Abstract
Appropriate postoperative antibiotic treatment in patients with infective endocarditis (IE) reduces the risks of recurrence and mortality. However, concerns about adverse drug reactions arise due to prolonged antibiotic usage. Therefore, we compared the recurrence and mortality rates according to the duration of postoperative antibiotic therapy in patients with IE. From 2005 to 2017, we retrospectively reviewed 416 patients with IE treated at a tertiary hospital in South Korea; among these, 216 patients who underwent heart valve surgery and received appropriate antibiotics were enrolled. The patients were divided into two groups based on the duration of usage of postoperative antibiotic therapy; the duration of postoperative antibiotic therapy was more than two weeks in 156 patients (72.2%) and two weeks or less in 60 patients (27.8%). The primary endpoint was IE relapse. The secondary endpoints were 1-year IE recurrence, 1-year mortality, and postoperative complication rates. The median age was 53 (interquartile range: 38–62) years. The relapse rate of IE was 0.9% (2/216). There was no statistical difference in relapse (0.0% vs. 1.3%, p = 0.379), 1-year recurrence (1.7% vs. 1.3%, p = 0.829), or 1-year mortality (10.0% vs. 5.8%, p = 0.274) between patients with postoperative antibiotic administration of two weeks or less versus more than two weeks. The duration of postoperative antibiotic therapy did not affect the 1-year mortality rate (log-rank test, p = 0.393). In conclusion, there was no statistically significant difference in recurrence, mortality, or postoperative complications according to the duration of postoperative antibiotic therapy.
1. Introduction
Infective endocarditis (IE) remains a major medical problem because of its association with high morbidity and mortality; the incidence thereof has increased despite improvements in diagnostic and therapeutic strategies [1,2]. Although surgical intervention plays an important role in reducing mortality, antibiotic therapy is also well established as an important treatment modality for patients with IE [3,4]. Appropriate antibiotic treatment, such as correct dose, duration, and agent selection, can reduce the risk of embolism associated with metastatic infection and poor prognosis in patients with IE [5,6,7]. In addition, appropriate antibiotic treatment is an important factor associated with recurrence and overall mortality in patients with IE [3,8]. However, clinicians tend to prescribe prolonged intravenous antibiotic therapy to patients with IE, because large amounts of bacteria are buried deep in cardiac vegetation, hindering antibacterial access and host immune response [9,10].
Prolonged antibiotic treatment raises concerns about adverse drug reactions and Clostridioides difficile infection (CDI) [11,12,13]. Prolonged parenteral antibiotic treatment dramatically increases the incidence of adverse events such as neutropenia, rash, fever, and eosinophilia [12]. Antibiotics also increase the risk of CDI by disrupting the gut microbiome [13]. Furthermore, prolonged postoperative antibiotic treatment does not have a significant positive effect on recurrence or mortality [14,15]. Rather, short-course postoperative antimicrobial therapy did not result in a significant difference in mortality, relapse, or re-infection in several selected IE cases (even in patients at high risk of complications) [16]. However, unlike total antibiotic duration, no clear guidelines address the duration of postoperative antibiotic therapy, other than to state that a new antibiotic treatment cycle should commence if the valve culture is positive [3].
Therefore, we compared the differences in recurrence, mortality, and major clinical outcomes according to the duration of postoperative antibiotic therapy (≤ or >2 weeks) in patients with IE.
2. Results
2.1. Patients’ Characteristics
Among 416 patients with IE, 216 patients who underwent heart valve surgery and finished antibiotic therapy were enrolled (Figure 1). The duration of postoperative antibiotic therapy was more than two weeks in 72.2% of the patients (156/216) and two weeks or less in 27.8% (60/216) of the patients.
