A Narrative Review on the Approach to Antimicrobial Use in Ventilated Patients with Multidrug Resistant Organisms in Respiratory Samples—To Treat or Not to Treat? That Is the Question
Abstract
:1. Introduction
2. Literature Search
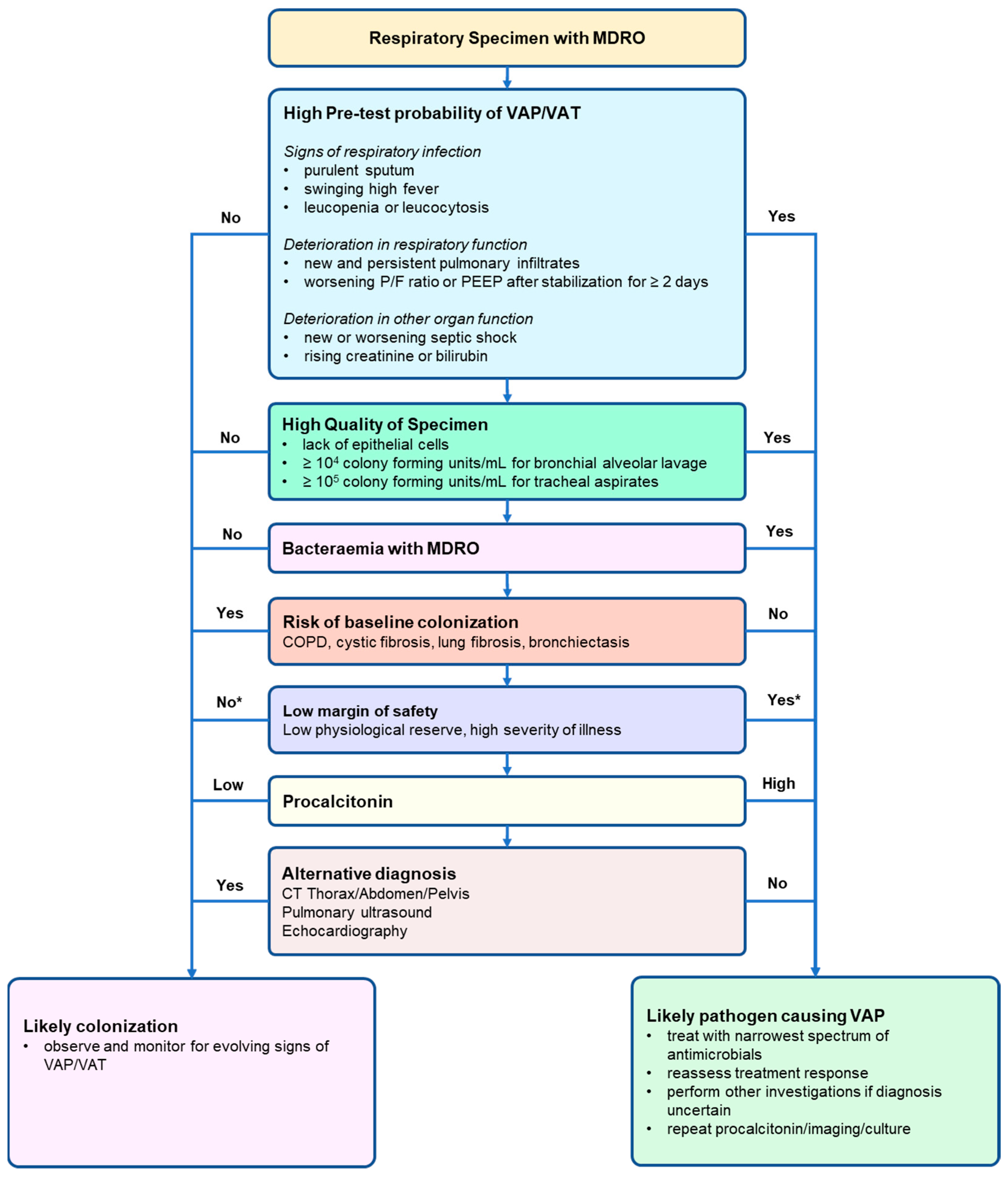
3. Definition of VAP/VAT
4. Characteristics of Respiratory Specimens
5. Severity of Illness
6. Infection and Inflammatory Markers
7. Comorbidities
8. Alternative Diagnoses
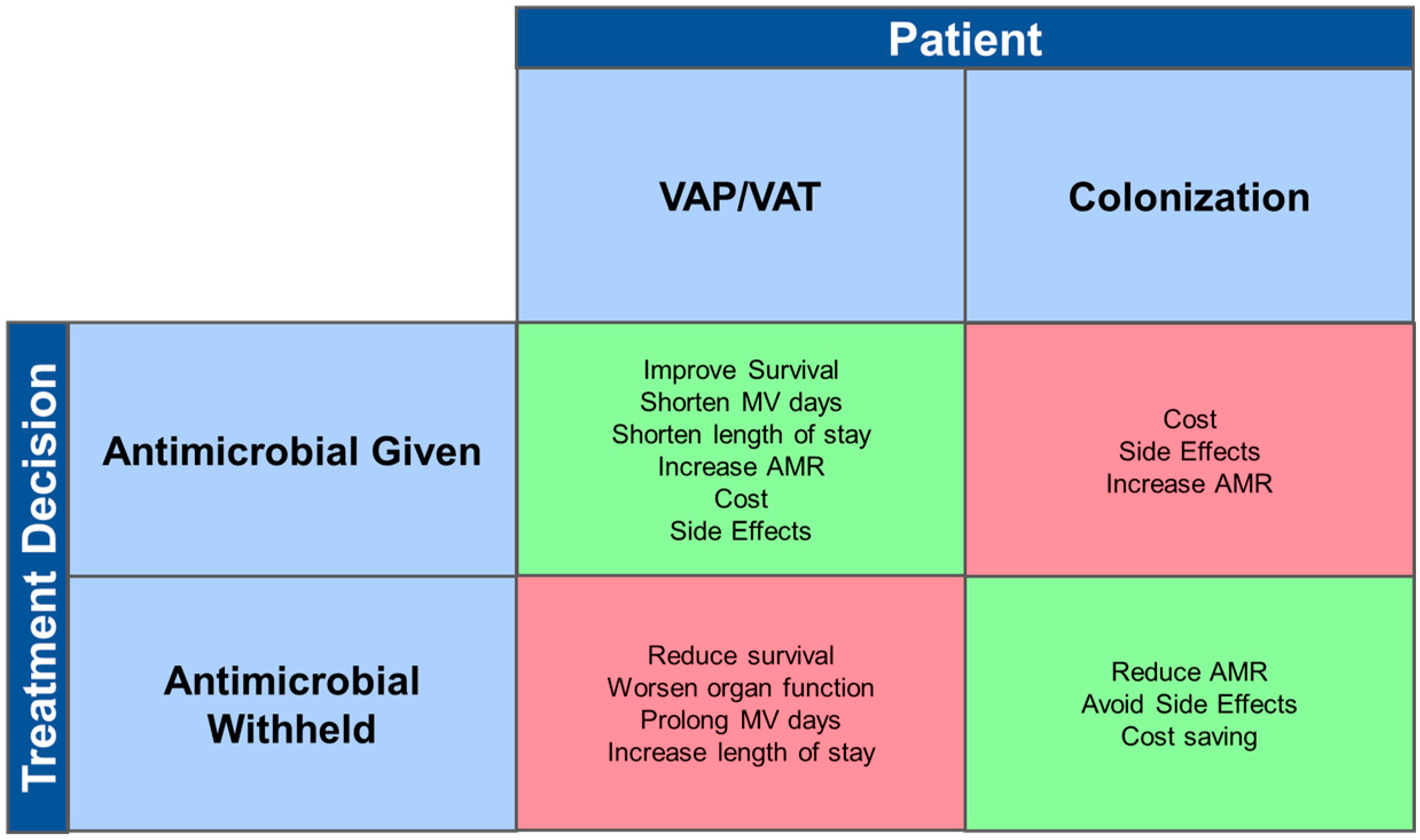
9. A Practical Approach to Management
10. Limitations
11. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Richards, M.J.; Edwards, J.R.; Culver, D.H.; Gaynes, R.P. Nosocomial infections in combined medical-surgical intensive care units in the United States. Infect. Control Hosp. Epidemiol. 2000, 21, 510–515. [Google Scholar] [CrossRef] [PubMed]
- Nseir, S.; Di Pompeo, C.; Pronnier, P.; Beague, S.; Onimus, T.; Saulnier, F.; Grandbastien, B.; Mathieu, D.; Delvallez-Roussel, M.; Durocher, A. Nosocomial tracheobronchitis in mechanically ventilated patients: Incidence, aetiology and outcome. Eur. Respir. J. 2002, 20, 1483–1489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dallas, J.; Skrupky, L.; Abebe, N.; Boyle, W.A., 3rd; Kollef, M.H. Ventilator-associated tracheobronchitis in a mixed surgical and medical ICU population. Chest 2011, 139, 513–518. [Google Scholar] [CrossRef]
- Luckraz, H.; Manga, N.; Senanayake, E.L.; Abdelaziz, M.; Gopal, S.; Charman, S.C.; Giri, R.; Oppong, R.; Andronis, L. Cost of treating ventilator-associated pneumonia post cardiac surgery in the National Health Service: Results from a propensity-matched cohort study. J. Intensive Care Soc. 2018, 19, 94–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Melsen, W.G.; Rovers, M.M.; Groenwold, R.H.; Bergmans, D.C.; Camus, C.; Bauer, T.T.; Hanisch, E.W.; Klarin, B.; Koeman, M.; Krueger, W.A.; et al. Attributable mortality of ventilator-associated pneumonia: A meta-analysis of individual patient data from randomised prevention studies. Lancet Infect. Dis. 2013, 13, 665–671. [Google Scholar] [CrossRef]
- Papazian, L.; Klompas, M.; Luyt, C.E. Ventilator-associated pneumonia in adults: A narrative review. Intensive Care Med. 2020, 46, 888–906. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Safdar, N.; Dezfulian, C.; Collard, H.R.; Saint, S. Clinical and economic consequences of ventilator-associated pneumonia: A systematic review. Crit. Care Med. 2005, 33, 2184–2193. [Google Scholar] [CrossRef]
- Melsen, W.G.; Rovers, M.M.; Koeman, M.; Bonten, M.J. Estimating the attributable mortality of ventilator-associated pneumonia from randomized prevention studies. Crit. Care Med. 2011, 39, 2736–2742. [Google Scholar] [CrossRef]
