Screening Repurposed Antiviral Small Molecules as Antimycobacterial Compounds by a Lux-Based phoP Promoter-Reporter Platform
Abstract
:1. Introduction
2. Results
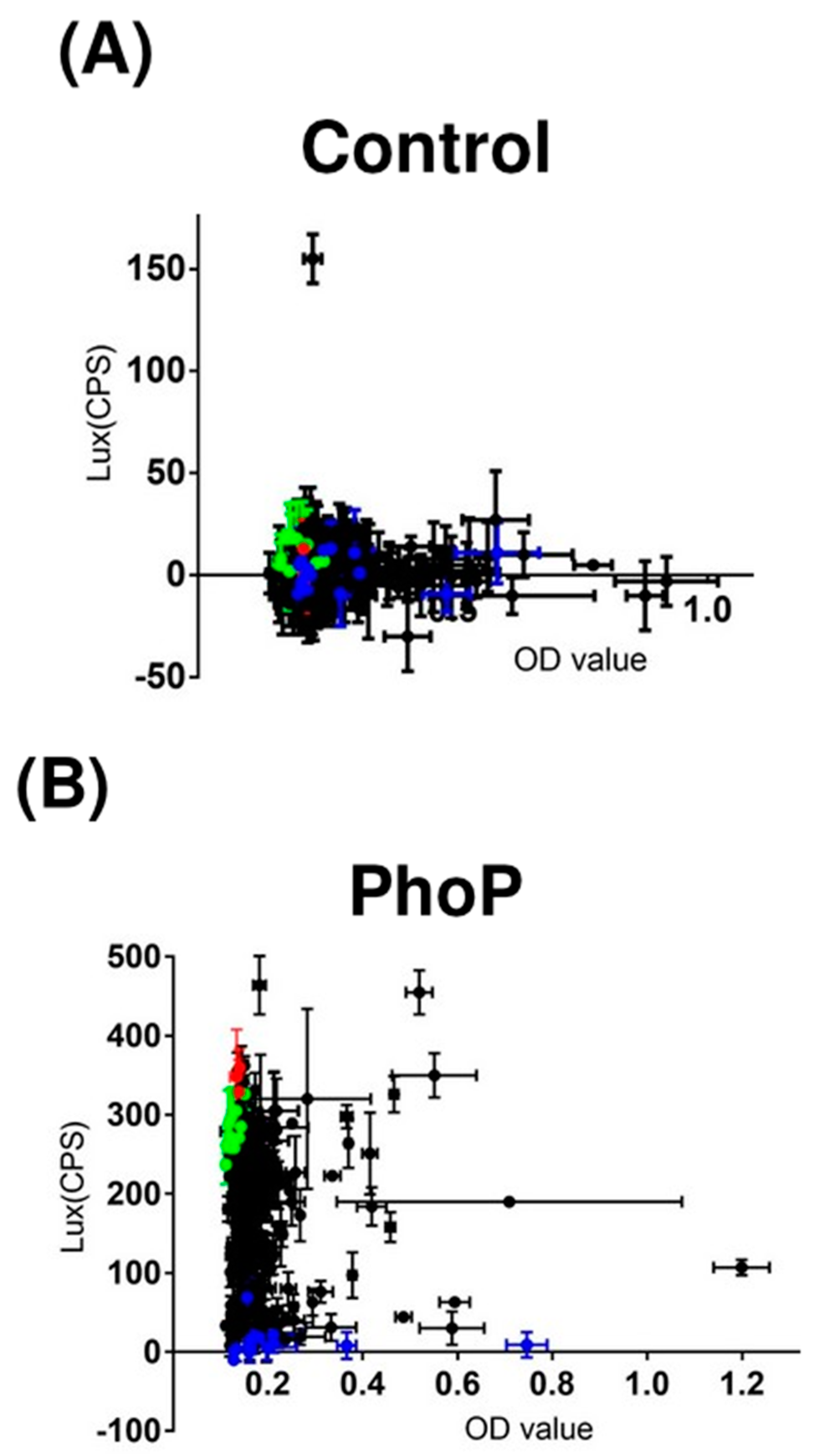
2.1. Construction and Validation of the Lux-Based Promoter-Reporter Platform
2.2. Screening of 320 Antiviral Compounds and 3 Anti-TB Drugs
2.3. MICs and MBCs of Six Compounds against BCG/M. Tuberculosis
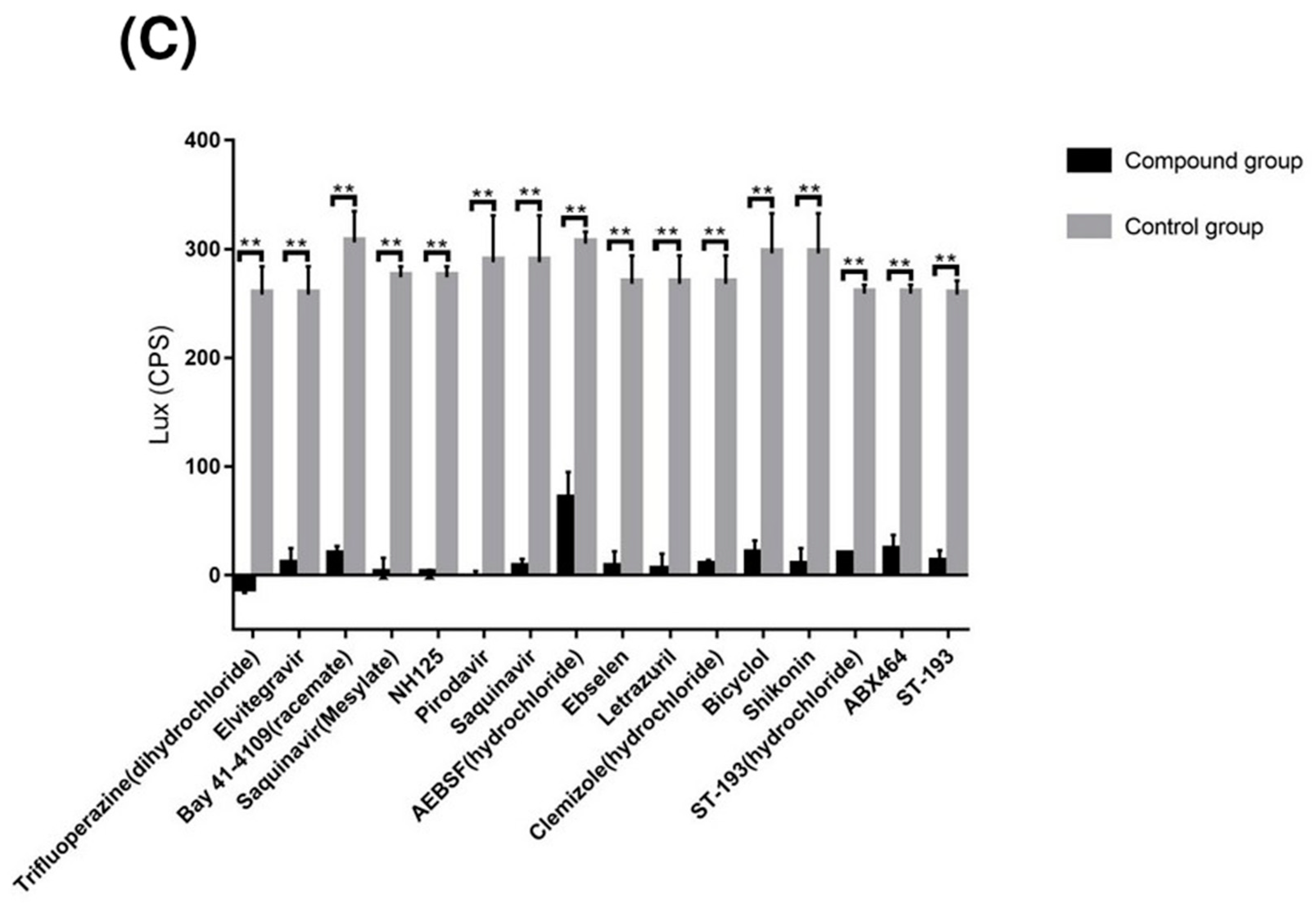
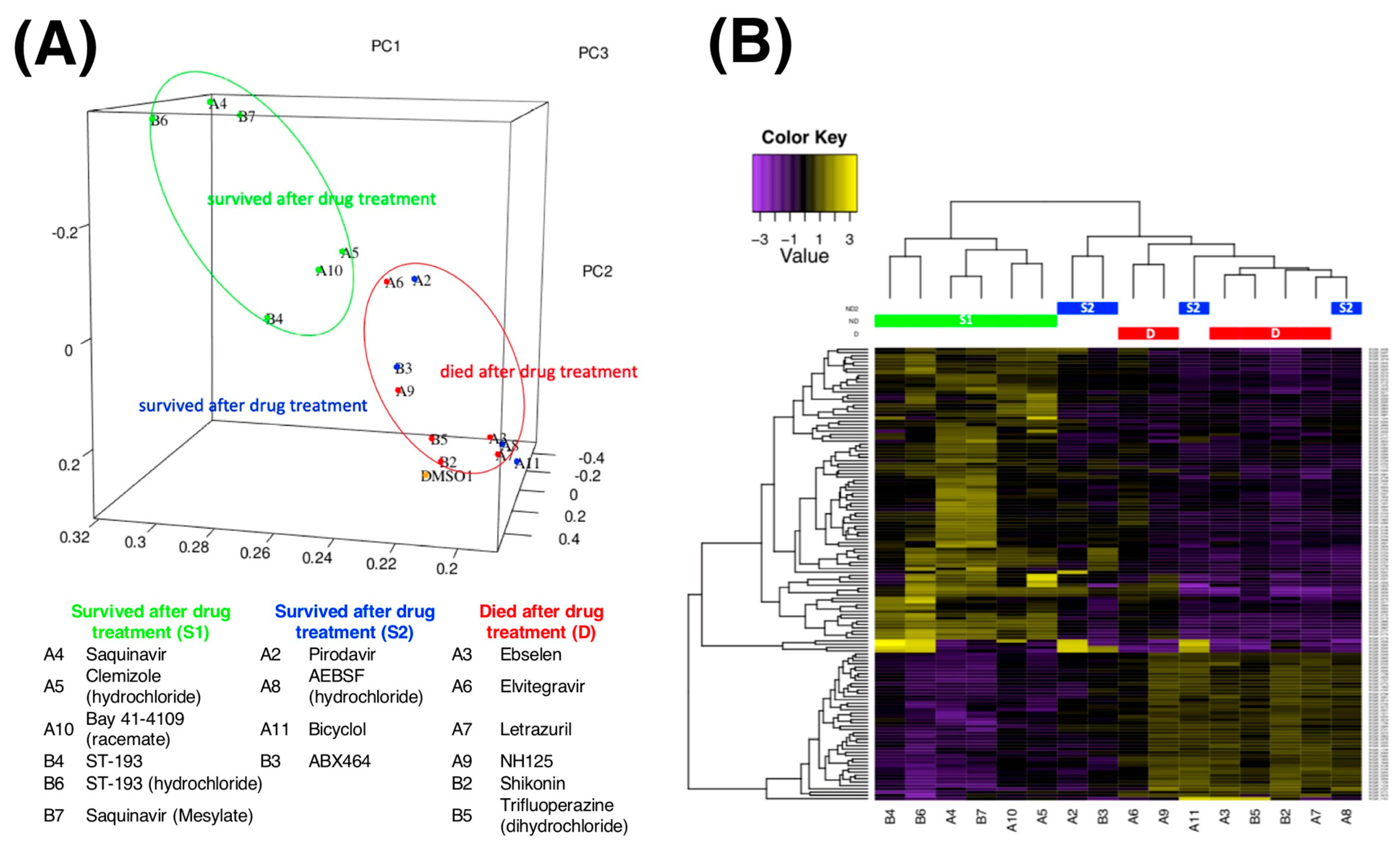
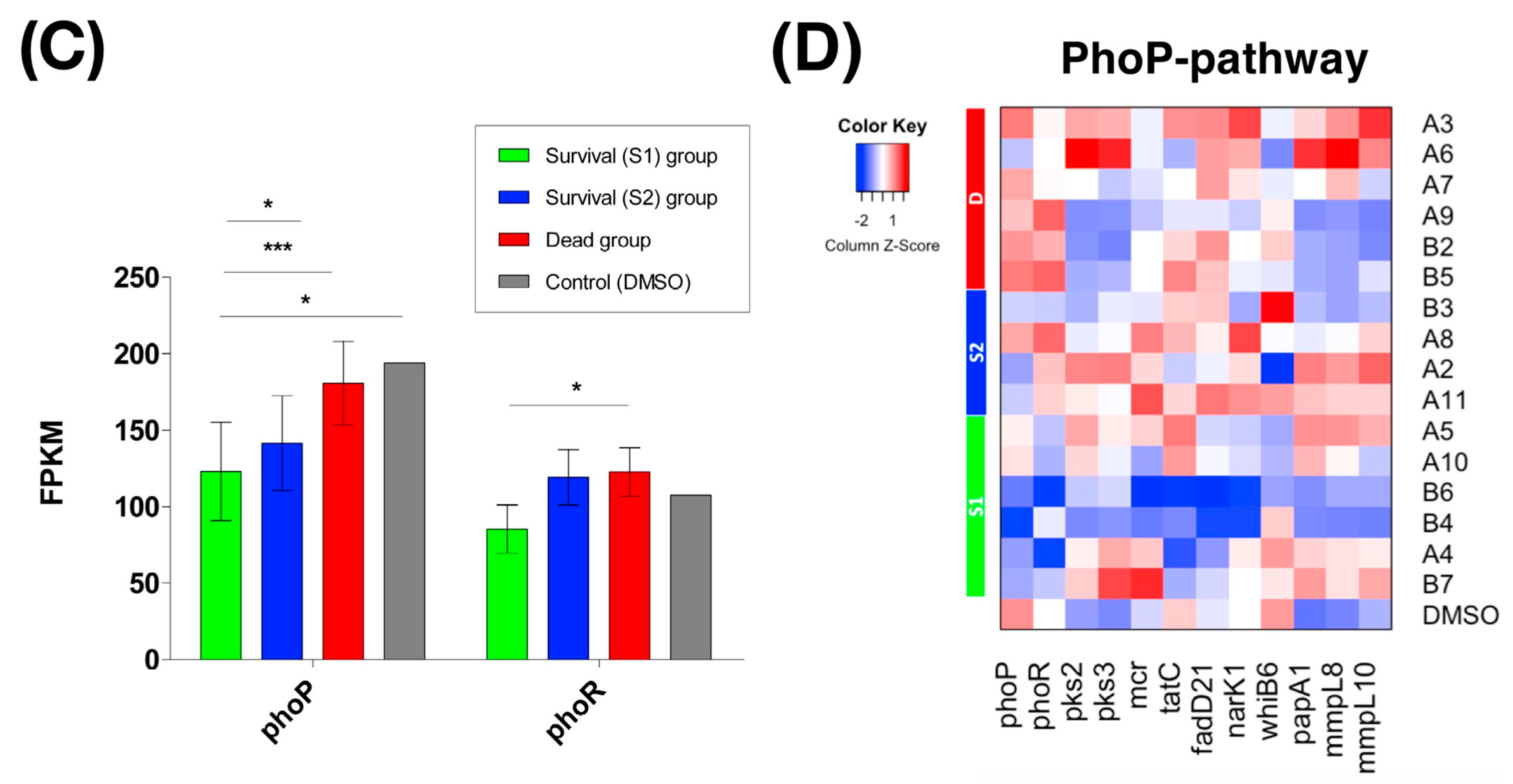
