Knowledge and Attitudes about Antibiotics and Antibiotic Resistance of 2404 UK Healthcare Workers
Abstract
:1. Introduction
- Assess the knowledge, attitudes and behaviour of UK HCWs (including prescribers) in regard to antibiotics and antibiotic use and resistance;
- Determine baseline data from a pre-COVID-19 pandemic landscape to allow for the future comparison of the impact of the pandemic on antimicrobial awareness and response and inform policy and interventions;
- Support the evaluation of UK communication campaigns (UK National Action Plan (NAP), Antibiotic Guardian and the Keep Antibiotics Working (KAW) campaign) and international awareness activities (World Antimicrobial Awareness Week (WAAW) and European Antibiotic Awareness Day (EAAD)) which have been targeting HCWs for over a decade.
2. Materials and Methods
3. Results
3.1. Demographics
3.2. Perceived Capability
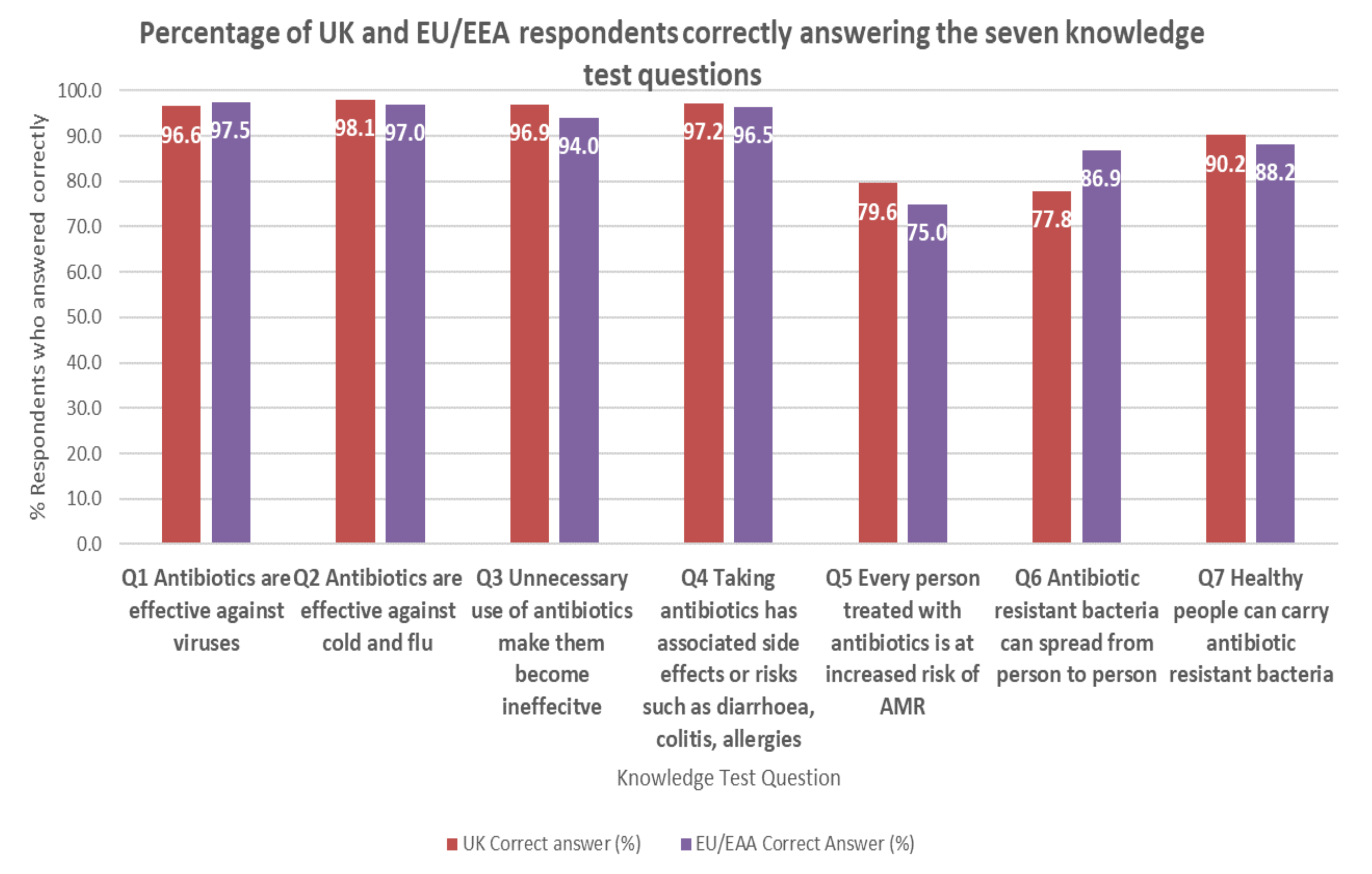
3.3. Actual Capability Assessed by Seven Knowledge Test Questions
3.4. Opportunities
3.5. Motivation/Attitude towards Antibiotic Resistance
3.6. Behaviour (Giving out Resources or Advice) and Barriers
3.7. Awareness of National Initiatives and Campaigns, and Perceived Effectiveness
3.8. Summary Recommendations for Action from Stakeholder Workshop
- Further analysis of the data should be undertaken to compare differences across professional groups and differences across settings.