- Agrafiotis, M.; Siempos, I.I.; Falagas, M.E. Frequency, prevention, outcome and treatment of ventilator-associated tracheobronchitis: Systematic review and meta-analysis. Respir. Med. 2010, 104, 325–336. [Google Scholar] [CrossRef] [Green Version]
- Kharel, S.; Bist, A.; Mishra, S.K. Ventilator-associated pneumonia among ICU patients in WHO Southeast Asian region: A systematic review. PLoS ONE 2021, 16, e0247832. [Google Scholar] [CrossRef]
- Skrupky, L.P.; McConnell, K.; Dallas, J.; Kollef, M.H. A comparison of ventilator-associated pneumonia rates as identified according to the National Healthcare Safety Network and American College of Chest Physicians criteria. Crit. Care Med. 2012, 40, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Cassini, A.; Hogberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef] [Green Version]
- Grasselli, G.; Scaravilli, V.; Mangioni, D.; Scudeller, L.; Alagna, L.; Bartoletti, M.; Bellani, G.; Biagioni, E.; Bonfanti, P.; Bottino, N.; et al. Hospital-Acquired Infections in Critically Ill Patients With COVID-19. Chest 2021, 160, 454–465. [Google Scholar] [CrossRef]
- Sangale, A.; Vivek, B.; Kelkar, R.; Biswas, S. Microbiology of Ventilator-associated Pneumonia in a Tertiary Care Cancer Hospital. Indian J. Crit. Care Med. 2021, 25, 421–428. [Google Scholar] [CrossRef]
- Giantsou, E.; Liratzopoulos, N.; Efraimidou, E.; Panopoulou, M.; Alepopoulou, E.; Kartali-Ktenidou, S.; Minopoulos, G.I.; Zakynthinos, S.; Manolas, K.I. Both early-onset and late-onset ventilator-associated pneumonia are caused mainly by potentially multiresistant bacteria. Intensive Care Med. 2005, 31, 1488–1494. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; Sakr, Y.; Singer, M.; Martin-Loeches, I.; Machado, F.R.; Marshall, J.C.; Finfer, S.; Pelosi, P.; Brazzi, L.; Aditianingsih, D.; et al. Prevalence and Outcomes of Infection Among Patients in Intensive Care Units in 2017. JAMA 2020, 323, 1478–1487. [Google Scholar] [CrossRef] [PubMed]
- Tedja, R.; Nowacki, A.; Fraser, T.; Fatica, C.; Griffiths, L.; Gordon, S.; Isada, C.; van Duin, D. The impact of multidrug resistance on outcomes in ventilator-associated pneumonia. Am. J. Infect. Control 2014, 42, 542–545. [Google Scholar] [CrossRef]
- Zheng, Y.L.; Wan, Y.F.; Zhou, L.Y.; Ye, M.L.; Liu, S.; Xu, C.Q.; He, Y.Q.; Chen, J.H. Risk factors and mortality of patients with nosocomial carbapenem-resistant Acinetobacter baumannii pneumonia. Am. J. Infect. Control 2013, 41, e59–e63. [Google Scholar] [CrossRef]
