Multicenter Study of Carbapenemase-Producing Enterobacterales in Havana, Cuba, 2016–2021
Abstract
:1. Introduction
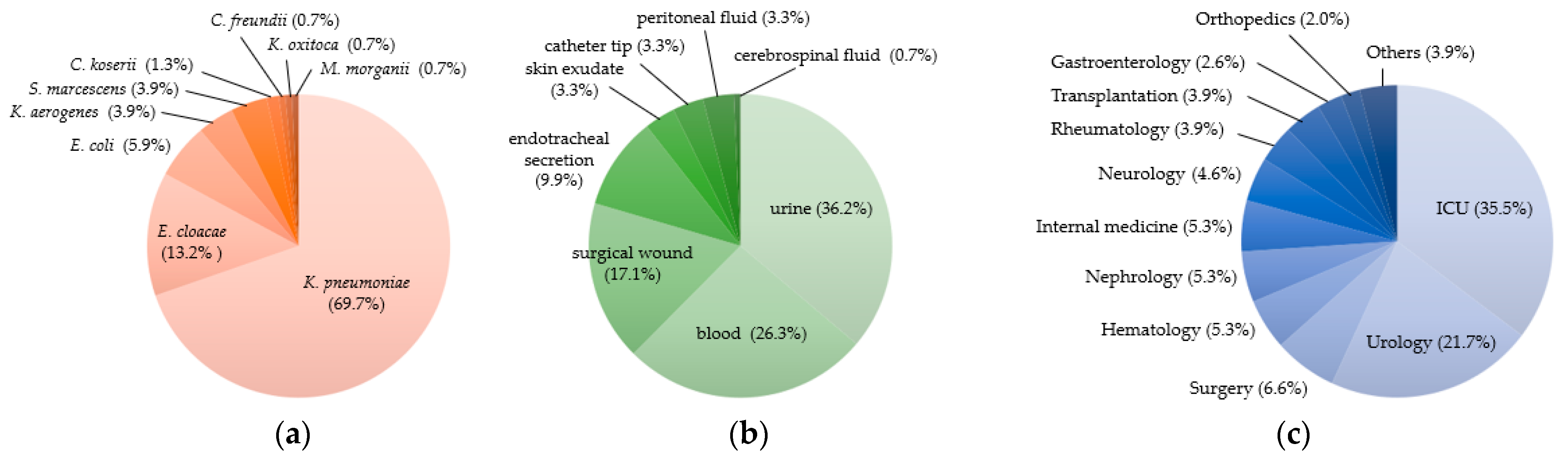
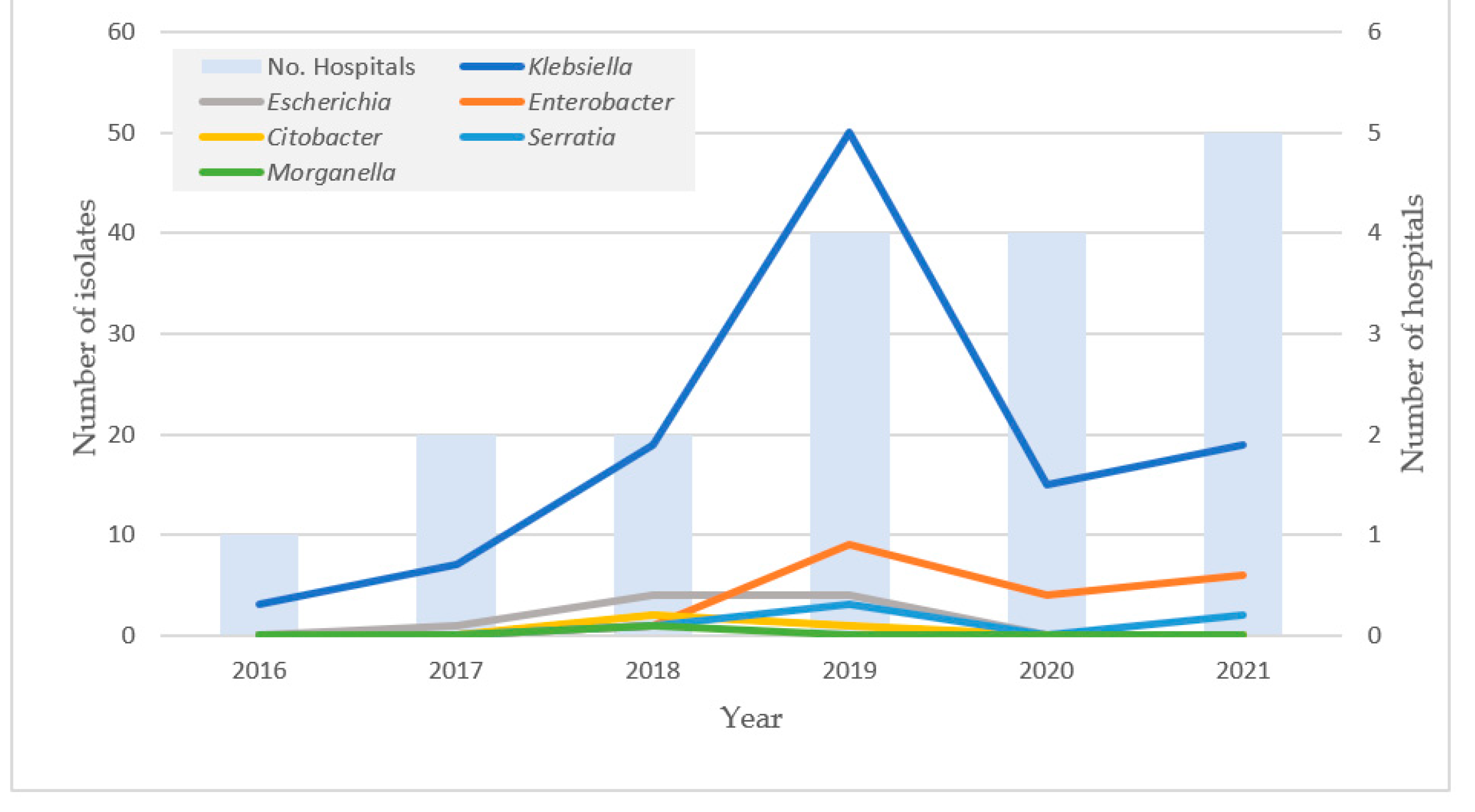
2. Results
3. Discussion
4. Materials and Methods
4.1. Bacterial Isolation and Species Identification
4.2. Determination of Antimicrobial Susceptibility
4.3. Phenotypic Detection of Carbapenemases
4.4. Detection of Genetic Types of Carbapenemases
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Yu, H.; Han, X.; Quiñones, D. La humanidad enfrenta un desastre: La resistencia antimicrobiana. Rev. Habanera Cienc. Méd. 2021, 20, e3850. [Google Scholar]
- Farfour, E.; Lecuru, M.; Dortet, L.; Le Guen, M.; Cerf, C.; Karnycheff, F.; Bonnin, R.A.; Vasse, M.; Lesprit, P. Carbapenemase-producing Enterobacterales outbreak: Another dark side of COVID-19. Am. J. Infect. Control 2020, 48, 1533–1536. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Bornman, C.; Zafer, M.M. Antimicrobial Resistance Threats in the emerging COVID-19 pandemic: Where do we stand? J. Infect. Public Health 2021, 14, 555–560. [Google Scholar] [CrossRef]
- WHO. WHO Publishes List of Bacteria for Which New Antibiotics are Urgently Needed. Available online: https://www.who.int/es/news/item/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed (accessed on 1 March 2022).
