Clinical Efficacy and Safety of Vancomycin Continuous Infusion in Patients Treated at Home in an Outpatient Parenteral Antimicrobial Therapy Program
Abstract
1. Introduction
2. Materials and Methods
2.1. Design, Setting and Study Participants
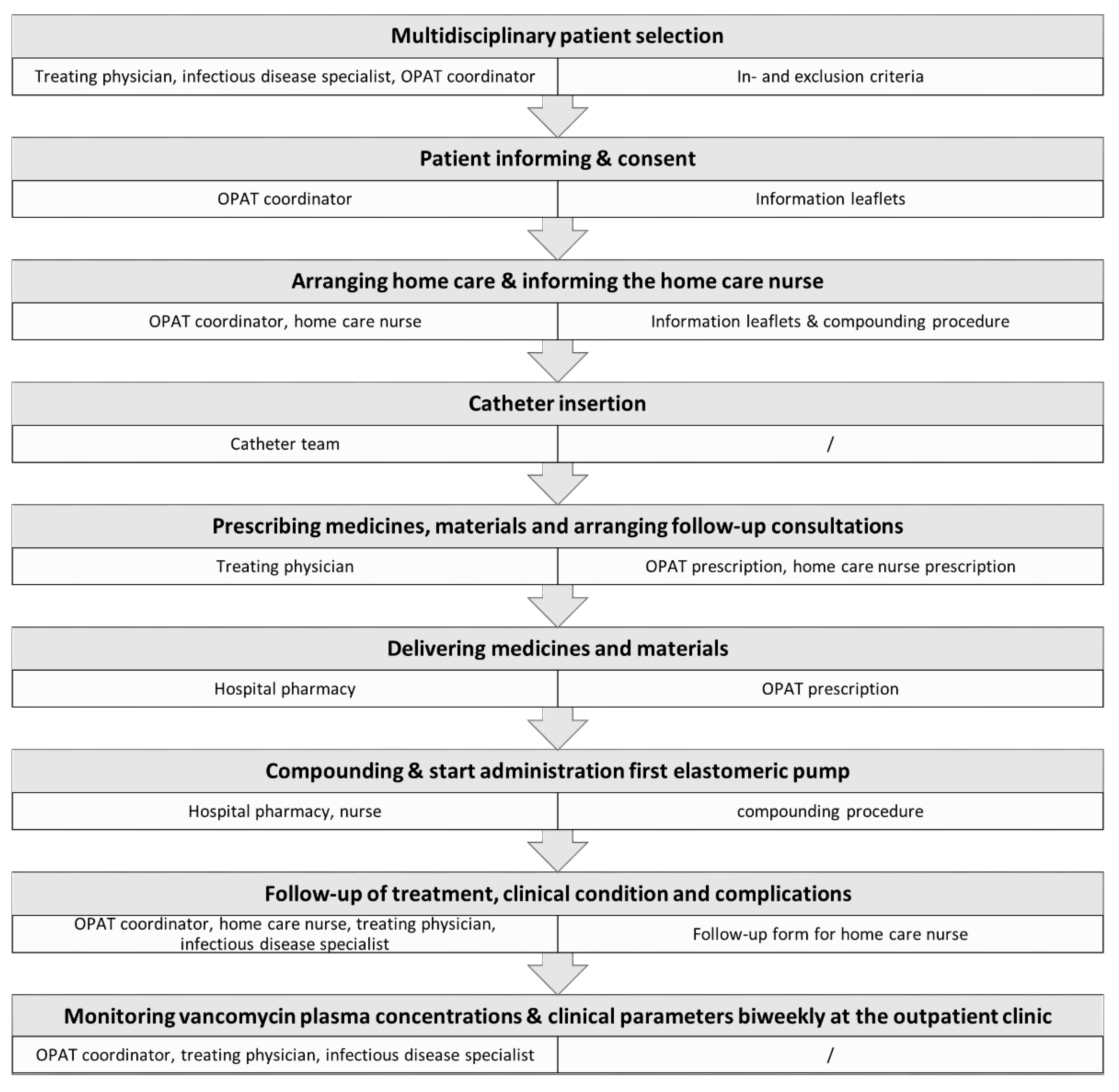
2.2. Organization of the vOPAT Care Path within a Structured Program
2.3. Data Collection and Analysis
3. Results
3.1. Demographics
3.2. Medical Discipline, Clinical Indication and Causative Pathogen
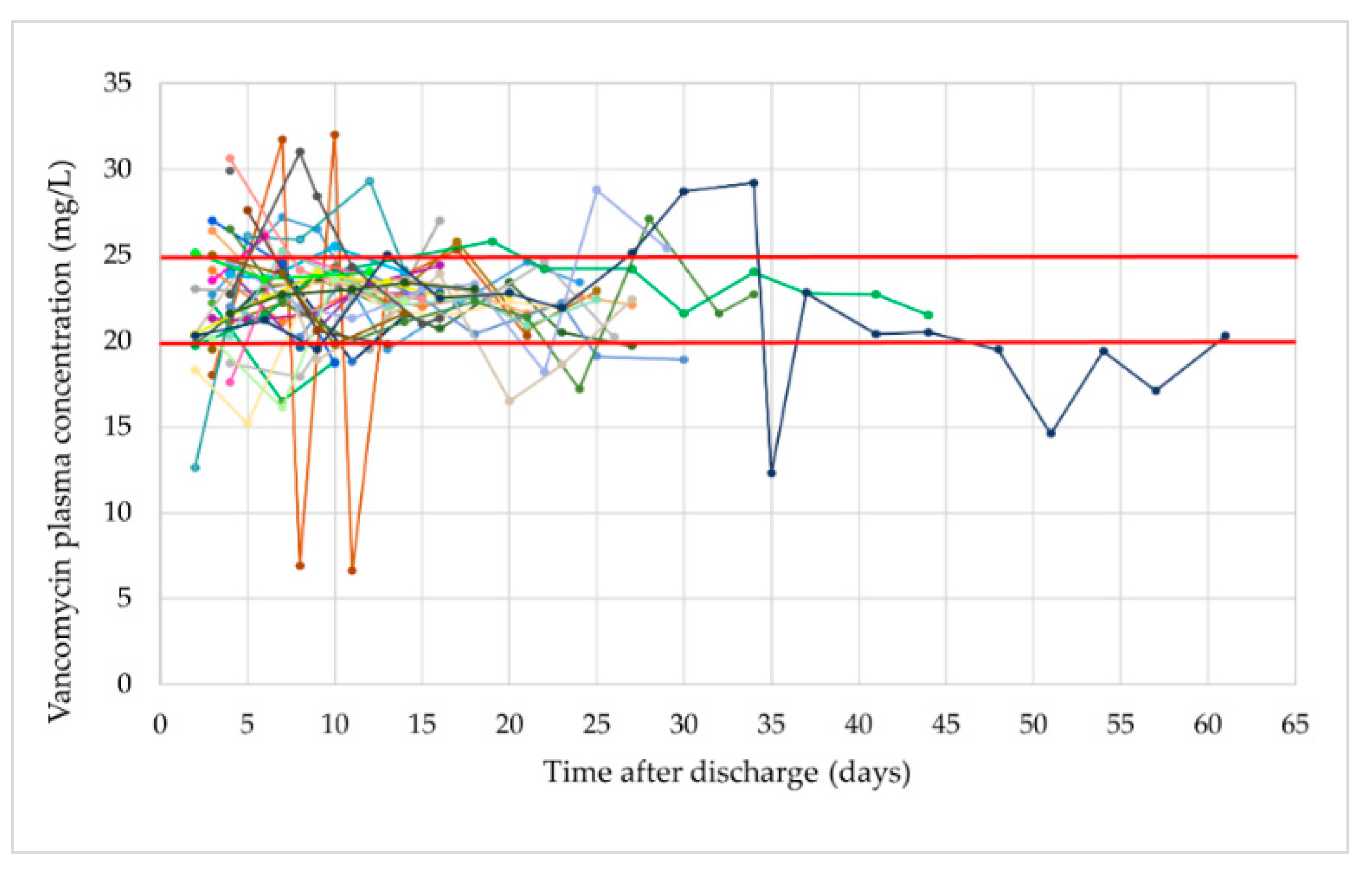
3.3. Vancomycin Administration, Target Attainment and Adherence to Dose Adjustment Protocol
3.4. Treatment Duration, Length of Hospital Stay and Avoided Hospitalization Days
3.5. Clinical Outcome, Adverse Events and Hospital Readmissions
3.6. Patients’ Satisfaction and Experience
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Voumard, R.; Gardiol, C.; André, P.; Arensdorff, L.; Cochet, C.; Boillat-Blanco, N.; Decosterd, L.; Buclin, T.; de Vallière, S. Efficacy and safety of continuous infusions with elastomeric pumps for outpatient parenteral antimicrobial therapy (OPAT): An observational study. J. Antimicrob. Chemother. 2018, 73, 2540–2545. [Google Scholar] [CrossRef]
- Diamantis, S.; Dawudi, Y.; Cassard, B.; Longuet, P.; Lesprit, P.; Gauzit, R. Home intravenous antibiotherapy and the proper use of elastomeric pumps: Systematic review of the literature and proposals for improved use. Infect. Dis. Now 2021, 51, 39–49. [Google Scholar] [CrossRef]
- Grattan, K.S.; Mohamed Ali, M.; Hosseini-Moghaddam, S.M.; Gilmour, H.J.I.; Crunican, G.P.; Hua, E.; Muhsin, K.A.; Johnstone, R.; Bondy, L.C.; Devlin, M.K.; et al. Evaluating the safety and effectiveness of a nurse-led outpatient virtual IV vancomycin monitoring clinic: A retrospective cohort study. JAC Antimicrob. Resist. 2021, 3, dlaa113. [Google Scholar] [CrossRef]
- Douiyeb, S.; de la Court, J.R.; Tuinte, B.; Sombogaard, F.; Schade, R.P.; Kuijvenhoven, M.; Minderhoud, T.; Sigaloff, K.C.E. Risk factors for readmission among patients receiving outpatient parenteral antimicrobial therapy: A retrospective cohort study. Int. J. Clin. Pharm. 2022, 44, 557–563. [Google Scholar] [CrossRef]
- Leggett, J.E. Ambulatory use of parenteral antibacterials: Contemporary perspectives. Drugs 2000, 59 (Suppl. 3), 1–8, discussion 47–49. [Google Scholar] [CrossRef]