- Sepsis messaging should be more strongly linked to antimicrobial resistance and focus on preventative measures.
- Facebook presents an opportunity to engage with UK healthcare workers. Campaigns, initiatives and interventions should be promoted on both Twitter and Facebook.
- Key organisations should be encouraged to produce a short video for WAAW outlining their AMR and AMS activities and available resources.
- All recommendations should align with the COM-B behaviour change wheel.
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Public Health England. English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR); 2020. Available online: https://www.gov.uk/government/publications/english-surveillance-programme-antimicrobial-utilisation-and-resistance-espaur-report (accessed on 21 June 2021).
- Global and Public Health Group. Tackling Antimicrobial Resistance 2019–2024; Emergency Preparedness and Health Protection Policy Directorate, Global and Public Health Group: London, UK, 2019. [Google Scholar]
- Global and Public Health Group. The UK’s 20-Year Vision for Antimicrobial Resistance; Emergency Preparedness and Health Protection Policy Directorate, Global and Public Health Group: London, UK, 2019. [Google Scholar]
- O’Neill, J. Tackling Drug-Resistant Infections Globally: Final Rpeort and Recommendations; Review on Antimicrobial Resistance: London, UK, 2016; Available online: https://amr-review.org/Publications.html (accessed on 21 June 2021).
- WHO. Global Action Plan on Antimicrobial Resistance; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- England, P.H. World Antimicrobial Awareness Week (WAAW) & European Antibiotic Awareness Day (EAAD): Resources Toolkit for Healthcare Professionals in England in the Context of the COVID-19 Pandemic. 2020. Available online: https://www.gov.uk/government/publications/european-antibiotic-awareness-day-resources-toolkit-for-healthcare-professionals-in-england (accessed on 1 April 2021).