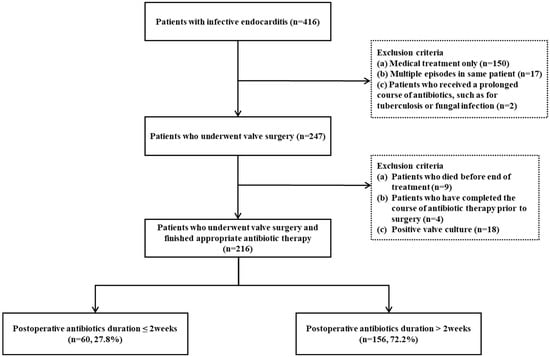
Figure 1.
Flow chart of study patients with infective endocarditis.
The median age of the patients was 53 (interquartile range [IQR], 38–62) years, and 67.1% of the patients were male (Table 1). Multiple-valve involvement was observed in 19.9% of IE patients. A previous history of IE was reported in eight patients (3.7%), and a prosthetic valve was reported in 25 patients (11.6%). The median Charlson Comorbidity Index was 1 (IQR, 0–3), and the median European System for Cardiac Operative Risk Evaluation (EuroSCORE) value was 2.04 (IQR, 1.53–2.83). Streptococcus species (42.1%), Staphylococcus species (14.4%), Enterococcus species (6.9%), and Haemophilus, Aggregatibacter, Cardiobacterium, Eikenella, and Kingella [HACEK] (0.5%) were isolated, whereas negative blood culture results were reported in 32.4% of the patients (70/216). Ampicillin/Sulbactam was used in 64 patients (29.6%), penicillin was used in 67 patients (31.0%), and vancomycin was used in 106 patients (49.1%). Two or more antibiotics were used together in 187 patients (86.6%).

Table 1.
Baseline characteristics of patients with infective endocarditis who underwent valve surgery.
There was no statistical difference in age, sex, nosocomial infection, previous IE history, previous history of valve, the affected valves, comorbidities, microorganisms, antibiotics usage, or vegetation size based on the two weeks of postoperative antibiotic therapy. However, the duration of overall antibiotic treatment was longer in those who received more than two weeks of postoperative therapy (28 days vs. 34 days, p < 0.001).
2.2. Outcomes According to the Duration of Postoperative Antibiotic Therapy
The median follow-up duration was 73 (IQR, 46–109) months. The IE relapse rate was 0.9% (2/216) (Table 2). There was no statistical difference in relapse (0.0% vs. 1.3%, p = 0.379), 1-year recurrence (1.7% vs. 1.3%, p = 0.829), 1-year reoperation (1.7% vs. 1.9%, p = 0.901), or 1-year mortality (10.0% vs. 5.8%, p = 0.274) according to postoperative antibiotics duration. The trend in 1-year mortality between groups was determined by the Kaplan–Meier curve and log-rank test (p = 0.393) (Figure 2).

Table 2.
Postoperative outcomes in patients with infective endocarditis who underwent valve surgery.
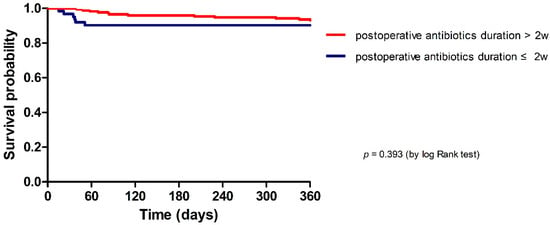
Figure 2.
Kaplan–Meier curves of 1-year mortality in patients with infective endocarditis according to the duration of postoperative antibiotic usage.
No statistically significant difference in postoperative complications was identified between the two postoperative antibiotics duration groups of more than two weeks and two weeks or less; the results are as follows: new-onset heart failure (HF) (16.7% vs. 8.3%, p = 0.075), new conduction abnormality (3.2% vs. 10.3%, p = 0.099), and new paravalvular complications (10.0% vs. 16.0%, p = 0.258) (Table 2).
