Stability Studies of 16 Antibiotics for Continuous Infusion in Intensive Care Units and for Performing Outpatient Parenteral Antimicrobial Therapy
Abstract
:1. Introduction
2. Results
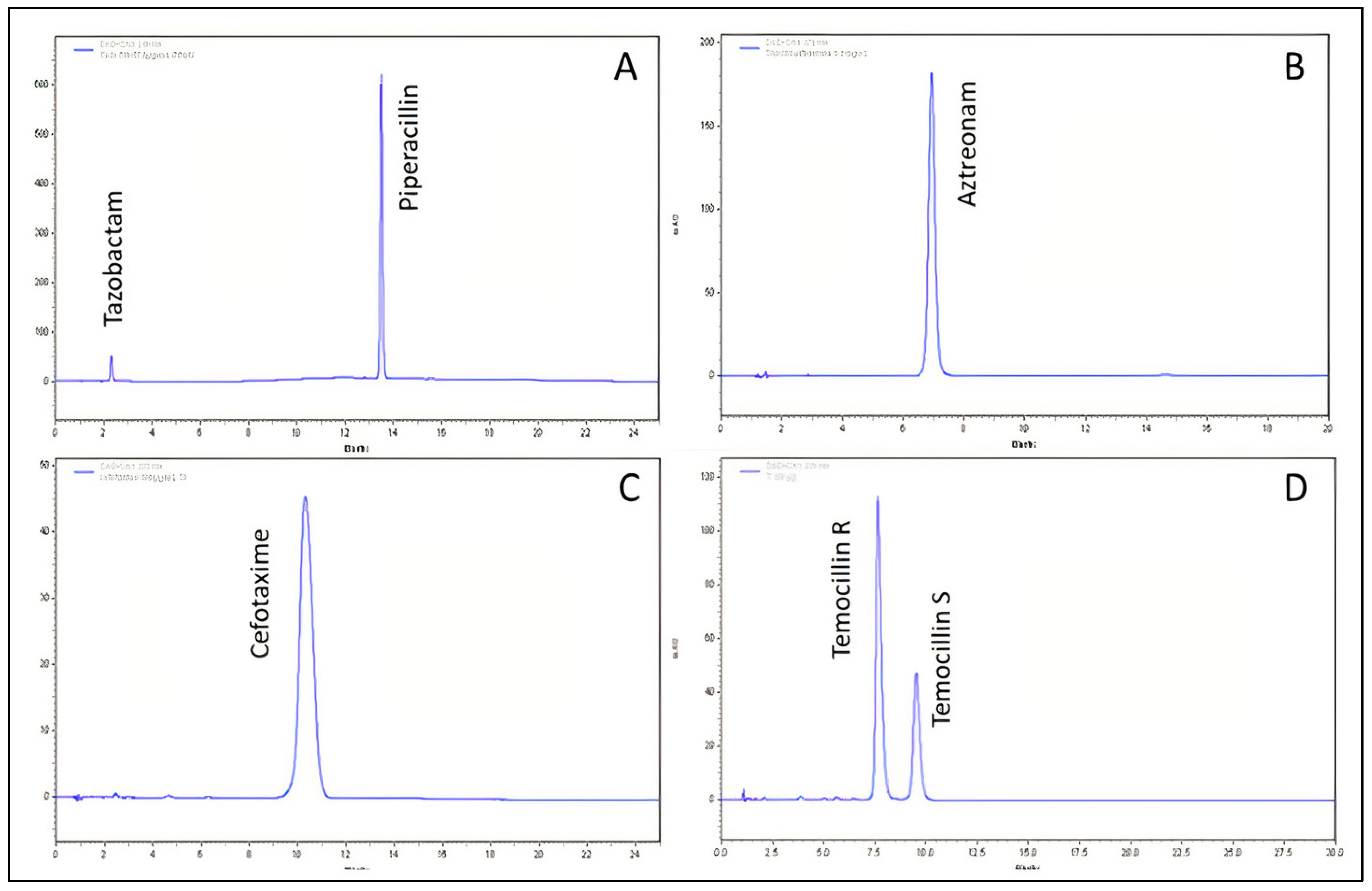
2.1. Chemical Stability by HPLC
2.2. The pH Measurement
2.3. The Visual and Subvisual Evaluation
3. Discussion
3.1. Choice of the Temperature
3.2. Choice of Molecules and Study Design
3.3. About the Solvents Used
3.4. Limiting Factors
3.5. Citrated Buffered Solutions
4. Materials and Methods
4.1. Chemical, Reagents and Products Used
4.2. Apparatuses
- –
- The High-Performance Liquid Chromatography (HPLC) system consisted of an ELITE LaChromVWR/ Hitachi plus autosampler, a VWR photodiode array detector L- 2455, and a VWR L-2130 HPLC pump. Data were acquired and integrated using EZChrom Elite (VWR, Agilent).
- –
- pH meter (Bioblock Scientific model 93313).
- –
- PAMAS particle counter, Rutesheim, Germany.