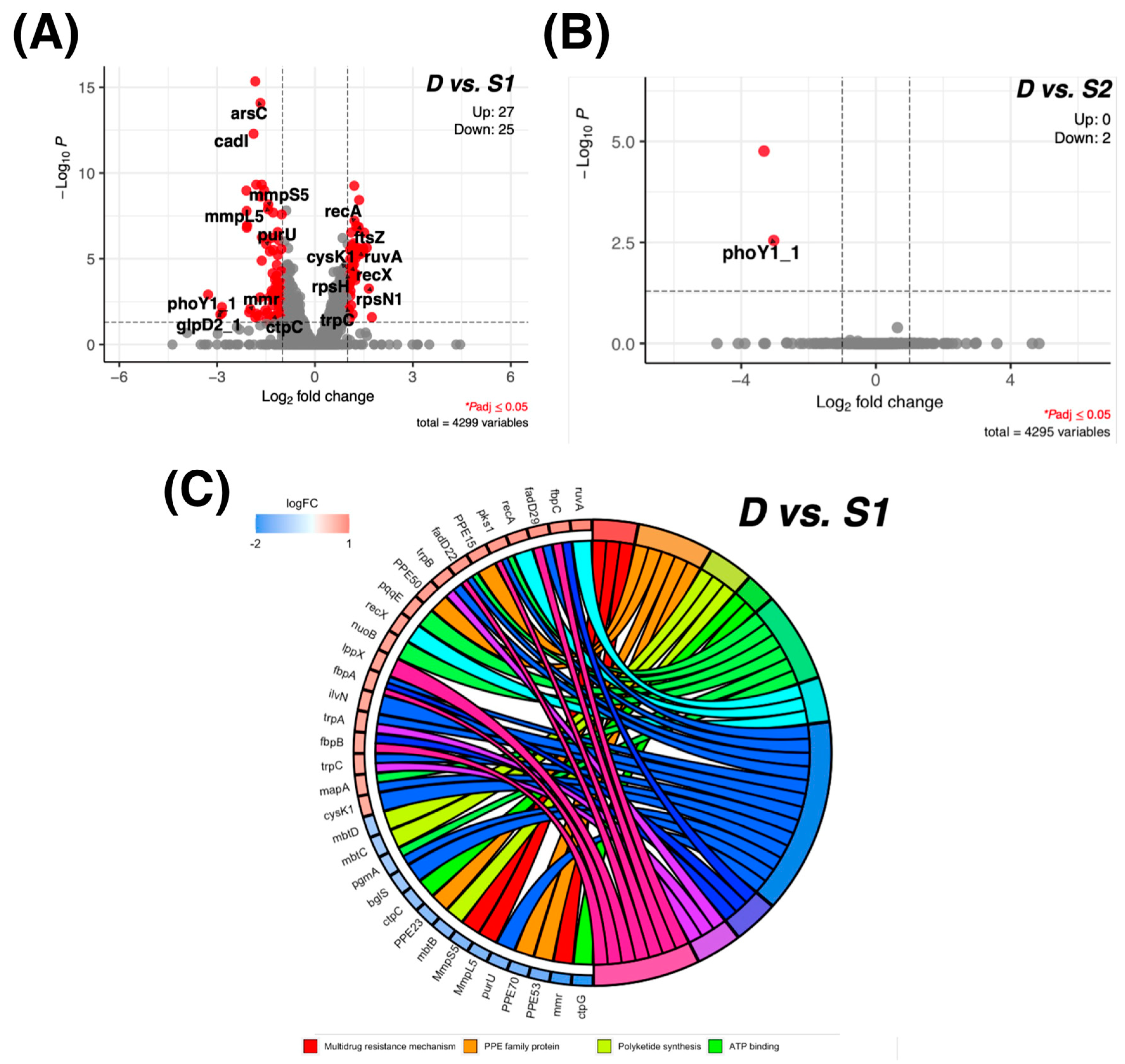
2.4. RNA-Seq Transcriptome Analysis
2.5. Expression of phoP-Associated Pathways upon Compound Treatment
2.6. Molecular Regulation Associated with the Anti-Virulence Process
2.7. Prediction of Drug Targets in the Dead Group
2.8. THP-1 Cytotoxicity of the Small-Molecule Compounds
3. Discussion
4. Materials and Methods
4.1. Bacterial Strains
4.2. Construction of Lux-Based Promoter-Reporter Plasmids and a Negative Control
4.3. Transformation of Lux-Based Reporter Plasmids into M. bovis BCG
