Application of Artificial Intelligence in Combating High Antimicrobial Resistance Rates
Abstract
1. Introduction
Antibiotic Resistance; the Current Scenario
2. Artificial Intelligence against Antibiotic Resistance
Assistance Strategies of AI in AMR
3. Use of Artificial Intelligence in Pakistan
4. Artificial Intelligence Treating Patients in the Intensive Care Unit (ICU)
Previously Adopted AI Models in ICUs in Relation to Infections and AMR
5. Strategies to Overcome Antibiotic Resistance
Strategic Considerations for Artificial Intelligence
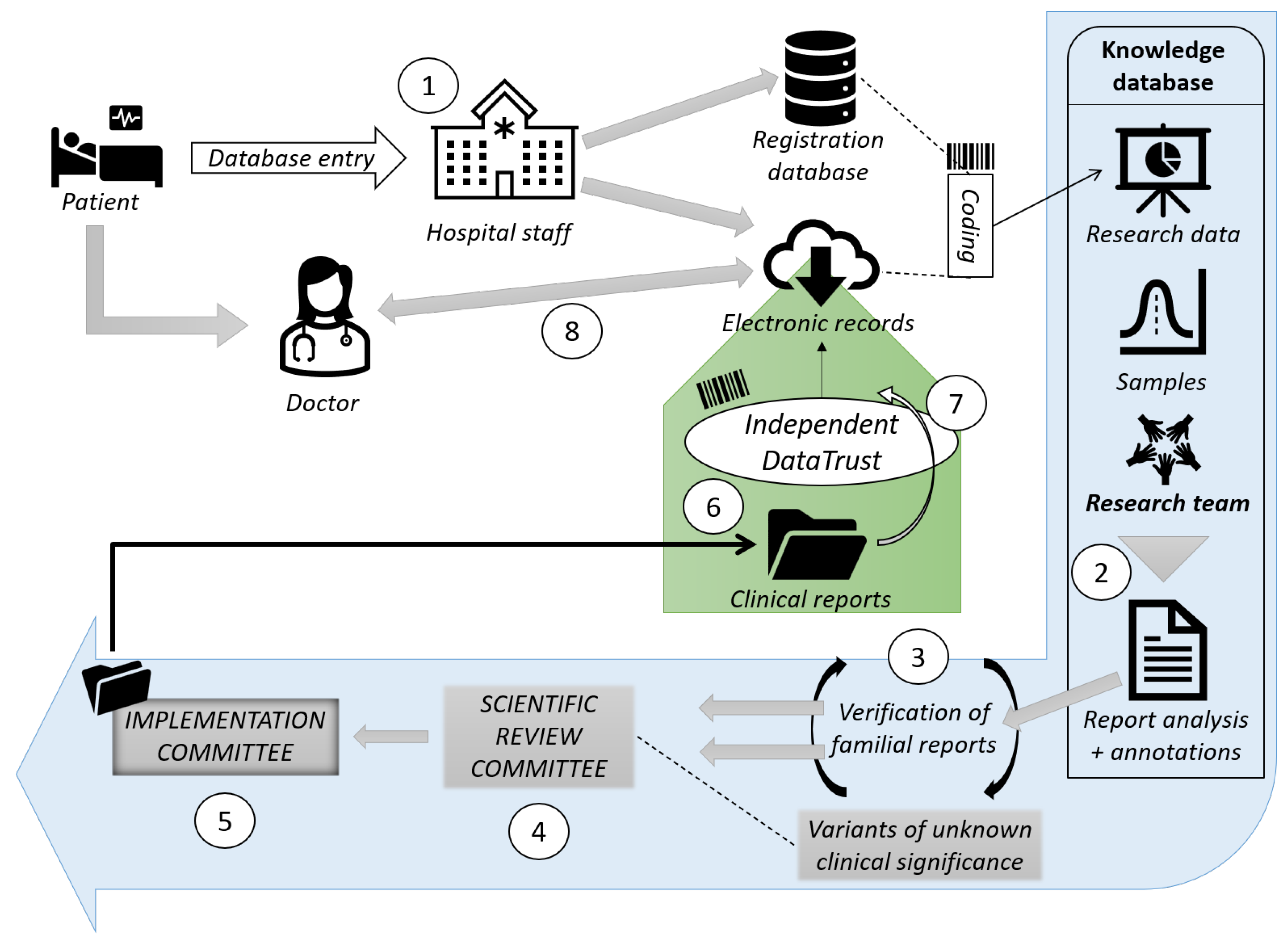
6. Artificial Intelligence Frameworks
7. Artificial Intelligence vs. Antibiotic Stewardship Program
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ahmed, I.; Rabbi, M.B.; Sultana, S. Antibiotic resistance in Bangladesh: A systematic review. Int. J. Infect. Dis. 2019, 80, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Bilal, H.; Khan, M.N.; Rehman, T.; Hameed, M.F.; Yang, X. Antibiotic resistance in Pakistan: A systematic review of past decade. BMC Infect. Dis. 2021, 21, 244. [Google Scholar] [CrossRef]
- Bullens, M.; de Cerqueira Melo, A.; Raziq, S.; Lee, J.; Khalid, G.; Khan, S.; Zada, A.; Wailly, Y.; Zeshan, S.; Saad, N. Antibiotic resistance in patients with urinary tract infections in Pakistan. Public Health Action 2022, 12, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Hormozi, S.F.; Vasei, N.; Aminianfar, M.; Darvishi, M.; Saeedi, A.A. Antibiotic resistance in patients suffering from nosocomial infections in Besat Hospital. Eur. J. Transl. Myol. 2018, 28, 7594. [Google Scholar] [CrossRef] [PubMed]
- Susmita, R.C.; Zubayed, A.; Krishna, R.; Abdullah, A.N.; Rashid, M.H.; Kamol, C.M. Emerging threats of antibiotic resistance in Salmonella typhi and Salmonella paratyphi A among enteric fever cases of Dhaka, Bangladesh. Afr. J. Bacteriol. Res. 2022, 14, 8–15. [Google Scholar]
- Martino, F.; Tijet, N.; Melano, R.; Petroni, A.; Heinz, E.; De Belder, D.; Faccone, D.; Rapoport, M.; Biondi, E.; Rodrigo, V. Isolation of five Enterobacteriaceae species harbouring bla NDM-1 and mcr-1 plasmids from a single paediatric patient. PLoS ONE 2019, 14, e0221960. [Google Scholar]
