A Randomized Controlled Trial of Colistin Combined with Sulbactam: 9 g per Day versus 12 g per Day in the Treatment of Extensively Drug-Resistant Acinetobacter baumannii Pneumonia: An Interim Analysis
Abstract
1. Introduction and Study Rationale
2. Objectives
3. Materials and Methods
3.1. Ethical Considerations
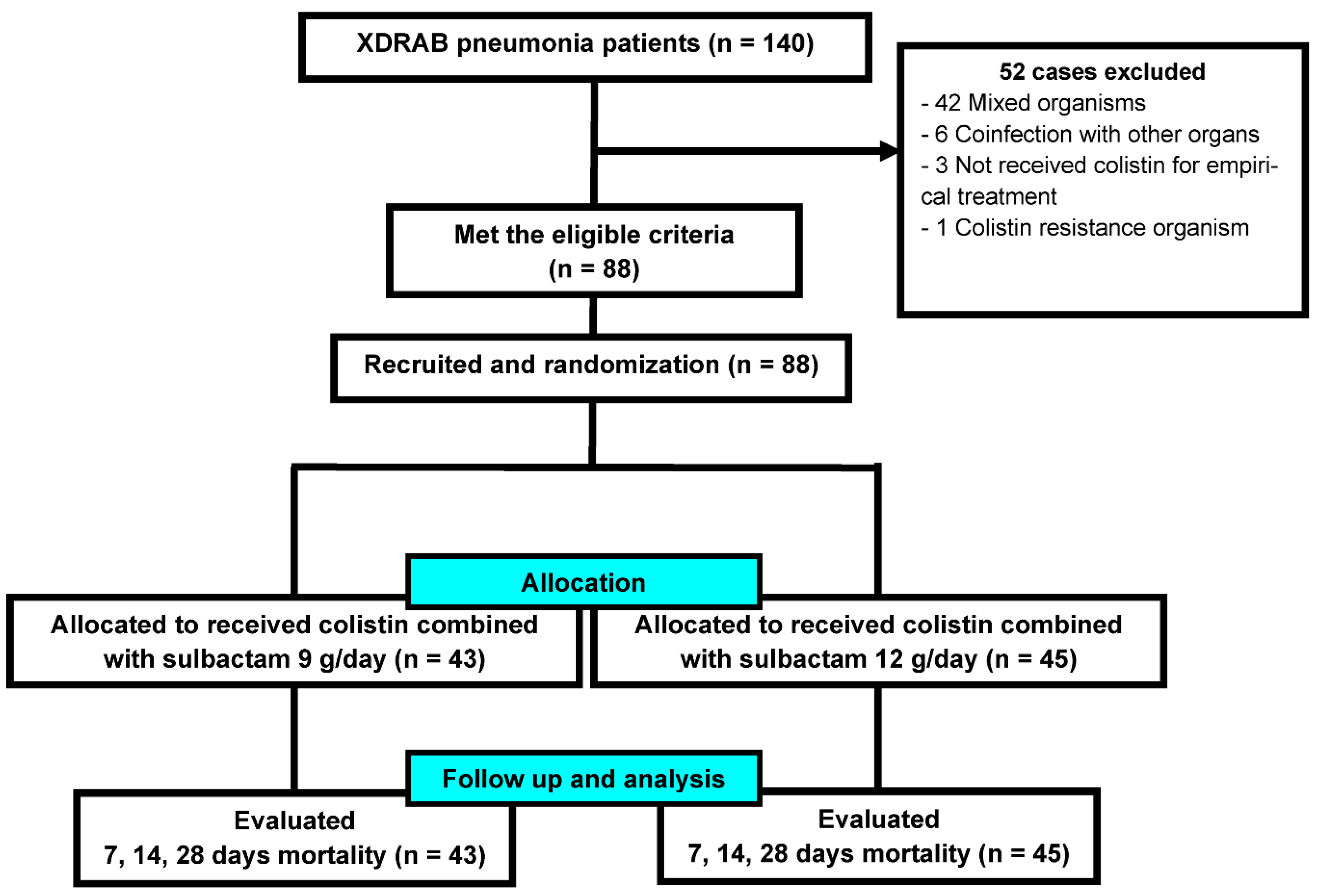
3.2. Study Design and Participants
3.3. Randomization and Masking
3.4. Procedures
3.5. Outcomes
3.6. Statistical Analysis
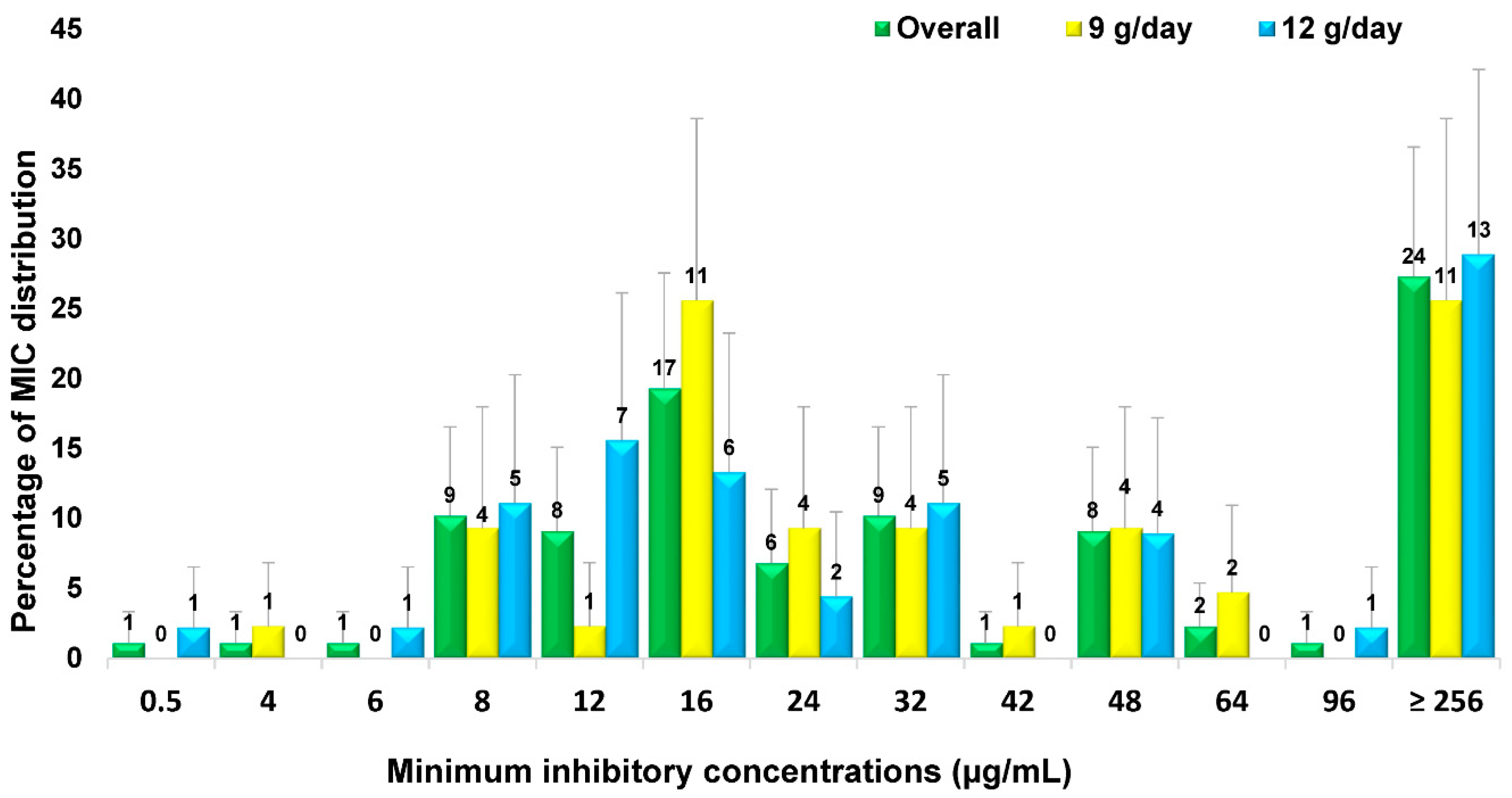
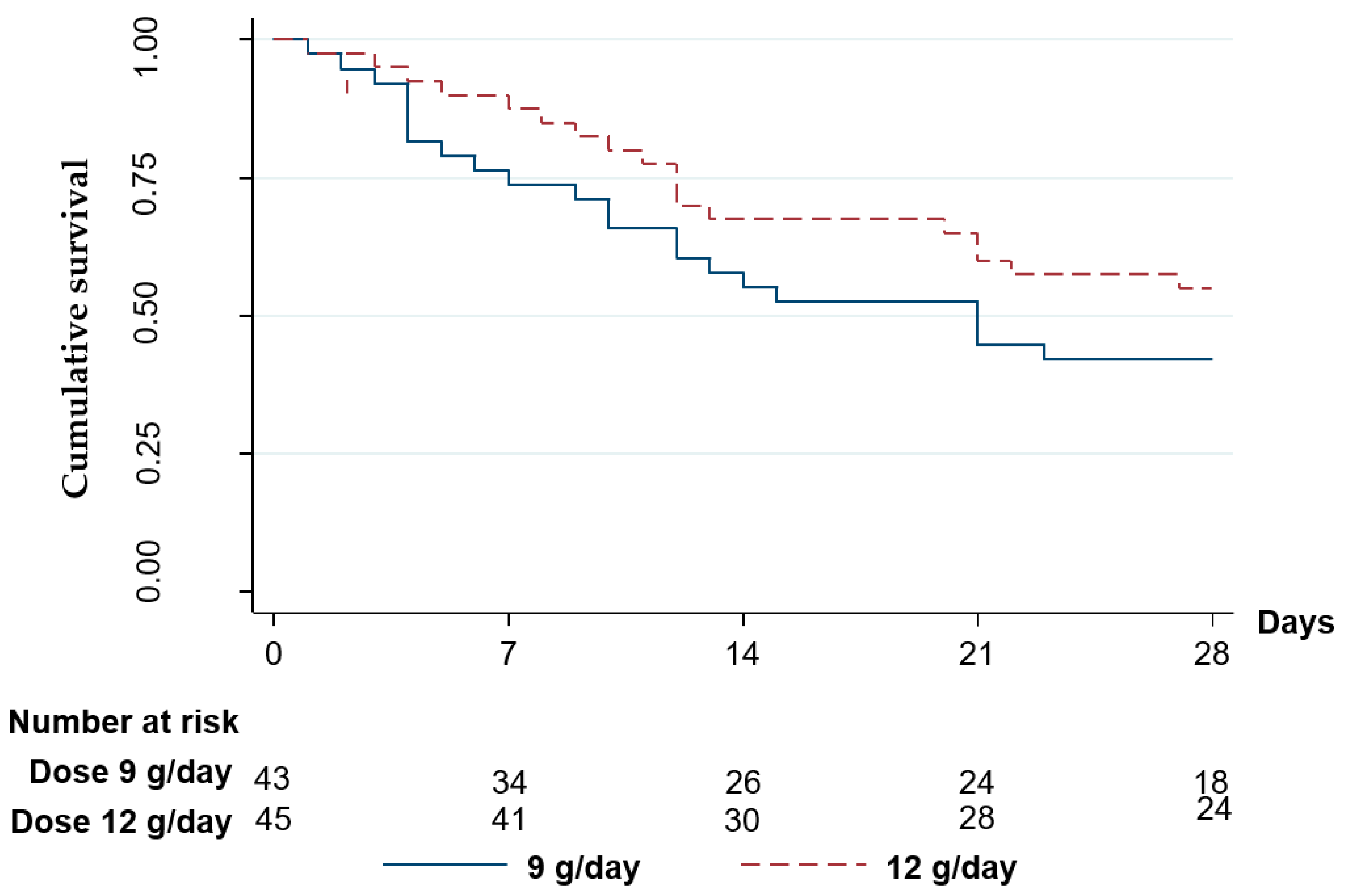
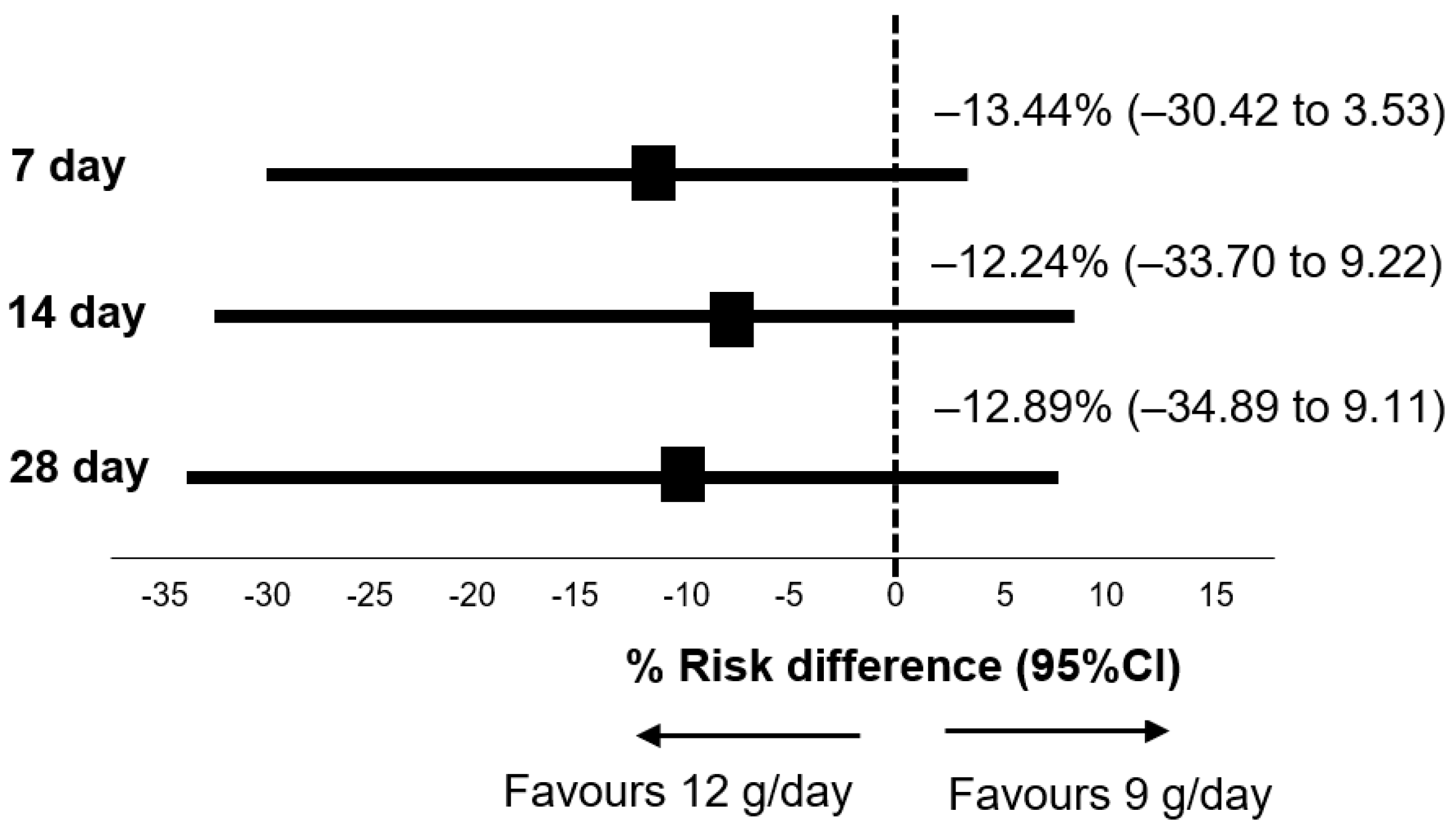
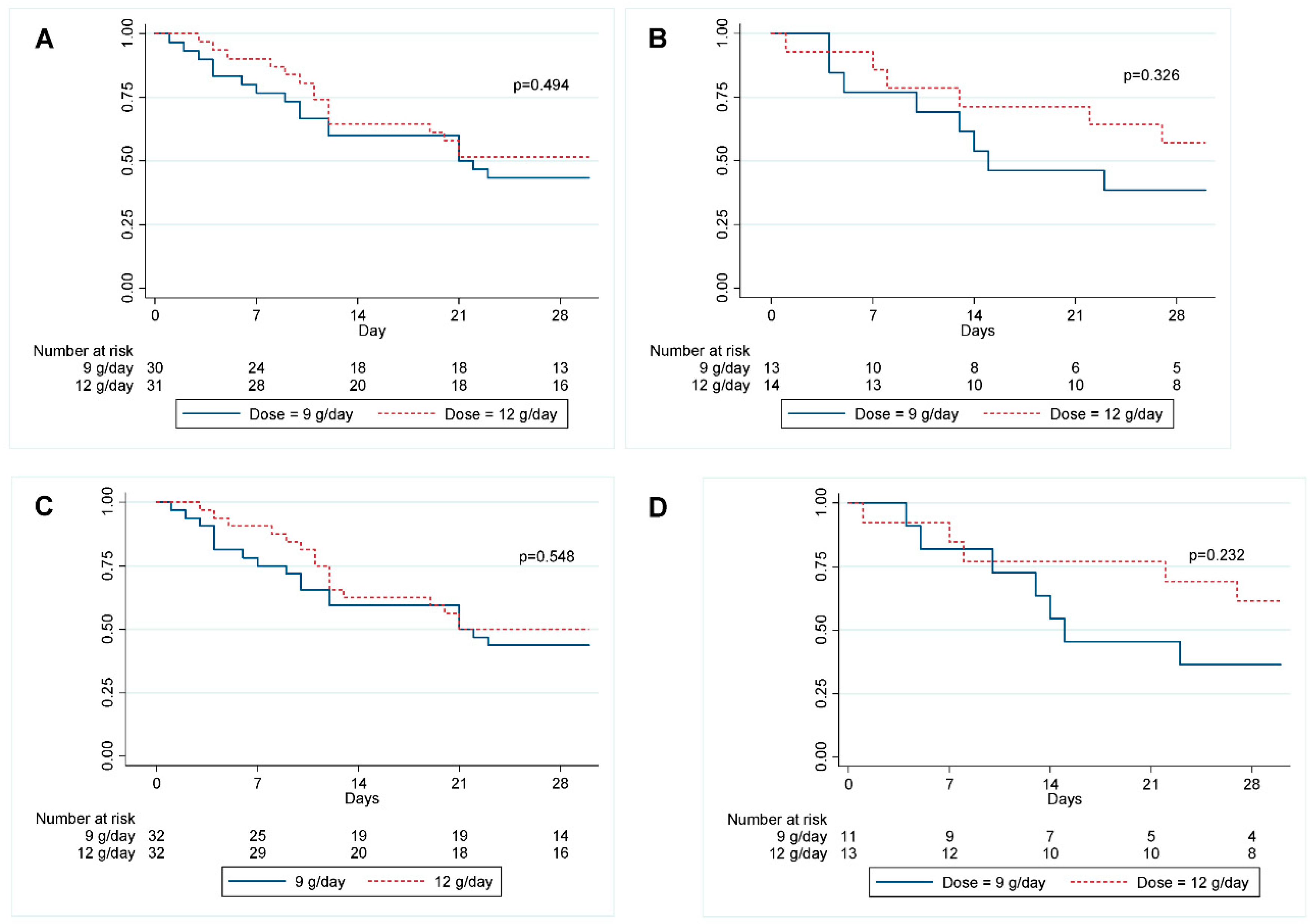
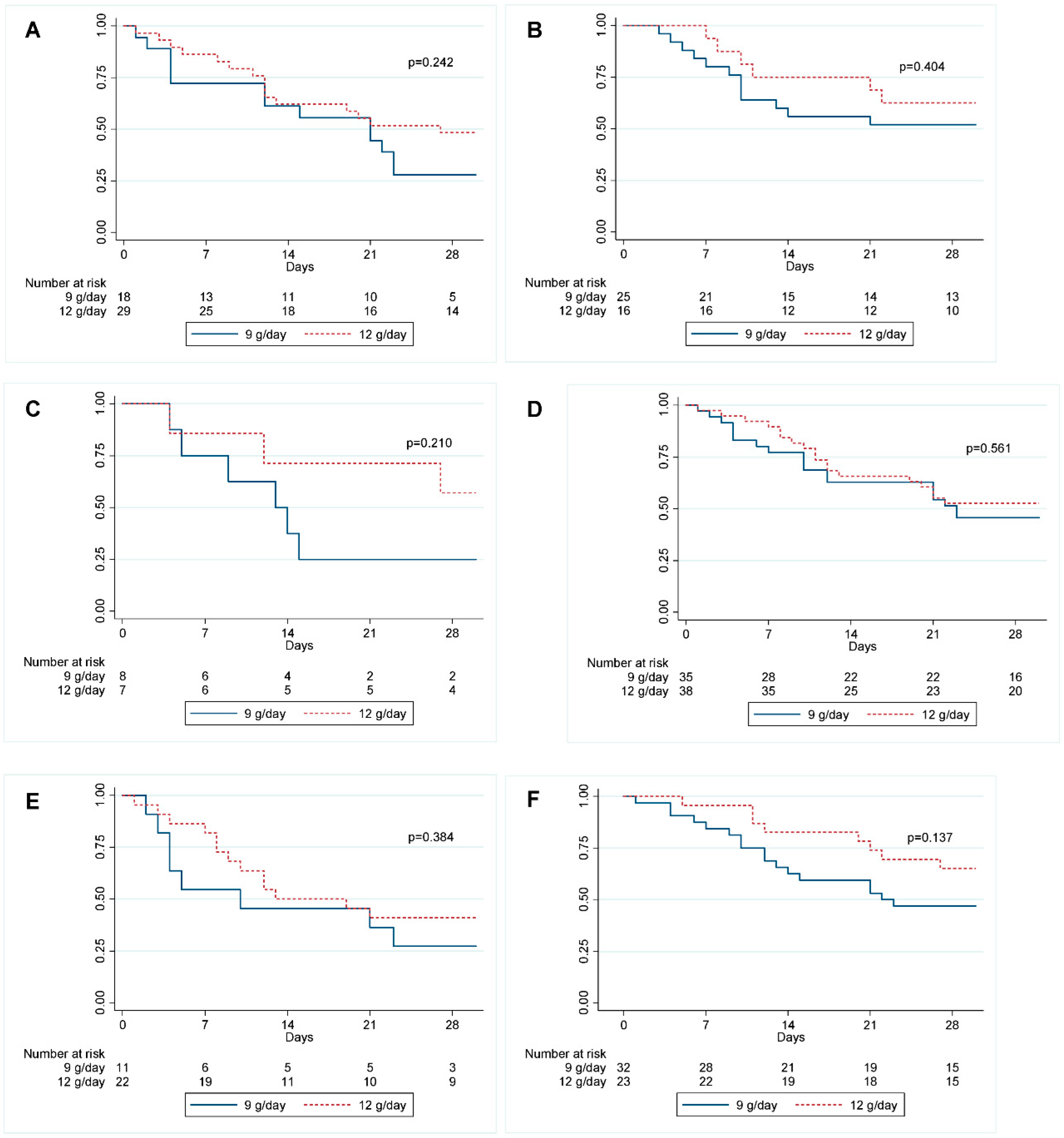
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Fournier, P.E.; Richet, H. The epidemiology and control of Acinetobacter baumannii in health care facilities. Clin. Infect. Dis. 2006, 42, 692–699. [Google Scholar] [CrossRef] [PubMed]
- Hidron, A.I.; Edwards, J.R.; Patel, J.; Horan, T.C.; Sievert, D.M.; Pollock, D.A.; Fridkin, S.K.; National Healthcare Safety Network Team; Participating National Healthcare Safety Network Facilities. Antimicrobial-resistant pathogens associated with healthcare-associated infections: Annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention 2006–2007. Infect. Control Hosp. Epidemiol. 2008, 29, 996–1011. [Google Scholar] [CrossRef] [PubMed]
- Karageorgopoulos, D.E.; Falagas, M.E. Current control and treatment of multidrug-resistant Acinetobacter baumannii infections. Lancet Infect. Dis. 2008, 8, 751–762. [Google Scholar] [CrossRef]
- Jeong, B.; Na, M.J.; Son, J.W.; Jo, D.Y.; Kwon, S.J. High-dose sulbactam treatment for ventilator-associated pneumonia caused by carbapenem-resistant Acinetobacter baumannii. Korean J. Crit. Care Med. 2016, 31, 308–316. [Google Scholar] [CrossRef]