- Tuon, F.F.; Graf, M.E.; Merlini, A.; Rocha, J.L.; Stallbaum, S.; Arend, L.N.; Pecoit-Filho, R. Risk factors for mortality in patients with ventilator-associated pneumonia caused by carbapenem-resistant Enterobacteriaceae. Braz. J. Infect. Dis. 2017, 21, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Baccolini, V.; Migliara, G.; Isonne, C.; Dorelli, B.; Barone, L.C.; Giannini, D.; Marotta, D.; Marte, M.; Mazzalai, E.; Alessandri, F.; et al. The impact of the COVID-19 pandemic on healthcare-associated infections in intensive care unit patients: A retrospective cohort study. Antimicrob. Resist. Infect. Control 2021, 10, 87. [Google Scholar] [CrossRef]
- Koulenti, D.; Arvaniti, K.; Judd, M.; Lalos, N.; Tjoeng, I.; Xu, E.; Armaganidis, A.; Lipman, J. Ventilator-Associated Tracheobronchitis: To Treat or Not to Treat? Antibiotics 2020, 9, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iregui, M.; Ward, S.; Sherman, G.; Fraser, V.J.; Kollef, M.H. Clinical importance of delays in the initiation of appropriate antibiotic treatment for ventilator-associated pneumonia. Chest 2002, 122, 262–268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nseir, S.; Favory, R.; Jozefowicz, E.; Decamps, F.; Dewavrin, F.; Brunin, G.; Di Pompeo, C.; Mathieu, D.; Durocher, A.; Group, V.A.T.S. Antimicrobial treatment for ventilator-associated tracheobronchitis: A randomized, controlled, multicenter study. Crit. Care 2008, 12, R62. [Google Scholar] [CrossRef] [Green Version]
- Arulkumaran, N.; Routledge, M.; Schlebusch, S.; Lipman, J.; Conway Morris, A. Antimicrobial-associated harm in critical care: A narrative review. Intensive Care Med. 2020, 46, 225–235. [Google Scholar] [CrossRef] [PubMed]
- Michael, C.A.; Dominey-Howes, D.; Labbate, M. The antimicrobial resistance crisis: Causes, consequences, and management. Front. Public Health 2014, 2, 145. [Google Scholar] [CrossRef] [PubMed]
- Armand-Lefevre, L.; Angebault, C.; Barbier, F.; Hamelet, E.; Defrance, G.; Ruppe, E.; Bronchard, R.; Lepeule, R.; Lucet, J.C.; El Mniai, A.; et al. Emergence of imipenem-resistant gram-negative bacilli in intestinal flora of intensive care patients. Antimicrob. Agents Chemother. 2013, 57, 1488–1495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trouillet, J.L.; Vuagnat, A.; Combes, A.; Kassis, N.; Chastre, J.; Gibert, C. Pseudomonas aeruginosa ventilator-associated pneumonia: Comparison of episodes due to piperacillin-resistant versus piperacillin-susceptible organisms. Clin. Infect. Dis. 2002, 34, 1047–1054. [Google Scholar] [CrossRef] [Green Version]
- Le Terrier, C.; Vinetti, M.; Bonjean, P.; Richard, R.; Jarrige, B.; Pons, B.; Madeux, B.; Piednoir, P.; Ardisson, F.; Elie, E.; et al. Impact of a restrictive antibiotic policy on the acquisition of extended-spectrum beta-lactamase-producing Enterobacteriaceae in an endemic region: A before-and-after, propensity-matched cohort study in a Caribbean intensive care unit. Crit. Care 2021, 25, 261. [Google Scholar] [CrossRef]