- Gemert, T.V. On the Influence of Dataset Characteristics on Classifier Performance. Bachelor’s Thesis, Utrecht University, Utrecht, The Netherlands, 2017. [Google Scholar]
- Ahmed, N.; Zeshan, B.; Naveed, M.; Afzal, M.; Mohamed, M. Antibiotic resistance profile in relation to virulence genes fimH, hlyA and usp of uropathogenic E. coli isolates in Lahore, Pakistan. Trop. Biomed. 2019, 36, 559–568. [Google Scholar]
- Lv, J.; Deng, S.; Zhang, L. A review of artificial intelligence applications for antimicrobial resistance. Biosaf. Health 2021, 3, 22–31. [Google Scholar] [CrossRef]
- Lau, H.J.; Lim, C.H.; Foo, S.C.; Tan, H.S. The role of artificial intelligence in the battle against antimicrobial-resistant bacteria. Curr. Genet. 2021, 67, 421–429. [Google Scholar] [CrossRef]
- Raisch, S.; Krakowski, S. Artificial intelligence and management: The automation–augmentation paradox. Acad. Manag. Rev. 2021, 46, 192–210. [Google Scholar] [CrossRef]
- Song, L.; Gildea, D.; Zhang, Y.; Wang, Z.; Su, J. Semantic neural machine translation using AMR. Trans. Assoc. Comput. Linguist. 2019, 7, 19–31. [Google Scholar] [CrossRef]
- Ahmed, N.; Khan, M.; Saleem, W.; Karobari, M.I.; Mohamed, R.N.; Heboyan, A.; Rabaan, A.A.; Mutair, A.A.; Alhumaid, S.; Alsadiq, S.A. Evaluation of bi-lateral co-infections and antibiotic resistance rates among COVID-19 patients. Antibiotics 2022, 11, 276. [Google Scholar] [CrossRef] [PubMed]
- Zhen, X.; Lundborg, C.S.; Sun, X.; Hu, X.; Dong, H. Economic burden of antibiotic resistance in ESKAPE organisms: A systematic review. Antimicrob. Resist. Infect. Control 2019, 8, 137. [Google Scholar] [CrossRef] [PubMed]
- Sattar, H.; Toleman, M.; Nahid, F.; Zahra, R. Co-existence of bla NDM-1 and bla KPC-2 in clinical isolates of Klebsiella pneumoniae from Pakistan. J. Chemother. 2016, 28, 346–349. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.A.; Wyner, S.N. Antimicrobial Resistance: Facing the Rise of a Global Threat; American Public Health Association: Washington, DC, USA, 2019. [Google Scholar]