4.4. Validating the Correlation of the Lux Signal of the Promoter-Reporter Screening Platform with Phop Gene Expression in M. bovis BCG
4.5. Screening Experiments
4.6. Minimal Inhibitory Concentrations (MICs) and Minimal Bactericidal Concentrations (MBCs) against M. tuberculosis Complex
4.7. RNA-Seq Transcriptome Analysis
4.8. Cell Viability Assay—LDH Assay
4.9. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Global Tuberculosis Report 2020. Available online: https://www.who.int/publications/i/item/9789240013131 (accessed on 15 October 2020).
- Shah, N.S.; Wright, A.; Bai, G.-H.; Barrera, L.; Boulahbal, F.; Martín-Casabona, N.; Drobniewski, F.; Gilpin, C.; Havelková, M.; Lepe, R.; et al. Worldwide Emergence of Extensively Drug-resistant Tuberculosis. Emerg. Infect. Dis. 2007, 13, 380–387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van der Werf, M.J.; Langendam, M.W.; Huitric, E.; Manissero, D. Multidrug resistance after inappropriate tuberculosis treatment: A meta-analysis. Eur. Respir. J. 2012, 39, 1511–1519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zumla, A.; Abubakar, I.; Raviglione, M.; Hoelscher, M.; Ditiu, L.; Mchugh, T.D.; Squire, S.B.; Cox, H.; Ford, N.; McNerney, R.; et al. Drug-resistant tuberculosis—current dilemmas, unanswered questions, challenges, and priority needs. J. Infect. Dis. 2012, 205 (Suppl. 2), S228–S240. [Google Scholar] [CrossRef] [PubMed]
- Stop, T.B. Partnership’s Working Group on New TB Drugs. Clinical Pipeline. Available online: https://www.newtbdrugs.org. (accessed on 24 February 2021).