2.3. Comparison of the Postoperative Antibiotic Therapy Duration According to the 1-Year Composite Outcome in Patients with Infective Endocarditis Who Underwent Valve Surgery
The median duration of postoperative antibiotic treatment was 21 (IQR: 14–28) days in IE patients who underwent valve surgery and lacked the 1-year composite outcome, but 20.5 (IQR: 5–34) days in IE patients with the 1-year composite outcome (p = 0.386). There was no statistically significant difference between the two groups (Figure 3). The variability of postoperative antibiotic duration is presented in Figure S1.
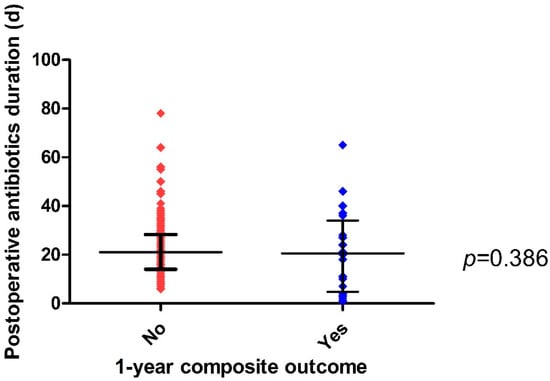
Figure 3.
Scatter plot of postoperative antibiotic treatment duration according to the 1-year composite outcome in patients with infective endocarditis who underwent valve surgery.
2.4. Univariable and Multivariable Logistic Regression Analysis of the 1-Year Composite Outcome in Patients with Infective Endocarditis
Upon univariable analysis, Staphylococcus species were related to an increase in the 1-year composite outcome (p = 0.026) (Table 3). Upon multivariable analysis, Staphylococcus species was also associated with an increasing 1-year composite outcome (odds ration [OR] 3.683, 95% confidence interval [CI] 1.341-10.114, p = 0.011). Postoperative antibiotics duration did not show a statistically significant association with the 1-year composite outcome.

Table 3.
Univariable and multivariable logistic regression analysis of the 1-year composite outcome in patients with infective endocarditis.
3. Discussion
In our study, the duration of postoperative antibiotic therapy did not show a statistically significant difference in relapse, 1-year recurrence, 1-year reoperation, 1-year mortality, or postoperative complications in IE patients who underwent valve surgery. The postoperative antibiotic duration was not statistically significant different according to the 1-year composite outcome in IE patients who underwent valve surgery.
Both surgical intervention and appropriate antibiotic therapy are important for patients with IE. In patients with IE who receive appropriate antibiotic treatment, the risk of embolic complication is reduced to less than half [5]. Embolism leads to ischemic stroke, mycotic aneurysms, and other metastatic infarctions, and is associated with IE recurrence and poor prognosis [3,6,7]. Inadequate antibiotic treatment due to the incorrect selection of dose, duration, or agent is a crucial factor associated with an increased rate of recurrence [3]. Thuny F. et al. reported that recurrence is an independent predictor of increased mortality in patients with IE [8]. Consequently, appropriate antibiotic treatment can reduce the risk of recurrence and mortality in patients with IE.
The total antibiotic duration is well specified for each species in the guidelines [3]. However, regarding the duration of postoperative antibiotics, it is recommended to start a new antibiotic treatment cycle when the valve culture is positive, but other opinions are not clear. Gisler et al. reported that the most prominent effect of preoperative antibiotic treatment on valve culture results was observed within the first few days, and did not significantly reduce the risk of positive valve culture beyond 21 days [17]. Morris et al. reported that prolonged postoperative antibiotic treatment (4–6 weeks) was not associated with the recurrence rate of IE, and two weeks seemed sufficient in the absence of metastatic infection [15]. Rao et al. also reported that a postoperative antibiotic course less than two weeks was not associated with recurrence and survival in patients with IE [14]. Thus, the need for prolonged postoperative antibiotics in IE patients who undergo valve surgery has been questioned. In our study, there was no significant difference in the types and duration of antibiotic treatment between the two groups of patients with more than and less than two weeks’ usage of postoperative antibiotic therapy, respectively. However, prolonged postoperative antibiotic treatment beyond two weeks did not show a significant effect on recurrence or mortality in patients with IE who underwent appropriate surgical intervention. A logistic regression analysis, after adjusting for various confounders, showed that prolonged postoperative antibiotic treatment did not show a significant effect on 1-year mortality. Furthermore, the duration of postoperative antibiotics did not affect the 1-year composite outcome in patients with infective endocarditis who underwent valve surgery.