- Kasiakou, S.K.; Michalopoulos, A.; Soteriades, E.S.; Samonis, G.; Sermaides, G.J.; Falagas, M.E. Combination therapy with intravenous colistin for management of infections due to multidrug-resistant Gram-negative bacteria in patients without cystic fibrosis. Antimicrob. Agents Chemother. 2005, 49, 3136–3146. [Google Scholar] [CrossRef]
- Infectious Diseases Society of America (IDSA). White paper: Recommendations on the conduct of superiority and organism-specific clinical trials of antibacterial agents for the treatment of infections caused by drug-resistant bacterial pathogens. Clin. Infect. Dis. 2012, 55, 1031–1046. [Google Scholar] [CrossRef]
- Girou, E.; Stephan, F.; Novara, A.; Safar, M.; Fagon, J.-Y. Risk factors and outcome of nosocomial infections: Results of a matched case-control study of ICU patients. Am. J. Respir. Crit. Care Med. 1998, 157, 1151–1158. [Google Scholar] [CrossRef]
- Sunenshine, R.H.; Wright, M.; Maragakis, L.L.; Harris, A.D.; Song, X.; Hebden, J.; Cosgrove, S.E.; Anderson, A.; Carnell, J.; Jernigan, D.B.; et al. Multidrug-resistant Acinetobacter infection mortality rate and length of hospitalization. Emerg. Infect. Dis. 2007, 13, 97. [Google Scholar] [CrossRef]
- Kwon, K.T.; Oh, W.S.; Song, J.-H.; Chang, H.-H.; Jung, S.-I.; Kim, S.; Ryu, S.Y.; Heo, S.T.; Jung, D.S.; Rhee, J.; et al. Impact of imipenem resistance on mortality in patients with Acinetobacter bacteraemia. J. Antimicrob. Chemother. 2007, 59, 525–530. [Google Scholar] [CrossRef]
- Kalin, G.; Alp, E.; Akin, A.; Coskun, R.; Doganay, M. Comparison of colistin and colistin/sulbactam for the treatment of multidrug resistant Acinetobacter baumannii ventilator-associated pneumonia. Infection 2014, 42, 37–42. [Google Scholar] [CrossRef]