- Hadjadj, L.; Syed, M.A.; Bushra, J.; Abbasi, S.A.; Rolain, J.-M. Emergence of Vancomycin-resistant Enterococcus faecium ST 80 in Pakistan. Surg. Infect. 2019, 20, 524–525. [Google Scholar] [CrossRef]
- Dantas, G.; Sommer, M.O.; Oluwasegun, R.D.; Church, G.M. Bacteria subsisting on antibiotics. Science 2008, 320, 100–103. [Google Scholar] [CrossRef]
- Sohail, M.; Khurshid, M.; Saleem, H.G.M.; Javed, H.; Khan, A.A. Characteristics and antibiotic resistance of urinary tract pathogens isolated from Punjab, Pakistan. Jundishapur J. Microbiol. 2015, 8, e19272. [Google Scholar] [CrossRef]
- Fasih, N.; Zafar, A.; Khan, E.; Jabeen, K.; Hasan, R. Clonal dissemination of vanA positive Enterococcus species in tertiary care hospitals in Karachi, Pakistan. J. Pak. Med. Assoc. 2010, 60, 805. [Google Scholar]
- Miller, J.R.; Dunham, S.; Mochalkin, I.; Banotai, C.; Bowman, M.; Buist, S.; Dunkle, B.; Hanna, D.; Harwood, H.J.; Huband, M.D. A class of selective antibacterials derived from a protein kinase inhibitor pharmacophore. Proc. Natl. Acad. Sci. USA 2009, 106, 1737–1742. [Google Scholar] [CrossRef]
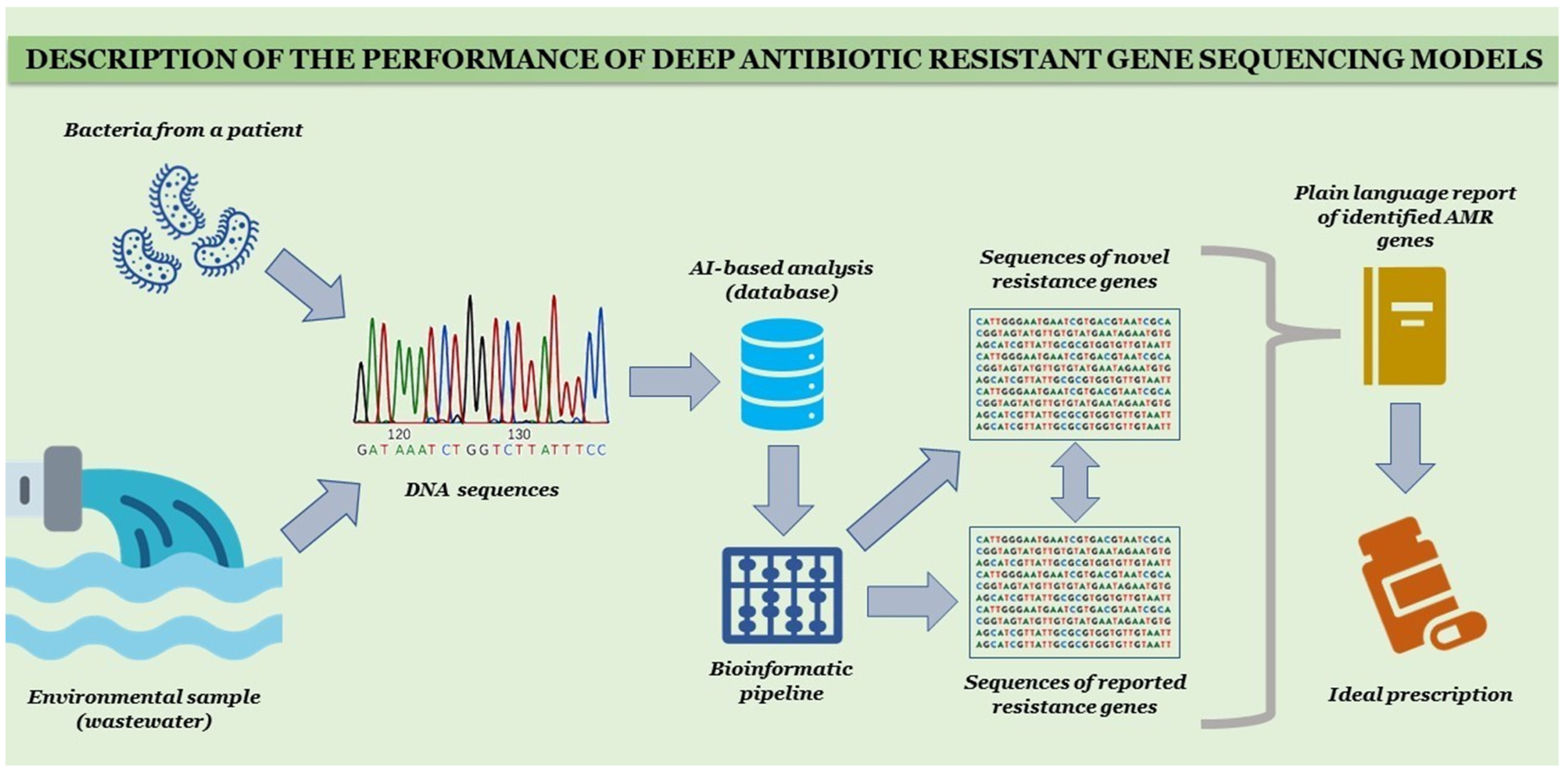
- Arango-Argoty, G.; Garner, E.; Pruden, A.; Heath, L.S.; Vikesland, P.; Zhang, L. DeepARG: A deep learning approach for predicting antibiotic resistance genes from metagenomic data. Microbiome 2018, 6, 23. [Google Scholar] [CrossRef]
- Cánovas-Segura, B.; Campos, M.; Morales, A.; Juarez, J.M.; Palacios, F. Development of a clinical decision support system for antibiotic management in a hospital environment. Prog. Artif. Intell. 2016, 5, 181–197. [Google Scholar] [CrossRef]
- Ahmed, N.; Ali, Z.; Riaz, M.; Zeshan, B.; Wattoo, J.I.; Aslam, M.N. Evaluation of antibiotic resistance and virulence genes among clinical isolates of Pseudomonas aeruginosa from cancer patients. Asian Pac. J. Cancer Prev. APJCP 2020, 21, 1333. [Google Scholar] [CrossRef] [PubMed]
