.1 | 11.3 | 6.9 | 11.4 | 7.9 | 14.3 | |
| Teats | 50/98 (51.0) | 5.1 | 11.5 | 30.3 | 25.6 | 2.1 | 6.5 | 11.1 | 7.6 | 9.5 | 8.5 | 8.8 | 4.3 | 19.7 | |
| Staphylococcus spp. | Workers | 19/25 (76.0) | 24.0 | 8.0 | 52.4 | 50.0 | 41.7 | 8.7 | 16.7 | 0.0 | 28.0 | 26.3 | 0.0 | 5.6 | 23.8 |
| Environmental | 26/32 (81.3) | 12.9 | 21.9 | 39.3 | 46.9 | 29.4 | 3.3 | 21.7 | 12.5 | 21.9 | 20.0 | 9.5 | 14.3 | 17.4 | |
| QMS | 100/176 (56.8) | 5.7 | 5.8 | 48.0 | 39.5 | 8.5 | 3.1 | 9.4 | 6.3 | 6.0 | 5.5 | 6.4 | 3.1 | 6.2 | |
| Teats | 61/116 (52.6) | 5.2 | 10.5 | 32.1 | 28.0 | 1.9 | 7.3 | 8.6 | 8.8 | 8.0 | 13.5 | 7.2 | 3.5 | 17.0 |
| Sample Source | Farm | Species | Resistance Profile |
|---|---|---|---|
| QMS | P2 | S. haemolyticus | FOX, OXA, PEN, AMP, CFP, CTN, EFT, ERI, TET, TMS |
| M1 | S. hyicus | FOX, OXA, PEN, AMP, CTN, EFT, ERI, TMS | |
| G2 | S. aureus | FOX, OXA, PEN, AMP, EFT, ERI | |
| P4 | S. aureus | FOX, OXA, CTN, CIP | |
| P1 | S. aureus | FOX, PEN. AMP, CIP | |
| G1 | S. aureus | OXA, PEN, AMP, AMX, CTN, ERI | |
| G4 | S. chromogenes | PEN, AMP, AMX, CFP, GEN | |
| G1 | S. aureus | CTN, TET, GEN | |
| P4 | S. epidermidis | PEN, ERI, CIP, GEN | |
| M4 | S. haemolyticus | PEN, CIP, TMS | |
| P4 | S. epidermidis | ERI, CIP, GEN | |
| Teats | P2 | S. haemolyticus | OXA, PEN, AMP, CFP, CTN, EFT, ERI, TET, CIP, TMS |
| P2 | S. equorum | OXA, PEN, AMP, CFP, CTN, EFT, ERI, TET, CIP, TMS | |
| G4 | S. xylosus | FOX, OXA, PEN, AMP, CFP, EFT, CIP | |
| P2 | S. aureus | FOX, OXA, PEN, AMP, CFP, TET | |
| P4 | S. epidermidis | FOX, PEN, AMP, ERI, CIP, GEN | |
| P4 | S. epidermidis | PEN, AMP, ERI, TET, CIP, GEN | |
| G4 | S. haemolyticus | OXA, AMP, CFP, TET | |
| P2 | S. lentus | OXA, PEN, AMP, CTN, TET | |
| M5 | S. arlettae | CFP, EFT, ERI, TET | |
| Workers | G3 | S. aureus | FOX, OXA, PEN, AMP, AMX, ERI |
| P4 | S. epidermidis | FOX, OXA, PEN, AMP, AMX, TET | |
| P4 | S. epidermidis | PEN, AMP, AMX, ERI, TET | |
| G2 | S. epidermidis | PEN, AMP, CTN, ERI | |
| G3 | S. epidermidis | AMP, ERI, TMS | |
| M5 | S. lentus | PEN, ERI, TMS | |
| Environment | P4 | S. warneri | FOX, OXA, PEN, AMP, CTN, TET, CIP |
| G1 | S. epidermidis | FOX, OXA, PEN, AMP, AMX, CTN, GEN | |
| P4 | S. epidermidis | FOX, PEN, AMP, ERI, TET, CIP, GEN | |
| P4 | S. epidermidis | OXA, PEN, ERI, GEN, TMS |
| AMR Genotypes and Phenotypes | n/Total | Percentage AMR (%) | AMR Genotype/Phenotype K ** (CI95%) (Observed Agreement %) |
|---|---|---|---|
| blaZ gene | 120/143 | 83.9 | 0.03 (−0.09, 0.16) (53.6) |
