Pharmacokinetics and Pharmacodynamics of Colistin Methanesulfonate in Healthy Chinese Subjects after Multi-Dose Regimen
Abstract
:1. Introduction
2. Results
2.1. Demographics of the Subjects
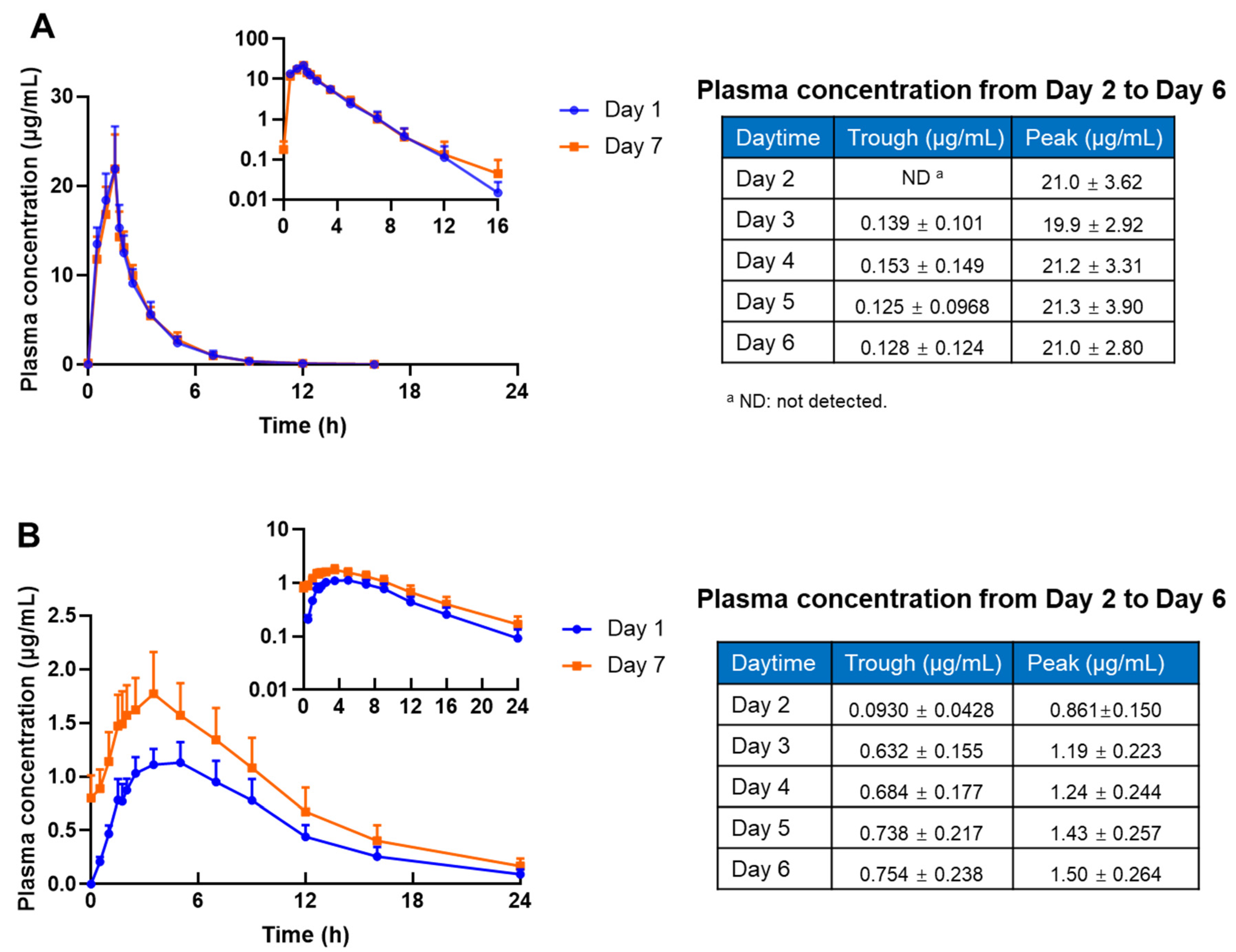
2.2. Pharmacokinetics Analysis
2.3. Pharmacokinetics/Pharmacodynamics Analysis
2.4. Safety Evaluation
3. Discussion
4. Materials and Methods
4.1. Study Design and Dosing Regimen
4.2. Subjects
4.3. Sample Collection and Preparation for Pharmacokinetics Analysis
4.4. Determination of CMS and Colistin Concentrations in Plasma and Urine Samples
4.5. Pharmacokinetics Analysis
4.6. Pharmacokinetics/Pharmacodynamics Analysis
4.7. Safety Evaluation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- CDC. Antibiotic Resistance Coordination and Strategy Unit. Antibiotic Resistance Threats in the United States. 2019. Available online: https://stacks.cdc.gov/view/cdc/82532 (accessed on 1 December 2019).