- Hranjec, T.; Rosenberger, L.H.; Swenson, B.; Metzger, R.; Flohr, T.R.; Politano, A.D.; Riccio, L.M.; Popovsky, K.A.; Sawyer, R.G. Aggressive versus conservative initiation of antimicrobial treatment in critically ill surgical patients with suspected intensive-care-unit-acquired infection: A quasi-experimental, before and after observational cohort study. Lancet Infect. Dis. 2012, 12, 774–780. [Google Scholar] [CrossRef] [Green Version]
- Chaïbi, K.; Péan de Ponfilly, G.; Dortet, L.; Zahar, J.-R.; Pilmis, B. Empiric Treatment in HAP/VAP: “Don’t You Want to Take a Leap of Faith?”. Antibiotics 2022, 11, 359. [Google Scholar] [CrossRef]
- Fabregas, N.; Ewig, S.; Torres, A.; El-Ebiary, M.; Ramirez, J.; de La Bellacasa, J.P.; Bauer, T.; Cabello, H. Clinical diagnosis of ventilator associated pneumonia revisited: Comparative validation using immediate post-mortem lung biopsies. Thorax 1999, 54, 867–873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corley, D.E.; Kirtland, S.H.; Winterbauer, R.H.; Hammar, S.P.; Dail, D.H.; Bauermeister, D.E.; Bolen, J.W. Reproducibility of the histologic diagnosis of pneumonia among a panel of four pathologists: Analysis of a gold standard. Chest 1997, 112, 458–465. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernando, S.M.; Tran, A.; Cheng, W.; Klompas, M.; Kyeremanteng, K.; Mehta, S.; English, S.W.; Muscedere, J.; Cook, D.J.; Torres, A.; et al. Diagnosis of ventilator-associated pneumonia in critically ill adult patients-a systematic review and meta-analysis. Intensive Care Med. 2020, 46, 1170–1179. [Google Scholar] [CrossRef] [PubMed]
- Butler, K.L.; Sinclair, K.E.; Henderson, V.J.; McKinney, G.; Mesidor, D.A.; Katon-Benitez, I.; Weaver, W.L. The chest radiograph in critically ill surgical patients is inaccurate in predicting ventilator-associated pneumonia. Am. Surg. 1999, 65, 805–809. [Google Scholar]
- Wunderink, R.G. Radiologic diagnosis of ventilator-associated pneumonia. Chest 2000, 117, 188S–190S. [Google Scholar] [CrossRef] [Green Version]
- Pugin, J.; Auckenthaler, R.; Mili, N.; Janssens, J.P.; Lew, P.D.; Suter, P.M. Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and nonbronchoscopic “blind” bronchoalveolar lavage fluid. Am. Rev. Respir. Dis. 1991, 143, 1121–1129. [Google Scholar] [CrossRef]
- Shan, J.; Chen, H.L.; Zhu, J.H. Diagnostic accuracy of clinical pulmonary infection score for ventilator-associated pneumonia: A meta-analysis. Respir. Care 2011, 56, 1087–1094. [Google Scholar] [CrossRef] [Green Version]
- Ventilator-Associated Event (VAE); National Healthcare Safety Network: Washington, DC, USA, 2022.