4.3. Methods
4.4. Chemical Stability by HPLC
4.5. Validation of the Analytical Methods
4.6. Physical Stability
4.7. pH Measurements
4.8. Summary of the Results
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mouton, J.W.; Punt, N.; Vinks, A.A. Concentration-Effect Relationship of Ceftazidime Explains Why the Time above the MIC Is 40 Percent for a Static Effect In Vivo. Antimicrob. Agents Chemother. 2007, 51, 3449–3451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, Y.R.; Miller, P.D.; Alzghari, S.K.; Blanco, D.D.; Hager, J.D.; Kuntz, K.S. Continuous Infusion Versus Intermittent Bolus of Beta-Lactams in Critically Ill Patients with Respiratory Infections: A Systematic Review and Meta-Analysis. Eur. J. Drug Metab. Pharmacokinet. 2018, 43, 155–170. [Google Scholar] [CrossRef]
- De Jongh, R.; Hens, R.; Basma, V.; Mouton, J.W.; Tulkens, P.M.; Carryn, S. Continuous versus Intermittent Infusion of Temocillin, a Directed Spectrum Penicillin for Intensive Care Patients with Nosocomial Pneumonia: Stability, Compatibility, Population Pharmacokinetic Studies and Breakpoint Selection. J. Antimicrob. Chemother. 2008, 61, 382–388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roberts, J.A.; Abdul-Aziz, M.-H.; Davis, J.S.; Dulhunty, J.M.; Cotta, M.O.; Myburgh, J.; Bellomo, R.; Lipman, J. Continuous versus Intermittent β-Lactam Infusion in Severe Sepsis. A Meta-Analysis of Individual Patient Data from Randomized Trials. Am. J. Respir. Crit. Care Med. 2016, 194, 681–691. [Google Scholar] [CrossRef]
- Flannery, A.; Bissell, B.; Thompson Bastin, M.; Morris, P.; Neyra, J. Continuous versus Intermittent Infusion of Vancomycin and the Risk of Acute Kidney Injury in Critically Ill Adults: A Systematic Review and Meta-Analysis. Crit Care Med. 2020, 48, 912–918. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.-L.; Sakr, Y.; Sprung, C.L.; Ranieri, V.M.; Reinhart, K.; Gerlach, H.; Moreno, R.; Carlet, J.; Le Gall, J.-R.; Payen, D.; et al. Sepsis in European Intensive Care Units: Results of the SOAP Study. Crit. Care Med. 2006, 34, 344–353. [Google Scholar] [CrossRef] [PubMed]
- Norris, A.H.; Shrestha, N.K.; Allison, G.M.; Keller, S.C.; Bhavan, K.P.; Zurlo, J.J.; Hersh, A.L.; Gorski, L.A.; Bosso, J.A.; Rathore, M.H.; et al. 2018 Infectious Diseases Society of America Clinical Practice Guideline for the Management of Outpatient Parenteral Antimicrobial Therapy. Clin. Infect. Dis. 2019, 68, e1–e35. [Google Scholar] [CrossRef]
- Gilchrist, M.; Seaton, R.A. Outpatient Parenteral Antimicrobial Therapy and Antimicrobial Stewardship: Challenges and Checklists. J. Antimicrob. Chemother. 2015, 70, 965–970. [Google Scholar] [CrossRef] [Green Version]
- Arensdorff, L.; Boillat-Blanco, N.; Decosterd, L.; Buclin, T.; de Vallière, S. Adequate Plasma Drug Concentrations Suggest That Amoxicillin Can Be Administered by Continuous Infusion Using Elastomeric Pumps. J. Antimicrob. Chemother. 2017, 72, 2613–2615. [Google Scholar] [CrossRef]
- Voumard, R.; Gardiol, C.; André, P.; Arensdorff, L.; Cochet, C.; Boillat-Blanco, N.; Decosterd, L.; Buclin, T.; de Vallière, S. Efficacy and Safety of Continuous Infusions with Elastomeric Pumps for Outpatient Parenteral Antimicrobial Therapy (OPAT): An Observational Study. J. Antimicrob. Chemother. 2018, 73, 2540–2545. [Google Scholar] [CrossRef] [Green Version]
- Diamantis, S.; Dawudi, Y.; Cassard, B.; Longuet, P.; Lesprit, P.; Gauzit, R. Home Intravenous Antibiotherapy and the Proper Use of Elastomeric Pumps: Systematic Review of the Literature and Proposals for Improved Use. Infect. Dis. Now 2021, 51, 39–49. [Google Scholar] [CrossRef]
- Jenkins, A.; Shanu, S.; Jamieson, C.; Santillo, M. Widening the Net: A Literature Review of Antimicrobial Agents with Potential Suitability for Outpatient Parenteral Antimicrobial Therapy Services-the Importance of Storage and Stability. Eur. J. Hosp. Pharm. Sci. Pract. 2021. [Google Scholar] [CrossRef]
- ASEAN Guidelines on Stability Study of Drug Product. Update Review 22 Février 2005. In Proceedings of the 9th ACCSQ-PPWG Meeting, Manila, Philippines, 21–24 February 2005.
- Guidance for Industry: Drug Stability Guidelines; U.S. Department of Health and Human Services Food and Drug Administration: Silver Spring, MD, USA, 2008.
- Longuet, P.; Lecapitaine, A.L.; Cassard, B.; Batista, R.; Gauzit, R.; Lesprit, P.; Haddad, R.; Vanjak, D.; Diamantis, S.; Groupe des référents en infectiologie d’Île-de-France (GRIF). Preparing and Administering Injectable Antibiotics: How to Avoid Playing God. Med. Mal. Infect. 2016, 46, 242–268. [Google Scholar] [CrossRef]
- Diamantis, S.; Longuet, P.; Lesprit, P.; Gauzit, R. Terms of Use of Outpatient Parenteral Antibiotic Therapy. Infect. Dis. Now 2020, 51, 14–38. [Google Scholar] [CrossRef]
- SFPC (French Society of Clinical Pharmacy) and GERPAC (Evaluation and Research Group on Protection in Controlled Atmospher). SFPC, GERPAC, Methodological Guidelines for Stability Studies of Hospital Pharmaceutical Preparations, Part I: Liquid Preparations. Available online: http://www.gerpac.eu/img/pdf/guide_stabilite_anglais.pdf (accessed on 24 March 2021).
- Allwood, M.C.; Stonkute, D.; Wallace, A.; Wilkinson, A.-S.; Hills, T.; Jamieson, C.; BSAC Drug Stability Working Party. Assessment of the Stability of Citrate-Buffered Flucloxacillin for Injection When Stored in Two Commercially Available Ambulatory Elastomeric Devices: INfusor LV (Baxter) and Accufuser (Woo Young Medical): A Study Compliant with the NHS Yellow Cover Document (YCD) Requirements. Eur. J. Hosp. Pharm. Sci. Pract. 2020, 27, 90–94. [Google Scholar] [CrossRef]
- Souza Barbosa, F.; Capra Pezzi, L.; Tsao, M.; Oliveira, T.F.; Manoela Dias Macedo, S.; Schapoval, E.E.S.; Mendez, A.S.L. Stability and Degradation Products of Imipenem Applying High-Resolution Mass Spectrometry: An Analytical Study Focused on Solutions for Infusion. Biomed. Chromatogr. 2018, 33, e4471. [Google Scholar] [CrossRef]
- Negaban 1 g, Powder for Solution for Injection/Infusio—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/466 (accessed on 3 March 2021).