- WHO. Guidelines for the Prevention and Control of Carbapenem-Resistant Enterobacteriaceae, Acinetobacter baumannii and Pseudomonas aeruginosa in Health Care Facilities; World Health Organization: Geneva, Switzerland, 2017; Available online: https://apps.who.int/iris/bitstream/handle/10665/259462/9789241550178-eng.pdf?sequence=1&isAllowed=y (accessed on 1 March 2022).
- Quiñones Pérez, D.; Diaz, G.; Carmona, Y.; Zayas, A.; Abreu, M.; Salazar, D.; García, S.; Santiesteban, Y.; Jiménez, T.N.; Hart, M. Infecciones por Klebsiella: Un desafío en Hospitales Cubanos. Contribución del LNRM-IPK en su prevención y control. An. Acad. Cienc. Cuba 2015, 5. Available online: http://revistaccuba.sld.cu/index.php/revacc/article/view/287/287 (accessed on 1 March 2022).
- Iredell, J.; Brown, J.; Tagg, K. Antibiotic resistance in Enterobacteriaceae: Mechanisms and clinical implications. BMJ 2016, 352, h6420. [Google Scholar] [CrossRef]
- van Duin, D.; Doi, Y. The global epidemiology of carbapenemase-producing Enterobacteriaceae. Virulence 2017, 8, 460–469. [Google Scholar] [CrossRef]
- Villegas, M.V.; Pallares, C.J.; Escandón-Vargas, K.; Hernández-Gómez, C.; Correa, A.; Álvarez, C.; Rosso, F.; Matta, L.; Luna, C.; Zurita, J.; et al. Characterization and Clinical Impact of Bloodstream Infection Caused by Carbapenemase-Producing Enterobacteriaceae in Seven Latin American Countries. PLoS ONE 2016, 11, e0154092. [Google Scholar] [CrossRef] [Green Version]
- Alerta Epidemiológica: Emergencia e Incremento de Nuevas Combinaciones de Carbapenemasas en Enterobacterales en Latinoamérica y el Caribe; Organización Panamericana de la Salud/Organización Mundial de la Salud: Washington, DC, USA, 2021.
- Quinones, D.; Hart, M.; Espinosa, F.; Garcia, S.; Carmona, Y.; Ghosh, S.; Urushibara, N.; Kawaguchiya, M.; Kobayashi, N. Emergence of Klebsiella pneumoniae clinical isolates producing KPC-2 carbapenemase in Cuba. New Microbes New Infect. 2014, 2, 123–126. [Google Scholar] [CrossRef] [Green Version]
- Quiñones, D.; Carvajal, I.; Perez, Y.; Hart, M.; Perez, J.; Garcia, S.; Salazar, D.; Ghosh, S.; Kawaguchiya, M.; Aung, M.S.; et al. High prevalence of blaOXA-23 in Acinetobacter spp. and detection of blaNDM-1 in A. soli in Cuba: Report from National Surveillance Program (2010–2012). New Microbes New Infect. 2015, 7, 52–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ortiz, T.J. Enterobacterias Productoras de Carbapenemasas en Cuba, Tipos, Evaluación de Métodos Para su Detección y Antibiotipos; Tesis de Maestría en Bacteriología-Micología; Instituto Pedro Kourí: La Habana, Cuba, 2018. [Google Scholar]
- Llerena, M.R. Caracterización Clínica, Epidemiológica y Microbiológica de Infecciones Por Enterobacterias Productoras de Carbapenemasas en Hospitales Centinelas; Tesis de Especialista en Microbiología Clínica; Instituto Pedro Kouri: La Habana, Cuba, 2019. [Google Scholar]