- Rahimibashar, F.; Miller, A.C.; Yaghoobi, M.H.; Vahedian-Azimi, A. A comparison of diagnostic algorithms and clinical parameters to diagnose ventilator-associated pneumonia: A prospective observational study. BMC Pulm. Med. 2021, 21, 161. [Google Scholar] [CrossRef]
- Lachiewicz, A.M.; Weber, D.J.; van Duin, D.; Carson, S.S.; DiBiase, L.M.; Jones, S.W.; Rutala, W.A.; Cairns, B.A.; Sickbert-Bennett, E.E. From VAP to VAE: Implications of the New CDC Definitions on a Burn Intensive Care Unit Population. Infect. Control Hosp. Epidemiol. 2017, 38, 867–869. [Google Scholar] [CrossRef]
- Panizo-Alcaniz, J.; Frutos-Vivar, F.; Thille, A.W.; Penuelas, O.; Aguilar-Rivilla, E.; Muriel, A.; Rodriguez-Barbero, J.M.; Jaramillo, C.; Nin, N.; Esteban, A. Diagnostic accuracy of portable chest radiograph in mechanically ventilated patients when compared with autopsy findings. J. Crit. Care 2020, 60, 6–9. [Google Scholar] [CrossRef]
- Lefcoe, M.S.; Fox, G.A.; Leasa, D.J.; Sparrow, R.K.; McCormack, D.G. Accuracy of portable chest radiography in the critical care setting. Diagnosis of pneumonia based on quantitative cultures obtained from protected brush catheter. Chest 1994, 105, 885–887. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Claessens, Y.E.; Debray, M.P.; Tubach, F.; Brun, A.L.; Rammaert, B.; Hausfater, P.; Naccache, J.M.; Ray, P.; Choquet, C.; Carette, M.F.; et al. Early Chest Computed Tomography Scan to Assist Diagnosis and Guide Treatment Decision for Suspected Community-acquired Pneumonia. Am. J. Respir. Crit. Care Med. 2015, 192, 974–982. [Google Scholar] [CrossRef] [PubMed]
- Bouhemad, B.; Dransart-Raye, O.; Mojoli, F.; Mongodi, S. Lung ultrasound for diagnosis and monitoring of ventilator-associated pneumonia. Ann. Transl. Med. 2018, 6, 418. [Google Scholar] [CrossRef] [PubMed]
- Long, L.; Zhao, H.T.; Zhang, Z.Y.; Wang, G.Y.; Zhao, H.L. Lung ultrasound for the diagnosis of pneumonia in adults: A meta-analysis. Medicine 2017, 96, e5713. [Google Scholar] [CrossRef]
- Craven, D.E.; Hjalmarson, K.I. Ventilator-associated tracheobronchitis and pneumonia: Thinking outside the box. Clin. Infect. Dis. 2010, 51 (Suppl. 1), S59–S66. [Google Scholar] [CrossRef] [PubMed]
- Gaudet, A.; Martin-Loeches, I.; Povoa, P.; Rodriguez, A.; Salluh, J.; Duhamel, A.; Nseir, S.; TAVeM Study Group. Accuracy of the clinical pulmonary infection score to differentiate ventilator-associated tracheobronchitis from ventilator-associated pneumonia. Ann. Intensive Care 2020, 10, 101. [Google Scholar] [CrossRef] [PubMed]
- Morris, A.J.; Tanner, D.C.; Reller, L.B. Rejection criteria for endotracheal aspirates from adults. J. Clin. Microbiol. 1993, 31, 1027–1029. [Google Scholar] [CrossRef] [Green Version]
- Danin, P.E.; Girou, E.; Legrand, P.; Louis, B.; Fodil, R.; Christov, C.; Devaquet, J.; Isabey, D.; Brochard, L. Description and microbiology of endotracheal tube biofilm in mechanically ventilated subjects. Respir. Care 2015, 60, 21–29. [Google Scholar] [CrossRef] [Green Version]
- Sanchez-Nieto, J.M.; Torres, A.; Garcia-Cordoba, F.; El-Ebiary, M.; Carrillo, A.; Ruiz, J.; Nunez, M.L.; Niederman, M. Impact of invasive and noninvasive quantitative culture sampling on outcome of ventilator-associated pneumonia: A pilot study. Am. J. Respir. Crit. Care Med. 1998, 157, 371–376. [Google Scholar] [CrossRef]
- Ruiz, M.; Torres, A.; Ewig, S.; Marcos, M.A.; Alcon, A.; Lledo, R.; Asenjo, M.A.; Maldonaldo, A. Noninvasive versus invasive microbial investigation in ventilator-associated pneumonia: Evaluation of outcome. Am. J. Respir. Crit. Care Med. 2000, 162, 119–125. [Google Scholar] [CrossRef]