- Zafar, A.; Hasan, R.; Nizami, S.Q.; von Seidlein, L.; Soofi, S.; Ahsan, T.; Chandio, S.; Habib, A.; Bhutto, N.; Siddiqui, F.J. Frequency of isolation of various subtypes and antimicrobial resistance of Shigella from urban slums of Karachi, Pakistan. Int. J. Infect. Dis. 2009, 13, 668–672. [Google Scholar] [CrossRef] [PubMed]
- Nava Lara, R.A.; Aguilera-Mendoza, L.; Brizuela, C.A.; Peña, A.; Del Rio, G. Heterologous machine learning for the identification of antimicrobial activity in Human-Targeted drugs. Molecules 2019, 24, 1258. [Google Scholar] [CrossRef]
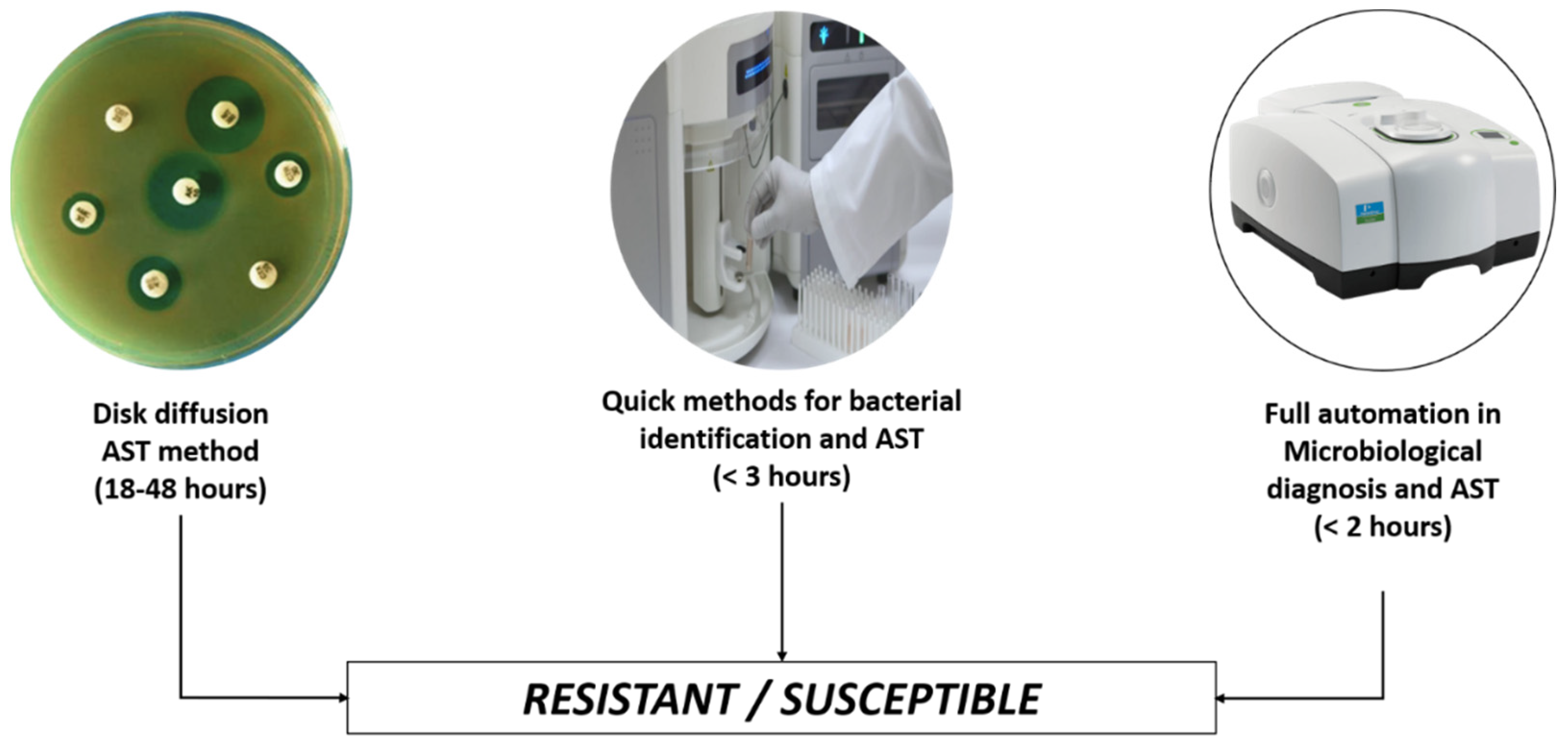
- van Belkum, A.; Burnham, C.-A.D.; Rossen, J.W.; Mallard, F.; Rochas, O.; Dunne, W.M. Innovative and rapid antimicrobial susceptibility testing systems. Nat. Rev. Microbiol. 2020, 18, 299–311. [Google Scholar] [CrossRef] [PubMed]
- Gajdács, M.; Paulik, E.; Szabó, A. Knowledge, attitude and practice of community pharmacists regarding antibiotic use and infectious diseases: A cross-sectional survey in Hungary (KAPPhA-HU). Antibiotics 2020, 9, 41. [Google Scholar] [CrossRef]
- Yelin, I.; Snitser, O.; Novich, G.; Katz, R.; Tal, O.; Parizade, M.; Chodick, G.; Koren, G.; Shalev, V.; Kishony, R. Personal clinical history predicts antibiotic resistance of urinary tract infections. Nat. Med. 2019, 25, 1143–1152. [Google Scholar] [CrossRef]
- Parveen, S.; Saqib, S.; Ahmed, A.; Shahzad, A.; Ahmed, N. Prevalence of MRSA colonization among healthcare-workers and effectiveness of decolonization regimen in ICU of a Tertiary care Hospital, Lahore, Pakistan. Adv. Life Sci. 2020, 8, 38–41. [Google Scholar]
- Zeshan, B.; Karobari, M.I.; Afzal, N.; Siddiq, A.; Basha, S.; Basheer, S.N.; Peeran, S.W.; Mustafa, M.; Daud, N.H.A.; Ahmed, N. The usage of antibiotics by COVID-19 patients with comorbidities: The risk of increased antimicrobial resistance. Antibiotics 2021, 11, 35. [Google Scholar] [CrossRef]
- Melo, M.C.; Maasch, J.R.; de la Fuente-Nunez, C. Accelerating antibiotic discovery through artificial intelligence. Commun. Biol. 2021, 4, 1050. [Google Scholar] [CrossRef]
- Pakistan Antimicrobial Resistance Network (PARN). Available online: https://parn.org.pk/antimicrobial-data/ (accessed on 20 May 2022).