- Betrosian, A.P.; Frantzeskaki, F.; Xanthaki, A.; Douzinas, E.E. Efficacy and safety of high-dose ampicillin/sulbactam vs. colistin as monotherapy for the treatment of multidrug resistant Acinetobacter baumannii ventilator-associated pneumonia. J. Infect. 2008, 56, 432–436. [Google Scholar] [CrossRef] [PubMed]
- Kallel, H.; Hergafi, L.; Bahloul, M.; Hakim, A.; Dammak, H.; Chelly, H.; Hamida, C.B.; Chaari, A.; Rekik, N.; Bouazi, M. Safety and efficacy of colistin compared with imipenem in the treatmentof ventilator-associated pneumonia: A matched case–control study. Intensive Care Med. 2007, 33, 1162–1167. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Kim, S.I.; Hong, K.-W.; Kim, Y.R.; Park, Y.J.; Kang, M.-W. Risk factors for mortality in patients with carbapenem-resistant Acinetobacter baumannii bacteremia: Impact of appropriate antimicrobial therapy. J. Korean Med. Sci. 2012, 27, 471. [Google Scholar] [CrossRef] [PubMed]
- Betrosian, A.P.; Frantzeskaki, F.; Xanthaki, A.; Georgiadis, G. High-dose ampicillin-sulbactam as an alternative treatment of late-onset VAP from multidrug-resistant Acinetobacter baumannii. Scand. J. Infect. Dis. 2007, 39, 38–43. [Google Scholar] [CrossRef]
- Oliveira, M.; Prado, G.; Costa, S.; Grinbaum, R.; Levin, A.S. Ampicillin/sulbactam compared with polymyxins for the treatment of infections caused by carbapenem-resistant Acinetobacter spp. J. Antimicrob. Chemother. 2008, 61, 1369–1375. [Google Scholar] [CrossRef]
- Kalil, A.C.; Metersky, M.L.; Klompas, M.; Muscedere, J.; Sweeney, D.A.; Palmer, L.B.; Napolitano, L.M.; O’Grady, N.P.; Bartlett, J.G.; Carratala, J.; et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 Clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin. Infect. Dis. 2016, 63, e61–e111. [Google Scholar] [CrossRef]