- Rattani, S.; Farooqi, J.; Jabeen, G.; Chandio, S.; Kash, Q.; Khan, A.; Jabeen, K. Evaluation of semi-quantitative compared to quantitative cultures of tracheal aspirates for the yield of culturable respiratory pathogens—A cross-sectional study. BMC Pulm. Med. 2020, 20, 284. [Google Scholar] [CrossRef] [PubMed]
- Durairaj, L.; Mohamad, Z.; Launspach, J.L.; Ashare, A.; Choi, J.Y.; Rajagopal, S.; Doern, G.V.; Zabner, J. Patterns and density of early tracheal colonization in intensive care unit patients. J. Crit. Care 2009, 24, 114–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chastre, J.; Fagon, J.Y. Ventilator-associated pneumonia. Am. J. Respir. Crit. Care Med. 2002, 165, 867–903. [Google Scholar] [CrossRef] [PubMed]
- Kalil, A.C.; Metersky, M.L.; Klompas, M.; Muscedere, J.; Sweeney, D.A.; Palmer, L.B.; Napolitano, L.M.; O’Grady, N.P.; Bartlett, J.G.; Carratala, J.; et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin. Infect. Dis. 2016, 63, e61–e111. [Google Scholar] [CrossRef]
- Berton, D.C.; Kalil, A.C.; Teixeira, P.J. Quantitative versus qualitative cultures of respiratory secretions for clinical outcomes in patients with ventilator-associated pneumonia. Cochrane Database Syst. Rev. 2014, 10, CD006482. [Google Scholar] [CrossRef] [Green Version]
- Fagon, J.Y.; Chastre, J.; Wolff, M.; Gervais, C.; Parer-Aubas, S.; Stephan, F.; Similowski, T.; Mercat, A.; Diehl, J.L.; Sollet, J.P.; et al. Invasive and noninvasive strategies for management of suspected ventilator-associated pneumonia. A randomized trial. Ann. Intern. Med. 2000, 132, 621–630. [Google Scholar] [CrossRef]
- Canadian Critical Care Trials, G. A randomized trial of diagnostic techniques for ventilator-associated pneumonia. N. Engl. J. Med. 2006, 355, 2619–2630. [Google Scholar] [CrossRef]
- Raman, K.; Nailor, M.D.; Nicolau, D.P.; Aslanzadeh, J.; Nadeau, M.; Kuti, J.L. Early antibiotic discontinuation in patients with clinically suspected ventilator-associated pneumonia and negative quantitative bronchoscopy cultures. Crit. Care Med. 2013, 41, 1656–1663. [Google Scholar] [CrossRef]
- Bonten, M.J.; Bergmans, D.C.; Stobberingh, E.E.; van der Geest, S.; De Leeuw, P.W.; van Tiel, F.H.; Gaillard, C.A. Implementation of bronchoscopic techniques in the diagnosis of ventilator-associated pneumonia to reduce antibiotic use. Am. J. Respir. Crit. Care Med. 1997, 156, 1820–1824. [Google Scholar] [CrossRef]
- Koenig, S.M.; Truwit, J.D. Ventilator-associated pneumonia: Diagnosis, treatment, and prevention. Clin. Microbiol. Rev. 2006, 19, 637–657. [Google Scholar] [CrossRef] [Green Version]
- Furtado, G.H.; Wiskirchen, D.E.; Kuti, J.L.; Nicolau, D.P. Performance of the PIRO score for predicting mortality in patients with ventilator-associated pneumonia. Anaesth. Intensive Care 2012, 40, 285–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Rhee, C.; Kadri, S.S.; Danner, R.L.; Suffredini, A.F.; Massaro, A.F.; Kitch, B.T.; Lee, G.; Klompas, M. Diagnosing sepsis is subjective and highly variable: A survey of intensivists using case vignettes. Crit. Care 2016, 20, 89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klein Klouwenberg, P.M.; Cremer, O.L.; van Vught, L.A.; Ong, D.S.; Frencken, J.F.; Schultz, M.J.; Bonten, M.J.; van der Poll, T. Likelihood of infection in patients with presumed sepsis at the time of intensive care unit admission: A cohort study. Crit. Care 2015, 19, 319. [Google Scholar] [CrossRef] [Green Version]
- Koulenti, D.; Lisboa, T.; Brun-Buisson, C.; Krueger, W.; Macor, A.; Sole-Violan, J.; Diaz, E.; Topeli, A.; DeWaele, J.; Carneiro, A.; et al. Spectrum of practice in the diagnosis of nosocomial pneumonia in patients requiring mechanical ventilation in European intensive care units. Crit. Care Med. 2009, 37, 2360–2368. [Google Scholar] [CrossRef]