There are concerns about prolonged use of antibiotics due to adverse drug reactions and CDI. Vancomycin has been associated with ototoxicity, nephrotoxicity, neutropenia, and thrombocytopenia, especially in adults who are receiving prolonged therapy [11]. Prolonged parenteral β-lactam therapy for more than two weeks in IE patients dramatically increases the incidence of delayed adverse events such as neutropenia, rash, fever, and eosinophilia [12]. Antibiotics also disrupt the normal gut microbiome and increase the risk of CDI [13]. Considering that an increase in adverse drug reactions and prolonged postoperative antibiotic treatment do not have significant effects on recurrence rate and mortality, an appropriate evaluation according to the duration of postoperative antibiotics therapy is necessary.
Inadequate antibiotic treatment, positive valve culture, prosthetic valve IE, persistent metastatic foci of infection, and empirical antimicrobial therapy for blood culture-negative IE are reported as factors that increase the rate of relapse [3,18]. In our study, we encountered a relapse in only two patients, one of whom had IE with multiple valve involvement and septic shock, and the other had a metastatic infection in a cardiac device. A shorter course of postoperative antibiotic therapy could be considered when employing a multidisciplinary approach, that is, when most vegetation is removed and neither a metastatic infection nor a positive valve culture is noted [3,14,15].
Staphylococcus species constitute an important causative pathogen in native and prosthetic valve endocarditis. Staphylococcus aureus is a common cause of acute and destructive IE and is an independent risk factor for relapse, in-hospital mortality, and 1-year mortality [19,20,21]. Coagulase negative staphylococci causes more protracted valve infections and increases the risk of in-hospital death and relapse in patients with IE [22,23,24]. In our study, the presence of Staphylococcus species was also a significant risk factor associated with the 1-year composite outcome in patients with infective endocarditis who underwent valve surgery.
Our study had certain limitations. First, due to the retrospective nature of the study, the baseline characteristics of the two groups classified by the postoperative antibiotic duration were not completely homogeneous. Second, as this was a single-center study, the sample size was small. Third, since cases that are inoperable or do not meet surgical indication were excluded, the severity or bacterial etiologies could be different. Fourth, patients with recurrent endocarditis who died before diagnosis, or cases where this was not followed up may be missed. However, most variables that could affect the outcomes did not have a statistically significant difference. In addition, a logistic regression analysis was performed to exclude the influence of confounders that could affect the clinical outcomes.
4. Materials and Methods
4.1. Patient Selection
From November 2005 to August 2017, we retrospectively reviewed 416 patients with IE at a single tertiary hospital in South Korea. The inclusion criteria were as follows: patients aged 18 years or older who were diagnosed with IE according to the modified Duke criteria, and who underwent heart valve surgery thereafter. Patients who did not require surgical treatment, who died before the end of treatment, who evidenced positive valve culture, or who completed the course of antibiotic therapy prior to surgery were excluded. Patients who received a prolonged course of antibiotics, such as for tuberculosis or a fungal infection, were also excluded. Only the first IE episode was counted in one patient, and subsequent events were described as recurrence.
This study was approved by the institutional review boards (IRBs) of Yonsei University College of Medicine (IRB no. 4-2018-0248). Due to the retrospective nature of the study, informed consent was waived. This study complied with the Good Clinical Practice guidelines and the Declaration of Helsinki.