- Kallel, H.; Bahloul, M.; Hergafi, L.; Akrout, M.; Ketata, W.; Chelly, H.; Hamida, C.B.; Rekik, N.; Hammami, A.; Bouaziz, M.; et al. Colistin as a salvage therapy for nosocomial infections caused by multidrug-resistant bacteria in the ICU. Int. J. Antimicrob. Agents 2006, 28, 366–369. [Google Scholar] [CrossRef]
- Aimsaad, L.; Diraphat, P.; Diraphat, P.; Utrarachkij, F.; Utrarachkij, F.; Thunyaharn, S.; Samakoses, R.; Siripanichgon, K.; Siripanichgon, K. Epidemiological characteristics of Acinetobacter baumannii infections at Phramongkutklao Hospital. J. Med. Assoc. Thail. 2009, 92, S164–S172. [Google Scholar]
- Perez, F.; Hujer, A.M.; Hujer, K.M.; Decker, B.K.; Rather, P.N.; Bonomo, R.A. Global challenge of multidrug-resistant Acinetobacter baumannii. Antimicrob. Agents Chemother. 2007, 51, 3471–3484. [Google Scholar] [CrossRef]
- Penwell, W.F.; Shapiro, A.B.; Giacobbe, R.A.; Gu, R.F.; Gao, N.; Thresher, J.; McLaughlin, R.E.; Huband, M.D.; DeJonge, B.L.M.; Ehmann, D.E.; et al. Molecular mechanisms of sulbactam antibacterial activity and resistance determinants in Acinetobacter baumannii. Antimicrob. Agents Chemother. 2015, 59, 1680–1689. [Google Scholar] [CrossRef]
- Frank, U.; Schmidt-Eisenlohr, E.; Daschner, F.; Joos-Württemberger, A.; Hasse, J. Concentrations of sulbactam/ampicillin in serum and lung tissue. Infection 1990, 18, 307–309. [Google Scholar] [CrossRef] [PubMed]
- Leelasupasri, S.; Santimaleeworagun, W.; Jitwasinkul, T. Antimicrobial susceptibility among colistin, sulbactam, and fosfomycin and a synergism study of colistin in combination with sulbactam or fosfomycin against clinical isolates of carbapenem-resistant Acinetobacter baumannii. J. Pathog. 2018, 2018, 3893492. [Google Scholar] [CrossRef] [PubMed]