- Álvarez, R.; López Cortés, L.E.; Molina, J.; Cisneros, J.M.; Pachón, J. Optimizing the Clinical Use of Vancomycin. Antimicrob. Agents Chemother. 2016, 60, 2601–2609. [Google Scholar] [CrossRef]
- Fraser, T.G.; Stosor, V.; Wang, Q.; Allen, A.; Zembower, T.R. Vancomycin and home health care. Emerg. Infect. Dis. 2005, 11, 1558–1564. [Google Scholar] [CrossRef]
- Patel, S.; Preuss, C.V.; Bernice, F. Vancomycin. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2022. [Google Scholar]
- Depypere, M.; Morgenstern, M.; Kuehl, R.; Senneville, E.; Moriarty, T.F.; Obremskey, W.T.; Zimmerli, W.; Trampuz, A.; Lagrou, K.; Metsemakers, W.J. Pathogenesis and management of fracture-related infection. Clin. Microbiol. Infect. 2020, 26, 572–578. [Google Scholar] [CrossRef]
- Mackintosh, C.L.; White, H.A.; Seaton, R.A. Outpatient parenteral antibiotic therapy (OPAT) for bone and joint infections: Experience from a UK teaching hospital-based service. J. Antimicrob. Chemother. 2011, 66, 408–415. [Google Scholar] [CrossRef]
- Bernard, L.; El-Hajj; Pron, B.; Lotthé, A.; Gleizes, V.; Signoret, F.; Denormandie, P.; Gaillard, J.L.; Perronne, C. Outpatient parenteral antimicrobial therapy (OPAT) for the treatment of osteomyelitis: Evaluation of efficacy, tolerance and cost. J. Clin. Pharm. Ther. 2001, 26, 445–451. [Google Scholar] [CrossRef]
- Le Vavasseur, B.; Zeller, V. Antibiotic Therapy for Prosthetic Joint Infections: An Overview. Antibiotics 2022, 11, 486. [Google Scholar] [CrossRef]
- Cassettari, V.; Novato, N.; Onuchic, M.H.F. Antimicrobial stewardship in the outpatient parenteral antimicrobial therapy (OPAT) setting: The impact of prescription assessment by an infectious diseases specialist. Braz. J. Infect. Dis. 2021, 25, 101560. [Google Scholar] [CrossRef]
- García-Queiruga, M.; Feal Cortizas, B.; Lamelo Alfonsín, F.; Pertega Diaz, S.; Martín-Herranz, I. Continuous infusion of antibiotics using elastomeric pumps in the hospital at home setting. Rev. Esp. Quimioter. 2021, 34, 200–206. [Google Scholar] [CrossRef]
- Norris, A.H.; Shrestha, N.K.; Allison, G.M.; Keller, S.C.; Bhavan, K.P.; Zurlo, J.J.; Hersh, A.L.; Gorski, L.A.; Bosso, J.A.; Rathore, M.H.; et al. 2018 Infectious Diseases Society of America Clinical Practice Guideline for the Management of Outpatient Parenteral Antimicrobial Therapy. Clin. Infect. Dis. 2019, 68, e1–e35. [Google Scholar] [CrossRef]