- Gorski, L.A. The 2016 Infusion Therapy Standards of Practice. Home Healthc. Now 2017, 35, 10–18. [Google Scholar] [CrossRef]
- Fetcroja 1 g Powder—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/11771#gref (accessed on 27 January 2022).
- To, T.P.; Ching, M.; Ellis, A.G.; Williams, L.; Garrett, M.K. Stability of Intravenous Flucloxacillin Solutions Used for Hospital-in-the-Home. J. Pharm. Pract. Res. 2010, 40, 101–105. [Google Scholar] [CrossRef]
- Jamieson, C.; Allwood, M.C.; Stonkute, D.; Wallace, A.; Wilkinson, A.-S.; Hills, T.; BSAC Drug Stability Working Party. Investigation of Meropenem Stability after Reconstitution: The Influence of Buffering and Challenges to Meet the NHS Yellow Cover Document Compliance for Continuous Infusions in an Outpatient Setting. Eur. J. Hosp. Pharm. Sci. Pract. 2020, 27, e53–e57. [Google Scholar] [CrossRef]
- Smith, E.K.; McWhinney, B.C. Stability of Buffered Benzylpenicillin and Flucloxacillin for a Paediatric Outpatient Parenteral Antibiotic Therapy Service. J. Pharm. Pract. Res. 2021, 51, 231–237. [Google Scholar] [CrossRef]
- Müller, H.; Haker, I. The Stability of Amoxicillin, Ampicillin, Benzylpenicillin, Flucloxacillin, Mezlocillin and Piperacillin in Isotonic Saline Solutions When Stored in an Innovative Infusion Container (Freeflex Container). Eur. J. Hosp. Pharm. 2003, 9, 106–112. [Google Scholar]
- Trissel, L.A.; Xu, Q.A.; Martinez, J.F. Compatibility and Stability of Aztreonam and Vancomycin Hydrochloride. Am. J. Health-Syst. Pharm. AJHP 1995, 52, 2560–2564. [Google Scholar] [CrossRef] [PubMed]
- Stiles, M.L.; Tu, Y.H.; Allen, L.V. Stability of Cefazolin Sodium, Cefoxitin Sodium, Ceftazidime, and Penicillin G Sodium in Portable Pump Reservoirs. Am. J. Hosp. Pharm. 1989, 46, 1408–1412. [Google Scholar] [CrossRef]
- Loeuille, G.; Vigneron, J.; D’Huart, E.; Charmillon, A.; Demoré, B. Physicochemical Stability of Cefiderocol, a Novel Siderophore Cephalosporin, in Syringes at 62.5 Mg/ML for Continuous Administration in Intensive Care Units. Eur. J. Hosp. Pharm. Sci. Pract. 2021. [Google Scholar] [CrossRef] [PubMed]
- Japanese Pharmacopeia, 17th ed.; Pharmaceuticals and Medical Devices Agency: Tokyo, Japan, 2016; pp. 634–635.
- Abdel-Hamid, M.E. FSQ Spectrophotometric and HPLC Analysis of Some Cephalosporins in the Presence of Their Alkali-Induced Degradation Products. Il Farm. 1998, 53, 132–138. [Google Scholar] [CrossRef]
- Vikram, A.; Prathap, B.; Mallikarjuna, G.; SnehaSowmya, G.; Ushakiranmai, G. Analytical Method Development and Validation for Simultaneous Estimation of Avibactam and Ceftazidime by Rp-Hplc Method. IOSR J. Pharm. 2020, 10, 52–85. [Google Scholar]
- Kratzer, A.; Rothe, U.; Kees, F.; Dorn, C. Stabilität von Ceftolozan/Tazobactam in Infusionslösungen Für Die Verlängerte Oder Kontinuierliche Applikation. Krankenhauspharmazie 2019, 40, 195–200. [Google Scholar]
- Walker, S.E.; Dufour, A.; Iazzetta, J. Concentration and Solution Dependent Stability of Cloxacillin Intravenous Solutions. Can. J. Hosp. Pharm. 1998, 51, 13–19. [Google Scholar] [CrossRef]
- Viaene, E.; Chanteux, H.; Servais, H.; Mingeot-Leclercq, M.-P.; Tulkens, P.M. Comparative Stability Studies of Antipseudomonal Beta-Lactams for Potential Administration through Portable Elastomeric Pumps (Home Therapy for Cystic Fibrosis Patients) and Motor-Operated Syringes (Intensive Care Units). Antimicrob. Agents Chemother. 2002, 46, 2327–2332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hecq, J.-D.; Berlage, V.; Vanbeckbergen, D.; Jamart, J.; Galanti, L. Effects of Freezing, Long-Term Storage, and Microwave Thawing on the Stability of Piperacillin Plus Tazobactam in 5% Dextrose for Infusion. Can. J. Hosp. Pharm. 2004, 57, 276–282. [Google Scholar] [CrossRef]
- Jamieson, C.; Ozolina, L.; Seaton, R.A.; Gilchrist, M.; Hills, T.; Drummond, F.; Wilkinson, A.S.; BSAC Drug Stability Testing Working Group. Assessment of the Stability of Citrate-Buffered Piperacillin/Tazobactam for Continuous Infusion When Stored in Two Commercially Available Elastomeric Devices for Outpatient Parenteral Antimicrobial Chemotherapy: A Study Compliant with the NHS Yellow Cover Document Requirements. Eur. J. Hosp. Pharm. Sci. Pract. 2020. [Google Scholar] [CrossRef]
- Bird, A.E.; Charsley, C.H.; Jennings, K.R.; Marshall, A.C. High-Performance Liquid Chromatographic Assay of Temocillin and Epimerisation of Its Diastereoisomers. Analyst 1984, 109, 1209–1212. [Google Scholar] [CrossRef]
- Masse, M.; Genay, S.; Carta, N.; Delannoy-Rousselière, C.; Moreau, F.; Faure, K.; Barthélémy, C.; Decaudin, B.; Odou, P. Étude de La Stabilité de La Vancomycine à 40 Mg/ML Au Cours d’une Perfusion de 24 Heures [Poster Presentation]. In Proceedings of the Hopipharm: 65th French Hospital Pharmacy Congress, Nancy, France, 10–12 May 2017. [Google Scholar]
- International Conference on Harmonisation: Validation of Analytical Procedures: Text and Methodology Q2 (R1). Guideline 2005. Available online: http://www.ich.org/fileadmin/public_web_site/ich_products/guidelines/quality/q2_r1/step4/q2_r1__guideline.pdf (accessed on 24 March 2021).