- Hu, F.; Guo, Y.; Zhu, D.; Wang, F.; Jiang, X.; Xu, Y.; Zhang, X. CHINET surveillance of bacterial resistance: Results of 2020. Chin. J. Infect. Chemother. 2021, 21, 377–387. [Google Scholar]
- Nordmann, P.; Poirel, L. Epidemiology and diagnostics of carbapenem resistance in Gram-negative bacteria. Clin. Infect. Dis. 2019, 69, S521–S528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cai, B.; Echols, R.; Magee, G.; Arjona Ferreira, J.C.; Morgan, G.; Ariyasu, M.; Sawada, T.; Nagata, T.D. Prevalence of carbapenem-resistant gram-negative infections in the United States predominated by Acinetobacter baumannii and Pseudomonas aeruginosa. Open Forum. Infect. Dis. 2017, 4, ofx176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nation, R.L.; Li, J. Colistin in the 21st century. Curr. Opin. Infect. Dis. 2009, 22, 535–543. [Google Scholar] [CrossRef] [PubMed]
- Cheah, S.E.; Wang, J.; Nguyen, V.T.; Turnidge, J.D.; Li, J.; Nation, R.L. New pharmacokinetic/pharmacodynamic studies of systemically administered colistin against Pseudomonas aeruginosa and Acinetobacter baumannii in mouse thigh and lung infection models: Smaller response in lung infection. J. Antimicrob. Chemother. 2015, 70, 3291–3297. [Google Scholar] [CrossRef] [Green Version]
- Tsuji, B.T.; Pogue, J.M.; Zavascki, A.P.; Paul, M.; Daikos, G.L.; Forrest, A.; Giacobbe, D.R.; Viscoli, C.; Giamarellou, H.; Karaiskos, I.; et al. International Consensus Guidelines for the Optimal Use of the Polymyxins: Endorsed by the American College of Clinical Pharmacy (ACCP), European Society of Clinical Microbiology and Infectious Diseases (ESCMID), Infectious Diseases Society of America (IDSA), International Society for Anti-infective Pharmacology (ISAP), Society of Critical Care Medicine (SCCM), and Society of Infectious Diseases Pharmacists (SIDP). Pharmacotherapy 2019, 39, 10–39. [Google Scholar] [CrossRef]
- Nation, R.L.; Garonzik, S.M.; Li, J.; Thamlikitkul, V.; Giamarellos-Bourboulis, E.J.; Paterson, D.L.; Turnidge, J.D.; Forrest, A.; Silveira, F.P. Updated US and European dose recommendations for intravenous colistin: How do they perform? Clin. Infect. Dis. 2016, 62, 552–558. [Google Scholar] [CrossRef] [Green Version]
- EDQM. Colistimethate Sodium. EP92. 2017. Available online: http://online6.edqm.eu/ep902/ (accessed on 23 February 2017).