4.2. Variables Definition
IE was defined according to the modified Duke criteria, and included both “definite IE” and “possible IE” [25]. Antibiotics were selected according to the European Society of Cardiology (ESC) guidelines and Infectious Diseases Society of America guidelines [3,26]. Appropriate antibiotic treatment was considered when at least one of the compounds was effective against the causative microorganism and when administered intravenously; specifically, if the identified strain was not susceptible to the empirically initiated antibiotics, the duration of antibiotic use was not counted until the date of change according to the susceptibility [17,27]. Decisions on surgical intervention were recommended by the multidisciplinary team, according to the guidelines [3,26]. A previous history of valves included prosthetic valves, previous valve surgery, cardiac devices, and other structural causes. Recurrence included both relapse and reinfection; “relapse” referred to repeated episodes of IE by the same microorganism, while “reinfection” referred to repeated episodes of IE by a different microorganism or later events [28]. Reoperation was defined as additional surgery on the same heart valve not only for the IE recurrence, but also for postoperative valve complications [14]. The 1-year composite outcome, including 1-year recurrence, 1-year reoperation, and 1-year mortality, was evaluated instead of evaluating each outcome individually, because there were few recurrence cases. The Charlson comorbidity index is a weighted index to estimate the risk of death from a comorbid disease at hospital admission [29]. The EuroSCORE was used for surgical risk stratification according to the patient’s demographic characteristics, cardiovascular and non-cardiovascular risk factors, and procedural variables [30]. The mortality data were obtained from the Ministry of the Interior and Safety of South Korea.
4.3. Primary and Secondary Endpoints
The primary endpoint was IE relapse. The secondary endpoints were 1-year IE recurrence, 1-year mortality, valve-related reoperation, and postoperative complications, such as new-onset HF, conduction abnormality, and paravalvular complications.
4.4. Statistical Analysis
Patients were divided into two groups according to the duration of postoperative antibiotic therapy: more than and less than two weeks. A comparison between the groups was analyzed using the Chi-square and Fisher’s exact test for categorical variables and the Mann–Whitney U test for continuous variables. A p-value of <0.05 was considered statistically significant. Kaplan–Meier (K-M) curves showed the probability of the survival of patients from the time of admission (due to IE) to either death, or the date of last known follow-up (18 September 2019) within one year. The log-rank test was used to explore any differences in the probability of death between the two groups. Scatter plots were used to display the distribution pattern of postoperative antibiotic duration according to the 1-year composite outcome. A logistic regression analysis was performed to further adjust for confounding factors and to analyze ORs and 95% CIs in terms of 1-year mortality. The variables for the multivariable analysis were selected based on clinically significant risk factors with p < 0.05 in the univariable analysis. The statistical analysis was performed using IBM SPSS Statistics for Windows, Version 26 software (IBM Corp. Armonk, NY, USA).
5. Conclusions
In conclusion, there was no statistically significant difference in the recurrence or mortality rates according to the duration of postoperative antibiotic therapy. If surgery and recommended antibiotic duration are properly performed, a shorter duration of postoperative antibiotics could be considered. Therefore, further larger prospective studies are warranted to assess the effect of postoperative antibiotic treatment duration on patients with IE.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/antibiotics12010173/s1: Figure S1: Scatter plot of the postoperative antibiotic therapy duration in patients with infective endocarditis who underwent valve surgery.