- Bardin, C.; Astier, A.; Vulto, A.; Sewell, G.; Vigneron, J.; Trittler, R.; Daouphars, M.; Paul, M.; Trojniak, M.; Pinguet, F.; et al. Guidelines for the Practical Stability Studies of Anticancer Drugs: A European Consensus Conference. Ann. Pharm. Fr. 2011, 69, 221–231. [Google Scholar] [CrossRef] [PubMed]
- Pharmaceutical Technical Procedures, 2.9.19: Particulate Contamination: Sub-Visible Particles. In European Pharmacopoeia, 10th ed.; European Directorate for the Quality of Medicines and Health Care: Strasbourg, France, 2019; pp. 360–362.
| Antibiotic | Calibration Range (µg/mL) | R2 | Intra-Day Precision [min; max] (%) | Inter-Day Precision [min; max] (%) | Limit of Detection [µg/mL] | Cochran’s Test Cexp | ANOVA (Non-Linearity) Fexp |
|---|---|---|---|---|---|---|---|
| Amoxicillin | 120–280 | 0.9999 | [0.06; 0.66] | [0.57–0.75] | 0.13 | 0.344 | 0.15 |
| Aztreonam | 50–150 | 0.9997 | [0.08; 1.48] | [1.18; 1.95] | 0.51 | 0.399 | 0.93 |
| Cefazolin | 75–175 | 0.9999 | [0.15; 0.85] | [0.44; 0.57] | 0.11 | 0.609 | 0.38 |
| Cefepime | 60–140 | 0.9999 | [0.04; 0.83] | [1.15; 1.70] | 0.36 | 0.269 | 0.13 |
| Cefiderocol | 25–75 | 0.9999 | [0.05; 1.53] | [0.41; 0.99] | 0.10 | 0.424 | 0.07 |
| Cefotaxime | 50–150 | 0.9998 | [0.08; 1.81] | [1.09; 1.66] | 2.02 | 0.600 | 1.93 |
| Cefoxitin | 75–175 | 0.9993 | [0.17; 2.04] | [1.40; 1.80] | 0.53 | 0.420 | 0.66 |
| Ceftazidime | 100–500 | 0.9999 | [0.02; 1.53] | [0.28; 0.94] | 0.23 | 0.533 | 3.06 |
| Ceftazidime/Avibactam | 100–500 | 0.9999 | [0.24; 0.50] | [0.31; 1.05] | 2.43 | 0.551 | 0.21 |
| 25–125 | 0.9999 | [0.13; 0.43] | [0.33; 0.72] | 3.17 | 0.514 | 1.38 | |
| Ceftozolane/Tazobactam | 50–250 | 0.9999 | [0.07; 1.93] | [0.62; 1.47] | 0.77 | 0.579 | 0.26 |
| 25–125 | 0.9999 | [0.06; 2.04] | [0.63; 1.60] | 0.84 | 0.643 | 0.49 | |
| Cloxacillin | 1200–2800 | 0.9981 | [0.33; 1.81] | [1.25; 1;95] | 4.26 | 0.575 | 0.92 |
| Meropenem | 50–250 | 0.9999 | [0.06; 1.30] | [0.71; 1.13] | 0.19 | 0.659 | 0.64 |
| Piperacillin | 100–300 | 0.9999 | [0.01; 0.46] | [0.55; 1.10] | 0.34 | 0.555 | 0.06 |
| Piperacillin/Tazobactam | 100–500 | 0.9999 | [0.12; 1.33] | [0.38; 1.62] | 0.23 | 0.599 | 0.99 |
| 12.5–62.5 | 0.9999 | [0.01; 1.28] | [0.76; 1.44] | 0.36 | 0.554 | 0.14 | |
| Temocillin | 50–250 | 0.9999 | [0.05; 1.72] | [0.91; 2.02] | 0.64 | 0.331 | 0.04 |
| Vancomycin | 50–150 | 0.9995 | [0.03; 1.65] | [1.70; 2.48] | 2.91 | 0.389 | 2.27 |
| Mean % of Initial Concentration ± RSD * % | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Antibiotic | Conc. | Solvent | T0 h | T4 h | T6 h | T8 h | T12 h | T24 h | T48 h |
| Amoxicillin ** | 20 mg/mL | NS | 100 ± 1.19 | - | 96.7 ± 1.77 | - | 94.1 ± 0.66 | 87.5 ± 0.45 | 78.5 ± 1.52 |
| Aztreonam | 125 mg/mL | NS *** | 100.0 ± 2.38 | - | 98.7 ± 0.90 | - | - | 95.3 ± 1.79 | 92.7 ± 1.95 |
| D5W **** | 100.0 ± 0.47 | - | 99.5 ± 0.77 | - | - | 98.1 ± 1.42 | 95.7 ± 0.57 | ||
| Cefazolin | 125 mg/mL | NS | 100.0 ± 2.35 | - | 103.3 ± 1.67 | - | - | 100.0 ± 1.98 | 100.6 ± 1.95 |
| D5W | 100.0 ± 0.91 | - | 99.8 ± 3.11 | - | - | 99.4 ± 1.99 | 97.7 ± 2.10 | ||
| Cefepime | 110 mg/mL | NS | 100.0 ± 2.15 | - | 98.1 ± 0.61 | - | - | 94.8 ± 1.85 | 87.3 ± 0.82 |
| D5W | 100.0 ± 1.78 | - | 94.7 ± 0.93 | - | - | 90.6 ± 0.43 | 85.5 ± 1.80 | ||
| Cefiderocol | 62.5 mg/mL | NS | 100.0 ± 1.30 | - | - | - | 94.2 ± 1.11 | 91.6 ± 0.98 | 85.7 ± 2.24 |
| D5W | 100.0 ± 1.43 | - | - | - | 97.4 ± 0.68 | 94.0 ± 0.73 | 87.1 ± 0.53 | ||
| Cefotaxime | 83.3 mg/mL | NS | 100.0 ± 2.15 | - | 95.3 ± 1.50 | - | 92.2 ± 1.93 | 87.2 ± 2.05 | - |
| D5W | 100.0 ± 1.48 | - | 95.4 ± 1.04 | - | 93.0 ± 1.43 | 88.3 ± 1.45 | - | ||