- Fan, Y.X.; Chen, Y.C.; Li, Y.; Yu, J.C.; Bian, X.C.; Li, X.; Li, W.Z.; Guo, B.N.; Wu, H.L.; Liu, X.F.; et al. Effects of different component contents of colistin methanesulfonate on the pharmacokinetics of prodrug and formed colistin in human. Pharm. Res. 2021, 38, 79–87. [Google Scholar] [CrossRef]
- Landersdorfer, C.B.; Wang, J.; Wirth, V.; Chen, K.; Kaye, K.S.; Tsuji, B.T.; Li, J.; Nation, R.L. Pharmacokinetics/pharmacodynamics of systemically administered polymyxin B against Klebsiella pneumoniae in mouse thigh and lung infection models. J. Antimicrob. Chemother. 2018, 73, 462–468. [Google Scholar] [CrossRef] [Green Version]
- Guo, Y.; Yin, D.; Hu, F.; Gao, J.; He, L.; Wu, W.; Sun, J.; Ni, Y.; Tang, J.; Yu, J.; et al. Evaluation of methods for testing the susceptibility of carbapenem-resistant gram-negative bacilli to colistin and polymyxin B. Chin. J. Infect. Chemother. 2020, 20, 525–535. [Google Scholar] [CrossRef]
- Nation, R.L.; Garonzik, S.M.; Thamlikitkul, V.; Giamarellos-Bourboulis, E.J.; Forrest, A.; Paterson, D.L.; Li, J.; Silveira, F.P. Dosing guidance for intravenous colistin in critically-ill patients. Clin. Infect. Dis. 2017, 64, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Kristoffersson, A.N.; Rognas, V.; Brill, M.J.E.; Dishon-Benattar, Y.; Durante-Mangoni, E.; Daitch, V.; Skiada, A.; Lellouche, J.; Nutman, A.; Kotsaki, A.; et al. Population pharmacokinetics of colistin and the relation to survival in critically ill patients infected with colistin susceptible and carbapenem-resistant bacteria. Clin. Microbiol. Infect. 2020, 26, 1644–1650. [Google Scholar] [CrossRef] [PubMed]
- Jitaree, K.; Sathirakul, K.; Houngsaitong, J.; Asuphon, O.; Saelim, W.; Thamlikitkul, V.; Montakantikul, P. Pharmacokinetic/pharmacodynamic (PK/PD) simulation for dosage optimization of colistin against carbapenem-resistant Klebsiella pneumoniae and carbapenem-resistant Escherichia coli. Antibiotics 2019, 8, 125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sorli, L.; Luque, S.; Li, J.; Campillo, N.; Danes, M.; Montero, M.; Segura, C.; Grau, S.; Horcajada, J.P. Colistin for the treatment of urinary tract infections caused by extremely drug-resistant Pseudomonas aeruginosa: Dose is critical. J. Infect. 2019, 79, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.; Liu, X.F.; Huang, J.; Zhu, D.M.; Li, J.; Zhang, J. Activities of colistin- and minocycline-based combinations against extensive drug resistant Acinetobacter baumannii isolates from intensive care unit patients. BMC Infect. Dis. 2011, 11, 109. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.; Zhao, M.; Chen, Y.; Bian, X.; Li, Y.; Shi, J.; Zhang, J. Synergistic killing by meropenem and colistin combination of carbapenem-resistant Acinetobacter baumannii isolates from Chinese patients in an in vitro pharmacokinetic/pharmacodynamic model. Int. J. Antimicrob. Agents 2016, 48, 559–563. [Google Scholar] [CrossRef]