Author Contributions
Conceptualization, N.S.K. and S.H.L.; data curation, J.H.K., H.J.L. and S.J.L.; formal analysis, J.K., J.H.K. and N.S.K.; funding acquisition, N.S.K.; investigation, J.K. and J.H.K.; methodology, S.J.L., C.K., J.A.L., K.H.L., W.K.P., N.S.K. and S.H.L.; resources, J.H.K. and J.-S.Y.; supervision, N.S.K. and S.H.L.; validation, J.Y.A., S.J.J., J.Y.C. and J.-S.Y.; visualization, J.K.; writing—original draft, J.K. and J.H.K.; writing—review and editing, J.K., H.J.L., S.J.L., C.K., J.A.L., K.H.L., W.K.P., J.Y.A., S.J.J., N.S.K., S.H.L., J.Y.C. and J.-S.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2022R1C1C1010012).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the institutional review boards (IRBs) of Yonsei University College of Medicine (IRB no. 4-2018-0248).
Informed Consent Statement
The need for patient consent was waived due to the retrospective nature of the study.
Data Availability Statement
The data presented in this study are available upon reasonable request from the corresponding author.
Acknowledgments
This manuscript has not been published elsewhere in part or in entirety and is not under consideration by another journal. However, part of this manuscript was presented in a poster presentation in Washington, DC, USA at IDWeek 2022 (19–23 October 2022).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Habib, G.; Erba, P.A.; Iung, B.; Donal, E.; Cosyns, B.; Laroche, C.; Popescu, B.A.; Prendergast, B.; Tornos, P.; Sadeghpour, A.; et al. Clinical presentation, aetiology and outcome of infective endocarditis. Results of the ESC-EORP EURO-ENDO (European infective endocarditis) registry: A prospective cohort study. Eur. Heart J. 2019, 40, 3222–3232. [Google Scholar] [CrossRef] [PubMed]
- Talha, K.M.; Baddour, L.M.; Thornhill, M.H.; Arshad, V.; Tariq, W.; Tleyjeh, I.M.; Scott, C.G.; Hyun, M.C.; Bailey, K.R.; Anavekar, N.S.; et al. Escalating incidence of infective endocarditis in Europe in the 21st century. Open Heart 2021, 8, e001846. [Google Scholar] [CrossRef] [PubMed]
- Habib, G.; Lancellotti, P.; Antunes, M.J.; Bongiorni, M.G.; Casalta, J.P.; Del Zotti, F.; Dulgheru, R.; El Khoury, G.; Erba, P.A.; Iung, B.; et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Eur. Heart J. 2015, 36, 3075–3128. [Google Scholar] [CrossRef] [PubMed]
- Baddour, L.M.; Wilson, W.R.; Bayer, A.S.; Fowler, V.G., Jr.; Tleyjeh, I.M.; Rybak, M.J.; Barsic, B.; Lockhart, P.B.; Gewitz, M.H.; Levison, M.E.; et al. Infective endocarditis in adults: Diagnosis, antimicrobial therapy, and management of complications: A scientific statement for healthcare professionals from the American Heart Association. Circulation 2015, 132, 1435–1486. [Google Scholar] [CrossRef] [PubMed]
- Dickerman, S.A.; Abrutyn, E.; Barsic, B.; Bouza, E.; Cecchi, E.; Moreno, A.; Doco-Lecompte, T.; Eisen, D.P.; Fortes, C.Q.; Fowler, V.G.; et al. The relationship between the initiation of antimicrobial therapy and the incidence of stroke in infective endocarditis: An analysis from the ICE Prospective Cohort Study (ICE-PCS). Am. Heart J. 2007, 154, 1086–1094. [Google Scholar] [CrossRef]