| 125 mg/mL | NS | 100.0 ± 1.70 | - | 95.7 ± 1.38 | - | 95.2 ± 1.23 | 51.4 ± 1.53 | - | |
| D5W | 100.0 ± 1.21 | - | 97.4 ± 2.00 | - | 94.9 ± 1.18 | - | - | ||
| Cefoxitin | 125 mg/mL | NS | 100.0 ± 1.88 | - | 99.5 ± 0.79 | - | 97.3 ± 3.73 | 94.4 ± 1.60 | 89.8 ± 2.03 |
| D5W | 100.0 ± 1.79 | - | 98.9 ± 1.32 | - | 96.4 ± 3.00 | 93.8 ± 1.80 | 89.6 ± 2.14 | ||
| Ceftazidime | 125 mg/mL | NS | 100.0 ± 0.94 | - | - | 98.3 ± 2.04 | - | 94.9 ± 1.80 | 86.5 ± 1.89 |
| D5W | 100.0 ± 1.69 | - | - | 95.1 ± 1.06 | - | 89.0 ± 0.78 | 82.2 ± 0.44 | ||
| Ceftazidime | 125 mg/mL | NS | 100.0 ± 0.98 | - | - | - | 96.7 ± 0.31 | 95.2 ± 1.33 | 87.4 ± 1.22 |
| D5W | 100.0 ± 1.26 | - | - | - | 98.1 ± 0.86 | 91.7 ± 0.55 | 87.1 ± 1.36 | ||
| Avibactam | 31.25 mg/mL | NS | 100.0 ± 0.86 | - | - | - | 96.4 ± 0.91 | 96.2 ± 1.77 | 91.0 ± 0.89 |
| D5W | 100.0 ± 1.47 | - | - | - | 99.1 ± 0.79 | 94.7 ± 0.77 | 93.0 ± 1.41 | ||
| Ceftozolane | 62.5 mg/mL | NS | 100.0 ± 2.15 | - | - | 96.4 ± 2.25 | - | 93.9 ± 2.25 | 91.8 ± 1.52 |
| D5W | 100.0 ± 1.92 | - | - | 98.5 ± 1.55 | - | 96.2 ± 2.50 | 92.8 ± 0.54 | ||
| Tazobactam | 31.25 mg/mL | NS | 100.0 ± 2.27 | - | - | 98.0 ± 2.57 | - | 99.0 ± 2.30 | 101.0 ± 2.34 |
| D5W | 100.0 ± 2.09 | - | - | 100.0 ± 1.79 | - | 101.3 ± 2.74 | 102.3 ± 0.83 | ||
| Cloxacillin | 250 mg/mL | SWFI ***** | 100.0 ± 1.91 | - | 98.8 ± 1.70 | - | - | 96.2 ± 1.63 | 90.2 ± 1.45 |
| 125 mg/mL | NS | 100.0 ± 3.07 | - | 100.2 ± 1.93 | - | - | 97.2 ± 3.01 | 90.5 ± 2.73 | |
| D5W | 100.0 ± 1.48 | - | 100.0 ± 2.06 | - | - | 97.3 ± 1.47 | 90.1 ± 1.21 | ||
| Meropenem | 41.7 mg/mL | NS | 100.0 ± 1.59 | 97.1 ± 0.66 | - | 93.0 ± 0.93 | - | - | - |
| D5W | 100.0 ± 1.52 | 93.8 ± 0.68 | - | 85.9 ± 0.74 | - | - | - | ||
| Piperacillin | 125 mg/mL | NS | 100.0 ± 0.87 | - | 97.6 ± 0.24 | - | - | 92.8 ± 2.05 | 88.9 ± 1.37 |
| D5W | 100.0 ± 1.11 | - | 100.0 ± 1.97 | - | - | 98.3 ± 1.23 | 97.5 ± 1.26 | ||
| Piperacillin | 125 mg/mL | NS | 100.0 ± 0.96 | - | - | 101.3 ± 0.44 | - | 101 ± 1.26 | 98.1 ± 1.45 |
| D5W | 100.0 ± 2.34 | - | - | 97.1 ± 0.59 | - | 95.9 ± 1.05 | 93.5 ± 0.68 | ||
| Tazobactam | 15.6 mg/mL | NS | 100.0 ± 1.16 | - | - | 100.8 ± 0.40 | - | 101.1 ± 1.56 | 99.4 ± 1.52 |
| D5W | 100.0 ± 2.26 | - | - | 96.3 ± 0.36 | - | 96.7 ± 1.49 | 95.1 ± 1.22 | ||
| Temocillin | Unrealized in syringe | ||||||||
| Vancomycin | 62.5 mg/mL | NS | 100.0 ± 1.65 | - | 99.8 ± 1.17 | - | - | 100.7 ± 1.05 | 99.5 ± 1.27 |
| D5W | 100.0 ± 0.50 | - | 99.3 ± 1.03 | - | - | 98.2 ± 1.34 | 94.6 ± 2.88 | ||
| 83.3 mg/mL | NS | 100.0 ± 1.84 | - | 99.4 ± 1.28 | - | - | 98.4 ± 2.06 | - | |
| D5W | 100.0 ± 1.62 | - | 100.8 ± 0.92 | - | - | 96.0 ± 6.31 | 101.0 ± 0.86 | ||
| Mean % of Initial Concentration ± RSD * | ||||||||
|---|---|---|---|---|---|---|---|---|
| Antibiotic | Conc. | Solvent NS/D5W | T0 h | T6 h | T8 h | T12 h | T24 h | T48 h |
| Aztreonam | 50 mg/mL | NS ** | 100.0 ± 1.97 | - | - | - | 102.5 ± 3.39 | 100.2 ± 2.17 |
| D5W *** | 100.0 ± 1.64 | - | - | - | 101.7 ± 1.67 | 95.3 ± 2.96 | ||
| Cefazolin | 50 mg/mL | NS | Unstable, precipitate formation during pre-study | |||||
| D5W | ||||||||
| Cefepim | 50 mg/mL | NS | 100.0 ± 1.43 | 93.2 ± 2.00 | - | - | 83.3 ± 2.28 | 59.5 ± 2.21 |
| Cefiderocol | Unrealized in elastomeric device | |||||||
| Cefotaxime | 25 mg/mL | NS | Unstable, colour change after 6 h during pre-study | |||||
| D5W | ||||||||
| Cefoxitine | 25 mg/mL | NS | Unstable, Colour change after 12 h during pre-study | |||||
| D5W | ||||||||
| Ceftazidime | 25 mg/mL | NS | 100.0 ± 3.22 | - | 95.2 ± 1.56 | - | 85.6 ± 2.24 | - |
| D5W | 100.0 ± 2.94 | - | 94.8 ± 3.29 | - | 77.5 ± 1.94 | - | ||