- Castanheira, M.; Deshpande, L.M.; Mendes, R.E.; Canton, R.; Sader, H.S.; Jones, R.N. Variations in the Occurrence of Resistance Phenotypes and Carbapenemase Genes Among Enterobacteriaceae Isolates in 20 Years of the SENTRY Antimicrobial Surveillance Program. Open Forum Infect. Dis. 2019, 6, S23–S33. [Google Scholar] [CrossRef] [Green Version]
- Bolaño Ardila, N.D. Uso de la terapia combinada en infecciones causadas por enterobacterias resistente a carbapenémicos desde un enfoque microbiológico: Revisión sistemática. Med. Lab. 2016, 22, 165–180. [Google Scholar] [CrossRef]
- Lob, S.H.; Karlowsky, J.A.; Young, K.; Motyl, M.R.; Hawser, S.; Kothari, N.D.; Sahm, D.F. In vitro activity of imipenem-relebactam against resistant phenotypes of Enterobacteriaceae and Pseudomonas aeruginosa isolated from intraabdominal and urinary tract infection samples—SMART Surveillance Europe 2015–2017. J. Med. Microbiol. 2020, 69, 207–217. [Google Scholar] [CrossRef] [PubMed]
- Soria-Segarra, C.; Soria-Segarra, C.; Catagua-González, A.; Gutiérrez-Fernández, J. Carbapenemase producing Enterobacteriaceae in intensive care units in Ecuador: Results from a multicenter study. J. Infect. Public Health 2020, 13, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Padilla-Serrano, A.; Serrano-Castañeda, J.J.; Carranza-González, R.; García-Bonillo, M.P. Clinical significance and risk factors for multidrug resistant Enterobacteriaceae colonization. Rev. Esp. Quim. 2018, 31, 257–262. [Google Scholar]
- Femi, A.; Chidalu Nnabude, B.; Otuechere, C.A. Hand Hygiene Practices and the Effectiveness of Hand Sanitizers at Controlling Enteropathogens among the Residents of a University Community in Osun State Nigeria. Microbiol. Res. J. Int. 2019, 27, 1–9. [Google Scholar]
- Mariappan, S.; Sekar, U.; Kamalanathan, A. Carbapenemase-producing Enterobacteriaceae: Risk factors for infection and impact of resistance on outcomes. Int. J. Appl. Basic Med. Res. 2017, 7, 32–39. [Google Scholar] [CrossRef] [Green Version]
- Zhang, R.; Liu, L.; Zhou, H.; Chan, E.W.; Li, J.; Fang, Y.; Li, Y.; Liao, K.; Chen, S. Nationwide Surveillance of Clinical Carbapenem-resistant Enterobacteriaceae (CRE) Strains in China. EBioMedicine 2017, 19, 98–106. [Google Scholar] [CrossRef] [Green Version]
- Grundmann, H.; Glasner, C.; Albiger, B.; Aanensen, D.M.; Tomlinson, C.T.; Andrasević, A.T.; Cantón, R.; Carmeli, Y.; Friedrich, A.W.; Giske, C.G.; et al. Occurrence of carbapenemase-producing Klebsiella pneumoniae and Escherichia coli in the European survey of carbapenemase-producing Enterobacteriaceae (EuSCAPE): A prospective, multinational study. Lancet Infect. Dis. 2017, 17, 153–163. [Google Scholar] [CrossRef] [Green Version]
- Khan, A.U.; Maryam, L.; Zarrilli, R. Structure, Genetics and Worldwide Spread of New Delhi Metallo-β-lactamase (NDM): A threat to public health. BMC Microbiol. 2017, 17, 101. [Google Scholar] [CrossRef] [Green Version]