- Redfern, J.; Bowater, L.; Coulthwaite, L.; Verran, J. Raising awareness of antimicrobial resistance among the general public in the UK: The role of public engagement activities. JAC-Antimicrob. Resist. 2020, 2, dlaa012. [Google Scholar] [CrossRef] [PubMed]
- Kosiyaporn, H.; Chanvatik, S.; Issaramalai, T.; Kaewkhankhaeng, W.; Kulthanmanusorn, A.; Saengruang, N.; Witthayapipopsakul, W.; Viriyathorn, S.; Kirivan, S.; Kunpeuk, W.; et al. Surveys of knowledge and awareness of antibiotic use and antimicrobial resistance in general population: A systematic review. PLoS ONE 2020, 15, e0227973. [Google Scholar] [CrossRef] [PubMed]
- McNulty, C.A.M.; Collin, S.M.; Cooper, E.; Lecky, D.M.; Butler, C.C. Public understanding and use of antibiotics in England: Findings from a household survey in 2017. BMJ Open 2019, 9, e030845. [Google Scholar] [CrossRef] [PubMed]
- Mason, T.; Trochez, C.; Thomas, R.; Babar, M.; Hesso, I.; Kayyali, R. Knowledge and awareness of the general public and perception of pharmacists about antibiotic resistance. BMC Public Health 2018, 18, 711. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, R.M.; Merrill, K.C.; Luthy, K.E.; Nuttall, C. Knowledge, attitudes, and perceptions of nurse practitioners about antibiotic stewardship. J. Am. Assoc. Nurse Pr. 2020, 33, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Ness, V.; Currie, K.; Reilly, J.; McAloney-Kocaman, K.; Price, L. Factors associated with independent nurse prescribers’ antibiotic prescribing practice: A mixed-methods study using the Reasoned Action Approach. J. Hosp. Infect. 2021, 113, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Teixeira Rodrigues, A.; Roque, F.; Falcão, A.; Figueiras, A.; Herdeiro, M.T. Understanding physician antibiotic prescribing behaviour: A systematic review of qualitative studies. Int. J. Antimicrob. Agents 2013, 41, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Ness, V.; Price, L.; Currie, K.; Reilly, J. Influences on independent nurse prescribers’ antimicrobial prescribing behaviour: A systematic review. J. Clin. Nurs. 2016, 25, 1206–1217. [Google Scholar] [CrossRef] [PubMed]
- Nuttall, D. Nurse prescribing in primary care: A metasynthesis of the literature. Prim. Health Care Res. Amp. Dev. 2018, 19, 7–22. [Google Scholar] [CrossRef] [PubMed]
- Ashiru-Oredope, D.; Hopkins, S.; Vasandani, S.; Umoh, E.; Oloyede, O.; Nilsson, A.; Kinsman, J.; Elsert, L.; Monnet, D.L. Healthcare workers’ knowledge, attitudes and behaviours with respect to antibiotics, antibiotic use and antibiotic resistance across 30 EU/EEA countries in 2019. Eurosurveillance 2021, 26, 1900633. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control & Public Health England. Survey of Healthcare Workers’ Knowledge, Attitudes and Behaviours on Antibiotics, Antibiotic Use and Antibiotic Resistance in the EU/EEA; European Centre for Disease Prevention and Control: Stockholm, Sweden, 2019. [Google Scholar]
- Michie, S.; Van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- Cane, J.; O’Connor, D.; Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 2012, 7, 37. [Google Scholar] [CrossRef] [PubMed]
- Eurostat. Healthcare Personnel Statistics. Available online: https://ec.europa.eu/eurostat/statisticsexplained/index.php/Healthcare_personnel_statistics_-_physicians#Healthcare_personnel (accessed on 2 August 2021).
- United Kingdom Health Security Agency. English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2020 to 2021; United Kingdom Health Security Agency: London, UK, 2021.
- Public Health England. Achieving Behaviour Change: A Guide for National Government. Available online: https://www.gov.uk/government/publications/behaviour-change-guide-for-local-government-and-partners (accessed on 27 July 2021).
- McEwen, S.A.; Collignon, P.J. Antimicrobial Resistance: A One Health Perspective. Microbiol. Spectr. 2018. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.F.; Hawking, M.K.D.; Owens, R.; Lecky, D.; Francis, N.A.; Butler, C.; Gal, M.; McNulty, C.A.M. An evaluation of the TARGET (Treat Antibiotics Responsibly; Guidance, Education, Tools) Antibiotics Toolkit to improve antimicrobial stewardship in primary care-is it fit for purpose? Fam. Pr. 2018, 35, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Ellen, M.E.; Shach, R.; Perlman, S. Exploring community healthcare providers’ perceptions on antimicrobial resistance. J. Glob. Antimicrob. Resist. 2019, 18, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Kesten, J.M.; Bhattacharya, A.; Ashiru-Oredope, D.; Gobin, M.; Audrey, S. The Antibiotic Guardian campaign: A qualitative evaluation of an online pledge-based system focused on making better use of antibiotics. BMC Public Health 2017, 18, 5. [Google Scholar] [CrossRef] [PubMed]
- Chaintarli, K.; Ingle, S.M.; Bhattacharya, A.; Ashiru-Oredope, D.; Oliver, I.; Gobin, M. Impact of a United Kingdom-wide campaign to tackle antimicrobial resistance on self-reported knowledge and behaviour change. BMC Public Health 2016, 16, 393. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. Antibiotic Guardian. Available online: https://antibioticguardian.com/ (accessed on 27 July 2021).