| Ceftazidime | 25 mg/mL | NS | 100.0 ± 3.35 | - | - | 92.2 ± 2.86 | 82.3 ± 2.28 | 66.3 ± 1.90 |
| D5W | 100.0 ± 7.35 | - | - | 86.2 ± 6.54 | 75.4 ± 7.53 | 58.1 ± 8.56 | ||
| Avibactam | 6.25 mg/mL | NS | 100.0 ± 4.59 | - | - | 98.4 ± 4.08 | 96.5 ± 2.95 | 93.9 ± 2.95 |
| D5W | 100.0 ± 7.81 | - | - | 95.4 ± 6.92 | 93.9 ± 7.46 | 90.3 ± 8.35 | ||
| Ceftozolane | 25 mg/mL | NS | 100.0 ± 1.80 | - | 100.0 ± 1.20 | - | 91.8 ± 0.95 | 81.4 ± 3.67 |
| D5W | 100.0 ± 0.99 | - | 97.5 ± 0.85 | - | 89.3 ± 2.11 | 81.7 ± 6.02 | ||
| Tazobactam | 12.5 mg/mL | NS | 100.0 ± 2.08 | - | 104.6 ± 1.47 | - | 109.2 ± 1.33 | 116.7 ± 3.02 |
| D5W | 100.0 ± 0.99 | - | 103.1 ± 0.82 | - | 109.5 ± 1.33 | 116.6 ± 1.83 | ||
| Cloxacillin | 50–100 mg/mL | NS | Unstable, precipitate formation during pre-study | |||||
| D5W | ||||||||
| Meropenem | Unrealized in elastomeric device | |||||||
| Piperacillin | 66.7 mg/mL | NS | Unstable, precipitate formation during pre-study | |||||
| D5W | ||||||||
| Piperacilline | 66.7 mg/mL | NS | 100.0 ± 2.17 | - | 98.5 ± 0.46 | - | 93.6 ± 1.06 | 85.7 ± 1.92 |
| D5W | 100.0 ± 0.74 | - | 97.9 ± 0.87 | - | 93.6 ± 0.60 | 84.1 ± 0.17 | ||
| Tazobactam | 8.3 mg/mL | NS | 100.0 ± 2.26 | - | 98.9 ± 0.53 | - | 97.0 ± 0.93 | 96.2 ± 1.58 |
| D5W | 100.0 ± 0.78 | - | 98.7 ± 0.90 | - | 98.2 ± 0.55 | 95.8 ± 0.25 | ||
| Temocillin | 25 mg/mL | NS | 100.0 ± 2.37 | - | - | - | 92.6 ± 2.95 | 80.4 ± 2.84 |
| D5W | 100.0 ± 2.36 | - | - | - | 87.5 ± 2.23 | 78.8 ± 2.61 | ||
| Vancomycin | 37.5 mg/mL | NS | 100.0 ± 2.06 | - | - | - | 97.9 ± 2.91 | 98.3 ± 3.26 |
| D5W | 100.0 ± 2.70 | - | - | - | 101.0 ± 1.61 | 103.3 ± 1.54 | ||
| Tradename/Manufacturer | Batch Number | |
|---|---|---|
| Amoxicillin | Amoxicilline PANPHARMA 1 g | 307197 |
| Aztreonam | AZACTAM® 1 g SANOFI-AVENTIS | ABC7060 |
| Cefazolin | Céfazoline MYLAN 2 g | 200902–200903 |
| Cefepime | Céfépime MYLAN 2 g | 4M2119FR |
| Cefiderocol | FETCROJA® 1 g SHIONOGI | FEFR0120 |
| Cefotaxime | Céfotaxime MYLAN 2 g | R3052 |
| Cefoxitin | Céfoxitine PANPHARMA 2 g | N4-03 |
| Ceftazidime | Ceftazidime MYLAN 2 g | 191102 |
| Ceftazidime/Avibactam | ZAVICEFTA® 2/0.5 g PFIZER | 3M05L95690 |
| Ceftozolane/Tazobactam | ZERBAXA® 1/0.5 g MERCK SHARP & DOHME BV | T003341 |
| Cloxacillin | ORBENINE® 1 g ASTELLAS | 25AND02/ 25AQF03 |
| Meropenem | Méropénem PANPHARMA 1 g | MFR1020 |
| Piperacillin | Pipéracilline PANPHARMA 4 g Pipéracilline PANPHARMA 1 g | 306609–306699 306421 |
| Piperacillin/Tazobactam | Pipéracilline/tazobactam PANPHARMA 4/0.5 g | 306584 |
| Temocillin | NEGABAN® 1 g EUMEDICA NEGABAN® 2 g | L154510 L162439 |
| Vancomycin | Vancomycine SANDOZ 1 g | EC0107 |
| Antibiotic | Polyolefin Bag (100 mL, 20–25 °C) | Syringe (48 mL, 20–25 °C) | Elastomeric Device (37 °C) | |||
|---|---|---|---|---|---|---|
| Amount (g) | Solvent | Amount (g) | Solvent | Amount (g) | Solvent | |
| (Concentration mg/mL) | (Concentration mg/mL) | (Concentration mg/mL) | ||||
| Amoxicillin | 2 g 20 mg/mL | NS * | Unrealized | |||
| Aztreonam | Unrealized | 6 g (125 mg/mL) | NS—D5W ** | 6 g (120 mL) (50 mg/mL) | NS—D5W | |
| Cefazolin | Unrealized | 6 g (125 mg/mL) | NS—D5W | 6 g (120 mL) (50 mg/mL) | NS—D5W | |
| Cefepime | Unrealized | 6 g (125 mg/mL) | NS—D5W | 6 g (120 mL) (50 mg/mL) | NS | |
| Cefiderocol | Unrealized | 3 g (62.5 mg/mL) | NS—D5W | 6 g (240 mL) (25 mg/mL) | NS—D5W | |
| Cefotaxime | Unrealized | 4 g (83.3 mg/mL) | NS—D5W | 6 g (240 mL) (25 mg/mL) | NS—D5W | |
| 6 g (125 mg/mL) | NS—D5W | |||||
| Cefoxitin | Unrealized | 6 g (125 mg/mL) | NS—D5W | 6 g (240 mL) (25 mg/mL) | NS—D5W | |