- Bian, X.; Liu, X.; Feng, M.; Bergen, P.J.; Li, J.; Chen, Y.; Zheng, H.; Song, S.; Zhang, J. Enhanced bacterial killing with colistin/sulbactam combination against carbapenem-resistant Acinetobacter baumannii. Int. J. Antimicrob. Agents 2021, 57, 106271. [Google Scholar] [CrossRef]
- Katip, W.; Oberdorfer, P. Clinical efficacy and nephrotoxicity of colistin alone versus colistin plus vancomycin in critically ill patients infected with carbapenem-resistant Acinetobacter baumannii: A propensity score-matched analysis. Pharmaceutics 2021, 13, 162. [Google Scholar] [CrossRef]
- Paul, M.; Daikos, G.L.; Durante-Mangoni, E.; Yahav, D.; Carmeli, Y.; Benattar, Y.D.; Skiada, A.; Andini, R.; Eliakim-Raz, N.; Nutman, A.; et al. Colistin alone versus colistin plus meropenem for treatment of severe infections caused by carbapenem-resistant Gram-negative bacteria: An open-label, randomised controlled trial. Lancet Infect. Dis. 2018, 18, 391–400. [Google Scholar] [CrossRef]
- Kengkla, K.; Kongpakwattana, K.; Saokaew, S.; Apisarnthanarak, A.; Chaiyakunapruk, N. Comparative efficacy and safety of treatment options for MDR and XDR Acinetobacter baumannii infections: A systematic review and network meta-analysis. J. Antimicrob. Chemother. 2018, 73, 22–32. [Google Scholar] [CrossRef] [Green Version]
- Zhao, M.; Wu, X.; Fan, Y.; Zhang, Y.; Guo, B.; Yu, J.; Cao, G.; Chen, Y.; Wu, J.; Shi, Y.; et al. Pharmacokinetics of colistin methanesulfonate (CMS) in healthy Chinese subjects after single and multiple intravenous doses. Int. J. Antimicrob. Agents. 2018, 51, 714–720. [Google Scholar] [CrossRef] [PubMed]
- Mizuyachi, K.; Hara, K.; Wakamatsu, A.; Nohda, S.; Hirama, T. Safety and pharmacokinetic evaluation of intravenous colistin methanesulfonate sodium in Japanese healthy male subjects. Curr. Med. Res. Opin. 2011, 27, 2261–2270. [Google Scholar] [CrossRef] [PubMed]
- Luque, S.; Escano, C.; Sorli, L.; Li, J.; Campillo, N.; Horcajada, J.P.; Salas, E.; Grau, S. Urinary concentrations of colistimethate and formed colistin after intravenous administration in patients with multidrug-resistant gram-negative bacterial infections. Antimicrob. Agents Chemother. 2017, 61, e02595-16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miano, T.A.; Lautenbach, E.; Wilson, F.P.; Guo, W.; Borovskiy, Y.; Hennessy, S. Attributable risk and time course of colistin-associated acute kidney injury. Clin. J. Am. Soc. Nephrol. 2018, 13, 542–550. [Google Scholar] [CrossRef] [Green Version]
- Yendewa, G.A.; Griffiss, J.M.; Gray, W.A.; Healen, A.; Proskin, H.M.; Fulton, S.A.; O’Riordan, M.A.; Hoppel, C.; Blumer, J.L.; Salata, R.A. Dosing colistimethate every 8 h results in higher plasma concentrations of active colistin than every 12-hourly dosing without increase in nephrotoxicity: A phase 1 pharmacokinetics trial in healthy adult volunteers. Antibiotics 2022, 11, 490. [Google Scholar] [CrossRef]