- García-Cabrera, E.; Fernández-Hidalgo, N.; Almirante, B.; Ivanova-Georgieva, R.; Noureddine, M.; Plata, A.; Lomas, J.M.; Gálvez-Acebal, J.; Hidalgo-Tenorio, C.; Ruíz-Morales, J.; et al. Neurological complications of infective endocarditis: Risk factors, outcome, and impact of cardiac surgery: A multicenter observational study. Circulation 2013, 127, 2272–2284. [Google Scholar] [CrossRef]
- Iung, B.; Duval, X. Infective endocarditis: Innovations in the management of an old disease. Nat. Rev. Cardiol. 2019, 16, 623–635. [Google Scholar] [CrossRef]
- Thuny, F.; Giorgi, R.; Habachi, R.; Ansaldi, S.; Le Dolley, Y.; Casalta, J.-P.; Avierinos, J.-F.; Riberi, A.; Renard, S.; Collart, F.; et al. Excess mortality and morbidity in patients surviving infective endocarditis. Am. Heart J. 2012, 164, 94–101. [Google Scholar] [CrossRef]
- Spellberg, B.; Chambers, H.F.; Musher, D.M.; Walsh, T.L.; Bayer, A.S. Evaluation of a paradigm shift from intravenous antibiotics to oral step-down therapy for the treatment of infective endocarditis: A narrative review. JAMA Intern. Med. 2020, 180, 769–777. [Google Scholar] [CrossRef]
- Werdan, K.; Dietz, S.; Löffler, B.; Niemann, S.; Bushnaq, H.; Silber, R.-E.; Peters, G.; Müller-Werdan, U. Mechanisms of infective endocarditis: Pathogen-host interaction and risk states. Nat. Rev. Cardiol. 2014, 11, 35–50. [Google Scholar] [CrossRef]
- Levine, D.P. Vancomycin: A history. Clin. Infect Dis. 2006, 42 (Suppl. 1), S5–S12. [Google Scholar] [CrossRef]
- Olaison, L.; Belin, L.; Hogevik, H.; Alestig, K. Incidence of beta-lactam-induced delayed hypersensitivity and neutropenia during treatment of infective endocarditis. Arch. Intern. Med. 1999, 159, 607–615. [Google Scholar] [CrossRef]
- Rupnik, M.; Wilcox, M.H.; Gerding, D.N. Clostridium difficile infection: New developments in epidemiology and pathogenesis. Nat. Rev. Microbiol. 2009, 7, 526–536. [Google Scholar] [CrossRef]
- Rao, V.P.; Wu, J.; Gillott, R.; Baig, M.W.; Kaul, P.; Sandoe, J.A.T. Impact of the duration of antibiotic therapy on relapse and survival following surgery for active infective endocarditis. Eur. J. Cardiothorac. Surg. 2019, 55, 760–765. [Google Scholar] [CrossRef]
- Morris, A.J.; Drinković, D.; Pottumarthy, S.; MacCulloch, D.; Kerr, A.R.; West, T. Bacteriological outcome after valve surgery for active infective endocarditis: Implications for duration of treatment after surgery. Clin. Infect. Dis. 2005, 41, 187–194. [Google Scholar] [CrossRef]
- Muñoz, P.; Giannella, M.; Scoti, F.; Predomingo, M.; Puga, D.; Pinto, A.; Roda, J.; Marin, M.; Bouza, E. Two weeks of postsurgical therapy may be enough for high-risk cases of endocarditis caused by Streptococcus viridans or Streptococcus bovis. Clin. Microbiol. Infect. 2012, 18, 293–299. [Google Scholar] [CrossRef]
- Gisler, V.; Dürr, S.; Irincheeva, I.; Limacher, A.; Droz, S.; Carrel, T.; Englberger, L.; Sendi, P. Duration of pre-operative antibiotic treatment and culture results in patients with infective endocarditis. J. Am. Coll. Cardiol. 2020, 76, 31–40. [Google Scholar] [CrossRef]
- Heiro, M.; Helenius, H.; Mäkilä, S.; Hohenthal, U.; Savunen, T.; Engblom, E.; Nikoskelainen, J.; Kotilainen, P. Infective endocarditis in a Finnish teaching hospital: A study on 326 episodes treated during 1980–2004. Heart 2006, 92, 1457–1462. [Google Scholar] [CrossRef]