- Pasteran, F.; Albornoz, E.; Faccone, D.; Gomez, S.; Valenzuela, C.; Morales, M.; Estrada, P.; Valenzuela, L.; Matheu, J.; Guerriero, L.; et al. Emergence of NDM-1-producing Klebsiella pneumoniae in Guatemala. J. Antimicrob. Chemother. 2012, 67, 1795–1797. [Google Scholar] [CrossRef] [Green Version]
- García-Betancur, J.C.; Appel, T.M.; Esparza, G.; Gales, A.C.; Levy-Hara, G.; Cornistein, W.; Vega, S.; Nuñez, D.; Cuellar, L.; Bavestrello, L.; et al. Update on the epidemiology of carbapenemases in Latin America and the Caribbean. Expert Rev. Anti-Infect. Ther. 2021, 19, 197–213. [Google Scholar] [CrossRef] [PubMed]
- Findlay, J.; Poirel, L.; Kessler, J.; Kronenberg, A.; Nordmann, P. New Delhi Metallo-β-Lactamase–Producing Enterobacterales Bacteria, Switzerland, 2019–2020. Emerg. Infect. Dis. 2021, 27, 2628–2637. [Google Scholar] [CrossRef] [PubMed]
- Doi, Y.; Wachino, J.I.; Arakawa, Y. Aminoglycoside resistance: The emergence of acquired 16S ribosomal RNA methyltransferases. Infect. Dis. Clin. 2016, 30, 523–537. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zurfluh, K.; Treier, A.; Schmitt, K.; Stephan, R. Mobile fosfomycin resistance genes in Enterobacteriaceae-An increasing threat. Microbiologyopen 2020, 9, e1135. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Feng, Y.; Tang, G.; Qiao, F.; McNally, A.; Zong, Z. NDM Metallo-β-Lactamases and Their Bacterial Producers in Health Care Settings. Clin. Microbiol. Rev. 2019, 32, e00115–e00118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dundar, D.; Duymaz, Z.; Genc, S.; Er, D.K.; İrvem, A.; Kandemir, N. In-vitro activities of imipenem–colistin, imipenem–tigecycline, and tigecycline–colistin combinations against carbapenem-resistant Enterobacteriaceae. J. Chemother. 2018, 30, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Ramos, J.R.; Lletí, M.S. Fosfomicina en las infecciones producidas por gramnegativos multirresistentes. Rev. Esp. De Quimioter. 2019, 32, 45–54. [Google Scholar]
- Alves, P.H.; Boff, R.T.; Barth, A.L.; Martins, A.F. Synergy of polymyxin B, tigecycline and meropenem against carbapenem-resistant Enterobacter cloacae complex isolates. Diagn. Microbiol. Infect. Dis. 2019, 94, 81–85. [Google Scholar] [CrossRef]
- Sheu, C.C.; Chang, Y.T.; Lin, S.Y.; Chen, Y.H.; Hsueh, P.R. Infections Caused by Carbapenem-Resistant Enterobacteriaceae: An Update on Therapeutic Options. Front. Microbiol. 2019, 10, 80. [Google Scholar] [CrossRef] [Green Version]
- Tumbarello, M.; Losito, A.R.; Giamarellou, H. Optimizing therapy in carbapenem-resistant Enterobacteriaceae infections. Curr. Opin. Infect. Dis. 2018, 31, 566–577. [Google Scholar] [CrossRef]
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing, 31st ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2021. [Google Scholar]
- EUCAST. Breakpoint Tables for Interpretation of MICs and Zone Diameters, version 11.0; The European Committee on Antimicrobial Susceptibility Testing: Växjö, Sweden, 2021; Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_11.0_Breakpoint_Tables.pdf (accessed on 1 March 2022).