- Ahmed, Z.; Bhinder, K.K.; Tariq, A.; Tahir, M.J.; Mehmood, Q.; Tabassum, M.S.; Malik, M.; Aslam, S.; Asghar, M.S.; Yousaf, Z. Knowledge, attitude, and practice of artificial intelligence among doctors and medical students in Pakistan: A cross-sectional online survey. Ann. Med. Surg. 2022, 76, 103493. [Google Scholar] [CrossRef] [PubMed]
- Rasheed, M.A.; Chand, P.; Ahmed, S.; Sharif, H.; Hoodbhoy, Z.; Siddiqui, A.; Hasan, B.S. Use of artificial intelligence on Electroencephalogram (EEG) waveforms to predict failure in early school grades in children from a rural cohort in Pakistan. PLoS ONE 2021, 16, e0246236. [Google Scholar] [CrossRef]
- Kazi, A.M.; Qazi, S.A.; Khawaja, S.; Ahsan, N.; Ahmed, R.M.; Sameen, F.; Mughal, M.A.K.; Saqib, M.; Ali, S.; Kaleemuddin, H. An artificial intelligence–based, personalized smartphone app to improve childhood immunization coverage and timelines among children in Pakistan: Protocol for a randomized controlled trial. JMIR Res. Protoc. 2020, 9, e22996. [Google Scholar] [CrossRef] [PubMed]
- Dahri, A.S.; Al-Athwari, A.; Hussain, A. Usability evaluation of mobile health application from AI perspective in rural areas of Pakistan. Int. Assoc. Online Eng. 2019. Available online: https://www.learntechlib.org/p/216620/ (accessed on 22 May 2022).
- Khan, A.U.; Melzer, F.; Hendam, A.; Sayour, A.E.; Khan, I.; Elschner, M.C.; Younus, M.; Ehtisham-ul-Haque, S.; Waheed, U.; Farooq, M. Seroprevalence and Molecular Identification of Brucella spp. in Bovines in Pakistan—Investigating Association with Risk Factors Using Machine Learning. Front. Vet. Sci. 2020, 7, 980. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Mehran, M.T.; Haq, Z.U.; Ullah, Z.; Naqvi, S.R.; Ihsan, M.; Abbass, H. Applications of artificial intelligence in COVID-19 pandemic: A comprehensive review. Expert Syst. Appl. 2021, 185, 115695. [Google Scholar] [CrossRef]
- Elyan, E.; Hussain, A.; Sheikh, A.; Elmanama, A.A.; Vuttpittayamongkol, P.; Hijazi, K. Antimicrobial Resistance and Machine Learning: Challenges and Opportunities. IEEE Access 2022, 10, 31561–31577. [Google Scholar] [CrossRef]
- Steinkey, R.; Moat, J.; Gannon, V.; Zovoilis, A.; Laing, C. Application of artificial intelligence to the in silico assessment of antimicrobial resistance and risks to human and animal health presented by priority enteric bacterial pathogens. Can. Commun. Dis. Rep. 2020, 46, 180–185. [Google Scholar] [CrossRef]
- Anahtar, M.N.; Yang, J.H.; Kanjilal, S. Applications of machine learning to the problem of antimicrobial resistance: An emerging model for translational research. J. Clin. Microbiol. 2021, 59, e01260-20. [Google Scholar] [CrossRef]
- Yakar, D.; Ongena, Y.P.; Kwee, T.C.; Haan, M. Do people favor artificial intelligence over physicians? A survey among the general population and their view on artificial intelligence in medicine. Value Health 2022, 25, 374–381. [Google Scholar] [CrossRef]
- Rawson, T.M.; Ahmad, R.; Toumazou, C.; Georgiou, P.; Holmes, A.H. Artificial intelligence can improve decision-making in infection management. Nat. Hum. Behav. 2019, 3, 543–545. [Google Scholar] [CrossRef] [PubMed]
- Baxi, V.; Edwards, R.; Montalto, M.; Saha, S. Digital pathology and artificial intelligence in translational medicine and clinical practice. Mod. Pathol. 2022, 35, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Wan, X.; Yao, S. Better AMR-to-text generation with graph structure reconstruction. In Proceedings of the Twenty-Ninth International Conference on International Joint Conferences on Artificial Intelligence, Yokohama, Japan, 7–15 January 2021; pp. 3919–3925. [Google Scholar]