- Pongpech, P.; Amornnopparattanakul, S.; Panapakdee, S.; Fungwithaya, S.; Nannha, P.; Dhiraputra, C.; Leelarasamee, A. Antibacterial activity of carbapenem-based combinations against multidrug-resistant Acinetobacter baumannii. J. Med. Assoc. Thail. 2011, 93, 161. [Google Scholar]
- Ni, W.; Cui, J.; Liang, B.; Cai, Y.; Bai, N.; Cai, X.; Wang, R. In vitro effects of tigecycline in combination with colistin (polymyxin E) and sulbactam against multidrug-resistant Acinetobacter baumannii. J. Antibiot. 2013, 66, 705–708. [Google Scholar] [CrossRef]
- David, M.D.; Gill, M.J. Potential for underdosing and emergence of resistance in Acinetobacter baumannii during treatment with colistin. J. Antimicrob. Chemother. 2008, 61, 962–964. [Google Scholar] [CrossRef]
- Batirel, A.; Balkan, I.; Karabay, O.; Agalar, C.; Akalin, S.; Alici, O.; Alp, E.; Altay, F.A.; Altin, N.; Arslan, F.; et al. Comparison of colistin–carbapenem, colistin–sulbactam, and colistin plus other antibacterial agents for the treatment of extremely drug-resistant Acinetobacter baumannii bloodstream infections. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 1311–1322. [Google Scholar] [CrossRef]
- Tamma, P.D.; Aitken, S.L.; Bonomo, R.A.; Mathers, A.J.; van Duin, D.; Clancy, C.J. Infectious Diseases Society of America Guidance on the Treatment of AmpC β-Lactamase–Producing Enterobacterales, Carbapenem-Resistant Acinetobacter baumannii, and Stenotrophomonas maltophilia Infections. Clin. Infect. Dis. 2022, 74, 2089–2114. [Google Scholar] [CrossRef]
- Michalopoulos, A.; Falagas, M.E. Treatment of Acinetobacter infections. Expert Opin. Pharmacother. 2010, 11, 779–788. [Google Scholar] [CrossRef]