- Tanner, L.; Denti, P.; Wiesner, L.; Warner, D.F. Drug permeation and metabolism inMycobacterium tuberculosis: Prioritising local exposure as essential criterion in new TB drug development. IUBMB Life 2018, 70, 926–937. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dartois, V. The path of anti-tuberculosis drugs: From blood to lesions to mycobacterial cells. Nat. Rev. Genet. 2014, 12, 159–167. [Google Scholar] [CrossRef] [Green Version]
- Silva, D.R.; Dalcolmo, M.; Tiberi, S.; Arbex, M.A.; Munoz-Torrico, M.; Duarte, R.; D’Ambrosio, L.; Visca, D.; Rendon, A.; Gaga, M.; et al. New and repurposed drugs to treat multidrug- and extensively drug-resistant tuberculosis. J. Bras. de Pneumol. 2018, 44, 153–160. [Google Scholar] [CrossRef]
- An, Q.; Li, C.; Chen, Y.; Deng, Y.; Yang, T.; Luo, Y. Repurposed drug candidates for antituberculosis therapy. Eur. J. Med. Chem. 2020, 192, 112175. [Google Scholar] [CrossRef]
- Mishra, A.K.; Yabaji, S.M.; Dubey, R.K. Evaluation of isoprinosine to be repurposed as an adjunct anti-tuberculosis chemotherapy. Med. Hypotheses 2018, 115, 77–80. [Google Scholar] [CrossRef]
- Dickey, S.W.; Cheung, G.Y.C.; Otto, M. Different drugs for bad bugs: Antivirulence strategies in the age of antibiotic resistance. Nat. Rev. Drug Discov. 2017, 16, 457–471. [Google Scholar] [CrossRef]
- Fernandez-Soto, P.; Bruce, A.J.E.; Fielding, A.J.; Cavet, J.S.; Tabernero, L. Mechanism of catalysis and inhibition of Mycobacterium tuberculosis SapM, implications for the development of novel antivirulence drugs. Sci. Rep. 2019, 9, 10315. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.S.; Krause, R.; Schreiber, J.; Mollenkopf, H.-J.; Kowall, J.; Stein, R.; Jeon, B.-Y.; Kwak, J.-Y.; Song, M.-K.; Patron, J.P.; et al. Mutation in the Transcriptional Regulator PhoP Contributes to Avirulence of Mycobacterium tuberculosis H37Ra Strain. Cell Host Microbe 2008, 3, 97–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pérez, E.; Samper, S.; Bordas, Y.; Guilhot, C.; Gicquel, B.; Martín, C. An essential role for phoP in Mycobacterium tuberculosis virulence. Mol. Microbiol. 2001, 41, 179–187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajwani, R.; Yam, W.C.; Zhang, Y.; Kang, Y.; Wong, B.K.C.; Leung, K.S.S.; Tam, K.K.G.; Tulu, K.T.; Zhu, L.; Siu, G.K.H. Comparative Whole-Genomic Analysis of an Ancient L2 Lineage Mycobacterium tuberculosis Reveals a Novel Phylogenetic Clade and Common Genetic Determinants of Hypervirulent Strains. Front. Cell Infect. Microbiol. 2017, 7, 539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garnier, T.; Eiglmeier, K.; Camus, J.-C.; Medina, N.; Mansoor, H.; Pryor, M.; Duthoy, S.; Grondin, S.; Lacroix, C.; Monsempe, C.; et al. The complete genome sequence of Mycobacterium bovis. Proc. Natl. Acad. Sci. USA 2003, 100, 7877–7882. [Google Scholar] [CrossRef] [Green Version]
- Meza, A.N.; Cambui, C.C.N.; Moreno, A.C.R.; Fessel, M.R.; Balan, A. Mycobacterium tuberculosis CysA2 is a dual sulfurtransferase with activity against thiosulfate and 3-mercaptopyruvate and interacts with mammalian cells. Sci. Rep. 2019, 9, 16791. [Google Scholar] [CrossRef]
- Hatzios, S.; Bertozzi, C.R. The Regulation of Sulfur Metabolism in Mycobacterium tuberculosis. PLoS Pathog. 2011, 7, e1002036. [Google Scholar] [CrossRef]
- Akester, J.N.; Njaria, P.; Nchinda, A.T.; Le Manach, C.; Myrick, A.; Singh, V.; Lawrence, N.; Njoroge, M.; Taylor, D.; Moosa, A.; et al. Synthesis, Structure–Activity Relationship, and Mechanistic Studies of Aminoquinazolinones Displaying Antimycobacterial Activity. ACS Infect. Dis. 2020, 6, 1951–1964. [Google Scholar] [CrossRef]
- Namugenyi, S.B.; Aagesen, A.M.; Elliott, S.R.; Tischler, A.D. Mycobacterium tuberculosis PhoY Proteins Promote Persister Formation by Mediating Pst/SenX3-RegX3 Phosphate Sensing. mBio 2017, 8, e00494-17. [Google Scholar] [CrossRef] [Green Version]