- Afshinnekoo, E.; Bhattacharya, C.; Burguete-García, A.; Castro-Nallar, E.; Deng, Y.; Desnues, C.; Dias-Neto, E.; Elhaik, E.; Iraola, G.; Jang, S. COVID-19 drug practices risk antimicrobial resistance evolution. Lancet Microb. 2021, 2, e135–e136. [Google Scholar] [CrossRef]
- Fanelli, U.; Pappalardo, M.; Chinè, V.; Gismondi, P.; Neglia, C.; Argentiero, A.; Calderaro, A.; Prati, A.; Esposito, S. Role of artificial intelligence in fighting antimicrobial resistance in pediatrics. Antibiotics 2020, 9, 767. [Google Scholar] [CrossRef]
- Neumann, D.; Mansi, T.; Itu, L.; Georgescu, B.; Kayvanpour, E.; Sedaghat-Hamedani, F.; Amr, A.; Haas, J.; Katus, H.; Meder, B. A self-taught artificial agent for multi-physics computational model personalization. Med. Image Anal. 2016, 34, 52–64. [Google Scholar] [CrossRef][Green Version]
- Van Steenkiste, T.; Ruyssinck, J.; De Baets, L.; Decruyenaere, J.; De Turck, F.; Ongenae, F.; Dhaene, T. Accurate prediction of blood culture outcome in the intensive care unit using long short-term memory neural networks. Artif. Intell. Med. 2019, 97, 38–43. [Google Scholar] [CrossRef]
- Kaji, D.A.; Zech, J.R.; Kim, J.S.; Cho, S.K.; Dangayach, N.S.; Costa, A.B.; Oermann, E.K. An attention based deep learning model of clinical events in the intensive care unit. PLoS ONE 2019, 14, e0211057. [Google Scholar] [CrossRef]
- Smith, K.P.; Wang, H.; Durant, T.J.S.; Mathison, B.A.; Sharp, S.E.; Kirby, J.E.; Long, S.W.; Rhoads, D.D. Applications of Artificial Intelligence in Clinical Microbiology Diagnostic Testing. Clin. Microbiol. Newsl. 2020, 42, 61–70. [Google Scholar] [CrossRef]
- Cartelle Gestal, M.; Dedloff, M.R.; Torres-Sangiao, E. Computational health engineering applied to model infectious diseases and antimicrobial resistance spread. Appl. Sci. 2019, 9, 2486. [Google Scholar] [CrossRef]
- Khaledi, A.; Weimann, A.; Schniederjans, M.; Asgari, E.; Kuo, T.H.; Oliver, A.; Cabot, G.; Kola, A.; Gastmeier, P.; Hogardt, M. Predicting antimicrobial resistance in Pseudomonas aeruginosa with machine learning-enabled molecular diagnostics. EMBO Mol. Med. 2020, 12, e10264. [Google Scholar] [CrossRef]
- Luz, C.F.; van Niekerk, J.M.; Keizer, J.; Beerlage-de Jong, N.; Braakman-Jansen, L.A.; Stein, A.; Sinha, B.; van Gemert-Pijnen, J.; Glasner, C. Mapping twenty years of antimicrobial resistance research trends. Artif. Intell. Med. 2022, 123, 102216. [Google Scholar] [CrossRef] [PubMed]
- Agnello, S.; Brand, M.; Chellat, M.F.; Gazzola, S.; Riedl, R. A structural view on medicinal chemistry strategies against drug resistance. Angew. Chem. Int. Ed. 2019, 58, 3300–3345. [Google Scholar] [CrossRef]
- Kayid, A. The Role of Artificial Intelligence in Future Technology; Academic Press: Cambridge, MA, USA, 2020. [Google Scholar] [CrossRef]
- VanOeffelen, M.; Nguyen, M.; Aytan-Aktug, D.; Brettin, T.; Dietrich, E.M.; Kenyon, R.W.; Machi, D.; Mao, C.; Olson, R.; Pusch, G.D. A genomic data resource for predicting antimicrobial resistance from laboratory-derived antimicrobial susceptibility phenotypes. Brief. Bioinform. 2021, 22, bbab313. [Google Scholar] [CrossRef] [PubMed]