- Khawcharoenporn, T.; Pruetpongpun, N.; Tiamsak, P.; Rutchanawech, S.; Mundy, L.M.; Apisarnthanarak, A. Colistin-based treatment for extensively drug-resistant Acinetobacter baumannii pneumonia. Int. J. Antimicrob. Agents 2014, 43, 378–382. [Google Scholar] [CrossRef]
- Chan, J.D.; Graves, J.A.; Dellit, T.H. Antimicrobial treatment and clinical outcomes of carbapenem-resistant Acinetobacter baumannii ventilator-associated pneumonia. J. Intensive Care Med. 2010, 25, 343–348. [Google Scholar] [CrossRef]
- Koulenti, D.; Rello, J. Gram-negative bacterial pneumonia: Aetiology and management. Curr. Opin. Pulm. Med. 2006, 12, 198–204. [Google Scholar] [CrossRef] [PubMed]
- Urban, C.; Segal-Maurer, S.; Rahal, J. Considerations in control and treatment of nosocomial infections due to multidrug-resistant Acinetobacter baumannii. Clin. Infect. Dis. 2003, 36, 1268–1274. [Google Scholar] [CrossRef] [PubMed]
- Garnacho-Montero, J.; Dimopoulos, G.; Poulakou, G.; Akova, M.; Cisneros, J.M.; De Waele, J.; Petrosillo, N.; Seifert, H.; Timsit, J.F.; Vila, J.; et al. Task force on management and prevention of Acinetobacter baumannii infections in the ICU. Intensive Care Med. 2015, 41, 2057–2075. [Google Scholar] [CrossRef] [PubMed]
- Saelim, W.; Santimaleeworagun, W.; Thunyaharn, S.; Changpradub, D.; Juntanawiwat, P. Pharmacodynamic profiling of optimal sulbactam regimens against carbapenem-resistant Acinetobacter baumannii for critically ill patients. Clin. Res. 2018, 8, 14–18. [Google Scholar]
- CDC/NHSN Surveillance Definitions for Specific Types of Infections [Internet]. Available online: https://www.cdc.gov/nhsn/pdfs/pscmanual/17pscnosinfdef_current.pdf (accessed on 1 May 2022).