- Shah, A.S.; McAllister, D.A.; Gallacher, P.; Astengo, F.; Pérez, J.A.R.; Hall, J.; Lee, K.K.; Bing, R.; Anand, A.; Nathwani, D.; et al. Incidence, microbiology, and outcomes in patients hospitalized with infective endocarditis. Circulation 2020, 141, 2067–2077. [Google Scholar] [CrossRef]
- Freitas-Ferraz, A.B.; Tirado, G.; Vilacosta, I.; Olmos, C.; Sáez, C.; López, J.; Sarriá, C.; Pérez-García, C.N.; García-Arribas, D.; Ciudad, M.; et al. Contemporary epidemiology and outcomes in recurrent infective endocarditis. Heart 2020, 106, 596–602. [Google Scholar] [CrossRef]
- Manne, M.B.; Shrestha, N.; Lytle, B.W.; Nowicki, E.R.; Blackstone, E.; Gordon, S.M.; Pettersson, G.; Fraser, T.G. Outcomes after surgical treatment of native and prosthetic valve infective endocarditis. Ann. Thorac. Surg. 2012, 93, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Abramczuk, E.; Hryniewiecki, T.; Stepińska, J. Effects of pathogenic factors on prognosis in patients with prosthetic valve endocarditis. Kardiol. Pol. 2007, 65, 115–122. [Google Scholar] [PubMed]
- Tchana-Sato, V.; Hans, G.; Frippiat, F.; Zekhnini, I.; Dulgheru, R.; Lavigne, J.P.; Defraigne, J.O. Surgical management of Staphylococcus capitis prosthetic valve infective endocarditis: Retrospective review of a 10-year single center experience and review of the literature. J. Infect. Public Health 2020, 13, 1705–1709. [Google Scholar] [CrossRef] [PubMed]
- Chu, V.H.; Woods, C.W.; Miro, J.M.; Hoen, B.; Cabell, C.H.; Pappas, P.A.; Federspiel, J.; Athan, E.; Stryjewski, M.; Nacinovich, F.; et al. Emergence of coagulase-negative Staphylococci as a cause of native valve endocarditis. Clin. Infect. Dis. 2008, 46, 232–242. [Google Scholar] [CrossRef] [PubMed]
- Li, J.S.; Sexton, D.J.; Mick, N.; Nettles, R.; Fowler, V.G., Jr.; Ryan, T.; Bashore, T.; Corey, G.R. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin. Infect. Dis. 2000, 30, 633–638. [Google Scholar] [CrossRef]
- Baddour, L.M.; Wilson, W.R.; Bayer, A.S.; Fowler, V.G., Jr.; Bolger, A.F.; Levison, M.E.; Ferrieri, P.; Gerber, M.A.; Tani, L.Y.; Gewitz, M.H.; et al. Infective endocarditis: Diagnosis, antimicrobial therapy, and management of complications: A statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: Endorsed by the Infectious Diseases Society of America. Circulation 2005, 111, e394–e434. [Google Scholar]
- Kim, J.; Kim, J.H.; Lee, H.J.; Lee, S.J.; Lee, K.H.; Lee, E.H.; Baek, Y.J.; Ahn, J.Y.; Jeong, S.J.; Ku, N.S.; et al. Impact of valve culture positivity on prognosis in patients with infective endocarditis who underwent valve surgery. Infect. Dis. Ther. 2022, 11, 1253–1265. [Google Scholar] [CrossRef]
- Chu, V.H.; Sexton, D.J.; Cabell, C.H.; Barth, R.L.; Pappas, P.A.; Singh, R.; Fowler, V.G.; Ralph, C.G.; Aksoy, O.; Woods, C.W. Repeat infective endocarditis: Differentiating relapse from reinfection. Clin. Infect. Dis. 2005, 41, 406–409. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Nashef, S.A.; Roques, F.; Sharples, L.D.; Nilsson, J.; Smith, C.; Goldstone, A.R.; Lockowandt, U. EuroSCORE II. Eur. J. Cardiothorac. Surg. 2012, 41, 734–744. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).