- Katip, W.; Uitrakul, S.; Oberdorfer, P. Clinical efficacy and nephrotoxicity of the loading dose colistin for the treatment of carbapenem-resistant Acinetobacter baumannii in critically ill patients. Pharmaceutics 2021, 14, 31. [Google Scholar] [CrossRef]
- Bellos, I.; Pergialiotis, V.; Frountzas, M.; Kontzoglou, K.; Daskalakis, G.; Perrea, D.N. Efficacy and safety of colistin loading dose: A meta-analysis. J. Antimicrob. Chemother. 2020, 75, 1689–1698. [Google Scholar] [CrossRef]
- Zhao, M.; Wu, X.J.; Fan, Y.X.; Guo, B.N.; Zhang, J. Development and validation of a UHPLC-MS/MS assay for colistin methanesulphonate (CMS) and colistin in human plasma and urine using weak-cation exchange solid-phase extraction. J. Pharm. Biomed. Anal. 2016, 124, 303–308. [Google Scholar] [CrossRef]
- Matzneller, P.; Gobin, P.; Lackner, E.; Zeitlinger, M. Feasibility of microdialysis for determination of protein binding and target site pharmacokinetics of colistin in vivo. J. Clin. Pharmacol. 2015, 55, 431–437. [Google Scholar] [CrossRef]

| PK Parameter | Unit | CMS | Colistin | ||||
|---|---|---|---|---|---|---|---|
| Day 1 (First Dose) | Day 7 (Last Dose) | p Value * | Day 1 (First Dose) | Day 7 (Last Dose) | p Value * | ||
| Cmax | μg/mL | 22.2 ± 4.38 | 21.9 ± 3.85 | 0.882 | 1.17 ± 0.18 | 1.79 ± 0.37 | <0.001 |
| Cmin,ss | μg/mL | \ | 0.133 ± 0.141 | \ | \ | 0.67 ± 0.22 | \ |
| Cavg,ss | μg/mL | \ | 4.41 ± 0.754 | \ | \ | 1.27 ± 0.27 | \ |
| AUC0–12 | h·μg/mL | 53.73 ± 9.77 | 52.93 ± 9.05 | 0.636 | 9.80 ± 1.71 | 15.28 ± 3.29 | <0.001 |
| AUC0–24 | h·μg/mL | 53.96 ± 9.93 | \ | \ | 12.59 ± 2.55 | \ | \ |
| Tmax a | h | 1.35 ± 0.18 | 1.41 ± 0.13 | 0.414 | 4.42 ± 0.90 | 3.38 ± 0.68 | 0.015 |
| T1/2 b | h | 1.37 ± 0.34 | 2.32 ± 1.68 | 0.083 | 5.15 ± 0.95 | 5.90 ± 0.58 | 0.011 |
| CLt | L/(h·kg) | 0.08 ± 0.02 | 0.08 ± 0.02 | 0.777 | 0.21 ± 0.05 | 0.18 ± 0.04 | <0.001 |
| CLr | L/(h·kg) | 0.06 ± 0.01 | 0.04 ± 0.02 | 0.008 | 0.0008 ± 0.0004 | 0.0015 ± 0.0007 | <0.001 |
| Vd | L/kg | 0.15 ± 0.03 | 0.14 ± 0.01 | 0.367 | 1.52 ± 0.22 | 1.66 ± 0.25 | 0.019 |
| AI | \ | \ | 1.07 ± 0.10 | \ | \ | 1.32 ± 0.06 | \ |
| fm | \ | 0.27 ± 0.12 | 0.45 ± 0.15 | 0.007 | \ | \ | \ |
| Bacteria Type | Effect | fAUC0–24/MIC Target a | MIC of Colistin (μg/mL) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 0.06 | 0.125 | 0.25 | 0.5 | 1 | 2 | 4 | |||
| Acinetobacter baumannii | 1 log kill b | 13.9 | 99.99 | 99.99 | 99.98 | 99.68 | 67.26 | 0.00 | 0.00 |
| 2 log kill c | 17.6 | 99.99 | 99.99 | 99.96 | 97.69 | 24.01 | 0.00 | 0.00 | |
| Klebsiella pneumoniae | 1 log kill b | 17.4 | 99.99 | 99.99 | 99.96 | 97.90 | 26.08 | 0.00 | 0.00 |
| Pseudomonas aeruginosa | 1 log kill b | 10.9 | 100.00 | 99.99 | 99.98 | 99.88 | 91.27 | 2.52 | 0.00 |