- Nation, R.L.; Garonzik, S.M.; Thamlikitkul, V.; Giamarellos-Bourboulis, E.J.; Forrest, A.; Paterson, D.L.; Li, J.; Silveira, F.P. Dosing guidance for intravenous colistin in critically-ill patients. Clin. Infect. Dis. 2017, 64, 565–571. [Google Scholar] [CrossRef]
- Thamlikitkul, V.; Popum, S. Monitoring of effectiveness and safety of Colistin for therapy in resistant gram-negative bacterial infections in hospitalized patients at Siriraj hospital. J. Med. Assoc. Thail. 2016, 99, 301–307. [Google Scholar]
- Jaruratanasirikul, S.; Wongpoowarak, W.; Wattanavijitkul, T.; Sukarnjanaset, W.; Samaeng, M.; Nawakitrangsan, M.; Ingviya, N. Population pharmacokinetics and pharmacodynamics modeling to optimize dosage regimens of sulbactam in critically ill patients with severe sepsis caused by Acinetobacter baumannii. Antimicrob. Agents Chemother. 2016, 60, 7236–7244. [Google Scholar] [CrossRef]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. APACHE II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonca, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef]
- Patel, J.B. Performance Standards for Antimicrobial Susceptibility Testing, 32nd ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2022. [Google Scholar]
- Levin, A.; Stevens, P.E.; Bilous, R.W.; Coresh, J.; Angel, L.M.; Francisco, D.; de Jong, P.E.; Griffith, K.E.; Hemmelgarn, B.R.; Kunitoshi Iseki, E.J.L.; et al. Kidney disease: Improving global outcomes (KDIGO) CKD work group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 2013, 3, 1–150. [Google Scholar]
- Koomanachai, P.; Tiengrim, S.; Kiratisin, P.; Thamlikitkul, V. Efficacy and safety of colistin (colistimethate sodium) for therapy of infections caused by multidrug-resistant Pseudomonas aeruginosa and Acinetobacter baumannii in Siriraj Hospital, Bangkok, Thailand. Int. J. Infect. Dis. 2007, 11, 402–406. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yilmaz, G.R.; Guven, T.; Guner, R.; Kocak Tufan, Z.; Izdes, S.; Tasyaran, M.A.; Acikgoz, Z.C. Colistin alone or combined with sulbactam or carbapenem against A. baumannii in ventilator-associated pneumonia. J. Infect. Dev. Ctries. 2015, 9, 476–485. [Google Scholar] [CrossRef] [PubMed]
- Ungthammakhun, C.; Vasikasin, V.; Changpradub, D. Clinical Outcomes of Colistin in Combination with Either 6-G Sulbactam or Carbapenems for the Treatment of Extensively Drug-Resistant Acinetobacter baumannii Pneumonia with High MIC to Sulbactam, a Prospective Cohort Study. Infect. Drug Resist. 2019, 12, 2899–2904. [Google Scholar] [CrossRef]
- Thet, K.T.; Lunha, K.; Srisrattakarn, A.; Lulitanond, A.; Tavichakorntrakool, R.; Kuwatjanakul, W.; Charoensri, N.; Chanawong, A. Colistin heteroresistance in carbapenem-resistant Acinetobacter baumannii clinical isolates from a Thai university hospital. World J. Microbiol. Biotechnol. 2020, 36, 102. [Google Scholar] [CrossRef] [PubMed]
- Yau, W.; Owen, R.J.; Poudyal, A.; Bell, J.M.; Turnidge, J.D.; Li, J. Colistin hetero-resistance in multidrug-resistant Acinetobacter baumannii clinical isolates from the Western Pacific region in the SENTRY antimicrobial surveillance programme. J. Infect. 2009, 58, 138–144. [Google Scholar] [CrossRef] [PubMed]
| Colistin/Sulbactam 9 g/Day (n = 43) | Colistin/Sulbactam 12 g/Day (n = 45) | |
|---|---|---|
| Male sex, n (%) | 30/43 (69.8%) | 35/45 (77.8%) |
| Age, years; mean ± SD | 75.35 ± 12.85 | 67.84 ± 17.74 |
| BMI, kg/m2; mean ± SD | 22.7 ± 3.92 | 21.53 ± 3.74 |
| ICU Ward, n (%) | 22/43 (51.2%) | 31/45 (68.9%) |
| Underlying disease, n (%) | ||
| Diabetes mellitus | 23/43 (53.5%) | 18/45 (40.0%) |
| Hypertension | 35/43 (81.4%) | 31/45 (68.9%) |
| Dyslipidemia | 21/43 (48.8%) | 20/45 (44.4%) |
| COPD | 4/43 (9.3%) | 2/45 (4.4%) |
| Asthma | 1/43 (2.3%) | 2/45 (4.4%) |
| Chronic kidney disease | ||
| Stage 3 | 5/43 (11.6%) | 6/45 (13.3%) |
| Stage 4 and 5 | 4/43 (9.3%) | 1/45 (2.2%) |
| ESRD | 7/43 (16.3%) | 7/45 (15.6%) |
| Cirrhosis | 2/43 (4.7%) | 2/45 (4.4%) |
| Gout | 1/43 (2.3%) | 2/45 (4.4%) |
| Ischemic heart disease | 7/43 (16.3%) | 8/45 (17.8%) |