- Rybak, M.J.; Le, J.; Lodise, T.; Levine, D.; Bradley, J.; Liu, C.; Mueller, B.; Pai, M.; Wong-Beringer, A.; Rotschafer, J.C.; et al. Executive Summary: Therapeutic Monitoring of Vancomycin for Serious Methicillin-Resistant Staphylococcus aureus Infections: A Revised Consensus Guideline and Review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists. J. Pediatric Infect. Dis. Soc. 2020, 9, 281–284. [Google Scholar] [CrossRef]
- Shah, A.; Norris, A. OPAT eHandbook: CRG Publishing and Infectious Diseases Society of America. 2016. Available online: https://www.idsociety.org/opat-ehandbook/ (accessed on 4 April 2022).
- Keller, S.C.; Williams, D.; Gavgani, M.; Hirsch, D.; Adamovich, J.; Hohl, D.; Gurses, A.P.; Cosgrove, S.E. Rates of and Risk Factors for Adverse Drug Events in Outpatient Parenteral Antimicrobial Therapy. Clin. Infect. Dis. 2018, 66, 11–19. [Google Scholar] [CrossRef]
- Huang, V.; Ruhe, J.J.; Lerner, P.; Fedorenko, M. Risk factors for readmission in patients discharged with outpatient parenteral antimicrobial therapy: A retrospective cohort study. BMC Pharmacol. Toxicol. 2018, 19, 50. [Google Scholar] [CrossRef]
- Shah, P.J.; Bergman, S.J.; Graham, D.R.; Glenn, S. Monitoring of Outpatient Parenteral Antimicrobial Therapy and Implementation of Clinical Pharmacy Services at a Community Hospital Infusion Unit. J. Pharm. Pract. 2015, 28, 462–468. [Google Scholar] [CrossRef]
- Quintens, C.; Steffens, E.; Jacobs, K.; Schuermans, A.; Van Eldere, J.; Lagrou, K.; De Munter, P.; Derdelinckx, I.; Peetermans, W.E.; Spriet, I. Efficacy and safety of a Belgian tertiary care outpatient parenteral antimicrobial therapy (OPAT) program. Infection 2020, 48, 357–366. [Google Scholar] [CrossRef]
- Gijsen, M.; Wilmer, A.; Meyfroidt, G.; Wauters, J.; Spriet, I. Can augmented renal clearance be detected using estimators of glomerular filtration rate? Crit. Care 2020, 24, 359. [Google Scholar] [CrossRef]
- Depypere, M.; Kuehl, R.; Metsemakers, W.J.; Senneville, E.; McNally, M.A.; Obremskey, W.T.; Zimmerli, W.; Atkins, B.L.; Trampuz, A.; Group, F.-R.I.F.C. Recommendations for Systemic Antimicrobial Therapy in Fracture-Related Infection: A Consensus From an International Expert Group. J. Orthop. Trauma 2020, 34, 30–41. [Google Scholar] [CrossRef]