| K.B. penicillins * | 79/152 | 52.5 | |
| mecA gene | 17/140 | 12.1 | 0.16 (0.0, 0.3) (85.7) |
| K.B. FOX | 11/152 | 7.2 | |
| ermC gene | 34/145 | 23.5 | 0.07 (−0.04, 0.19) (75.4) |
| K.B. ERI | 8/148 | 5.4 | |
| tetK gene | 18/140 | 12.9 | 0.14 (−0.04, 0.32) (86.2) |
| K.B. TET | 8/113 | 7.1 | |
| aacA-aphD gene | 71/146 | 48.6 | −0.06 (−0.15, 0.03) (54.2%) |
| K.B. GEN | 2/118 | 1.7 |
| PCR/ Program | Genes | Primer Sequence | Amplicon Size (bp) | Reference |
|---|---|---|---|---|
| Simple 1 | mecA | 5′-GTAGAAATGACTGAACGTCCGATAA-3′ 5′-CCA ATT CCA CAT TGT TTC GGT CTAA-3′ | 310 | [65] |
| Multiplex 2 | blaZ | 5′-ACTTCAACACCTGCTGCTTTC-3′ 5′-TGACCACTTTTATCAGCAACC-3′ | 173 | [66] |
| tetK | 5′-GTAGCGACAATAGGTAATAGT-3′ 5′-GTAGTGACAATAAACCTCCTA-3′ | 360 | ||
| ermB | 5′-CTATCTGATTGTTGAAGAAGGATT-3′ 5′-GTTTACTCTTGGTTTAGGATGAAA-3′ | 142 | ||
| Simple 3 | aacA-aphD | 5′-GAAGTACGCAGAAGAGA-3′ 5′-ACATGGCAAGCTCTAGGA-3′ | 491 | [66] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez, M.F.; Gomez, A.P.; Ceballos-Garzon, A. Antimicrobial Resistance Profiles of Staphylococcus Isolated from Cows with Subclinical Mastitis: Do Strains from the Environment and from Humans Contribute to the Dissemination of Resistance among Bacteria on Dairy Farms in Colombia? Antibiotics 2023, 12, 1574. https://doi.org/10.3390/antibiotics12111574
Rodríguez MF, Gomez AP, Ceballos-Garzon A. Antimicrobial Resistance Profiles of Staphylococcus Isolated from Cows with Subclinical Mastitis: Do Strains from the Environment and from Humans Contribute to the Dissemination of Resistance among Bacteria on Dairy Farms in Colombia? Antibiotics. 2023; 12(11):1574. https://doi.org/10.3390/antibiotics12111574
Chicago/Turabian StyleRodríguez, Martha Fabiola, Arlen Patricia Gomez, and Andres Ceballos-Garzon. 2023. "Antimicrobial Resistance Profiles of Staphylococcus Isolated from Cows with Subclinical Mastitis: Do Strains from the Environment and from Humans Contribute to the Dissemination of Resistance among Bacteria on Dairy Farms in Colombia?" Antibiotics 12, no. 11: 1574. https://doi.org/10.3390/antibiotics12111574
APA StyleRodríguez, M. F., Gomez, A. P., & Ceballos-Garzon, A. (2023). Antimicrobial Resistance Profiles of Staphylococcus Isolated from Cows with Subclinical Mastitis: Do Strains from the Environment and from Humans Contribute to the Dissemination of Resistance among Bacteria on Dairy Farms in Colombia? Antibiotics, 12(11), 1574. https://doi.org/10.3390/antibiotics12111574