- Wirz, Y.; Meier, M.A.; Bouadma, L.; Luyt, C.E.; Wolff, M.; Chastre, J.; Tubach, F.; Schroeder, S.; Nobre, V.; Annane, D.; et al. Effect of procalcitonin-guided antibiotic treatment on clinical outcomes in intensive care unit patients with infection and sepsis patients: A patient-level meta-analysis of randomized trials. Crit. Care 2018, 22, 191. [Google Scholar] [CrossRef] [Green Version]
- Bouadma, L.; Luyt, C.E.; Tubach, F.; Cracco, C.; Alvarez, A.; Schwebel, C.; Schortgen, F.; Lasocki, S.; Veber, B.; Dehoux, M.; et al. Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): A multicentre randomised controlled trial. Lancet 2010, 375, 463–474. [Google Scholar] [CrossRef]
- de Jong, E.; van Oers, J.A.; Beishuizen, A.; Vos, P.; Vermeijden, W.J.; Haas, L.E.; Loef, B.G.; Dormans, T.; van Melsen, G.C.; Kluiters, Y.C.; et al. Efficacy and safety of procalcitonin guidance in reducing the duration of antibiotic treatment in critically ill patients: A randomised, controlled, open-label trial. Lancet Infect. Dis. 2016, 16, 819–827. [Google Scholar] [CrossRef]
- Bloos, F.; Trips, E.; Nierhaus, A.; Briegel, J.; Heyland, D.K.; Jaschinski, U.; Moerer, O.; Weyland, A.; Marx, G.; Grundling, M.; et al. Effect of Sodium Selenite Administration and Procalcitonin-Guided Therapy on Mortality in Patients With Severe Sepsis or Septic Shock: A Randomized Clinical Trial. JAMA Intern. Med. 2016, 176, 1266–1276. [Google Scholar] [CrossRef]
- Kyriazopoulou, E.; Liaskou-Antoniou, L.; Adamis, G.; Panagaki, A.; Melachroinopoulos, N.; Drakou, E.; Marousis, K.; Chrysos, G.; Spyrou, A.; Alexiou, N.; et al. Procalcitonin to Reduce Long-Term Infection-associated Adverse Events in Sepsis. A Randomized Trial. Am. J. Respir. Crit. Care Med. 2021, 203, 202–210. [Google Scholar] [CrossRef]
- Stolz, D.; Smyrnios, N.; Eggimann, P.; Pargger, H.; Thakkar, N.; Siegemund, M.; Marsch, S.; Azzola, A.; Rakic, J.; Mueller, B.; et al. Procalcitonin for reduced antibiotic exposure in ventilator-associated pneumonia: A randomised study. Eur. Respir. J. 2009, 34, 1364–1375. [Google Scholar] [CrossRef] [Green Version]
- Yu, X.Y.; Wang, Y.; Zhong, H.; Dou, Q.L.; Song, Y.L.; Wen, H. Diagnostic value of serum procalcitonin in solid organ transplant recipients: A systematic review and meta-analysis. Transpl. Proc. 2014, 46, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Lima, S.S.; Nobre, V.; de Castro Romanelli, R.M.; Clemente, W.T.; da Silva Bittencourt, H.N.; Melo, A.C.; Salomao, L.C.; Serufo, J.C. Procalcitonin-guided protocol is not useful to manage antibiotic therapy in febrile neutropenia: A randomized controlled trial. Ann. Hematol. 2016, 95, 1169–1176. [Google Scholar] [CrossRef] [PubMed]
- Chae, H.; Bevins, N.; Seymann, G.B.; Fitzgerald, R.L. Diagnostic Value of Procalcitonin in Transplant Patients Receiving Immunosuppressant Drugs: A Retrospective Electronic Medical Record-Based Analysis. Am. J. Clin. Pathol. 2021, 156, 1083–1091. [Google Scholar] [CrossRef]
- Nseir, S.; Di Pompeo, C.; Cavestri, B.; Jozefowicz, E.; Nyunga, M.; Soubrier, S.; Roussel-Delvallez, M.; Saulnier, F.; Mathieu, D.; Durocher, A. Multiple-drug-resistant bacteria in patients with severe acute exacerbation of chronic obstructive pulmonary disease: Prevalence, risk factors, and outcome. Crit. Care Med. 2006, 34, 2959–2966. [Google Scholar] [CrossRef]
- Engler, K.; Muhlemann, K.; Garzoni, C.; Pfahler, H.; Geiser, T.; von Garnier, C. Colonisation with Pseudomonas aeruginosa and antibiotic resistance patterns in COPD patients. Swiss Med. Wkly. 2012, 142, w13509. [Google Scholar] [CrossRef] [PubMed]