- Viarengo, G.; Sciara, M.I.; Salazar, M.O.; Kieffer, P.M.; Furlán, R.L.E.; Véscovi, E.G. Unsaturated Long Chain Free Fatty Acids Are Input Signals of the Salmonella enterica PhoP/PhoQ Regulatory System. J. Biol. Chem. 2013, 288, 22346–22358. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Wu, S.; Wang, L.; Li, Y.; Shi, F.; Wang, X. Differentiation of bacteria using fatty acid profiles from gas chromatography-tandem mass spectrometry. J. Sci. Food Agric. 2010, 90, 1380–1383. [Google Scholar] [CrossRef]
- Cashman, K.A.; Smith, M.A.; Twenhafel, N.A.; Larson, R.A.; Jones, K.F.; Allen, R.D.; Dai, D.; Chinsangaram, J.; Bolken, T.C.; Hruby, D.E.; et al. Evaluation of Lassa antiviral compound ST-193 in a guinea pig model. Antivir. Res. 2011, 90, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Kerber, R.; Reindl, S.; Romanowski, V.; Gómez, R.; Ogbaini-Emovon, E.; Günther, S.; ter Meulen, J. Research efforts to control highly pathogenic arenaviruses: A summary of the progress and gaps. J. Clin. Virol. 2015, 64, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Larson, R.A.; Dai, D.; Hosack, V.T.; Tan, Y.; Bolken, T.C.; Hruby, D.E.; Amberg, S.M. Identification of a Broad-Spectrum Arenavirus Entry Inhibitor. J. Virol. 2008, 82, 10768–10775. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, A.M.; Rojek, J.M.; Spiropoulou, C.F.; Gundersen, A.T.; Jin, W.; Shaginian, A.; York, J.; Nunberg, J.H.; Boger, D.L.; Oldstone, M.B.A.; et al. Unique Small Molecule Entry Inhibitors of Hemorrhagic Fever Arenaviruses. J. Biol. Chem. 2008, 283, 18734–18742. [Google Scholar] [CrossRef] [Green Version]
- Madu, I.G.; Files, M.; Gharaibeh, D.N.; Moore, A.L.; Jung, K.-H.; Gowen, B.B.; Dai, D.; Jones, K.F.; Tyavanagimatt, S.R.; Burgeson, J.R.; et al. A potent Lassa virus antiviral targets an arenavirus virulence determinant. PLoS Pathog. 2018, 14, e1007439. [Google Scholar] [CrossRef] [Green Version]
- Lienhardt, C.; Nahid, P. Advances in clinical trial design for development of new TB treatments: A call for innovation. PLoS Med. 2019, 16, e1002769. [Google Scholar] [CrossRef]
- World Health Organization. Position Statement on Innovative Clinical Trial Design for Development of New TB Treatments. 2021. WHO Global Tuberculosis Programme: World Health Organization. Available online: https://www.who.int/news/item/19-07-2021-position-statement-on-clinical-trial-designs (accessed on 19 July 2021).
- Andreu, N.; Zelmer, A.; Fletcher, T.; Elkington, P.; Ward, T.; Ripoll, J.; Parish, T.; Bancroft, G.J.; Schaible, U.; Robertson, B.D.; et al. Optimisation of Bioluminescent Reporters for Use with Mycobacteria. PLoS ONE 2010, 5, e10777. [Google Scholar] [CrossRef] [Green Version]
- Johnson, B.K.; Colvin, C.J.; Needle, D.B.; Medie, F.M.; Champion, P.A.D.; Abramovitch, R.B. The Carbonic Anhydrase Inhibitor Ethoxzolamide Inhibits the Mycobacterium tuberculosis PhoPR Regulon and Esx-1 Secretion and Attenuates Virulence. Antimicrob. Agents Chemother. 2015, 59, 4436–4445. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.-H.; Chung, T.D.Y.; Oldenburg, K.R. A Simple Statistical Parameter for Use in Evaluation and Validation of High Throughput Screening Assays. J. Biomol. Screen. 1999, 4, 67–73. [Google Scholar] [CrossRef]
- Zhang, W.; Zhang, Y.; Zheng, H.; Pan, Y.; Liu, H.; Du, P.; Wan, L.; Liu, J.; Zhu, B.; Zhao, G.; et al. Genome Sequencing and Analysis of BCG Vaccine Strains. PLoS ONE 2013, 8, e71243. [Google Scholar] [CrossRef]
- Ritz, N.; Tebruegge, M.; Connell, T.G.; Sievers, A.; Robins-Browne, R.; Curtis, N. Susceptibility of Mycobacterium bovis BCG Vaccine Strains to Antituberculous Antibiotics. Antimicrob. Agents Chemother. 2009, 53, 316–318. [Google Scholar] [CrossRef] [Green Version]
- CLSI. Susceptibility Testing of Mycobacteria, Nocardia spp., and Other Aerobic Actinomycetes; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018; Available online: https://clsi.org/standards/products/microbiology/documents/m24/ (accessed on 23 April 2021).