| 2 log kill c | 13.7 | 99.99 | 99.99 | 99.98 | 99.68 | 69.49 | 0.00 | 0.00 | |
| Pathogen a | Effect | PK/PD Breakpoint | MIC of Colistin d | |
|---|---|---|---|---|
| MIC50 | MIC90 | |||
| CRAB | 1 log kill b | 0.5 | 0.5 | 1 |
| 2 log kill c | 0.5 | 0.5 | 1 | |
| CRKP | 1 log kill b | 0.5 | 0.25 | 0.5 |
| CRPA | 1 log kill b | 1 | 1 | 1 |
| 2 log kill c | 0.5 | 1 | 1 | |
| Subject ID | Clinical Adverse Event (Duration) | Abnormality in Laboratory Test |
|---|---|---|
| S01 | Facial itchiness (2 days) | Normal |
| S02 | Normal | Normal |
| S03 | Tongue numbness (5 days and 20 h) Dizziness (4 h) | Normal |
| S04 | Tongue numbness (5 days and 14 h) | Normal |
| S05 | Tongue numbness (5 days and 8 h) Dizziness (2 days and 13 h) Headache (1 day and 19 h) Lip numbness (1 day and 10 h) Skin itchiness (1 day and 20 h) | Normal |
| S06 | Tongue numbness (5 days and 20 h) Lip numbness (2 days and 15 h) Pharyngeal discomfort (5 days and 16 h) Facial numbness (4 days and 16 h) | Normal |
| S07 | Facial itchiness (5 days and 4 h) | Normal |
| S08 | Facial itchiness (4 days and 12 h) Tongue numbness (5 days and 2 h) Dizziness (2 days and 16 h) | Normal |
| S09 | Facial itchiness (8 h) | Normal |
| S10 | Tongue numbness (1 day and 20 h) | Normal |
| S11 | Facial itchiness (2 days and 3 h) Tongue numbness (5 days and 8 h) | Normal |
| S12 | Tongue numbness (6 days and 12 h) Lip numbness (5 days and 10 h) Sore throat (1 day and 23 h) Erythema (6 days and 13 h) | Decreased absolute value of neutrophils (2 days) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, Y.; Li, Y.; Chen, Y.; Yu, J.; Liu, X.; Li, W.; Guo, B.; Li, X.; Wang, J.; Wu, H.; et al. Pharmacokinetics and Pharmacodynamics of Colistin Methanesulfonate in Healthy Chinese Subjects after Multi-Dose Regimen. Antibiotics 2022, 11, 798. https://doi.org/10.3390/antibiotics11060798
Fan Y, Li Y, Chen Y, Yu J, Liu X, Li W, Guo B, Li X, Wang J, Wu H, et al. Pharmacokinetics and Pharmacodynamics of Colistin Methanesulfonate in Healthy Chinese Subjects after Multi-Dose Regimen. Antibiotics. 2022; 11(6):798. https://doi.org/10.3390/antibiotics11060798
Chicago/Turabian StyleFan, Yaxin, Yi Li, Yuancheng Chen, Jicheng Yu, Xiaofen Liu, Wanzhen Li, Beining Guo, Xin Li, Jingjing Wang, Hailan Wu, and et al. 2022. "Pharmacokinetics and Pharmacodynamics of Colistin Methanesulfonate in Healthy Chinese Subjects after Multi-Dose Regimen" Antibiotics 11, no. 6: 798. https://doi.org/10.3390/antibiotics11060798
APA StyleFan, Y., Li, Y., Chen, Y., Yu, J., Liu, X., Li, W., Guo, B., Li, X., Wang, J., Wu, H., Wang, Y., Hu, J., Guo, Y., Hu, F., Xu, X., Cao, G., Wu, J., Zhang, Y., Zhang, J., & Wu, X. (2022). Pharmacokinetics and Pharmacodynamics of Colistin Methanesulfonate in Healthy Chinese Subjects after Multi-Dose Regimen. Antibiotics, 11(6), 798. https://doi.org/10.3390/antibiotics11060798