- Anemüller, R.; Belden, K.; Brause, B.; Citak, M.; Del Pozo, J.L.; Frommelt, L.; Gehrke, T.; Hewlett, A.; Higuera, C.A.; Hughes, H.; et al. Hip and Knee Section, Treatment, Antimicrobials: Proceedings of International Consensus on Orthopedic Infections. J. Arthroplasty 2019, 34, S463–S475. [Google Scholar] [CrossRef]
- Ingram, P.R.; Lye, D.C.; Fisher, D.A.; Goh, W.P.; Tam, V.H. Nephrotoxicity of continuous versus intermittent infusion of vancomycin in outpatient parenteral antimicrobial therapy. Int. J. Antimicrob. Agents 2009, 34, 570–574. [Google Scholar] [CrossRef]
- Verrall, A.J.; Llorin, R.; Tam, V.H.; Lye, D.C.; Sulaiman, Z.; Zhong, L.; Archuleta, S.; Fisher, D.A. Efficacy of continuous infusion of vancomycin for the outpatient treatment of methicillin-resistant Staphylococcus aureus infections. J. Antimicrob. Chemother. 2012, 67, 2970–2973. [Google Scholar] [CrossRef]
- Shakeraneh, P.; Fazili, T.; Wang, D.; Gilotra, T.; Steele, J.M.; Seabury, R.W.; Miller, C.D.; Darko, W.; Probst, L.A.; Kufel, W.D. Nephrotoxicity Risk and Clinical Effectiveness of Continuous versus Intermittent Infusion Vancomycin Among Patients in an Outpatient Parenteral Antimicrobial Therapy Program. Pharmacotherapy 2020, 40, 357–362. [Google Scholar] [CrossRef]
- Ingram, P.R.; Lye, D.C.; Tambyah, P.A.; Goh, W.P.; Tam, V.H.; Fisher, D.A. Risk factors for nephrotoxicity associated with continuous vancomycin infusion in outpatient parenteral antibiotic therapy. J. Antimicrob. Chemother. 2008, 62, 168–171. [Google Scholar] [CrossRef]
- Norton, K.; Ingram, P.R.; Heath, C.H.; Manning, L. Risk factors for nephrotoxicity in patients receiving outpatient continuous infusions of vancomycin in an Australian tertiary hospital. J. Antimicrob. Chemother. 2014, 69, 805–808. [Google Scholar] [CrossRef][Green Version]
- Krueger, K.M.; LaCloche, L.; Buros Stein, A.; Kates, R.; Murray, M.; Angarone, M.P. Risk Factors Associated With Nephrotoxicity During Outpatient Intravenous Vancomycin Administration. J. Pharm. Technol. 2022, 38, 10–17. [Google Scholar] [CrossRef]
- Tuerff, D.; Nunez, M. More Frequent Premature Antibiotic Discontinuations and Acute Kidney Injury in the Outpatient Setting With Vancomycin Compared to Daptomycin. J. Clin. Pharmacol. 2020, 60, 384–390. [Google Scholar] [CrossRef]
- Spadaro, S.; Berselli, A.; Fogagnolo, A.; Capuzzo, M.; Ragazzi, R.; Marangoni, E.; Bertacchini, S.; Volta, C.A. Evaluation of a protocol for vancomycin administration in critically patients with and without kidney dysfunction. BMC Anesthesiol. 2015, 15, 95. [Google Scholar] [CrossRef]