- Love, M.I.; Huber, W.; Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014, 15, 550. [Google Scholar] [CrossRef] [Green Version]
- Davis, J.J.; Wattam, A.R.; Aziz, R.K.; Brettin, T.; Butler, R.; Butler, R.M.; Chlenski, P.; Conrad, N.; Dickerman, A.; Dietrich, E.M.; et al. The PATRIC Bioinformatics Resource Center: Expanding data and analysis capabilities. Nucleic Acids Res. 2020, 48, D606–D612. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gene Ontology Consortium. The Gene Ontology resource: Enriching a GOld mine. Nucleic Acids Res. 2021, 49, D325–D334. [Google Scholar] [CrossRef] [PubMed]
- Ashburner, M.; Ball, C.A.; Blake, J.A.; Botstein, D.; Butler, H.; Cherry, J.M.; Davis, A.P.; Dolinski, K.; Dwight, S.S.; Eppig, J.T.; et al. Gene ontology: Tool for the unification of biology. The Gene Ontology Consortium. Nat. Genet. 2000, 25, 25–29. [Google Scholar] [CrossRef] [Green Version]
- Mi, H.; Muruganujan, A.; Ebert, D.; Huang, X.; Thomas, P.D. PANTHER version 14: More genomes, a new PANTHER GO-slim and improvements in enrichment analysis tools. Nucleic Acids Res. 2018, 47, D419–D426. [Google Scholar] [CrossRef] [PubMed]



| BCG | H37Rv | MDR-MTB | XDR-MTB | |||||
|---|---|---|---|---|---|---|---|---|
| Compounds | MIC (μM) | MBC (μM) | MIC (μM) | MBC (μM) | MIC (μM) | MBC (μM) | MIC (μM) | MBC (μM) |
| Ebselen | 50 | 100 | 100 | 200 | 50 | 100 | 50 | 50 |
| Elvitegravir | 100 | 200 | >400 | >400 | >400 | >400 | >400 | >400 |
| Letrazuril | 25 | 100 | 200 | >400 | 200 | 400 | 200 | >400 |
| NH125 | 25 | 50 | 50 | 100 | 25 | 50 | 25 | 50 |
| Shikonin | 25 | 50 | 50 | 100 | 25 | 100 | 25 | 100 |
| Trifluoperazine (dihydrochloride) | 12.5 | 25 | 25 | 50 | 25 | 50 | 25 | 50 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, L.; Lee, A.W.-T.; Wu, K.K.-L.; Gao, P.; Tam, K.K.-G.; Rajwani, R.; Chaburte, G.C.; Ng, T.T.-L.; Chan, C.T.-M.; Lao, H.Y.; et al. Screening Repurposed Antiviral Small Molecules as Antimycobacterial Compounds by a Lux-Based phoP Promoter-Reporter Platform. Antibiotics 2022, 11, 369. https://doi.org/10.3390/antibiotics11030369
Zhu L, Lee AW-T, Wu KK-L, Gao P, Tam KK-G, Rajwani R, Chaburte GC, Ng TT-L, Chan CT-M, Lao HY, et al. Screening Repurposed Antiviral Small Molecules as Antimycobacterial Compounds by a Lux-Based phoP Promoter-Reporter Platform. Antibiotics. 2022; 11(3):369. https://doi.org/10.3390/antibiotics11030369
Chicago/Turabian StyleZhu, Li, Annie Wing-Tung Lee, Kelvin Ka-Lok Wu, Peng Gao, Kingsley King-Gee Tam, Rahim Rajwani, Galata Chala Chaburte, Timothy Ting-Leung Ng, Chloe Toi-Mei Chan, Hiu Yin Lao, and et al. 2022. "Screening Repurposed Antiviral Small Molecules as Antimycobacterial Compounds by a Lux-Based phoP Promoter-Reporter Platform" Antibiotics 11, no. 3: 369. https://doi.org/10.3390/antibiotics11030369
APA StyleZhu, L., Lee, A. W.-T., Wu, K. K.-L., Gao, P., Tam, K. K.-G., Rajwani, R., Chaburte, G. C., Ng, T. T.-L., Chan, C. T.-M., Lao, H. Y., Yam, W. C., Kao, R. Y.-T., & Siu, G. K. H. (2022). Screening Repurposed Antiviral Small Molecules as Antimycobacterial Compounds by a Lux-Based phoP Promoter-Reporter Platform. Antibiotics, 11(3), 369. https://doi.org/10.3390/antibiotics11030369