- Charani, E.; Edwards, R.; Sevdalis, N.; Alexandrou, B.; Sibley, E.; Mullett, D.; Franklin, B.D.; Holmes, A. Behavior change strategies to influence antimicrobial prescribing in acute care: A systematic review. Clin. Infect. Dis. 2011, 53, 651–662. [Google Scholar] [CrossRef] [PubMed]
- Arnold, S.R.; Straus, S.E. Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database Syst. Rev. 2005, 2005, Cd003539. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. Behaviour Change and Antibiotic Prescribing in Healthcare Settings: Literature Review and Behavioural Analysis. 2015. Available online: https://www.gov.uk/government/publications/antibiotic-prescribing-and-behaviour-change-in-healthcare-settings (accessed on 1 April 2021).




| Statement | UK | EU/EEA |
|---|---|---|
| I have easy access to guidelines I need on managing infections (UK, n = 2291; EU/EEA, n = 14,301) | 79.7% | 75.1% |
| I have easy access to the materials I need to give advice on prudent antibiotic use and antibiotic resistance (UK, n = 2291; EU/EEA, n = 14,299) | 67.5% | 67.5% |
| I have good opportunities to provide advice on prudent antibiotic use to individuals (UK, n = 2291; EU/EEA, n = 14,296) | 61.6% | 72.3% |
| Motivation Statement | Agree or Strongly Agree | Disagree or Strongly Disagree | Undecided | Do Not Understand the Question |
|---|---|---|---|---|
| I am confident making antibiotic prescribing decisions (n = 682) | 90.0 | 3.2 | 6.6 | 0.1 |
| I have confidence in the antibiotic guidelines available to me (n = 681) | 95.6 | 1.5 | 2.8 | 0.1 |
| I have a key role in helping control antibiotic resistance (n = 681) | 88.4 | 3.7 | 7.6 | 0.3 |
| I consider antibiotic resistance when treating a patient (n = 681) | 91.6 | 3.1 | 5.0 | 0.3 |
| I have easy access to antibiotic guidelines I need to treat infections (n = 681) | 94.0 | 1.9 | 4.0 | 0.1 |
| I feel supported to not prescribe antibiotic when they are not necessary (n = 680) | 74.3 | 8.4 | 17.1 | 0.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ashiru-Oredope, D.; Casale, E.; Harvey, E.; Umoh, E.; Vasandani, S.; Reilly, J.; Hopkins, S. Knowledge and Attitudes about Antibiotics and Antibiotic Resistance of 2404 UK Healthcare Workers. Antibiotics 2022, 11, 1133. https://doi.org/10.3390/antibiotics11081133
Ashiru-Oredope D, Casale E, Harvey E, Umoh E, Vasandani S, Reilly J, Hopkins S. Knowledge and Attitudes about Antibiotics and Antibiotic Resistance of 2404 UK Healthcare Workers. Antibiotics. 2022; 11(8):1133. https://doi.org/10.3390/antibiotics11081133
Chicago/Turabian StyleAshiru-Oredope, Diane, Ella Casale, Eleanor Harvey, Eno Umoh, Sagar Vasandani, Jacqui Reilly, and Susan Hopkins. 2022. "Knowledge and Attitudes about Antibiotics and Antibiotic Resistance of 2404 UK Healthcare Workers" Antibiotics 11, no. 8: 1133. https://doi.org/10.3390/antibiotics11081133
APA StyleAshiru-Oredope, D., Casale, E., Harvey, E., Umoh, E., Vasandani, S., Reilly, J., & Hopkins, S. (2022). Knowledge and Attitudes about Antibiotics and Antibiotic Resistance of 2404 UK Healthcare Workers. Antibiotics, 11(8), 1133. https://doi.org/10.3390/antibiotics11081133