- Athans, V.; Kenney, R.M.; Wong, J.; Davis, S.L. Outpatient use of ceftaroline fosamil versus vancomycin for osteoarticular infection: A matched cohort study. J. Antimicrob. Chemother. 2016, 71, 3568–3574. [Google Scholar] [CrossRef] [PubMed]
- Schrank, G.M.; Wright, S.B.; Branch-Elliman, W.; LaSalvia, M.T. A retrospective analysis of adverse events among patients receiving daptomycin versus vancomycin during outpatient parenteral antimicrobial therapy. Infect. Control Hosp. Epidemiol. 2018, 39, 947–954. [Google Scholar] [CrossRef] [PubMed]
- Muldoon, E.G.; Snydman, D.R.; Penland, E.C.; Allison, G.M. Are we ready for an outpatient parenteral antimicrobial therapy bundle? A critical appraisal of the evidence. Clin. Infect. Dis. 2013, 57, 419–424. [Google Scholar] [CrossRef] [PubMed]
- Heintz, B.H.; Halilovic, J.; Christensen, C.L. Impact of a multidisciplinary team review of potential outpatient parenteral antimicrobial therapy prior to discharge from an academic medical center. Ann. Pharmacother. 2011, 45, 1329–1337. [Google Scholar] [CrossRef]
- Heus, A.; Uster, D.W.; Grootaert, V.; Vermeulen, N.; Somers, A.; Huis In’t Veld, D.; Wicha, S.G.; De Cock, P.A. Model-informed precision dosing of vancomycin via continuous infusion: A clinical fit-for-purpose evaluation of published PK models. Int. J. Antimicrob. Agents 2022, 59, 106579. [Google Scholar] [CrossRef]
- Bakhtiari, I.G.; Vles, G.; Busch, S.M.; Frommelt, L.; Gehrke, T.; Salber, J.; Citak, M. Septic Failure After One-Stage Exchange for Prosthetic Joint Infection of the Hip: Microbiological Implications. J. Arthroplasty 2022, 37, 373–378. [Google Scholar] [CrossRef]
- Zalavras, C.G.; Aerden, L.; Declercq, P.; Belmans, A.; Metsemakers, W.J. Ninety-Day Follow-up Is Inadequate for Diagnosis of Fracture-related Infections in Patients with Open Fractures. Clin. Orthop. Relat. Res. 2022, 480, 139–146. [Google Scholar] [CrossRef]
| Medical, Infection-Related Criteria | ||
| Need for vancomycin antimicrobial therapy | ||
| Monotherapy with vancomycin | ||
| Proven infectious focus or diagnosis | ||
| Directed therapy against an identified micro-organism with susceptibility to vancomycin | ||
| At least first dose of vancomycin administered in the hospital | ||
| Treatment with oral antimicrobial agent not possible or appropriate | ||