- Poirel, L.; Walsh, T.R.; Cuvillier, V.; Nordmann, P. Multiplex PCR for detection of acquired carbapenemase genes. Diagn. Microbiol. Infect. Dis. 2011, 70, 119–123. [Google Scholar] [CrossRef] [PubMed]
| Antimicrobials 1 | Susceptibility 2 | Bacterial Species | ||||||
|---|---|---|---|---|---|---|---|---|
| K. peumoniae | Enterobacter cloacae complex | E. coli | K. aerogenes | S. marcescens | Others 3 | Total | ||
| (n = 106) | (n = 20) | (n = 9) | (n = 6) | (n = 6) | (n = 5) | (n = 152) | ||
| SAM | R | 100% | 100% | 100% | 100% | 100% | 100% | 100% |
| TZP | R | 100% | 100% | 100% | 100% | 100% | 100% | 100% |
| MEM | I | 2% | 0% | 0% | 17% | 0% | 20% | 3% |
| R | 98% | 100% | 100% | 83% | 100% | 80% | 97% | |
| IPM | I | 4% | 5% | 0% | 17% | 0% | 20% | 5% |
| R | 96% | 95% | 100% | 83% | 100% | 80% | 95% | |
| ATM | S | 1% | 10% | 11% | 17% | 0% | 20% | 4% |
| I | 0% | 0% | 11% | 0% | 0% | 0% | 1% | |
| R | 99% | 90% | 78% | 83% | 100% | 80% | 95% | |
| CIP | S | 8% | 10% | 33% | 0% | 17% | 0% | 10% |
| I | 1% | 0% | 0% | 0% | 0% | 0% | 1% | |
| R | 91% | 90% | 67% | 100% | 83% | 100% | 89% | |
| GEN | S | 5% | 5% | 11% | 0% | 0% | 0% | 5% |
| I | 2% | 0% | 0% | 0% | 0% | 0% | 1% | |
| R | 93% | 95% | 89% | 100% | 100% | 100% | 94% | |
| AMK | S | 8% | 10% | 22% | 0% | 0% | 0% | 8% |
| I | 2% | 0% | 11% | 0% | 0% | 0% | 2% | |
| R | 90% | 90% | 67% | 100% | 100% | 100% | 90% | |
| SXT | S | 3% | 0% | 22% | 0% | 17% | 0% | 4% |
| I | 0% | 0% | 0% | 0% | 0% | 0% | 0% | |
| R | 97% | 100% | 78% | 100% | 83% | 100% | 96% | |
| FOS | S | 22% | 20% | 78% | 0% | 17% | 20% | 24% |
| I | 4% | 5% | 0% | 0% | 33% | 0% | 5% | |
| R | 74% | 75% | 22% | 100% | 50% | 80% | 71% | |
| CST 4 | S | 75% | 75% | 100% | 67% | - | 100% | 73% |
| I | 0% | 0% | 0% | 0% | - | 0% | 0% | |
| R | 25% | 25% | 0% | 33% | - | 0% | 27% | |
| TGC | S | 58% | 75% | 67% | 83% | 66% | 80% | 63% |
| I | 27% | 10% | 22% | 17% | 17% | 0% | 23% | |
| R | 15% | 15% | 11% | 0% | 17% | 20% | 14% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, H.; González Molina, M.K.; Carmona Cartaya, Y.; Hart Casares, M.; Aung, M.S.; Kobayashi, N.; Quiñones Pérez, D. Multicenter Study of Carbapenemase-Producing Enterobacterales in Havana, Cuba, 2016–2021. Antibiotics 2022, 11, 514. https://doi.org/10.3390/antibiotics11040514
Yu H, González Molina MK, Carmona Cartaya Y, Hart Casares M, Aung MS, Kobayashi N, Quiñones Pérez D. Multicenter Study of Carbapenemase-Producing Enterobacterales in Havana, Cuba, 2016–2021. Antibiotics. 2022; 11(4):514. https://doi.org/10.3390/antibiotics11040514
Chicago/Turabian StyleYu, Haiyang, María Karla González Molina, Yenisel Carmona Cartaya, Marcia Hart Casares, Meiji Soe Aung, Nobumichi Kobayashi, and Dianelys Quiñones Pérez. 2022. "Multicenter Study of Carbapenemase-Producing Enterobacterales in Havana, Cuba, 2016–2021" Antibiotics 11, no. 4: 514. https://doi.org/10.3390/antibiotics11040514
APA StyleYu, H., González Molina, M. K., Carmona Cartaya, Y., Hart Casares, M., Aung, M. S., Kobayashi, N., & Quiñones Pérez, D. (2022). Multicenter Study of Carbapenemase-Producing Enterobacterales in Havana, Cuba, 2016–2021. Antibiotics, 11(4), 514. https://doi.org/10.3390/antibiotics11040514