- Macesic, N.; Polubriaginof, F.; Tatonetti, N.P. Machine learning: Novel bioinformatics approaches for combating antimicrobial resistance. Curr. Opin. Infect. Dis. 2017, 30, 511–517. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Agüero, S.; Mora-Jiménez, I.; Lérida-García, J.; Álvarez-Rodríguez, J.; Soguero-Ruiz, C. Machine learning techniques to identify antimicrobial resistance in the intensive care unit. Entropy 2019, 21, 603. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-González, A.; Zanin, M.; Menasalvas-Ruiz, E. Public health and epidemiology informatics: Can artificial intelligence help future global challenges? An overview of antimicrobial resistance and impact of climate change in disease epidemiology. Yearb. Med. Inform. 2019, 28, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Santerre, J.W.; Davis, J.J.; Xia, F.; Stevens, R. Machine learning for antimicrobial resistance. arXiv 2016, arXiv:1607.01224. [Google Scholar]
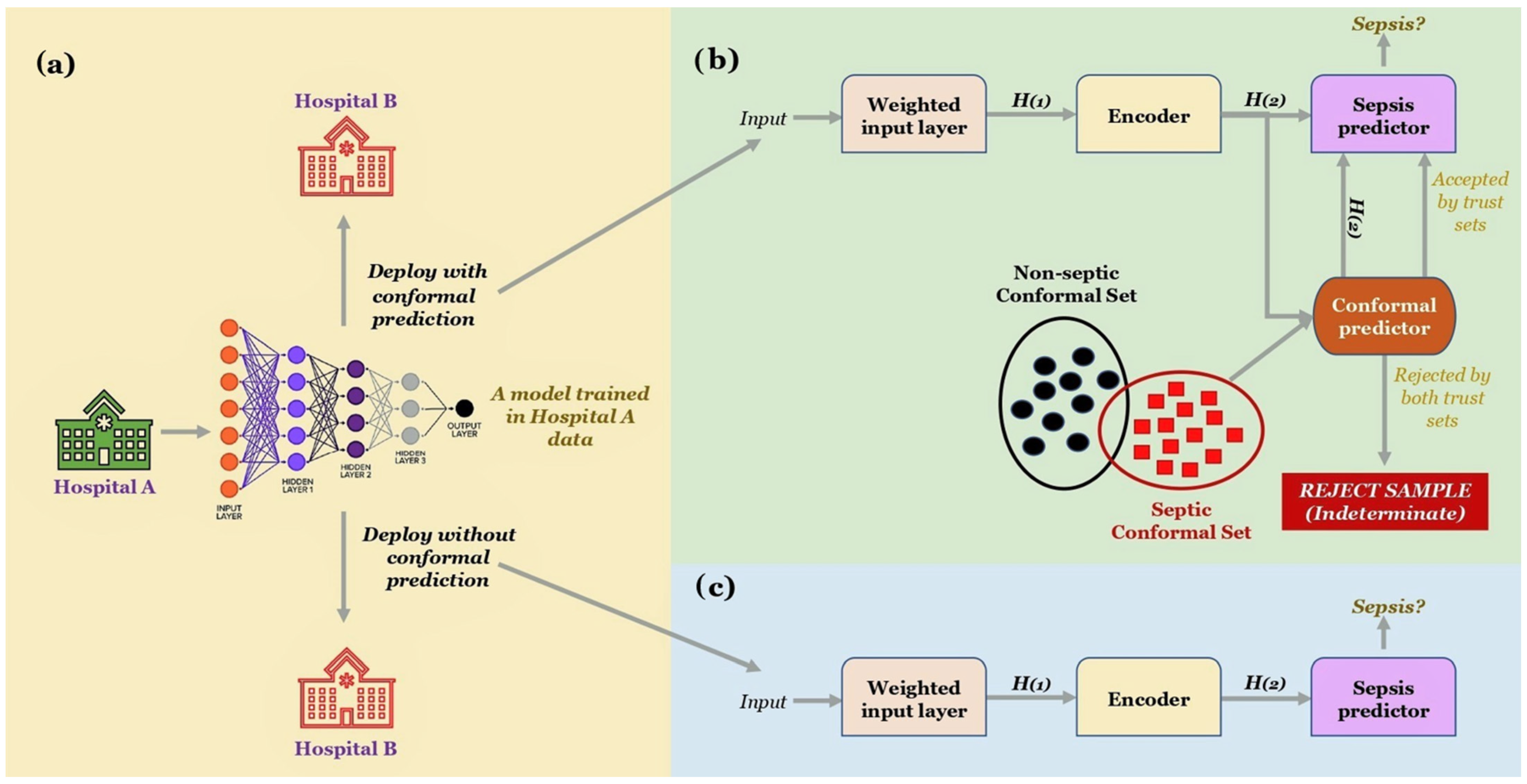
- Shashikumar, S.P.; Wardi, G.; Malhotra, A.; Nemati, S. Artificial intelligence sepsis prediction algorithm learns to say “I don’t know”. NPJ Digit. Med. 2021, 4, 134. [Google Scholar] [CrossRef]
- Feretzakis, G.; Sakagianni, A.; Loupelis, E.; Kalles, D.; Skarmoutsou, N.; Martsoukou, M.; Christopoulos, C.; Lada, M.; Petropoulou, S.; Velentza, A. Machine Learning for Antibiotic Resistance Prediction: A Prototype Using Off-the-Shelf Techniques and Entry-Level Data to Guide Empiric Antimicrobial Therapy. Healthc. Inform. Res. 2021, 27, 214–221. [Google Scholar] [CrossRef]
- Hameed, F.; Khan, M.A.; Muhammad, H.; Sarwar, T.; Bilal, H.; Rehman, T.U. Plasmid-mediated mcr-1 gene in Acinetobacter baumannii and Pseudomonas aeruginosa: First report from Pakistan. Rev. Soc. Bras. Med. Trop. 2019, 52, e20190237. [Google Scholar] [CrossRef]
- Pal, C.; Bengtsson-Palme, J.; Kristiansson, E.; Larsson, D.J. The structure and diversity of human, animal and environmental resistomes. Microbiome 2016, 4, 1–15. [Google Scholar] [CrossRef]
- Ahmed, N.; Khalid, H.; Mushtaq, M.; Basha, S.; Rabaan, A.A.; Garout, M.; Halwani, M.A.; Al Mutair, A.; Alhumaid, S.; Al Alawi, Z.; et al. The Molecular Characterization of Virulence Determinants and Antibiotic Resistance Patterns in Human Bacterial Uropathogens. Antibiotics 2022, 11, 516. [Google Scholar] [CrossRef] [PubMed]
- Zahra, N.; Zeshan, B.; Qadri, M.M.A.; Ishaq, M.; Afzal, M.; Ahmed, N. Phenotypic and Genotypic Evaluation of Antibiotic Resistance of Acinetobacter baumannii Bacteria Isolated from Surgical Intensive Care Unit Patients in Pakistan. Jundishapur J. Microbiol. 2021, 14, 104922. [Google Scholar] [CrossRef]
- Saleem, Z.; Godman, B.; Azhar, F.; Kalungia, A.C.; Fadare, J.; Opanga, S.; Markovic-Pekovic, V.; Hoxha, I.; Saeed, A.; Al-Gethamy, M. Progress on the national action plan of Pakistan on antimicrobial resistance (AMR): A narrative review and the implications. Expert Rev. Anti-Infect. Ther. 2022, 20, 71–93. [Google Scholar] [CrossRef] [PubMed]
- Oluwafemi, R.; Olawale, I.; Alagbe, J. Recent trends in the utilization of medicinal plants as growth promoters in poultry nutrition—A review. Res. Agric. Vet. Sci. 2020, 4, 5–11. [Google Scholar]
| AI Applications for AMR | Concepts | Advantages | Drawbacks |
|---|---|---|---|
| AI health industry and antibiotics | |||
| Antimicrobial peptides | A natural class of small host defense peptides, found in all classes of biological species. |
|
|
| New antibiotics | Discovery of new and structurally different antibiotics from the ones already known using AI. |