| e.g., no oral antimicrobial with same spectrum and sufficient bio-availability | ||
| Infection is biochemically and clinically stable with a predictable course | ||
| Declining C-reactive protein since start antibiotic treatment | ||
| Afebrile for at least 48 h | ||
| Medical, Non-Infection-Related Criteria | ||
| No psychological or cognitive disease or disability | ||
| No active intravenous drug use | ||
| No planned hospital admission for (additional) surgery within 7 days after OPAT discharge | ||
| Patient-Related Criteria | ||
| No stay in a nursing or retirement home | ||
| Self-sufficient patient with adequate cognitive and psychosocial function or sufficient professional support at home | ||
| Hygienic and adequate home situation | ||
| Vancomycin-Specific Criteria | ||
| Administration by continuous infusion | ||
| Last two steady-state plasma concentrations within therapeutic range (20–25 mg/L) | ||
| Central venous line (PICC or venous port) | ||
| Plasma Concentration | Recommendations |
|---|---|
| <15 mg/L |
|
| 15–17.5 mg/L |
|
| 17.5–20 mg/L |
|
| 20–25 mg/L |
|
| 25–27.5 mg/L |
|
| 27.5–30 mg/L |
|
| >30 mg/L |
|
| Demographics | ||
| vOPAT episodes, n | 35 | |
| Patients, n | 32 | |
| Patients with 2 vOPAT episodes, n | 3 | |
| Male/female, n | 23/12 | |
| Age (years), median (range) | 61 (11–75) | |
| eGFR (at start vancomycin therapy), CKD-EPI, mL/min/1.73 m2, median (range) | 90.0 (45.0–188.0) | |
| Medical Discipline | ||
| Surgical, n (%) | 30 (85.7) | |
| Orthopedic surgery, n (%) | 15 (42.9) | |
| Trauma surgery, n (%) | 13 (37.1) | |
| Urology, n (%) | 1 (2.9) | |
| Vascular surgery, n (%) | 1 (2.9) | |
| Internal medicine, n (%) | 3 (8.6) | |
| Hematology, n (%) | 1 (2.9) | |
| General internal medicine, n (%) | 1 (2.9) | |
| Nephrology, n (%) | 1 (2.9) | |
| Pediatric, n (%) | 2 (5.7) | |
| Clinical Indication | ||
| Bone and joint infections, n (%) | 30 (85.7) | |
| (Catheter-related) blood stream infection, n (%) | 3 (8.6) | |
| (Endo)vascular infection, n (%) | 2 (5.7) | |
| Causative Pathogen(s) | ||
| S. epidermidis, n (%) | 21 (60.0) | |
| S. epidermidis + E. faecalis, n (%) | 1 (2.9) | |
| S. epidermidis + E. faecium, n (%) | 2 (5.7) | |
| S. epidermidis + S. capitis + Bacillus, n (%) | 1 (2.9) | |
| S. epidermidis + S. capitis, n (%) | 1 (2.9) | |
| (Methicillin resistant) S. aureus, n (%) | 3 (8.6) | |