| Ceftazidime | Unrealized | 6 g (125 mg/mL) | NS—D5W | 3 g (120 mL) (25 mg/mL) | NS—D5W | |
| Ceftazidime/Avibactam | Unrealized | 6/1.5 g (125/31.25 mg/mL) | NS—D5W | 3/0.75 g (120 mL) (25/6.25 mg/mL) | NS- D5W | |
| Ceftozolane/Tazobactam | Unrealized | 3/1.5 g (62.5/31.25 mg/mL) | NS—D5W | 3/1.5 g (120 mL) (25/12.5 mg/mL) | NS—D5W | |
| Cloxacillin | Unrealized | 12 g (250 mg/mL) | SWFI *** | 12 g (120 mL) (100 mg/mL) 12 g (240 mL) (50 mg/mL) | NS—D5W | |
| 6 g (125 mg/mL) | NS—D5W | |||||
| Meropenem | Unrealized | 2 g (41.7 mg/mL) | NS—D5W | Unrealized | ||
| Piperacillin | Unrealized | 6 g (125 mg/mL) | NS—D5W | 16 g (240 mL) (66.7 mg/mL) | NS—D5W | |
| Piperacillin/Tazobactam | Unrealized | 6/0.75 g (125/15.6 mg/mL) | NS—D5W | 16 g/2 (240 mL) (66.7/8.3 mg/mL) | NS—D5W | |
| Temocillin | Unrealized | Unrealized 1 | 6 g (240 mL) (25 mg/mL) | NS—D5W | ||
| Vancomycin | Unrealized | 3 g (62.5 mg/mL) | NS—D5W | 4.5 g (120 mL) (37.5 mg/mL) | NS—D5W | |
| Unrealized | 4 g (83.3 mg/mL) | |||||
| Antibiotic | Mobile Phase (v/v) | pH | Flow Rate (mL/min) | Injection Volume (µL) | Wavelength (nm) | Retention Time (min) | Reference |
|---|---|---|---|---|---|---|---|
| Amoxicillin | Isocratic: NaH2PO4 buffer 0.05 M/methanol (95/5) | 4.4 | 1.0 | 50 | 220 | 4.45 | [26] |
| Aztreonam | Isocratic: KH2PO4 buffer 0.05 M/methanol (90/10) | 3.0 | 1.0 | 20 | 270 | 6.9 | [27] |
| Cefazolin | Isocratic: KH2PO4 buffer 0.005 M/methanol (80/20) | 7.5 | 1.0 | 50 | 272 | 3.0 | [28] |
| Cefepime | Isocratic: KH2PO4 buffer 0.005 M/methanol (90/10) | 7.5 | 1.0 | 50 | 257 | 3.8 | [28] |
| Cefiderocol | Gradient: KH2PO4 buffer 0.05 M (A) + methanol (B) T0 to T7 min gradual increase 83/17 (A/B) to 70/30; T7 to T15 min: 70/30; T16 to T20 min: 83/17 | 3.0 | 1.5 | 50 | 260 | 5.9 | [29] |
| Cefotaxime | Gradient: Na2HPO4 buffer 0.05 M/methanol (86/14) (A); Na2HPO4 buffer 0.05 M/methanol (60/40) (B) T0 to T7 min: 100/0 (A/B); T9 to T16 min: 80/20; T16 to T30 min: gradual increase until 41.4/58.6; T35 to T40 min: 100/0 | 6.25 | 1.3 | 10 | 235 | 9.0 | [30] |
| Cefoxitin | Isocratic: KH2PO4 buffer 0.005 M/methanol (80/20) | 7.5 | 1.0 | 10 | 272 | 3.2 | [28] |
| Ceftazidime | Isocratic: ammonium acetate 0.1 M/acetonitrile 90/10 | 7.5 | 1.0 | 20 | 260 | 4.1 | [31] |
| Ceftazidime/Avibactam | Gradient: KH2PO4 buffer 0.05 M (A) + methanol (B) T0 to T4 min: 99/1 (A/B); T9 to T28 min: 90/10; T36 to T40 min: 99/1 | 3 | 1.5 | 20 | 260 | 20.3/1.6 | [32] |
| Ceftozolane/Tazobactam | Isocratic: KH2PO4 buffer 0.005 M/acetonitrile (1000/26) | 3.4 | 1.0 | 20 | 220 | 8.7/4.8 | [33] |
| Cloxacillin | Isocratic: triethylamine + tetrabutylammonium buffer/methanol (35/65) | 6 | 0.5 | 5 | 250 | 4.5 | [34] |
| Meropenem | Isocratic: ammonium acetate 10.53 mM /acetonitrile (95/5) | 3.0 | 1.0 | 20 | 297 | 8.1 | [35] |
| Piperacillin | Isocratic: KH2PO4 buffer 0.05 M/acetonitrile (55/45) | 3.0 | 1.0 | 2 | 230 | 3.4 | [36] |
| Piperacillin/Tazobactam | Gradient: KH2PO4 0.02 M (A)/acetonitrile (B) T0 to T5 min: 92.5/7.5 (A/B); T10 to T15 min: 70/30; T20 to T25 min: 92.5/7.5 | 2.5 | 1.5 | 10 | 210/280 | 13.5/ | [37] |
| 2.2 | |||||||
| Temocillin | Isocratic: KH2PO4 buffer 0.1 M/methanol (93/7) | 7.0 | 1.0 | 20 | 230 | 7.6 and 9.2 | [38] |
| Vancomycin | Isocratic: KH2PO4 buffer 0.1 M/acetonitrile (92/8) | 3.5 | 1.5 | 10 | 220 | 7.2 | [39] |
| Antibiotic | Syringe (48 mL, 25 °C), Polyolefin Bags * (100 mL, 25 °C) | Diffuser (37 °C) | ||||
|---|---|---|---|---|---|---|
| Amount (g) | Solvent | Stability (Hours) | Amount (g) | Solvent | Stability (Hours) | |
| (Concentration) | (Concentration) | |||||