|
|
| AI, infectious diseases, and pediatric practices | |||
| Appropriate antibiotic prescription | Appropriate therapy selection, dose, and correct administration route |
|
|
| Prediction of antibiotic resistance | ML techniques to predict early AMR or the probability of a microbial agent becoming resistant |
|
|
| The severity of infection prediction | Machine/deep learning tools for infectious pathology recognition and appropriate management |
|
|
| Algorithm | Description | Advantages | Disadvantages | Learning Speed | Interpretability |
|---|---|---|---|---|---|
| NB (Naïve Bayes) | Based on the Bayes theorem, a family of algorithms working on the principle of independent classification of each pair of features | Easily implemented, fast, suitable for missing value datasets | Independent features only | 5 | 2 |
| RF (Random Forest) | Solely based on decision trees’ predictions; takes the mean value of various trees’ outputs; precision increases with increasing no. of trees | Effective for large datasets, multi-feature handling | Insensitive to outlier information | 2 | 3 |
| ANN (Artificial Neuron Network) | Imitates the working of nerve cells in humans; makes independent judgments on new input based on learning | Multiple layer perceptron, higher accuracy with model depth | Speed of learning lowers with increasing model depth | 1 | 1 |
| SVM (Support Vector Machine) | Supervised algorithm for regression & classification; locates a hyperplane to classify data points in the N-dimensional space | Utility of kernel functions | Slow, requires specification of multiple parameters | 1 | 1 |
| DT (Decision Tree) | Prediction based on targeted variable; leaf nodes equal class label, internal node equals attributes | Easily interpreted, work with missing values in the dataset | May not work on missing data if the tree is too complex | 4 | 5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rabaan, A.A.; Alhumaid, S.; Mutair, A.A.; Garout, M.; Abulhamayel, Y.; Halwani, M.A.; Alestad, J.H.; Bshabshe, A.A.; Sulaiman, T.; AlFonaisan, M.K.; et al. Application of Artificial Intelligence in Combating High Antimicrobial Resistance Rates. Antibiotics 2022, 11, 784. https://doi.org/10.3390/antibiotics11060784
Rabaan AA, Alhumaid S, Mutair AA, Garout M, Abulhamayel Y, Halwani MA, Alestad JH, Bshabshe AA, Sulaiman T, AlFonaisan MK, et al. Application of Artificial Intelligence in Combating High Antimicrobial Resistance Rates. Antibiotics. 2022; 11(6):784. https://doi.org/10.3390/antibiotics11060784
Chicago/Turabian StyleRabaan, Ali A., Saad Alhumaid, Abbas Al Mutair, Mohammed Garout, Yem Abulhamayel, Muhammad A. Halwani, Jeehan H. Alestad, Ali Al Bshabshe, Tarek Sulaiman, Meshal K. AlFonaisan, and et al. 2022. "Application of Artificial Intelligence in Combating High Antimicrobial Resistance Rates" Antibiotics 11, no. 6: 784. https://doi.org/10.3390/antibiotics11060784
APA StyleRabaan, A. A., Alhumaid, S., Mutair, A. A., Garout, M., Abulhamayel, Y., Halwani, M. A., Alestad, J. H., Bshabshe, A. A., Sulaiman, T., AlFonaisan, M. K., Almusawi, T., Albayat, H., Alsaeed, M., Alfaresi, M., Alotaibi, S., Alhashem, Y. N., Temsah, M.-H., Ali, U., & Ahmed, N. (2022). Application of Artificial Intelligence in Combating High Antimicrobial Resistance Rates. Antibiotics, 11(6), 784. https://doi.org/10.3390/antibiotics11060784