| S. aureus + E. faecalis, n (%) | 1 (2.9) | |
| S. capitis + S. salivarius, n (%) | 1 (2.9) | |
| S. hominis + S. epidermidis + S. warneri, n (%) | 1 (2.9) | |
| S. hominis + S. epidermidis + S. warneri + S. pettenkoferi + Arthrobacter species, n (%) | 1 (2.9) | |
| S. hominis, n (%) | 1 (2.9) | |
| E. faecalis + E. faecium, n (%) | 1 (2.9) | |
| Target Attainment | ||
| Total number of vancomycin plasma concentrations measured during vOPAT | 203 | |
| Total number of therapeutic plasma concentrations during vOPAT (%) | 139 (68.5) | |
| Total number of non-therapeutic plasma concentrations during vOPAT (%) | 64 (31.5) | |
| Total number of subtherapeutic plasma concentrations (%) | 34 (16.7) | |
| Total number of supratherapeutic plasma concentrations (%) | 30 (14.8) | |
| Total number of therapeutic plasma concentrations + 5% deviation during vOPAT (%) | 164 (80.8) | |
| Total number of therapeutic plasma concentrations + 10% deviation during vOPAT (%) | 182 (89.7) | |
| Median vancomycin plasma concentration during vOPAT (mg/L) (range) | 22.5 (6.6–32.0) | |
| Median number of non-therapeutic plasma concentrations per vOPAT episode (range) | 2 (0–8) | |
| Adherence to Dose Adjustment Protocol | ||
| Total number of dose adjustments during vOPAT | 51 | |
| Therapeutic plasma concentration after dose adjustment, n (%) | 31 (60.8) | |
| Compliance with dose adjustment protocol, n (%) | 14 (45.2) | |
| Non-therapeutic plasma concentration after dose adjustment, n (%) | 18 (35.3) | |
| Compliance with dose adjustment protocol, n (%) | 10 (55.6) | |
| Two consecutive subtherapeutic plasma concentrations despite dose increase, n (%) | 2 (11.1) | |
| Two consecutive supratherapeutic plasma concentrations despite dose reduction, n (%) | 6 (33.3) | |
| Switch from subtherapeutic to supratherapeutic plasma concentration after dose increase, n (%) | 6 (33.3) | |
| Switch from supratherapeutic to subtherapeutic plasma concentration after dose reduction, n (%) | 2 (11.1) | |
| Switch from therapeutic to subtherapeutic plasma concentration after dose reduction, n (%) | 2 (11.1) | |
| No new plasma concentration following dose adjustment, n (%) | 2 (3.9) | |
| Treatment Duration, Length of Hospital Stay and Avoided Hospitalization Days | ||
| Length of hospital stay (days), median (range) | 22 (13–57) | |
| Vancomycin treatment duration before discharge (days), median (range) | 20 (9–47) | |