- King, P.T.; Holdsworth, S.R.; Freezer, N.J.; Villanueva, E.; Holmes, P.W. Microbiologic follow-up study in adult bronchiectasis. Respir. Med. 2007, 101, 1633–1638. [Google Scholar] [CrossRef] [Green Version]
- Mitchell, S.L.; Shaffer, M.L.; Loeb, M.B.; Givens, J.L.; Habtemariam, D.; Kiely, D.K.; D’Agata, E. Infection management and multidrug-resistant organisms in nursing home residents with advanced dementia. JAMA Intern. Med. 2014, 174, 1660–1667. [Google Scholar] [CrossRef]
- Sickles, E.A.; Greene, W.H.; Wiernik, P.H. Clinical presentation of infection in granulocytopenic patients. Arch. Intern. Med. 1975, 135, 715–719. [Google Scholar] [CrossRef]
- Ordonez, C.L.; Shaughnessy, T.E.; Matthay, M.A.; Fahy, J.V. Increased neutrophil numbers and IL-8 levels in airway secretions in acute severe asthma: Clinical and biologic significance. Am. J. Respir. Crit. Care Med. 2000, 161, 1185–1190. [Google Scholar] [CrossRef]
- Schoemakers, R.J.; Schnabel, R.; Oudhuis, G.J.; Linssen, C.F.; van Mook, W.N.; Verbon, A.; Bergmans, D.C. Alternative diagnosis in the putative ventilator-associated pneumonia patient not meeting lavage-based diagnostic criteria. Scand. J. Infect. Dis. 2014, 46, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.; Carlet, J. Ventilator-associated pneumonia. European Task Force on ventilator-associated pneumonia. Eur. Respir. J. 2001, 17, 1034–1045. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suberviola Canas, B.; Jauregui, R.; Ballesteros, M.A.; Leizaola, O.; Gonzalez-Castro, A.; Castellanos-Ortega, A. Effects of antibiotic administration delay and inadequacy upon the survival of septic shock patients. Med. Intensiva 2015, 39, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Puech, B.; Canivet, C.; Teysseyre, L.; Miltgen, G.; Aujoulat, T.; Caron, M.; Combe, C.; Jabot, J.; Martinet, O.; Allyn, J.; et al. Effect of antibiotic therapy on the prognosis of ventilator-associated pneumonia caused by Stenotrophomonas maltophilia. Ann. Intensive Care 2021, 11, 160. [Google Scholar] [CrossRef]
- Nseir, S.; Martin-Loeches, I.; Makris, D.; Jaillette, E.; Karvouniaris, M.; Valles, J.; Zakynthinos, E.; Artigas, A. Impact of appropriate antimicrobial treatment on transition from ventilator-associated tracheobronchitis to ventilator-associated pneumonia. Crit. Care 2014, 18, R129. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ling, L.; Wong, W.-T.; Lipman, J.; Joynt, G.M. A Narrative Review on the Approach to Antimicrobial Use in Ventilated Patients with Multidrug Resistant Organisms in Respiratory Samples—To Treat or Not to Treat? That Is the Question. Antibiotics 2022, 11, 452. https://doi.org/10.3390/antibiotics11040452
Ling L, Wong W-T, Lipman J, Joynt GM. A Narrative Review on the Approach to Antimicrobial Use in Ventilated Patients with Multidrug Resistant Organisms in Respiratory Samples—To Treat or Not to Treat? That Is the Question. Antibiotics. 2022; 11(4):452. https://doi.org/10.3390/antibiotics11040452
Chicago/Turabian StyleLing, Lowell, Wai-Tat Wong, Jeffrey Lipman, and Gavin Matthew Joynt. 2022. "A Narrative Review on the Approach to Antimicrobial Use in Ventilated Patients with Multidrug Resistant Organisms in Respiratory Samples—To Treat or Not to Treat? That Is the Question" Antibiotics 11, no. 4: 452. https://doi.org/10.3390/antibiotics11040452
APA StyleLing, L., Wong, W.-T., Lipman, J., & Joynt, G. M. (2022). A Narrative Review on the Approach to Antimicrobial Use in Ventilated Patients with Multidrug Resistant Organisms in Respiratory Samples—To Treat or Not to Treat? That Is the Question. Antibiotics, 11(4), 452. https://doi.org/10.3390/antibiotics11040452