| Stroke | 9/43 (20.9%) | 5/45 (11.1%) |
| Malignancy | 6/43 (14%) | 11/45 (24.4%) |
| Diagnosis, n (%) | ||
| HAP | 12/43 (27.9%) | 8/45 (17.8%) |
| VAP | 31/43 (72.1%) | 37/45 (82.2%) |
| APACHE II score, n (%) | ||
| ≤19 | 7/43 (16.3%) | 7/45 (15.6%) |
| 20–24 | 12/43 (27.9%) | 15/45 (33.3%) |
| 25–29 | 16/43 (37.2%) | 10/45 (22.2%) |
| ≥30 | 8/43 (18.6%) | 13/45 (28.9%) |
| SOFA score, n (%) | ||
| ≤6 | 19/43 (44.2%) | 10/45 (22.2%) |
| 7–9 | 11/43 (25.6%) | 11/45 (24.4%) |
| 10–12 | 5/43 (11.6%) | 14/45 (31.1%) |
| ≥13 | 8/43 (18.6%) | 10/45 (22.2%) |
| Complication from pneumonia, n (%) | ||
| Septic shock | 18/43 (41.9%) | 29/45 (64.4%) |
| Bacteremia | 8/43 (18.6%) | 7/45 (15.6%) |
| DIC | 11/43 (25.6%) | 22/45 (48.9%) |
| Empirical antibiotics, n (%) | ||
| Carbapenems | 35/43 (81.4%) | 42/45 (93.3%) |
| Sulbactam | 2/43 (4.7%) | 2/45 (4.4%) |
| Others | 6/43 (14.0%) | 1/45 (2.2%) |
| Days | 9 g/day | 12 g/day | p-Value |
|---|---|---|---|
| Survivor Rate % (95% CI) | Survivor Rate % (95% CI) | ||
| 7 | 76.7 (61.1–86.8) | 88.9 (75.3–95.2) | 0.17 |
| 14 | 58.1 (42.1–71.2) | 66.7 (50.9–78.4) | 0.27 |
| 28 | 41.9 (27.1–55.9) | 53.3 (37.9–66.6) | 0.26 |
| Colistin/Sulbactam 9 g/Day | Colistin/Sulbactam 12 g/Day | p-Value | |
|---|---|---|---|
| Length of stay, days; median (95% CI) | 31 (19, 43) | 36 (7, 71) | 0.08 |
| Ventilator days, days; median (95% CI) | |||
| HAP group | 3 (1, 8) | 13 (1, 29) | 0.13 |
| VAP group | 19 (4, 34) | 23 (19, 27) | 0.46 |
| ICU days, days; median (95% CI) | 14 (12, 16) | 17 (6, 28) | 0.33 |
| Microbiological cure at day 7, n (%) | 25/43 (58.1%) | 38/42 (90.5%) | 0.02 |
| Adverse Events, n (%) | Colistin/Sulbactam 9 g/Day (n = 43) | Colistin/Sulbactam 12 g/Day (n = 45) | p-Value |
|---|---|---|---|
| Any adverse events | 17/43 (39.5%) | 17/45 (37.8%) | 0.87 |
| AKI | 12/43 (27.9%) | 15/45 (33.3%) | 0.58 |
| Diarrhea | 5/43 (11.6%) | 2/45 (4.4%) | 0.21 |
| Variables | Crude Analysis | Adjusted Analysis | ||
|---|---|---|---|---|
| HR (95%CI) | p-Value | HR (95%CI) | p-Value | |
| Underlying disease | ||||
| Asthma | 3.59 (1.09, 11.81) | 0.04 | 4.69 (1.22, 18.09) | 0.03 |
| Cirrhosis | 4.39 (1.53, 12.56) | 0.01 | 3.8 (1.06, 13.57) | 0.04 |
| APACHE score ≥ 28 | 3.57 (1.99, 6.40) | <0.01 | 2.94 (1.51, 5.72) | <0.01 |
| SOFA score ≥ 9 | 1.93 (1.05, 3.55) | 0.03 | 1.71 (0.58, 5.01) | 0.33 |
| Dosage ofSulbactam | ||||
| 9 g/day | 1.39 (0.78,2.47) | 0.27 | 2.02 (1.1, 3.71) | 0.02 |
| 12 g/day | Reference | 1 | Reference | 1 |
| Complication from pneumonia | ||||
| DIC | 1.84 (1.03, 3.29) | 0.04 | 1.53 (0.79, 2.96) | 0.21 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ungthammakhun, C.; Vasikasin, V.; Changpradub, D. A Randomized Controlled Trial of Colistin Combined with Sulbactam: 9 g per Day versus 12 g per Day in the Treatment of Extensively Drug-Resistant Acinetobacter baumannii Pneumonia: An Interim Analysis. Antibiotics 2022, 11, 1112. https://doi.org/10.3390/antibiotics11081112
Ungthammakhun C, Vasikasin V, Changpradub D. A Randomized Controlled Trial of Colistin Combined with Sulbactam: 9 g per Day versus 12 g per Day in the Treatment of Extensively Drug-Resistant Acinetobacter baumannii Pneumonia: An Interim Analysis. Antibiotics. 2022; 11(8):1112. https://doi.org/10.3390/antibiotics11081112
Chicago/Turabian StyleUngthammakhun, Chutchawan, Vasin Vasikasin, and Dhitiwat Changpradub. 2022. "A Randomized Controlled Trial of Colistin Combined with Sulbactam: 9 g per Day versus 12 g per Day in the Treatment of Extensively Drug-Resistant Acinetobacter baumannii Pneumonia: An Interim Analysis" Antibiotics 11, no. 8: 1112. https://doi.org/10.3390/antibiotics11081112
APA StyleUngthammakhun, C., Vasikasin, V., & Changpradub, D. (2022). A Randomized Controlled Trial of Colistin Combined with Sulbactam: 9 g per Day versus 12 g per Day in the Treatment of Extensively Drug-Resistant Acinetobacter baumannii Pneumonia: An Interim Analysis. Antibiotics, 11(8), 1112. https://doi.org/10.3390/antibiotics11081112