| Amoxicillin * | 2 g (100 mL) (20 mg/mL) | NS ** | 12 h | Unrealized in elastomeric device | ||
| Aztreonam | 6 g | NS-D5W *** | 48 h | 6 g (120 mL) (50 mg/mL) | NS-D5W | 48 h |
| (125 mg/mL) | ||||||
| Cefazolin | 6 g | NS-D5W | 24 h | 6 g (120 mL) (50 mg/mL) | NS-D5W | Precipitate formation during the pre-study |
| (125 mg/mL) | ||||||
| Cefepime | 6 g | NS-D5W | 24 h | 6 g (120 mL) (50 mg/mL) | NS | Visual modification after 6 h at 37 °C |
| (125 mg/mL) | ||||||
| Cefiderocol | 3 g | NS-D5W | 24 h | 6 g (240 mL) (25 mg/mL) | NS- D5W | 6 h |
| (62.5 mg/mL) | ||||||
| Cefotaxime | 4 g–6 g | NS-D5W | 6 h | 6 g (240 mL) (25 mg/mL) | NS-D5W | Colour change after 6 h during the pre-study |
| (83.3–125 mg/mL) | ||||||
| Cefoxitin | 6 g | D5W | 12 h | 6 g (240 mL) (25 mg/mL) | NS-D5W | Instability during the pre-study |
| (125 mg/mL) | ||||||
| Ceftazidime | 6 g | NS | 24 h | 3 g (120 mL) (25 mg/mL) | NS-D5W | 8 h |
| (125 mg/mL) | D5W | 8 h | ||||
| Ceftazidime/ | 6/1.5 g | NS-D5W | 24 h | 3/0.75 g (120 mL) | NS | 12 h |
| Avibactam | (125/31.25 mg/mL) | (25/6.25 mg/mL) | D5W | Unstable | ||
| Ceftozolane/ | 3/1.5 g | NS-D5W | 48 h | 3/1.5 g (120 mL) | NS D5W | 12 h 8 h |
| Tazobactam | (62.5/31.25 mg/mL) | (25/12.5 mg/mL) | ||||
| Cloxacillin | 12 g | SWFI **** | 24 h | 6–12 g (120 mL) (50–100 mg/mL) | NS-D5W | Precipitate formation during the pre-study |
| (250 mg/mL) | ||||||
| 6 g | NS-D5W | 24 h | ||||
| (125 mg/mL) | ||||||
| Meropenem | 2 g | NS | 8 h | Unrealized in elastomeric device | ||
| (41.7 mg/mL) | D5W | 4 h | ||||
| Piperacillin | 6 g | NS | 24 h | 16 g (240 mL) (66.7 mg/mL) | NS-D5W | Instability during the pre-study |
| (125 mg/mL) | D5W | 48 h | ||||
| Piperacillin / | 6/0.75 g | NS-D5W | 48 h | 16/2 g (240 mL) | NS | 8 h |
| Tazobactam | (125/15.6 mg/mL) | (66.7/8.3 mg/mL) | D5W | 24 h | ||
| Temocillin | Unrealized | 6 g (240 mL) | NS | 24 h | ||
| (25 mg/mL) | D5W | Unstable | ||||
| Vancomycin | 3 g | D5W | 48 h | 4,5 g (120 mL) (37.5 mg/mL) | NS-D5W | 48 h |
| (62.5 mg/mL) | ||||||
| 4 g | D5W | 48 h | ||||
| (83.3 mg/mL) | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Loeuille, G.; D’Huart, E.; Vigneron, J.; Nisse, Y.-E.; Beiler, B.; Polo, C.; Ayari, G.; Sacrez, M.; Demoré, B.; Charmillon, A. Stability Studies of 16 Antibiotics for Continuous Infusion in Intensive Care Units and for Performing Outpatient Parenteral Antimicrobial Therapy. Antibiotics 2022, 11, 458. https://doi.org/10.3390/antibiotics11040458
Loeuille G, D’Huart E, Vigneron J, Nisse Y-E, Beiler B, Polo C, Ayari G, Sacrez M, Demoré B, Charmillon A. Stability Studies of 16 Antibiotics for Continuous Infusion in Intensive Care Units and for Performing Outpatient Parenteral Antimicrobial Therapy. Antibiotics. 2022; 11(4):458. https://doi.org/10.3390/antibiotics11040458
Chicago/Turabian StyleLoeuille, Guillaume, Elise D’Huart, Jean Vigneron, Yann-Eric Nisse, Benoit Beiler, Caroline Polo, Gillian Ayari, Matthieu Sacrez, Béatrice Demoré, and Alexandre Charmillon. 2022. "Stability Studies of 16 Antibiotics for Continuous Infusion in Intensive Care Units and for Performing Outpatient Parenteral Antimicrobial Therapy" Antibiotics 11, no. 4: 458. https://doi.org/10.3390/antibiotics11040458
APA StyleLoeuille, G., D’Huart, E., Vigneron, J., Nisse, Y.-E., Beiler, B., Polo, C., Ayari, G., Sacrez, M., Demoré, B., & Charmillon, A. (2022). Stability Studies of 16 Antibiotics for Continuous Infusion in Intensive Care Units and for Performing Outpatient Parenteral Antimicrobial Therapy. Antibiotics, 11(4), 458. https://doi.org/10.3390/antibiotics11040458