| Duration vOPAT episode (days), median (range) | 18 (4–63) | |
| Total vancomycin treatment duration (days), median (range) | 43 (13–92) | |
| Clinical Outcome and vOPAT-Related Adverse Events | ||
| Clinical cure (n = 32) *, n (%) | 32 (100) * | |
| Readmissions with stop vOPAT, n (%) | 3 (8.6) | |
| Readmissions non-vOPAT-related, n (%) | 1 (2.9) | |
| Readmissions because of ADEs, n (%) | 2 (5.7) | |
| Temporarily readmissions with continuation of vOPAT, n (%) | 3 (8.6) | |
| Readmission because of difficulties regulating vancomycin plasma concentrations, n (%) | 1 (2.9) | |
| Readmission because of LRAEs, n (%) | 2 (5.7) | |
| LRAEs, n (%) | 2 (5.7) | |
| Phlebitis, n (%) | 1 (2.9) | |
| Catheter migration, n (%) | 1 (2.9) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thijs, L.; Quintens, C.; Vander Elst, L.; De Munter, P.; Depypere, M.; Metsemakers, W.-J.; Vles, G.; Liesenborghs, A.; Neefs, J.; Peetermans, W.E.; et al. Clinical Efficacy and Safety of Vancomycin Continuous Infusion in Patients Treated at Home in an Outpatient Parenteral Antimicrobial Therapy Program. Antibiotics 2022, 11, 702. https://doi.org/10.3390/antibiotics11050702
Thijs L, Quintens C, Vander Elst L, De Munter P, Depypere M, Metsemakers W-J, Vles G, Liesenborghs A, Neefs J, Peetermans WE, et al. Clinical Efficacy and Safety of Vancomycin Continuous Infusion in Patients Treated at Home in an Outpatient Parenteral Antimicrobial Therapy Program. Antibiotics. 2022; 11(5):702. https://doi.org/10.3390/antibiotics11050702
Chicago/Turabian StyleThijs, Lore, Charlotte Quintens, Lotte Vander Elst, Paul De Munter, Melissa Depypere, Willem-Jan Metsemakers, Georges Vles, Astrid Liesenborghs, Jens Neefs, Willy E. Peetermans, and et al. 2022. "Clinical Efficacy and Safety of Vancomycin Continuous Infusion in Patients Treated at Home in an Outpatient Parenteral Antimicrobial Therapy Program" Antibiotics 11, no. 5: 702. https://doi.org/10.3390/antibiotics11050702
APA StyleThijs, L., Quintens, C., Vander Elst, L., De Munter, P., Depypere, M., Metsemakers, W.-J., Vles, G., Liesenborghs, A., Neefs, J., Peetermans, W. E., & Spriet, I. (2022). Clinical Efficacy and Safety of Vancomycin Continuous Infusion in Patients Treated at Home in an Outpatient Parenteral Antimicrobial Therapy Program. Antibiotics, 11(5), 702. https://doi.org/10.3390/antibiotics11050702







